Abstract
Background:
The MERCI Retrieval system (Concentric Medical, Mountain View, CA) was the first FDA-approved device for mechanical thrombectomy in patients with acute ischemic stroke. It remains one of the most commonly used devices today despite its failure to restore blood flow in approximately 50% of the occlusions after technically successful deployment and retrieval. It remains unclear whether additional endovascular techniques or continued use of MERCI device can achieve recanalization post-MERCI failure.
Objective:
To analyze the outcome of continued MERCI retriever use compared with other endovascular techniques after initial failure.
Methods:
Failure of MERCI retriever was defined by successful deployment and retrieval of MERCI across target occlusion without recanalization in a single pass. Pre- and post-treatment cerebral angiogram was classified using the Qureshi Grading Scale (QGS). Recanalization was defined by a reduction in ≥ 1 QGS grade between pre- and post-treatment cerebral angiogram in the Qureshi Grading Scale (QGS).We ascertained and compared the angiographic and clinical results with continued use of MERCI retriever or other endovascular techniques in patients following MERCI failure.
Results:
A total of 40 patients (53% men) had MERCI retrieval in this cohort with a mean age (±standard deviation) of 66.8 years ± 16 years and a mean admission National Institutes of Health Stroke Scale (NIHSS) score of 16.8 ± 6.7. Of the 40 patients treated with MERCI retrieval, there were 26 patients with MERCI failure. In group 1, there were 11 patients who underwent continued MERCI use and group 2 consisted of 15 patients who underwent an alternate endovascular technique. There was no significant difference in age, risk factors, or outcomes between the groups. The rate of recanalization (82% versus 80%, p = 1.0), asymptomatic intra cerebral hemorrhage (18% versus 13%, p = 0.77) and favorable outcome at discharge (27% versus 20%, p = 0.66) were similar amongst the two groups.
Conclusions:
Continued attempts using the MERCI device did not result in higher recanalization rates when compared to alternate endovascular treatment modalities following initial MERCI failure. Both techniques produced comparable rates of recanalization and favorable outcome.
Keywords: Merci retrieval, mechanical thrombectomy, intra-arterial thrombolysis, endovascular treatment
INTRODUCTION:
In patients with ischemic stroke that arrive outside of the intravenous (IV) recombinant tissue plasminogen activator (rt-PA) time window, have contraindications to IV rt-PA, or in those whom IV rt-PA has not resulted in improvement, mechanical thrombectomy devices along with other intra-arterial thrombolysis techniques are frequently used. The MERCI Retriever (Concentric Medical, Mountain View, California) was the first device to obtain clearance from the FDA through its 510(k) process and was approved to “restore blood flow in the neurovasculature by removing thrombus in patients experiencing ischemic stroke who are ineligible for the treatment with intravenous rt-PA or who fail intravenous rt-PA”1. Smith et al2 reported recanalization rate 46% on intention to treat analysis and 48% of patients in whom the device was properly deployed in patients with ischemic stroke. Recanalization was defined as achieving Thombolysis In Myocardial Infarction (TIMI) II or III flow in all treatable vessels3. The rate was higher than the rate of spontaneous recanalization of 18%, two hours after initial angiography that was reported in Prolyse in Acute Cerebral Thromboembolism II study (PROACT-II)4. Multiple passes of the MERCI retriever may be required to achieve recanalization in the subset of patients that show no angiographic improvement after a single pass2. However, aspirating the device prior to initiating a second pass entails re-guiding the device through the tortuous vasculature-a time consuming process in which a different intervention could be considered. For patients that fail to recanalize with multiple passes using the MERCI retriever, endovascular treatment modalities such as intra-arterial thrombolytics, balloon angioplasty, and Penumbra system (Penumbra, Alameda, California) may be utilized. To the best of our knowledge the success rates of such methods after MERCI failure to achieve recanalization have not been reported. Our study is directed towards determining whether multiple passes using the MERCI device yields a higher rate of recanalization compared with a different endovascular intervention following initial MERCI failure.
METHODS
A retrospective review was performed including patients treated with mechanical thrombectomy for acute ischemic stroke between January 2007 and June 2010 at two hospitals affiliated to the University of Minnesota, the University of Minnesota Medical Center and Hennepin County Medical Center. Patients were identified from a prospective endovascular procedure database, and the Institutional Review Board (IRB) at these hospitals approved the data collection protocol. The database was updated and maintained on a daily basis by staff at the institutions, and then cross-checked against the acute ischemic stroke admission diagnosis reports that are provided by the coding departments of the participating hospitals at the end of each month. We collected relevant information for each patient from the individual hospital records. Demographic data including age, sex, and race/ethnicity was collected from patient profile documented during admission registration. We collected data regarding stroke risk factors present before onset of stroke symptoms (as mentioned in the admission and/or discharge notes) e.g., hypertension, dyslipidemia, diabetes mellitus, atrial fibrillation, and coronary artery disease. Data regarding severity of stroke and baseline function was obtained by National Institutes of Health Stroke Scale(NIHSS)5 scores before and after the procedure. The functional status of the patients was assessed by using modified Rankin Scale (mRS)6–8 obtained from the discharge note . Good neurological outcome was defined as mRS 0-2. Arterial occlusion on pre- and post-treatment cerebral angiogram was classified by the Qureshi Grading Scale (QGS), a previously validated grading scheme based on the occlusion location and collateral supply to the affected region9. Recanalization was defined by a reduction in ≥ 1 grade from baseline in the QGS consistent with previous studies10. Failure of MERCI device was defined by successful deployment and retrieval of MERCI across target occlusion without recanalization in a single pass (Figures 1, 2 and 3). It has been shown that multiple attempts using MERCI retriever may be required to achieve angiographic recanalization2,11; however such technique is associated with similar risks as initiating a new therapy. We classified additional endovascular treatment into two groups: continued use of MERCI device or new strategy using a different device and/or additional intra-arterial thrombolytic administration. The primary safety end points were symptomatic intra-cerebral hemorrhage (ICH) and in- hospital death. ICH was considered symptomatic (sICH) if it was previously not seen on a non-contrast CT scan and was related to neurological deterioration defined by a 4 points increase in NIHSS score when compared to previous clinical assessment. All data were descriptively presented using mean ± standard deviation (SD) for continuous data and frequencies for categorical data. We assessed if cardiovascular risk factors, and severity of disease, were similar between patients treated with continued MERCI device and those treated with additional endovascular treatments. Statistical association was assessed with analysis of variance (ANOVA) and chi-square test for continuous and categorical variables, respectively. We compared the rates of favorable clinical outcome, sICH, and rate of recanalization, between the two patient groups. A p value <0.05 was considered significant. Subsequently, we performed multivariate logistic regression models to see the effect additional rescue devices after MERCI failure on clinical outcomes. We adjusted for age, gender and admission NIHSS in these models. All analyses were performed using the SAS statistical software (SAS, Cary, North Carolina).
Figure 1:
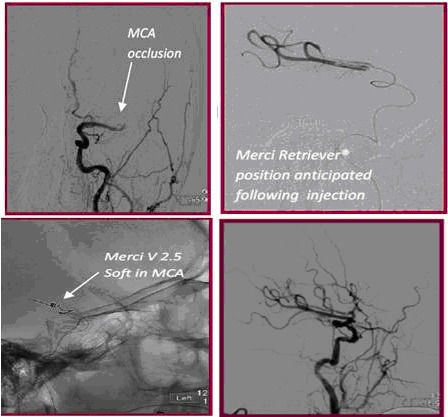
A, Occlusion of the MCA, B, Microcatheter run to determine positioning of the MERCI retriever C, Deployment of MERCI in the middle cerebral artery D, Successful recanalization post MERCI retrieval
RESULTS
A total of 40 acute ischemic stroke patients (53% men) were treated with the MERCI retriever. The mean age (±SD) of 66.8 years ± 16 years), mean (±SD) admission NIHSS score was 16.8 ± 6.7 and the average procedure time was 1.55 hours. The data was stratified into two groups based on the treatment modality that lead to recanalization. Of the 40 treated patients, there were 26 patients with MERCI failure. In group 1, there were 11 patients who underwent continued MERCI use and group 2 consisted of 15 patients who had an alternate endovascular technique. There were no significant differences in regards to age, gender and cardiovascular risk factors or type of treated vessel between the two groups (Table 1). The recanalization rate (82% versus 80%, p = 1.0), and favorable outcome at discharge (27% versus 20%, p = 0.66) were not significantly different between the two groups (Table 1). sICH was not observed in either group but asymptomatic ICHs occurred after the procedure in similar rates in the two groups (18% versus 13%, p = 0.77). There were no other complications such as arterial perforations, dissections or access site hematomas.
Table 1:
Patient demographics, thrombolytic treatment, site of vascular occlusion, and clinical outcome of patients with acute ischemic after MERCI retriever failure.
| Continued MERCI | Another endovascular technique | |||
|---|---|---|---|---|
| Total Patients | 11 | 15 | p value | |
| Mean age mean (±SD) | 60.2±15.4 | 69.1±16.2 | 0.18 | |
| Admission NIHSS score mean (±SD) | 17.7±5.8 | 16±5.8 | 0.59 | |
| Male | 5 (45%) | 8 (53%) | 0.69 | |
| Use of thrombolytic treatment | ||||
| Intra-arterial thrombolytic | 8 (73%) | 12 (80%) | 0.66 | |
| Intravenous thrombolytic | 6 (55%) | 7 (46%) | 0.69 | |
| Artery treatment | ||||
| Middle cerebral artery | 10 (91%) | 9 (60%) | 0.17 | |
| Internal carotid artery | 1 (9%) | 6 (40%) | ||
| Clinical Outcome | ||||
| Good clinical outcome mRS (0-2) | 3 (27%) | 3 (20) | 0.66 | |
| Asymptomatic intra cerebral hemorrhage | 2 (18%) | 2 (13%) | 0.77 | |
| Symptomatic intra cerebral hemorrhage | 0 | 0 | - | |
| Recanalization | 9 (82%) | 12 (80%) | 1.0 | |
| NIHSS score improvement at Discharge ≥ 4* | 6 (55%) | 8 (53%) | 1.0 | |
DISCUSSION
It is currently unclear which treatment modality yields a higher rate of recanalization following an unsuccessful thrombectomy using the MERCI retriever. We achieved an ~80% rate of recanalization in cases where MERCI was continued (group 1), as well another device was used (group 2). Failure to restore circulation in a single pass using the MERCI device was followed by either continued use of MERCI, or additional doses of intra-arterial thrombolytics, and/or angioplasty. The superiority of a successful thrombectomy over failed thrombectomy requiring adjunct therapy is difficult to ascertain, as both strategies were able recanalize the vessel in question with similar clinical outcomes.
Recanalization is an important predictor of good clinical outcome 11–14. The Mechanical Embolus Removal in Cerebral Ischemia (MERCI)2 trial observed a higher rate (four fold) of favorable outcomes (mRS score <2) at 90 days in patients with successful recanalization when compared to those with unsuccessful recanalization (46% versus 10%), and mortality was significantly lower (32% versus 54%). Furthermore, data from MULTI-MERCI11, an international multicenter single arm trial outlined similar findings of higher favorable outcomes (mRS ≤2) at 90 days in 49% of patients who achieved successful recanalization versus 10% who did not, along with a lower mortality rate of 25% vs. 52%, respectively. We observed a numerically higher, but statistically insignificant rate of good clinical outcome in the subset of patients that recanalized in a single MERCI pass, when compared to multiple MERCI attempts, and MERCI plus rescue (43% versus 27% versus 20%, p = 0.39). NIHSS score improvement at discharge of ≥4 was similar in all treatment groups.
In accordance with current FDA guidelines, IV rt-PA was given to all patients in whom it was indicated prior to initiating intervention with the MERCI retriever (55% and 46% of the patients in groups 1 and 2, respectively). The use of IV drugs however, is coupled with numerous limitations along with limited efficacy in the management of difficult patients who present with a high clot burden, multiple co-morbidities, and/or after the narrow time window advocated for the use of IV thrombolytics has elapsed. Endovascular approaches to achieve recanalization offer the potential of faster restoration of blood flow along with an extension in the treatment time window when compared to IV thrombolysis. Intra-arterial thrombolytics were administered in both subset of patients, 73% in group 1 and 80% in group 2 as it allows for higher concentrations of thrombolytics to be directly delivered at the site of occlusion with minimal systemic exposure.
While the value of other thrombectomy strategies such as angioplasty or stent placement has been shown previously15, the role of these strategies in patients who failed MERCI retriever is not well understood. Angioplasty was used in combination with thrombolytics in 15 of our patients post MERCI failure, resulting in 80% recanalization rate. Balloon angioplasty is used as a rescue modality in patients that were non-responsive to treatment with IV/Intra-arterial thrombolysis and mechanical clot disruption. Ringer et al 16 regarded balloon angioplasty as an effective alternative in patients that were resistant to Intra-arterial thrombolysis, with the added benefit of preventing reocclusion in a stenotic artery. The safety profile of angioplasty is being improved by employing low pressure more compliant balloons to achieve revascularization17. Advances in angioplasty using self–expanding stents for flow restoration also show promise. The Stent-Assisted Recanalization in Acute Ischemic Stroke (SARIS)18 trial reported a 100% recanalization rate in 20 patients with sICH occurring in only 1 patient (5%). The 30 day, post-procedural mRS was 0 or 1 in 45% of the treated patients. Currently, temporary stent–bypass with retrievable devices are being explored as an alternate to having a permanent stent19. This treatment modality however, is accompanied by the need for prolonged dual anti-platelet therapy that carries a risk of hemorrhage.
The majority of our patients (73%) had middle cerebral artery distribution strokes - the most commonly affected site of arterial occlusion in patients experiencing severe stroke of less than 6 hours duration20. However, it is interesting to note the discrepancy in internal carotid artery strokes, 9% in group one versus 40% in group two. This may indicate that the MERCI device is less effective in the internal carotid artery.
Although part of our data was prospectively collected, the main limitation of this study is attributed to its retrospective nature with broad principle for approaching MERCI retriever failure. Furthermore, due to the non-standardization of treatment, small number of patients analyzed and lack of a randomized control arm, no definitive conclusion can be drawn. Prospective large scale randomized studies are needed to demonstrate the superiority of continued MERCI device passes when compared to different endovascular interventions.
CONCLUSION
In case of MERCI retriever failure, additional passes or use of alternative endovascular technique can lead to similar recanalization and favorable outcome rates. This study illustrates the importance of persistent attempts to recanalize an occluded vessel in patients suffering from acute ischemic stroke. Continued MERCI passes or switching to another technique after initial MERCI failure both resulted in high rates of recanalization. There was no increase in sICH or mortality in this small series of patients.
References
- 1.Baker WL, Colby JA, Tongbram V, Talati R, Silverman IE, White CM, et al. Neurothrombectomy devices for the treatment of acute ischemic stroke: State of the evidence. Annals of internal medicine. 2011;154:243–252. doi: 10.7326/0003-4819-154-4-201102150-00306. [DOI] [PubMed] [Google Scholar]
- 2.Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: Results of the merci trial. Stroke; a journal of cerebral circulation. 2005;36:1432–1438. doi: 10.1161/01.STR.0000171066.25248.1d. [DOI] [PubMed] [Google Scholar]
- 3.Williams DO, Borer J, Braunwald E, Chesebro JH, Cohen LS, Dalen J, et al. Intravenous recombinant tissue-type plasminogen activator in patients with acute myocardial infarction: A report from the nhlbi thrombolysis in myocardial infarction trial. Circulation . 1986;73:338–346. doi: 10.1161/01.cir.73.2.338. [DOI] [PubMed] [Google Scholar]
- 4.Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The proact ii study: A randomized controlled trial. Prolyse in acute cerebral thromboembolism. JAMA : the journal of the American Medical Association . 1999;282:2003–2011. doi: 10.1001/jama.282.21.2003. [DOI] [PubMed] [Google Scholar]
- 5.Brott T, Adams HP, Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke; a journal of cerebral circulation. 1989;20:864–870. doi: 10.1161/01.str.20.7.864. [DOI] [PubMed] [Google Scholar]
- 6.Rankin J. Cerebral vascular accidents in patients over the age of 60. Ii. Prognosis. Scottish medical journal. 1957;2:200–215. doi: 10.1177/003693305700200504. [DOI] [PubMed] [Google Scholar]
- 7.Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke; a journal of cerebral circulation. 1988;19:1497–1500. doi: 10.1161/01.str.19.12.1497. [DOI] [PubMed] [Google Scholar]
- 8.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke; a journal of cerebral circulation. 1988;19:604–607. doi: 10.1161/01.str.19.5.604. [DOI] [PubMed] [Google Scholar]
- 9.Qureshi AI. New grading system for angiographic evaluation of arterial occlusions and recanalization response to intra-arterial thrombolysis in acute ischemic stroke. Neurosurgery. 2002;50:1405–1414. doi: 10.1097/00006123-200206000-00049. discussion 1414-1405. [DOI] [PubMed] [Google Scholar]
- 10.Mohammad YM, Christoforidis GA, Bourekas EC, Slivka AP. Qureshi grading scheme predicts subsequent volume of brain infarction following intra-arterial thrombolysis in patients with acute anterior circulation ischemic stroke. Journal of neuroimaging : official journal of the American Society of Neuroimaging. 2008;18:262–267. doi: 10.1111/j.1552-6569.2007.00233.x. [DOI] [PubMed] [Google Scholar]
- 11.Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: Final results of the multi merci trial. Stroke; a journal of cerebral circulation. 2008;39:1205–1212. doi: 10.1161/STROKEAHA.107.497115. [DOI] [PubMed] [Google Scholar]
- 12.del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. Proact: A phase ii randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. Proact investigators. Prolyse in acute cerebral thromboembolism. Stroke; a journal of cerebral circulation . 1998;29:4–11. doi: 10.1161/01.str.29.1.4. [DOI] [PubMed] [Google Scholar]
- 13.Christoforidis GA, Mohammad Y, Kehagias D, Avutu B, Slivka AP. Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR. American journal of neuroradiology. 2005;26:1789–1797. [PMC free article] [PubMed] [Google Scholar]
- 14.Suarez JI, Sunshine JL, Tarr R, Zaidat O, Selman WR, Kernich C, et al. Predictors of clinical improvement, angiographic recanalization, and intracranial hemorrhage after intra-arterial thrombolysis for acute ischemic stroke. Stroke; a journal of cerebral circulation. 1999;30:2094–2100. doi: 10.1161/01.str.30.10.2094. [DOI] [PubMed] [Google Scholar]
- 15.Qureshi AI, Siddiqui AM, Suri MF, Kim SH, Ali Z, Yahia AM, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: A prospective study. Neurosurgery. 2002;51:1319–1327. doi: 10.1097/00006123-200211000-00040. discussion 1327-1319. [DOI] [PubMed] [Google Scholar]
- 16.Ringer AJ, Qureshi AI, Fessler RD, Guterman LR, Hopkins LN. Angioplasty of intracranial occlusion resistant to thrombolysis in acute ischemic stroke. Neurosurgery. 2001;48:1282–1288. doi: 10.1097/00006123-200106000-00019. discussion 1288-1290. [DOI] [PubMed] [Google Scholar]
- 17.Nogueira RG, Schwamm LH, Buonanno FS, Koroshetz WJ, Yoo AJ, Rabinov JD, et al. Low-pressure balloon angioplasty with adjuvant pharmacological therapy in patients with acute ischemic stroke caused by intracranial arterial occlusions. Neuroradiology. 2008;50:331–340. doi: 10.1007/s00234-007-0340-z. [DOI] [PubMed] [Google Scholar]
- 18.Levy EI, Siddiqui AH, Crumlish A, Snyder KV, Hauck EF, Fiorella DJ, et al. First food and drug administration-approved prospective trial of primary intracranial stenting for acute stroke: Saris (stent-assisted recanalization in acute ischemic stroke) Stroke; a journal of cerebral circulation. 2009;40:3552–3556. doi: 10.1161/STROKEAHA.109.561274. [DOI] [PubMed] [Google Scholar]
- 19.Jahan R. Solitaire flow-restoration device for treatment of acute ischemic stroke: Safety and recanalization efficacy study in a swine vessel occlusion model. AJNR. American journal of neuroradiology. 2010;31:1938–1943. doi: 10.3174/ajnr.A2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.del Zoppo GJ, Poeck K, Pessin MS, Wolpert SM, Furlan AJ, Ferbert A, et al. Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Annals of neurology. 1992;32:78–86. doi: 10.1002/ana.410320113. [DOI] [PubMed] [Google Scholar]


