Abstract
Braun (murein) lipoprotein (Lpp) and lipopolysaccharide (LPS) are major components of the outer membranes of Enterobacteriaceae family members that are capable of triggering inflammatory immune responses by activating Toll-like receptors 2 and 4, respectively. Expanding on earlier studies that demonstrated a role played by Lpp in Yersinia pestis virulence in mouse models of bubonic and pneumonic plague, we characterized an msbB in-frame deletion mutant incapable of producing an acyltransferase that is responsible for the addition of lauric acid to the lipid A moiety of LPS, as well as a Δlpp ΔmsbB double mutant of the highly virulent Y. pestis CO92 strain. Although the ΔmsbB single mutant was minimally attenuated, the Δlpp single mutant and the Δlpp ΔmsbB double mutant were significantly more attenuated than the isogenic wild-type (WT) bacterium in bubonic and pneumonic animal models (mouse and rat) of plague. These data correlated with greatly reduced survivability of the aforementioned mutants in murine macrophages. Furthermore, the Δlpp ΔmsbB double mutant was grossly compromised in its ability to disseminate to distal organs in mice and in evoking cytokines/chemokines in infected animal tissues. Importantly, mice that survived challenge with the Δlpp ΔmsbB double mutant, but not the Δlpp or ΔmsbB single mutant, in a pneumonic plague model were significantly protected against a subsequent lethal WT CO92 rechallenge. These data were substantiated by the fact that the Δlpp ΔmsbB double mutant maintained an immunogenicity comparable to that of the WT strain and induced long-lasting T-cell responses against heat-killed WT CO92 antigens. Taken together, the data indicate that deletion of the msbB gene augmented the attenuation of the Δlpp mutant by crippling the spread of the double mutant to the peripheral organs of animals and by inducing cytokine/chemokine responses. Thus, the Δlpp ΔmsbB double mutant could provide a new live-attenuated background vaccine candidate strain, and this should be explored in the future.
INTRODUCTION
Yersinia pestis is the causative agent of plague, which has historically been credited for over 200 million human deaths worldwide (1). The organism is transmitted to humans through the bite of an infected flea or inhalation of the organism, resulting in bubonic, septicemic, or pneumonic plague. The latter two forms of plague are highly contagious and almost always fatal if antibiotic treatment is not initiated within 24 h of the onset of symptoms (2, 3). Today, Y. pestis infections remain a serious public health threat in several regions of the world (4), and the ability of this microbe to easily be weaponized represents a serious biothreat (5).
In Gram-negative bacteria of the Enterobacteriaceae family, lipopolysaccharide (LPS) and Braun (murein) lipoprotein (Lpp) are the most abundant components of the outer membrane and are important in maintaining the integrity of the bacterial cell envelope (6, 7). The maturation of Lpp requires modification of the lipid moiety, which is catalyzed by glycerol transferase (Lgt), O-acyltransferase, signal peptidase II, and N-acyltransferase (Lnt) (8). LPS, on the other hand, is composed of an O antigen, a polysaccharide core, and a lipid A domain, the latter of which represents a hydrophobic anchor that creates a permeability barrier for bacteria against toxic compounds encountered in the environment and within the host (9, 10). In most Gram-negative bacteria, lipid A is initially synthesized as a primary structure called lipid IVA, which can then be acylated further with laureate (C12) or myristate (C14) by the action of the so-called late acyltransferases HtrB (LpxL) and MsbB (LpxM) or LpxP, respectively (9, 11–13).
Unlike the other two enteropathogenic Yersinia species (Y. pseudotuberculosis and Y. enterocolitica), Y. pestis synthesizes a rough LPS which lacks the O antigen (14, 15). Interestingly, the change from tetra-acylated lipid A at 37°C to hexa-acylated lipid A at 21 to 27°C is the characteristic trait for all yersiniae (9, 16–20), and it is the absence of hexa-acylated lipid A in yersiniae at 37°C that prevents activation of Toll-like receptor 4 (TLR-4) (9, 16, 18, 20). Based on the published sequences for the Y. pestis genomes (20–23), only two late acyltransferases, LpxP and LpxM (MsbB), have been identified. The absence of LpxL and the inactivity of LpxP and MsbB at high temperatures are believed to be responsible for the lack of hexa-acylated lipid A in yersiniae at 37°C (9, 16, 18, 20). The acyltransferase MsbB in yersiniae is responsible for the addition of C12 to lipid A, while in other enteric bacteria, such as Escherichia coli and Salmonella enterica serovar Typhimurium, MsbB is responsible for the addition of C14 to lipid A (16).
Both Lpp and LPS induce toxic and biological responses within hosts through their lipid domains by inducing high levels of cytokines such as tumor necrosis factor alpha (TNF-α), gamma interferon (IFN-γ), interleukin-1β (IL-1β), and IL-6. Similarly, both Lpp and LPS activate the complement cascade, coagulation cascade, and other inflammatory mediators (24–27). In addition, Lpp purified from Y. enterocolitica synergizes with its LPS to induce production of proinflammatory cytokines in vitro and in vivo, leading to septic shock (28). Lpp binds to TLR-2 to activate host cells (27, 29), while LPS interacts with a host cell receptor complex consisting of TLR-4 and its coreceptor, myeloid differentiation protein 2 (MD-2), to induce cellular responses (30–35).
Vaccination represents an effective tool for combating infectious diseases; however, currently used live-attenuated plague vaccines have significant limitations (36). One of the drawbacks of these vaccines includes undesirable local and systemic reactions that are caused mainly by the inflammatory property of LPS. Although Y. pestis synthesizes less potent tetra-acylated LPS at 37°C, the current live plague vaccines, such as the EV76 strain, used in the countries of the former Soviet Union, is usually grown at 28°C. At this temperature, Y. pestis synthesizes the highly potent hexa-acylated LPS (14, 37), and it is used for human immunization as a single dose of 5.8 × 106 CFU (38). This vaccine strain is preferably grown at 28°C due to the observation that Y. pestis cells are more viable and survive long-term storage better at this temperature (14, 37). Consequently, these vaccines are not licensed in Western countries (5, 39).
Studies have shown that hexa-acylated lipid A tends to be a much stronger stimulator of human cells than tetra-acylated lipid A. Several research groups have reported that Y. pestis strains producing hexa-acylated lipid A at 37°C via expression of additional late acyltransferase (LpxL) from E. coli induce robust innate immunity, and such strains are attenuated in both in vivo and in vitro models of plague (20, 40, 41). However, in the context of live bacterial vaccines, especially for human use, it is important to consider the reduction of endotoxicity, and deletion of the msbB gene in several pathogenic bacteria, including Y. pestis, has yielded mutants with less toxic penta-acylated lipid A (9, 14, 17–20, 34, 42, 43).
In our earlier study, we engineered Δlpp mutants of two strains of Y. pestis, namely, the wild-type (WT) strain CO92 and a pigmentation (pgm) locus-negative KIM/D27 mutant of Y. pestis (44). The aforementioned Δlpp mutants were significantly attenuated in both bubonic and pneumonic mouse models of plague, and animals immunized with the KIM/D27 Δlpp mutant strain were protected against secondary intranasal WT CO92 challenge (44). Because of the synergy between Lpp and LPS in inducing proinflammatory cytokine/chemokine production (28), we deleted the msbB gene from the CO92 Δlpp mutant in this study. Our goal was to further reduce the virulence or toxicity associated with this deadly pathogen and to characterize the virulence potential of the generated Y. pestis CO92 Δlpp ΔmsbB double mutant by employing several infection model systems. Our data suggest that deletion of both MsbB and Lpp may serve as a novel strategy for developing live-attenuated plague vaccines in the future and warrants further studies.
MATERIALS AND METHODS
Bacterial strains, plasmids, and cell culture.
The WT Y. pestis CO92 strain was isolated in 1992 from a fatal pneumonic plague case and acquired through the Centers for Disease Control and Prevention (CDC), Atlanta, GA (44). The Δlpp single mutant of the CO92 strain was generated in our previous study (44). The suicide vector pDMS197, which has a conditional R6K origin of replication (ori) and a levansucrase gene (sacB) from Bacillus subtilis (45), was used in the current investigation.
Y. pestis strains were grown in heart infusion broth (HIB) medium (Difco, Voigt Global Distribution Inc., Lawrence, KS) at 26 to 28°C with constant agitation (180 rpm) or on either HIB agar or 5% sheep blood agar (SBA) plates (Teknova, Hollister, CA). Luria-Bertani (LB) medium was used for growing other bacterial cultures (e.g., recombinant E. coli) at 37°C with agitation.
Restriction endonucleases and T4 DNA ligase were obtained from Promega (Madison, WI). Advantage cDNA PCR kits were purchased from Clontech (Palo Alto, CA). All digested plasmid DNA or DNA fragments from agarose gels were purified using QIAquick kits (Qiagen, Inc., Valencia, CA).
The RAW 264.7 murine macrophage cell line was obtained from the American Type Culture Collection (Manassas, VA) and maintained in Dulbecco's modified Eagle medium (DMEM) with 10% fetal bovine serum (FBS) supplemented with penicillin-streptomycin (Invitrogen, Carlsbad, CA). The cells were incubated at 37°C with 5% CO2.
Generation and characterization of msbB mutants of Y. pestis CO92.
Based on the genome sequence of WT CO92 (GenBank accession number NC_003143), the up- and downstream DNA sequences flanking the msbB gene were PCR amplified by using the primer sets Mup5-Mup3 and Mdn5-Mdn3 (Table 1), respectively. A kanamycin resistance (Kmr) gene cassette with flippase (FLP) recombinase recognition target sites at both ends was PCR amplified from plasmid pKD13 by using a specific primer set (Km5-Km3) (Table 1). These DNA fragments were subsequently ligated together through their respective restriction enzyme sites (Table 1) in the order upstream flanking region-Kmr cassette-downstream flanking region and cloned into the pDMS197 suicide vector (45), resulting in the recombinant plasmid pDMS197msbBUDKm. The recombinant plasmid pDMS197msbBUDKm was transformed by electroporation (Genepulser Xcell; Bio-Rad, Hercules, CA) into the WT or the Δlpp mutant of CO92, generating either a single (ΔmsbB) or a double (Δlpp ΔmsbB) mutant, respectively.
Table 1.
Sequences of the primers used in this study
| Primer or primer pair | Primer sequences (5′–3′) (restriction enzymes)a | Purpose |
|---|---|---|
| Mup5-Mup3 | GAGCTCTGCGTAAAGGCGATCAGTTTGCGG (SacI), GGATCCTCATGGGGAAACTCTTAGAATTGG (BamHI) | PCR amplification of upstream flanking fragment for the msbB gene of Y. pestis CO92 |
| Mdn5-Mdn3 | AAGCTTTAGGGTGTGATAACCGTTC (HindIII), TGGATGGTACCGATGCGGTC (KpnI) | PCR amplification of downstream flanking fragment for the msbB gene of Y. pestis CO92 |
| Km5-Km3 | ATTCCGGGGATCCGTCGACC (BamHI), AAGCTTTGTAGGCTGGAGCTGCTT (HindIII) | PCR amplification of the Kmr gene cassette with FLP recombinase recognition target sites from plasmid pKD13 at both ends |
| MsbB5-MsbB3 | GGAGCGATTGCGGCGCTCGC, GCAATATAGGCGTCATCAGC | msbB mutant verification primers located outside the flanking DNA sequences that were used to generated the msbB mutants of Y. pestis |
| Up5-Dn3 | TGACCAAGGCACTACAGTGG, GGTGATGGATGTTGCCAACG | PCR amplification of the coding region of the msbB gene in Y. pestis CO92 |
| SqmsbB | ATTGCGAAGCGGTTATCTGC | Primer located 144 bp upstream of the msbB gene; used to confirm the in-frame deletion of the msbB gene by chromosomal DNA sequencing |
Underlining indicates restriction enzyme sites in the primers.
The transformants were plated onto HIB agar plates containing 5% sucrose and 100 μg/ml kanamycin. The Kmr colonies were PCR screened by using primer sets MsbB5-MsbB3 and Up5-Dn3 (Table 1). The clones showing genomic replacement of the msbB gene with the Kmr gene cassette were retransformed with the pFlp2 plasmid, which expresses the FLP recombinase, to remove the Kmr gene cassette. The plasmid pFlp2 was then cured with 5% sucrose in the growth medium, and the final ΔmsbB mutants were Kms and free of the plasmid pFlp2. The in-frame deletion of the msbB gene from the mutants was further confirmed by genome sequencing with the primer SqmsbB (Table 1).
LCR.
The low calcium response (LCR) is a characteristic trait of the Yersinia type III secretion system (T3SS) in which effectors called Yersinia outer membrane proteins (Yops), such as YopE and YopH, are secreted in response to a low calcium signal. Briefly, Y. pestis cultures (the WT as well as the Δlpp, ΔmsbB, and Δlpp ΔmsbB mutants of CO92) were first grown in HIB medium at 28°C overnight. The next morning, the cultures were diluted 1:20 with fresh HIB medium and continued to grow at 28°C for 3 h, followed by an additional 2 h of incubation at 37°C. During this time, the optical density at 600 nm (OD600) of the cultures reached approximately 0.8 to 1. EGTA (Sigma-Aldrich, St. Louis, MO) was then added to the cultures at a final concentration of 5 mM. Aliquots (1 ml) of the culture were removed 1, 5, and 30 min after the addition of EGTA, followed by the separation of bacterial cells from the supernatants. Subsequently, 500 μl of supernatant was precipitated with 55 μl of 100% trichloroacetic acid (TCA) on ice for 2 h, after which the samples were centrifuged at 12,000 rpm for 10 min at 4°C. The resulting precipitates and the bacterial cell pellets were dissolved in SDS-PAGE sample buffer and analyzed by immunoblotting with antibodies to YopE (Santa Cruz Biotechnology, Santa Cruz, CA) and YopH (Agrisera, Stockholm, Sweden), as we previously described (44).
Release of periplasmic RNase I and production of capsular F1 antigen.
Overnight Y. pestis CO92 WT, Δlpp, ΔmsbB, and Δlpp ΔmsbB cultures were diluted and spotted in triplicate onto HIB agar plates containing 1.5% Torula yeast RNA (Sigma-Aldrich). The release of RNase I was then measured as we previously described (44). For F1 production, the diluted cultures continued to grow at 37°C for an additional 2 h (as mentioned above) and then were analyzed with a commercially available plague detection kit, the Yersinia pestis (F1) Smart II kit (New Horizons Diagnostics, Baltimore, MD), as well as by immunofluorescence (IF) staining and microscopy as we previously described (46).
Phagocytosis and intracellular survival assays.
RAW 264.7 murine macrophages were seeded in six-well plates and incubated until they reached 60 to 70% confluence (approximately 3 × 106 cells/well) (47–49). The WT and CO92 mutant strains grown in HIB medium at 28°C were used to infect macrophages at a multiplicity of infection (MOI) of 1. The plates were centrifuged at 1,500 rpm for 10 min to facilitate adhesion of the bacteria to the host cells and were then incubated at 37°C in 5% CO2 for the duration of the experiment. After 30 min of incubation, the medium was aspirated, and the cells were carefully washed twice with phosphate-buffered saline (PBS). Subsequently, DMEM supplemented with 200 μg/ml gentamicin was added to each well to kill extracellular bacteria. After 1 h, the medium was removed, and the infected RAW cells were carefully washed twice with PBS before DMEM containing 10 μg/ml of gentamicin was added to each well.
The 0-h plates represented host cells that were infected with bacteria for 30 min and then treated with gentamicin for 1 h to determine the number of initially invaded/phagocytosed bacteria. Host cell viability was monitored during the course of the experiment. At 0 and 4 h postinfection (p.i.), the monolayers were carefully washed twice with PBS, and the macrophages were then lysed with 300 μl of sterile water and shaken to ensure complete disruption of the host cells. Suspensions of lysed macrophages were serially diluted 10-fold and cultured on SBA plates for enumerating CFU after incubation at 28°C for 24 to 48 h. The original bacterial suspension was also serially diluted and plated in order to calculate the percentage of invasion/phagocytosis (44).
Measurement of the MICs of gentamicin.
The MICs of gentamicin against WT Y. pestis CO92 and its Δlpp ΔmsbB mutant were determined by using Etest (bioMérieux, Inc., Durham, NC) as we previously described (44). Briefly, overnight Yersinia cultures were diluted (1:4) with fresh HIB medium and continued to grow at 28°C for 2 h (OD600 of ∼0.6). The bacterial cultures were then spread evenly onto 5% SBA plates, and predefined gentamicin (range, 0.016 to 256 μg/ml) Etest strips were placed onto the plates. The plates were incubated for 48 h at 28°C or 37°C, and the MICs were recorded.
Serum resistance assay.
Sera pooled from five naïve mice were used in the assay. A portion of the pooled serum was heated at 56°C for 30 min to inactivate complement. The heat-inactivated serum and PBS served as controls. Briefly, overnight Y. pestis CO92 WT and Δlpp ΔmsbB mutant cultures were harvested and diluted in PBS to obtain an OD600 of 0.2 (∼1 × 108 CFU/ml). Next, 50 μl of the diluted bacteria (∼5 × 106 CFU) was mixed with 200 μl of normal serum, heat-inactivated serum, or PBS. The samples were incubated at 37°C with shaking for 1 h. The number of surviving bacteria (CFU) in each sample was determined by serial dilutions and plating on SBA plates (50).
Animal studies.
All animal experiments were performed using protocols approved by the University of Texas Medical Branch Institutional Animal Care and Use and Institutional Biological Safety Committees in an animal biosafety level 3 (ABSL-3) facility. Five- to 6-week-old female Swiss-Webster mice (17 to 20 g) or inbred Brown Norway rats (50 to 75 g) were purchased from Charles River Laboratories (Wilmington, MA). Mice were challenged intranasally (i.n.) (51, 52) or subcutaneously (s.c.) (52) with 1 × 103 CFU or 30 CFU (representing 3 50% lethal doses [LD50]), respectively, of the WT as well as the same CFU of the Δlpp, ΔmsbB, or Δlpp ΔmsbB mutant of CO92. Rats were challenged by the i.n. or s.c. route with 2 to 3 or 8 LD50, respectively, of WT Y. pestis CO92 or its Δlpp ΔmsbB double mutant (53). One LD50 of WT CO92 corresponds to 340 CFU for mice and 250 CFU for rats in a pneumonic plague model, while in the bubonic plague model, 1 LD50 was determined to be 10 CFU for mice and 50 CFU for rats (44, 53; unpublished data).
Because of the highly virulent nature of WT CO92, we preferred to use a bacterial challenge dose of <10 LD50 for all of the animal studies. Animals were assessed for morbidity and/or mortality over the duration of each experiment. Survivors from the initial infections were rechallenged with 8 to 10 LD50 of WT CO92 25 to 40 days post-initial infection, and age-matched, naïve mice or rats were used as positive controls to ensure animal lethality due to infection.
Bacterial dissemination and cytokine/chemokine production in vivo.
Swiss-Webster mice were inoculated by the i.n. route (3.4 × 103 CFU, representing 10 LD50 of the WT bacterium) or the s.c. (250 CFU, or 25 LD50) route with the WT or the Δlpp, ΔmsbB, or Δlpp ΔmsbB mutant of CO92 (44). At 24, 48, and 72 h post-i.n. challenge and 48, 96, and 144 h post-s.c. infection, 5 mice from each group (at each time point) were euthanized using a mixture of ketamine (90 mg/kg of body weight) and xylazine (10 mg/kg) followed by cervical dislocation. Blood was collected via cardiac puncture, and the lungs, liver, and spleen were removed immediately following animal sacrifice. Organs were mixed with 1 ml of PBS and homogenized with a Kendall disposable tissue grinder (Fisher HealthCare, Houston, TX). Bacterial loads in different organs were determined by serial dilution and plating of the organ homogenates. Cytokine/chemokine levels in sera and spleen homogenates were measured using a multiplex assay with Milliplex (Millipore, Billerica, MA), which detects 32 cytokines/chemokines, as we previously described (44).
T-cell responses.
A total of 30 Swiss-Webster mice were challenged i.n. with 170 CFU of the WT or the Δlpp ΔmsbB double mutant (15 mice in each group). At 14, 21, and 60 days p.i., spleens from 5 mice in each infected group (at each time point) were harvested, and T cells were isolated from each animal separately, using a CD3ε MicroBead kit for MACS (Miltenyi Biotec GmbH, Bergisch Gladbach, Germany). T cells isolated from uninfected mice were used as a control at each time point, and all isolated T cells were then incubated with irradiated antigen-presenting cells (APCs) either pulsed with heat-killed WT CO92 or not. Subsequent cytokine/chemokine production and proliferation of T cells were then assessed.
(i) Preparation of heat-killed bacteria.
Overnight WT CO92 cultures grown in HIB medium at 28°C were diluted 10-fold in HIB medium and then grown for 4 h at 37°C. Bacterial cultures were spun (5,000 rpm for 10 min) and then resuspended in 6 ml of PBS. An aliquot (100 μl) of the suspension was serially diluted and plated to determine titers. The remaining bacterial culture was aliquoted into 1.5-ml volumes and heated at 70°C for 60 min, and the heat-killed nonviable bacteria were stored at −80°C.
(ii) Pulsing and irradiating APCs.
Splenocytes of Swiss-Webster mice were used as APCs. To pulse the APCs, splenocytes were incubated with heat-killed WT bacteria (MOI of 1) in a complete medium (RPMI with glutamine, 1% HEPES, 1 mM sodium pyruvate, 10% FBS, 50 μM β-mercaptoethanol, and 50 μg/ml gentamicin) at 37°C overnight. Splenocytes not pulsed with heat-killed bacteria were designated unpulsed control APCs. After washing, the APCs (pulsed and unpulsed) were irradiated at 3,000 rad (RS-200 biological irradiator; RAD Source, Suwanee, GA).
(iii) T-cell proliferation and cytokine/chemokine production.
T cells isolated from mice infected with the WT or the Δlpp ΔmsbB double mutant or from uninfected animals were cultured at 1 × 105/well with 2 × 105 pulsed or unpulsed APCs/well in complete RPMI medium containing 10% FBS in 96-well plates in a CO2 incubator at 37°C. The unpulsed groups served as negative controls, and T cells cultured with unpulsed APCs but 2 μg/ml of anti-CD3 antibody were used as a positive control. The culture supernatants were collected at 48 h to measure cytokine and chemokine production by using a multiplex assay with Milliplex (Millipore) (44). For T-cell proliferation, 1 μCi of [3H]thymidine was added to each well after 72 h of incubation, and the cells were harvested 16 h later by use of a semiautomated sample harvester (FilterMate harvester; PerkinElmer, Waltham, MA), followed by the measurement of radioactive counts (TopCount NXT; PerkinElmer).
Statistical analyses.
Whenever appropriate, analysis of variance with the Bonferroni correction or the Holm-Sidak/Shapiro-Wilk method with one-way analysis of variance (ANOVA) was employed for data analysis. We used the Kaplan-Meier survival estimate for animal studies, and P values of ≤0.05 were considered significant.
RESULTS
Characterization of Y. pestis CO92 ΔmsbB mutants.
After the authenticity of in-frame-deleted ΔmsbB single and Δlpp ΔmsbB double mutants was confirmed by chromosomal DNA sequencing, we observed no growth defects in the mutants. Since LPS and Lpp are important in maintaining integrity of the bacterial cell envelope (6, 7), we evaluated the membrane integrity of the generated mutants by measuring the release of periplasmic RNase I, which represents the most sensitive method of detecting alterations in bacterial membranes. We noted no difference in the level of periplasmic RNase I released among the mutants and the WT bacterium (data not shown).
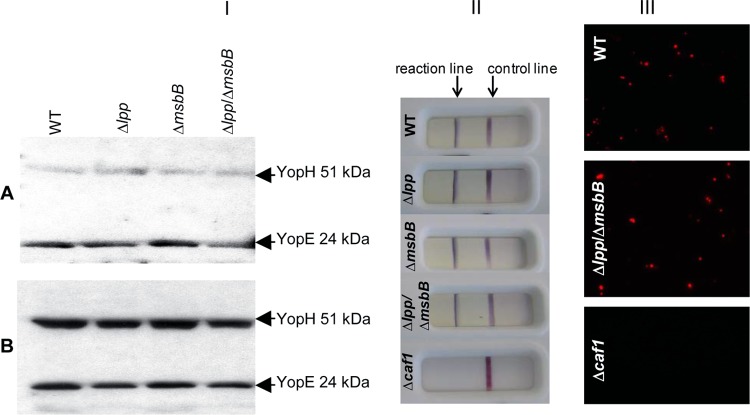
To determine whether deletion of the lpp or msbB gene affected the function of the T3SS, we measured T3SS-dependent protein secretion in the mutants in response to low calcium signals that mimic their contact with eukaryotic host cells in an in vitro assay. One minute following the addition of EGTA, a calcium chelator, secretion of the T3SS effectors YopE and YopH could be detected in the supernatants from all Y. pestis CO92 cultures tested (Fig. 1IA). Compared to the WT bacterium, there was no significant difference in either the levels of secretion of YopE and YopH among different mutants (Fig. 1IA) or the expression and production levels of YopE and YopH in bacterial cells (Fig. 1IB). Similar results were obtained 5 and 30 min following the addition of EGTA (data not shown).
Fig 1.
T3SS function and production of F1 antigen by CO92 msbB mutants. Various overnight Y. pestis cultures were diluted 1:20 with fresh HIB medium and continued to grow at 28°C for 3 h, followed by an additional 2 h of incubation at 37°C, until the OD600 of the cultures reached approximately 0.8 to 1. EGTA was then added to the cultures at a final concentration of 5 mM. The expression and secretion of YopE and YopH in bacterial supernatants (A) and cell extracts (B) were analyzed by immunoblotting with antibodies to YopE and YopH (I). F1 production was examined by using immunochromatographic reaction dipsticks (II), and IF staining was observed with anti-F1 antibodies (III), using a Nikon Ti microscope (Melville, NY). Magnification, ×400.
The capsular antigen (F1) of Y. pestis has antiphagocytic properties and is also a major immunoreactive antigen (39, 46). Therefore, we examined the production of F1 antigen in all strains by using a commercial dipstick kit as well as by IF staining. As shown in Fig. 1II, similar-intensity reaction lines were developed for all tested CO92 strains, except for the Δcaf1 mutant of CO92 (our negative control), as expected. These observations were further supported by IF staining, as the presence of the capsular antigen was detected on the surfaces of the WT and Δlpp ΔmsbB mutant strains by microscopy, while the Δcaf1 mutant was devoid of the capsule and lacked fluorescence (Fig. 1III).
Survivability of Y. pestis CO92 ΔmsbB mutants in murine macrophages.
To determine whether any of our mutants were more susceptible to macrophage killing, we infected RAW 264.7 cells with the WT, Δlpp, ΔmsbB, and Δlpp ΔmsbB CO92 strains at an MOI of 1. Nearly 100% phagocytosis was observed for all strains at the aforementioned MOI (data not shown). To evaluate intracellular survival of bacteria, a gentamicin protection assay was employed. Interestingly, 64% of the WT bacteria survived within macrophages at 4 h p.i., in contrast to only 26% for the Δlpp mutant, 48% for the ΔmsbB mutant, and 23% for the Δlpp ΔmsbB mutant (Fig. 2).
Fig 2.
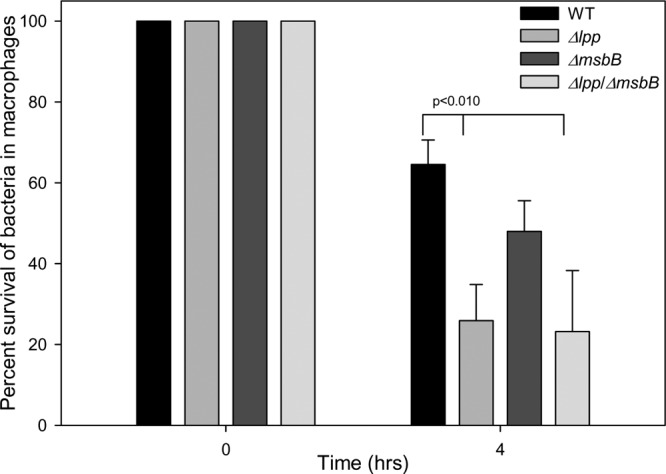
Intracellular survival of various Y. pestis CO92 strains in murine macrophages. RAW 264.7 murine macrophages were infected with overnight WT, Δlpp, ΔmsbB, or Δlpp ΔmsbB CO92 cultures at an MOI of 1. Following gentamicin treatment, cells were harvested at 4 h postinfection, and the number of bacteria surviving intracellularly was assessed by serial dilution and plating. Data were analyzed by using one-way ANOVA with the Holm-Sidak method, and statistically significant differences are indicated by lines with P values. The error bars indicate standard deviations.
Importantly, both the WT and its Δlpp ΔmsbB mutant exhibited similar sensitivities to gentamicin; the MICs for both the WT and the Δlpp ΔmsbB mutant were 0.5 μg/ml at 37°C and 0.75 μg/ml at 28°C. These data indicated that intracellular survivability was indeed impaired in all of the Y. pestis mutant strains. More importantly, the Δlpp and Δlpp ΔmsbB mutant survival rates of 23 to 26% were significantly lower than the 48% survivability noted for the ΔmsbB mutant. These data suggested that Lpp rather than MsbB contributed more significantly to the intracellular survival of Y. pestis during a macrophage assault. We obtained a similar survivability of mutants at the 4-h time point when macrophages derived from the human promyelocytic leukemia cell line HL-60 were used instead of RAW 264.7 cells for infection studies (data not shown).
Evaluation of Y. pestis CO92 ΔmsbB mutants in both pneumonic and bubonic plague mouse models.
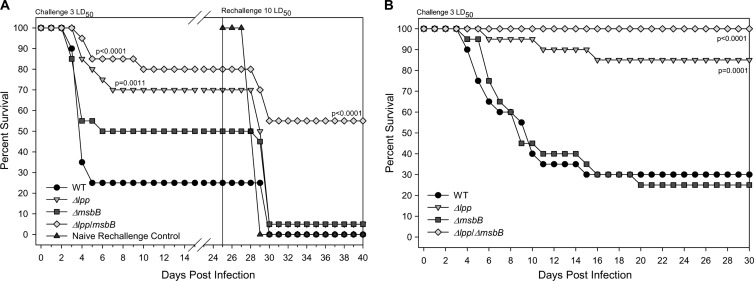
To assess the virulence potential of the ΔmsbB mutant strains, mice were first infected i.n. with the same dose (1.0 × 103 CFU, representing 3 LD50 of the WT bacterium) of the parental CO92 strain or the Δlpp, ΔmsbB, or Δlpp ΔmsbB mutant. As shown in Fig. 3A, mice from all groups started to die between days 4 and 5 p.i.; however, over time, an increased survival rate was observed for animals infected with either of the single mutants (i.e., the Δlpp or ΔmsbB strain) or the Δlpp ΔmsbB double mutant compared to that of the WT bacterium-infected mice. Furthermore, the Δlpp ΔmsbB double mutant-infected mice were 10 to 30% more protected than animals infected with the Δlpp or ΔmsbB single mutant (Fig. 3A). The increased survival rate between the ΔmsbB single mutant and the Δlpp ΔmsbB double mutant was statistically significant; however, the difference in the survival rates of the Δlpp mutant and the Δlpp ΔmsbB double mutant was not significant (Fig. 3A).
Fig 3.
Virulence potential of and subsequent protection conferred by CO92 Δlpp ΔmsbB mutant in pneumonic and bubonic plague mouse models of infection. Female Swiss-Webster mice (n = 20/group) were infected via the i.n. route (A) or the s.c. route (B) with 3 LD50 of the WT or 3 LD50 WT equivalent CFU of the Δlpp, ΔmsbB, or Δlpp ΔmsbB strain. Mouse mortality was recorded, and survivors of the initial i.n. infection were intranasally rechallenged with 10 LD50 of WT Y. pestis CO92; age-matched naïve mice (dark solid triangles) were administered 10 LD50 of the WT strain only and were used as a control (A). The Kaplan-Meier survival estimate was used to analyze the survival of mice between different groups. The P values represent statistically significant differences compared to the WT group only.
To evaluate specific immunity induced in mice after the initial infection, we rechallenged survivors of all groups with 10 LD50 (3,400 CFU) of WT CO92 via the i.n. route 25 days following the initial infection. As shown in Fig. 3A, 55% of the animals were still protected from developing pneumonic plague after they were initially infected with the Δlpp ΔmsbB double mutant. In contrast, no to minimal protection was observed in those groups of mice that were initially infected with the single mutants or the WT bacterium, as 95 to 100% of them succumbed to infection. Likewise, all of the animals in the age-matched control group died (Fig. 3A).
In a parallel study with a bubonic plague mouse model, animals were infected by the s.c. route with WT CO92 or the above-mentioned mutant strains at a dose of 30 CFU (representing 3 LD50 of the WT bacterium). As shown in Fig. 3B, the survival rates were 30%, 25%, 85%, and 100% for mice infected with the WT and the ΔmsbB, Δlpp, and Δlpp ΔmsbB mutants, respectively. Importantly, the difference in survival rate between the ΔmsbB single mutant and the Δlpp ΔmsbB double mutant was statistically significant. Likewise, mice infected with the Δlpp ΔmsbB double mutant exhibited increased survivability compared to animals that were challenged with the Δlpp single mutant, although the latter mutant alone was highly attenuated in evoking bubonic plague in mice (Fig. 3B).
Evaluation of Y. pestis CO92 ΔmsbB mutants in rat models of pneumonic and bubonic plague.
The attenuation of the Δlpp, ΔmsbB, and Δlpp ΔmsbB mutants and superior protection of those mice initially infected with the Δlpp ΔmsbB double mutant against the WT CO92 rechallenge prompted us to employ another rodent model. We chose rats because they better emulate human plague than the mouse model, and rats are the natural hosts for Y. pestis.
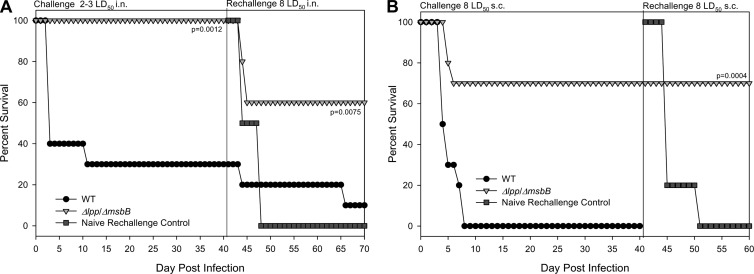
In these studies, we focused mainly on the Δlpp ΔmsbB double mutant, as it was by far the most attenuated strain in mouse models of bubonic and pneumonic plague. Consequently, rats were infected via the i.n. route with the WT or the Δlpp ΔmsbB mutant of Y. pestis CO92 at doses of 500 to 750 CFU (representing 2 to 3 LD50 of the WT bacterium). As shown in Fig. 4A, 100% of the rats in the Δlpp ΔmsbB double mutant-infected group survived, while in the WT bacterium-infected group, only 30% of the rats survived. Similar results were observed in the bubonic plague rat model, in which 70% of the animals in the Δlpp ΔmsbB double mutant-infected group survived a dose of 400 CFU (representing 8 LD50 of the WT bacterium), and all of the rats in the WT bacterium-infected group died (Fig. 4B).
Fig 4.
Virulence potential of and subsequent protection conferred by CO92 Δlpp ΔmsbB mutant in pneumonic and bubonic plague rat models of infection. Female Brown Norway rats (n = 10/group) were infected via the i.n. route (2 to 3 LD50 [500 to 750 CFU]) (A) or the s.c. route (8 LD50 [400 CFU]) (B) with the WT and Δlpp ΔmsbB CO92 strains. Rat mortality was recorded, and survivors of the initial infections were rechallenged with 8 LD50 of WT Y. pestis CO92 (via the routes corresponding to their initial infection routes); age-matched naïve rats were used as a control. The Kaplan-Meier survival estimate was used to analyze rat survival, and P values represent statistically significant differences compared to the WT group.
The survivors from the initial infection study were then rechallenged with 8 LD50 of WT CO92 on day 40 p.i. The rechallenged routes of infection corresponded with the initial routes, and age-matched animals were used as controls. As shown in Fig. 4A, 60% of rats initially infected i.n. with the Δlpp ΔmsbB double mutant were protected from developing pneumonic plague. In contrast, among rats that were initially protected from WT CO92 challenge, only 10% survived the second i.n. challenge dose of WT bacteria. All rats in the age-matched control group died when infected with WT CO92 at the time of rechallenge. Importantly, 100% of the rats that were initially inoculated by the s.c. route with the Δlpp ΔmsbB double mutant were protected from developing bubonic plague, while all age-matched control rats died when infected with WT CO92 at the time of rechallenge (Fig. 4B).
Bacterial dissemination and cytokine/chemokine production by various mutants in a mouse model of pneumonic plague.
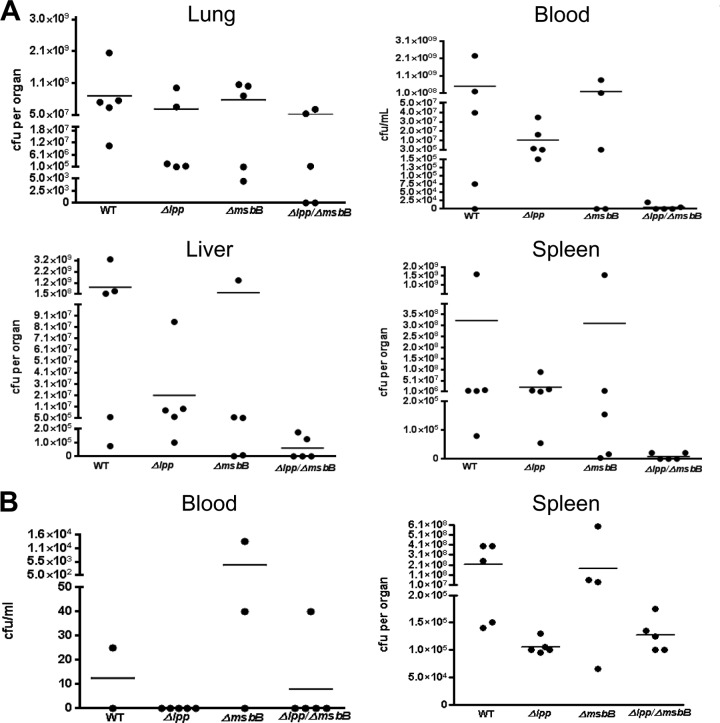
To further investigate the virulence potential of the CO92 ΔmsbB mutants, we monitored their ability to disseminate from the infection site (lungs during i.n. challenge) to the bloodstream and distal organs (e.g., spleen and liver). The cytokine/chemokine levels induced by infection were also evaluated for mouse sera and spleen homogenates. Fifteen mice in each group were challenged i.n. with 3.4 × 103 CFU of the WT, Δlpp, ΔmsbB, or Δlpp ΔmsbB CO92 strain.
Similar bacterial loads were observed in the lungs of all infected groups during the early stages of infection; the average bacterial counts were 2.7 × 105 and 4.8 × 107 CFU/organ at 24 and 48 h p.i., respectively. These average counts were approximately 2 to 4 log higher than the initial challenge dose given to the animals (10 LD50, or ∼3.4 × 103 CFU), indicating that infection was established in the lungs and progressed rapidly during the initial 24 to 48 h. At 72 h p.i. (Fig. 5A), lung bacterial loads further increased in the WT CO92-infected animals, reaching an average of 6.5 × 108 CFU/organ. Impressively, the Δlpp ΔmsbB double mutant was cleared from the lungs of some mice (2 of 5 mice) by 72 h p.i. (Fig. 5A).
Fig 5.
Dissemination of various CO92 strains in mice. Female Swiss-Webster mice (n = 15/group) were challenged either i.n. with 3.4 × 103 CFU (10 LD50) or s.c. with 250 CFU (25 LD50), using the WT, Δlpp, ΔmsbB, or Δlpp ΔmsbB CO92 strain. At different time points p.i., 5 mice from each group (at each time point) were euthanized. Tissues from mice (i.e., blood, lung, spleen, and liver) were collected immediately following sacrifice and assessed for bacterial loads. The data shown are the bacterial loads at 72 h p.i. for i.n. challenged groups (A) and 144 h p.i. for s.c. infected groups (B).
In the blood, no WT CO92 or any of the mutants tested were detected at 24 h p.i., and the blood remained negative for bacilli in the Δlpp and Δlpp ΔmsbB mutant-infected groups of mice on day 2 p.i. In contrast, bacilli were present in the bloodstream of most animals infected with WT CO92 (4 of 5 mice) and in some animals infected with the ΔmsbB single mutant (2 of 5 mice) on day 2 p.i., with average bacterial loads of 2.9 × 104 CFU/ml and 1,000 CFU/ml, respectively. By day 3 p.i., average bacterial loads in the blood were 5.0 × 108 CFU/ml for the WT-infected group of animals, 1.9 × 108 CFU/ml for the ΔmsbB group, and 1.1 × 107 CFU/ml for the Δlpp group of infected animals (Fig. 5A). In the Δlpp ΔmsbB double mutant-infected group of mice, 2/5 animals had relatively small numbers of bacteria in the blood, and the remaining 3 had undetectable levels of bacteria, which led to an average bacterial count of <500 CFU/ml.
In the liver on day 1 p.i., a relatively large number of bacilli were detected in WT CO92-infected animals (5.6 × 103 CFU/organ) and Δlpp mutant-infected groups of mice (8.0 × 103 CFU/organ). Comparatively, animals infected with the ΔmsbB (1.9 × 103 CFU/organ) and Δlpp ΔmsbB (7.0 × 102 CFU/organ) mutants had smaller bacterial numbers than mice infected with the above-mentioned strains. On day 2 p.i., the number of bacilli increased rapidly in the group of mice infected with WT CO92, with an average bacterial load of 1.5 × 105 CFU/organ. These numbers were 4.0 × 103 CFU/organ, 1.3 × 104 CFU/organ, and 6.7 × 103 CFU/organ for the groups of mice infected with the Δlpp, ΔmsbB, and Δlpp ΔmsbB mutants, respectively. Thus, livers of animals infected with the WT had 10- to 100-fold greater bacterial loads than those derived from mice infected with the other mutants tested. Interestingly, 2 and 4 animals out of 5 remained bacillus free in the liver tissues when infected with the ΔmsbB and Δlpp ΔmsbB mutants, respectively.
By day 3 p.i., the average bacterial counts in all groups of mice reached 2.1 × 107 to 7.7 × 108/organ, except in those animals infected with the Δlpp ΔmsbB double mutant, in which the load was 6.0 × 104 CFU/organ and 3 of 5 mice were negative for the bacilli in the liver (Fig. 5A).
In the spleen, average bacterial counts of 3.6 × 103 to 3.7 × 103 CFU/organ were detected in WT- and Δlpp mutant-infected animals on day 1 p.i. Animals infected with the ΔmsbB or Δlpp ΔmsbB mutant had lower bacterial counts, in the range of 0 to 350 CFU/organ, except for one mouse in the ΔmsbB group which had a load of 9.0 × 105 CFU/organ. On day 2 p.i., the average bacterial loads were 9.1 × 104 CFU/organ, 640 CFU/organ, 8.2 × 103 CFU/organ, and 240 CFU/organ for the WT, Δlpp, ΔmsbB, and Δlpp ΔmsbB strain-infected groups of mice, respectively. By day 3 p.i. (Fig. 5A), similar average loads of 3.1 × 108 to 3.2 × 108 CFU/organ were noted in the WT- and ΔmsbB mutant-infected animals, while relatively lower counts were observed in the Δlpp and Δlpp/ΔmsbB mutant-infected mice (2.1 × 107 CFU/organ and 8.6 × 103 CFU/organ, respectively). Importantly, 3/5 spleens were negative for the Δlpp ΔmsbB mutant, and the remaining 2 animals had very low counts.
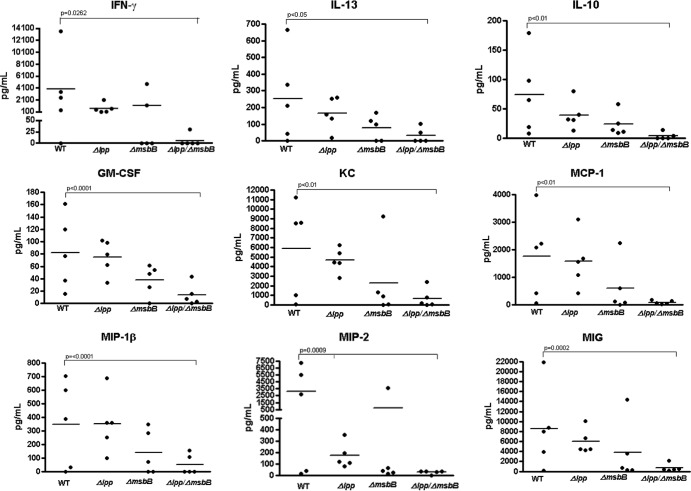
Cytokine/chemokine production was measured at 24, 48, and 72 h p.i. in the sera and at 72 h p.i. in the splenic homogenates of mice. In the sera of infected animals, similar levels of cytokines/chemokines were detected in all groups at 24 and 48 h p.i. However, at 72 h p.i., the overall levels of cytokines/chemokines in all of the mutant-infected groups were lower than those in animals infected with the WT strain. Mice infected with the Δlpp ΔmsbB double mutant generally elicited the least robust cytokine/chemokine responses, followed by the ΔmsbB mutant- and then the Δlpp mutant-infected group of animals. At 72 h p.i., significantly lower production levels of IFN-γ, granulocyte-macrophage colony-stimulating factor (GM-CSF), macrophage inflammatory protein 1β (MIP-1β), IL-13, KC, MIP-2, IL-10, macrophage chemoattractant protein 1 (MCP-1), and MIG were seen in mice infected with the Δlpp ΔmsbB double mutant than in animals challenged with WT CO92 (Fig. 6). Although these cytokines/chemokines were also lower in the sera of animals infected with the single mutants (i.e., the Δlpp or ΔmsbB mutant), the data were not statistically significant, except for MIP-2, which was significantly decreased in the Δlpp mutant-infected mice (Fig. 6). A detailed cytokine/chemokine profiling is provided in Table S1 in the supplemental material. The cytokine/chemokine production in the spleens of infected mice followed the same trend as that for the sera at 72 h p.i.: smaller amounts of cytokine/chemokine production were noticed in mutant-infected groups of mice (see Table S1). Compared to those in the WT-infected mice, significantly lower levels of GM-CSF, IL-3, IL-5, IL-12(p70), IL-13, IL-15, and MIG were observed in the Δlpp ΔmsbB mutant-infected mice, while the TNF-α, GM-CSF, IL-12(p70), IL-13, and IL-15 levels were significantly lower in animals infected with the ΔmsbB mutant (see Table S1).
Fig 6.
Cytokine/chemokine analysis of sera from mice 72 h after pneumonic plague infection. Female Swiss-Webster mice (n = 15/group) were challenged i.n. with 3.4 × 103 CFU (10 LD50) of the WT, Δlpp, ΔmsbB, or Δlpp ΔmsbB strain. At 24, 48, and 72 h p.i., 5 mice from each group (at each time point) were euthanized. Blood was collected via cardiac puncture, and production of various cytokines/chemokines was measured by using a multiplex assay with Milliplex. The entire cytokine/chemokine profile is presented in Table S1 in the supplemental material, and only the cytokines/chemokines showing statistically significant differences compared to WT-infected mice are shown here. Significant differences are indicated by lines, and P values shown are based on one-way ANOVA with the Bonferroni correction.
Bacterial dissemination and cytokine/chemokine production in a mouse model of bubonic plague.
To evaluate a model of bubonic plague, 15 mice were challenged with 250 CFU (25 LD50 of the WT bacterium) of the parental, Δlpp, ΔmsbB, or Δlpp ΔmsbB Y. pestis CO92 strain via the s.c. route. At 48, 96, and 144 h p.i., 5 mice from each group (at each time point) were scarified for assessing bacterial loads and the production of cytokines/chemokines in the blood and spleen.
In the blood at 48 and 96 h p.i., only 1 or 2 of 5 mice infected with WT CO92 were positive for the bacterium, while the blood from mice infected with any of the mutants did not show any detectable organisms. By 144 h p.i. (Fig. 5B), 1 animal in the group infected with WT CO92 had died, and another two mice were terminal, and hence blood could not be drawn. The remaining two mice in the WT-infected group had bacterial counts of 0 and 25 CFU/ml, respectively. In the ΔmsbB mutant-infected group of mice, only 3 survivors were assessed for bacterial loads in the bloodstream, and they had counts of 0, 40, and 1.3 × 104/ml. In the Δlpp and Δlpp ΔmsbB mutant-infected groups of mice, all animals were alive, with no detectable Y. pestis, except for one animal with a bacterial count of 40 CFU/ml.
In the spleen at 48 h p.i., all bacterial loads were in the range of 3.0 × 104 to 7.5 × 104 CFU/organ, except for in one animal infected with WT CO92, which had a relatively higher bacterial count of 1.53 × 106 CFU/organ. Interestingly, this pattern continued at 96 h p.i., as mice from all groups had similar bacterial counts, in the range of 1.5 × 105 to 6.0 × 105 CFU/organ, except for one ΔmsbB mutant-infected animal (1.45 × 107 CFU/organ). At 144 h p.i. (Fig. 5B), averages of 1.6 × 108 to 2.1 × 108 CFU/organ were seen in mice infected with the WT or the ΔmsbB mutant, while the averages were lower (in the range of 1.3 × 105 to 1.6 × 105 CFU/organ) for the Δlpp and Δlpp ΔmsbB mutant-infected mice. However, the differences were not significant.
The cytokine/chemokine production in mice with bubonic plague was also evaluated, and detailed information can be found in Table S2 in the supplemental material. Overall, the levels of cytokines/chemokines produced in the sera of mice infected with the various mutants were either comparable or slightly lower than those of animals infected with WT CO92 at all tested time points (48, 96, and 144 h p.i.). However, the production of IP-10 was significantly lower in the Δlpp ΔmsbB mutant-infected mice at 48 h p.i., while the MIP-1α level was significantly decreased in mice infected with either the Δlpp or Δlpp ΔmsbB mutant at 144 h p.i. (see Table S2).
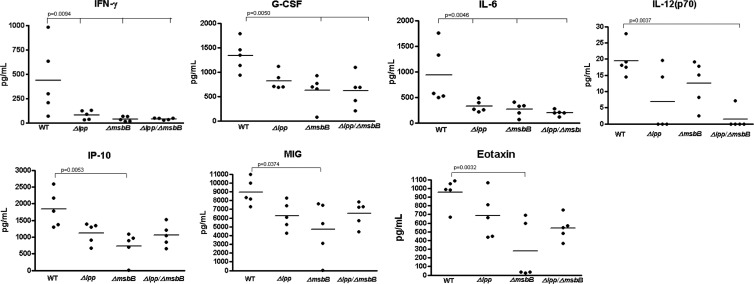
Splenic cytokine/chemokine production was measured at 96 h p.i. Similar to the data derived from infected sera, all mutants generally elicited lower or comparable levels of cytokines/chemokines compared to animals infected with WT CO92. Specifically, the levels of IL-6 and IFN-γ were significantly lower in all of the mutant groups of animals than in WT CO92-infected mice (Fig. 7). Likewise, significantly lower levels of G-CSF were observed in both ΔmsbB and Δlpp ΔmsbB mutant-infected mice, while the level of IL-12(p70) was significantly decreased in the Δlpp ΔmsbB mutant-infected animals. In contrast, the levels of IP-10, eotaxin, and MIG were significantly decreased only in the ΔmsbB mutant-infected mice (Fig. 7).
Fig 7.
Cytokine/chemokine analysis of spleens from mice 96 h after bubonic plague infection. Female Swiss-Webster mice (n = 15/group) were challenged s.c. with 250 CFU (25 LD50) of the WT, Δlpp, ΔmsbB, or Δlpp ΔmsbB strain. At 48, 96, and 144 h p.i., 5 mice from each group (at each time point) were euthanized. Spleens were removed and homogenized, and cytokine/chemokine production was measured by using a multiplex assay with Milliplex. The entire cytokine/chemokine profile is presented in Table S2 in the supplemental material, and only the cytokines/chemokines showing statistically significant differences compared to WT-infected mice are shown here. Significant differences are indicated by lines, and P values shown are based on one-way ANOVA with the Bonferroni correction.
Serum resistance.
The highly attenuated phenotype of the Δlpp ΔmsbB mutant and its inability to disseminate to various mouse organs prompted us to evaluate the mutant's resistance to serum killing. Our data showed that both the WT and its Δlpp ΔmsbB mutant had a 100% survival rate after 1 h of incubation in either untreated or heat-inactivated sera and/or PBS at 37°C, indicating that the deletion of the lpp and msbB genes did not affect bacterial resistance to serum, a phenomenon which was reported previously (50).
Activation of T cells by the Δlpp ΔmsbB CO92 mutant in a mouse model of pneumonic plague.
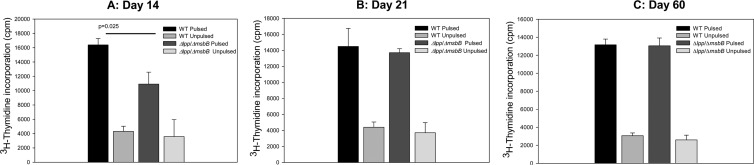
To investigate T-cell responses in mice infected with the Δlpp ΔmsbB double mutant, T cells were isolated from animals infected with a sublethal dose of either WT CO92 or the Δlpp ΔmsbB mutant and restimulated with heat-killed WT Y. pestis CO92. As shown in Fig. 8, T cells from both WT- and mutant-infected mice proliferated strongly, at comparable levels, to stimulation of Y. pestis CO92 antigens, as detected from 14 days p.i. to 60 days p.i. This indicated that both WT and mutant bacteria induced a long-lasting T-cell response to Y. pestis.
Fig 8.
T-cell proliferation. Fifteen Swiss-Webster mice were challenged i.n. with 170 CFU (0.5 LD50) of either the WT or Δlpp msbB CO92 strain (30 mice total). At 14 (A), 21 (B), and 60 (C) days p.i., spleens from 5 mice in each infected group (at each time point) were harvested. T cells were isolated from each animal separately and incubated with γ-irradiated APCs either stimulated (pulsed) with heat-killed WT Y. pestis CO92 or without stimulation (unpulsed). T-cell proliferation was measured by [3H]thymidine incorporation. Data were analyzed by one-way ANOVA with the Holm-Sidak method, and statistically significant differences are indicated by lines with P values. The error bars indicate standard deviations.
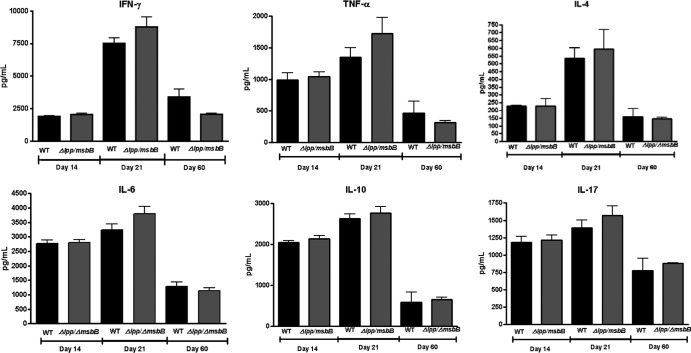
Robust cytokine/chemokine production was observed in T cells from both the WT- and Δlpp ΔmsbB mutant-infected mice in response to stimulation with Y. pestis CO92. A detailed cytokine profiling of T cells is provided in Table S3 in the supplemental material. A slightly increased cytokine/chemokine production was observed in T cells isolated from Δlpp/ΔmsbB mutant-infected mice relative to those of WT-infected animals, although the increases were not statistically significant. This trend was most apparent for IFN-γ, TNF-α, IL-4, IL-6, and IL-17, which are produced by Th1, Th2, or Th17 cells (Fig. 9). In contrast, levels of the anti-inflammatory cytokine IL-10 were similar for T cells isolated from both WT- and Δlpp ΔmsbB mutant-infected mice (Fig. 9). Interestingly, the levels of cytokines/chemokines reached their highest on day 21 p.i., corresponding to the time point when the animals were rechallenged for observation of protection (Fig. 3).
Fig 9.
Cytokine/chemokine production by T cells. Fifteen Swiss-Webster mice were challenged i.n. with 170 CFU (0.5 LD50) of either the WT or Δlpp msbB CO92 strain (30 mice total). At 14, 21, and 60 days p.i., spleens from 5 mice in each infected group (at each time point) were harvested. T cells were isolated from each animal separately and incubated with γ-irradiated APCs either stimulated (pulsed) with heat-killed WT Y. pestis CO92 or without stimulation (unpulsed). T-cell-secreted cytokines/chemokines were then measured by using a multiplex assay with Milliplex. Data were analyzed by one-way ANOVA using the Bonferroni correction, and statistically significant differences are indicated by lines with P values. The error bars indicate standard deviations.
DISCUSSION
Immunogenicity and safety are the two most important aspects in the development of effective vaccines. The endotoxic nature of LPS has always been a concern in the preparation of vaccines against Gram-negative bacterial pathogens. Since a clear correlation between underacylated lipid A and a reduced endotoxic potential of LPS has been demonstrated in numerous studies (54), detoxifying LPS by deleting the late acyltransferase genes, such as msbB, from the genome to create mutant stains with less toxic LPS has become a strategy to generate novel vaccine candidates (47, 54–56).
Since the first report on the ΔmsbB mutant of E. coli (13), this gene has been deleted from several pathogenic bacteria, including S. enterica serovar Typhimurium, Neisseria meningitidis, Shigella flexneri, and Y. pestis (9, 14, 39, 47, 54, 56–58). Compared to the most toxic, hexa-acylated lipid A synthesized in WT bacteria, deletion of the msbB gene generally resulted in the production of a less toxic, penta-acylated lipid A in the mutant strains. Almost all ΔmsbB mutants have been shown to be attenuated in both in vitro and in vivo models of infection (14, 47, 54, 56, 57).
In our previous study, we deleted the lpp gene from various Y. pestis strains, which resulted in attenuated phenotypes (44). Since Lpp synergizes with LPS to induce production of proinflammatory cytokines in vitro and in vivo by activating different TLRs (28), it was logical to speculate that deletion of the msbB gene from the lpp-negative background of a Y. pestis CO92 mutant would further reduce its toxicity. Consequently, we deleted the msbB gene from both the WT and the Δlpp mutant of CO92. As expected, both the ΔmsbB and Δlpp ΔmsbB mutants were attenuated in mouse and rat models of both bubonic and pneumonic plague. Furthermore, both mutants suffered impaired abilities to disseminate and to evoke cytokine/chemokine production.
The attenuation of virulence noted with our msbB mutants in both rodent models was thought to be due mainly to the production of the less toxic penta-acylated lipid A moiety of LPS, which is considered a common mechanism of reduced virulence for several other pathogenic bacteria (11, 14, 16, 39, 54, 56, 57). However, indistinguishable levels of cytokines/chemokines produced in the host during infection with both the WT bacteria and our msbB mutants at early stages of infection (i.e., 24 and 48 h p.i.) did not support this view for Y. pestis, although a possible explanation could be the promiscuous nature of murine TLR-4, which fails to effectively discriminate between penta-acylated and hexa-acylated LPS (54, 59), especially at high LD50s (54, 60).
However, unlike the case in other pathogenic bacteria, the acylation of lipid A in yersiniae is temperature regulated, and the ΔmsbB mutants and WT bacteria are likely to produce the same predominant tetra-acylated lipid A of LPS under in vivo conditions (37°C). Therefore, detoxified LPS is not likely the major contributor to the attenuation of Y. pestis ΔmsbB mutants. On the other hand, our ΔmsbB mutants were impaired in the ability to survive within macrophages, and this correlated with the mutants' crippled dissemination in vivo and decreased levels of cytokine/chemokine production at 72 h p.i. Therefore, an inability to survive intracellularly is likely the underlying mechanism of attenuation for Y. pestis msbB mutants.
The molecular basis for the inability of the ΔmsbB mutants to survive within macrophages remains unknown; however, it is not due to impaired T3SS function (Fig. 1). In our previous study, we also demonstrated that the Δlpp mutant of Y. pestis was defective in surviving in macrophages, and the defect was related to decreased expression of the gene encoding the global stress protein GsrA (61). Perhaps decreased production of GsrA, or a related stress response protein, is responsible for poor intracellular survival of the ΔmsbB mutants as well. Although both the ΔmsbB and Δlpp ΔmsbB mutants showed significant differences in terms of attenuation and survivability in macrophages compared to the WT bacteria, such differences were not significant between the ΔmsbB mutants and the Δlpp mutant (Fig. 2), suggesting that they may use similar mechanisms leading to attenuation.
Studies have shown that both innate and adaptive immunity play important roles during Y. pestis infections (62). The interaction of LPS with TLR-4 represents a “double-edged sword,” as overstimulation of TLR-4 results in uncontrolled production of proinflammatory cytokines, while detoxified LPS will limit TLRs' ability to stimulate innate immune responses that can subsequently affect the adaptive immunity. In our study, decreased cytokine/chemokine production was clearly noted in mice infected with the Δlpp ΔmsbB mutant (Fig. 6 and 7). Importantly, surviving mice and rats of a double mutant infection were better protected during secondary challenge with the WT bacterium (Fig. 3 and 4).
Although lower cytokine/chemokine production was observed in the Δlpp ΔmsbB double mutant-infected mice (Fig. 6 and 7), it still induced strong T-cell responses at WT-like induced levels. For example, the T-cell proliferative responses were similar to those in the WT-infected mice (Fig. 8), and even slightly higher levels of cytokine/chemokine production were observed in T cells isolated from animals infected with the Δlpp ΔmsbB double mutant, especially at 21 days p.i. (Fig. 9). Such T-cell responses were long-lasting, as they could be detected even at 60 days p.i. Thus, the decreased cytokine/chemokine production in the early stages of infection did not affect the nature or magnitude of acquired immunity, which is consistent with a previous study with ΔmsbB mutants of S. flexneri (54).
Recently, an ΔlpxM (msbB) mutant generated in the Y. pestis strain EV line NIIEG was reported to have significantly reduced virulence and better immunogenicity in mouse and guinea pig models of bubonic plague (14, 39, 57). Further study of the Y. pestis EV ΔlpxM mutant revealed pleiotropic effects of lpxM resulting in altered synthesis of major immunoreactive antigens, such as F1 antigen, low-calcium-response V antigen (LcrV), Pla (plasminogen-activating protease), Ymt (murine toxin), and surface-specific polysaccharides (SSP) (39). In addition, Y. pestis EV ΔlpxM showed a lower growth rate in vitro but replicated and remained at the site of inoculation significantly longer than the parental EV NIIEG strain (39). Therefore, the better immunogenicity of Y. pestis EV ΔlpxM was most likely due to these pleiotropic effects, including the dampening of the host innate immune response as well as enhanced bacterial persistence, leading to the activation of adaptive immunity (39, 63).
However, our data presented here did not support this argument. First, the ΔmsbB mutants were cleared more rapidly than the WT bacteria both from the sites of infection and systemically during the initial 1 to 3 days p.i. in both bubonic and pneumonic mouse models of infection. Second, the ΔmsbB mutants were not defective in their growth rates and had intact T3SS function and F1 capsular antigen levels (Fig. 1). Most importantly, the mutant strains had a similar level of periplasmic RNase I release to that of the parental strain, indicating that the membrane integrity of the mutants was likely unaffected. Finally, the WT and the ΔmsbB mutants produced similar levels of IL-10 during the first 24 to 48 h p.i. (see Tables S1 and S2 in the supplemental material), which indicated an early anti-inflammatory response that is normally observed due to T3SS effectors.
This discrepancy among different Y. pestis ΔmsbB mutants could have resulted from different parental strains used for deletion of the msbB gene (i.e., highly virulent Y. pestis CO92 versus the vaccine strain EV76, with a pigmentation [pgm] locus deletion), different ways to prepare the ΔmsbB mutants (i.e., in-frame deletion versus truncation mutagenesis), or possibly the fact that late acyltransferases (such as MsbB) could be strain-specific virulence factors in Y. pestis, similar to the case in Shigella, Neisseria, and Salmonella species (54). Another possible explanation could be related to the fact that ΔmsbB mutants (specifically in Salmonella) are reported to have higher rates of spontaneous suppressor mutations (54, 64). Extragenic suppressors picked up during strain construction could suppress other phenotypes without affecting the pattern of lipid A acylation (54, 64).
Regardless of these differences, it is clear that a greater vaccine potential for the ΔmsbB mutants was noted when this gene was deleted from relatively attenuated parental strains, such as the WT CO92 strain deleted for the lpp gene and the pgm locus-negative strain EV76 of Y. pestis. In contrast, ΔmsbB mutants generated from highly virulent strains such as Y. pestis CO92 or Y. pestis 231 did not possess such traits (39). Therefore, better protection may be linked directly to the less virulent phenotypes of the ΔmsbB mutants in conjunction with the reduced virulence of the parental background strain. In support of this, higher levels of protection against WT CO92 rechallenge were observed in mice immunized with the Δlpp mutant generated in the Y. pestis KIM/D27 background strain, which is pgm locus negative (44). However, deletion of the lpp gene from CO92 did result in attenuated virulence but did not provide significant protection from subsequent WT rechallenge (Fig. 3).
Although we have provided evidence indicating similar T-cell responses in mice infected with either the Δlpp ΔmsbB mutant or the WT strain, other cellular immune components and the humoral immune response also play critical roles against Y. pestis infections, and their alterations may lead to the increased protection seen in the Δlpp ΔmsbB mutant-infected mice. Indeed, an increased F1 antibody titer was recently reported for Y. pestis EV ΔlpxM-immunized mice, despite decreased F1 antigen production in this mutant (39). Likewise, we previously reported that the Y. pestis KIM/D27 Δlpp mutant induced higher levels of cytokine production from T cells and macrophages, evoked NF-κB activation, and resulted in decreased apoptosis of macrophages and splenocytes of mice (4). The Δlpp ΔmsbB mutant of S. Typhimurium induced significantly higher IL-6 and minimal IFN-γ from mouse splenic T cells and evoked superior T-cell activation compared to WT S. Typhimurium (55). Therefore, detailed studies are still needed to further dissect the immunity elicited by the various ΔmsbB mutant strains.
Recently, several studies reported that Y. pestis strains producing hexa-acylated lipid A LPS at 37°C via expression of an additional late acyltransferase (LpxL) from E. coli induced robust innate immunity and were attenuated in both in vivo and in vitro models (20, 40, 41). Perhaps taking such an approach and expressing the gene encoding LpxL in our Δlpp strain(s) may result in a more balanced response of innate immunity and proinflammatory cytokine/chemokine production while serving as an excellent candidate for a live plague vaccine.
In summary, we have generated ΔmsbB and Δlpp ΔmsbB mutants from the highly virulent Y. pestis CO92 strain and provided new information regarding adaptive immunity and memory responses elicited by the WT and the Δlpp ΔmsbB mutant. The Δlpp ΔmsbB double mutant was significantly attenuated in mouse and rat models of bubonic and pneumonic plague. This double mutant was also compromised in its abilities to disseminate to various mouse organs and to survive within murine macrophages. The Δlpp ΔmsbB double mutant exhibited much reduced bacterial virulence but maintained immunogenicity at a level comparable to that of the WT bacterium, and it induced long-lasting T-cell responses. Most importantly, animals immunized with the Δlpp ΔmsbB mutant exhibited maximum protection against rechallenge with WT CO92 in both bubonic and pneumonic plague models. Thus, deletion of both the lpp and msbB genes from WT CO92 could perhaps represent an attractive strategy for developing a live-attenuated vaccine in the future. In addition, whether further alteration of such a vaccine strain may fine-tune innate and adaptive immunity, which is beneficial, needs to be studied.
Supplementary Material
ACKNOWLEDGMENTS
This research was supported by NIH/NIAID grants AI064389 and NO1-AI-30065 awarded to A.K.C. We also acknowledge a UC7 grant (AI070083) which facilitated our research in the Galveston National Laboratory, Galveston, TX. C.J.V.L. was supported by an NIH/NIAID T32 predoctoral training grant on biodefense (AI060549).
We thank Lynn Soong, Department of Microbiology and Immunology, UTMB, for helpful discussions on performing immunological experiments.
Footnotes
Published ahead of print 28 December 2012
Supplemental material for this article may be found at http://dx.doi.org/10.1128/IAI.01067-12.
REFERENCES
- 1. Dennis DT, Chu MC. 2003. A major new test for plague. Lancet 361: 191– 192 [DOI] [PubMed] [Google Scholar]
- 2. Chanteau S, Rahalison L, Ralafiarisoa L, Foulon J, Ratsitorahina M, Ratsifasoamanana L, Carniel E, Nato F. 2003. Development and testing of a rapid diagnostic test for bubonic and pneumonic plague. Lancet 361: 211– 216 [DOI] [PubMed] [Google Scholar]
- 3. Ratsitorahina M, Chanteau S, Rahalison L, Ratsifasoamanana L, Boisier P. 2000. Epidemiological and diagnostic aspects of the outbreak of pneumonic plague in Madagascar. Lancet 355: 111– 113 [DOI] [PubMed] [Google Scholar]
- 4. Liu T, Agar SL, Sha J, Chopra AK. 2010. Deletion of Braun lipoprotein gene (lpp) attenuates Yersinia pestis KIM/D27 strain: role of Lpp in modulating host immune response, NF-kappaB activation and cell death. Microb. Pathog. 48: 42– 52 [DOI] [PubMed] [Google Scholar]
- 5. Feodorova VA, Corbel MJ. 2009. Prospects for new plague vaccines. Expert Rev. Vaccines 8: 1721– 1738 [DOI] [PubMed] [Google Scholar]
- 6. Glauser MP, Zanetti G, Baumgartner JD, Cohen J. 1991. Septic shock: pathogenesis. Lancet 338: 732– 736 [DOI] [PubMed] [Google Scholar]
- 7. Braun V, Hantke K. 1974. Biochemistry of bacterial cell envelopes. Annu. Rev. Biochem. 43: 89– 121 [DOI] [PubMed] [Google Scholar]
- 8. Hayashi S, Wu HC. 1990. Lipoproteins in bacteria. J. Bioenerg. Biomembr. 22: 451– 471 [DOI] [PubMed] [Google Scholar]
- 9. Rebeil R, Ernst RK, Jarrett CO, Adams KN, Miller SI, Hinnebusch BJ. 2006. Characterization of late acyltransferase genes of Yersinia pestis and their role in temperature-dependent lipid A variation. J. Bacteriol. 188: 1381– 1388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nikaido H. 2003. Molecular basis of bacterial outer membrane permeability revisited. Microbiol. Mol. Biol. Rev. 67: 593– 656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Somerville JE, Jr, Cassiano L, Bainbridge B, Cunningham MD, Darveau RP. 1996. A novel Escherichia coli lipid A mutant that produces an anti-inflammatory lipopolysaccharide. J. Clin. Invest. 97: 359– 365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Clementz T, Bednarski JJ, Raetz CR. 1996. Function of the htrB high temperature requirement gene of Escherichia coli in the acylation of lipid A: HtrB catalyzed incorporation of laurate. J. Biol. Chem. 271: 12095– 12102 [DOI] [PubMed] [Google Scholar]
- 13. Clementz T, Zhou Z, Raetz CR. 1997. Function of the Escherichia coli msbB gene, a multicopy suppressor of htrB knockouts, in the acylation of lipid A. Acylation by MsbB follows laurate incorporation by HtrB. J. Biol. Chem. 272: 10353– 10360 [DOI] [PubMed] [Google Scholar]
- 14. Anisimov AP, Shaikhutdinova RZ, Pan'kina LN, Feodorova VA, Savostina EP, Bystrova OV, Lindner B, Mokrievich AN, Bakhteeva IV, Titareva GM, Dentovskaya SV, Kocharova NA, Senchenkova SN, Holst O, Devdariani ZL, Popov YA, Pier GB, Knirel YA. 2007. Effect of deletion of the lpxM gene on virulence and vaccine potential of Yersinia pestis in mice. J. Med. Microbiol. 56: 443– 453 [DOI] [PubMed] [Google Scholar]
- 15. Oyston PC, Prior JL, Kiljunen S, Skurnik M, Hill J, Titball RW. 2003. Expression of heterologous O-antigen in Yersinia pestis KIM does not affect virulence by the intravenous route. J. Med. Microbiol. 52: 289– 294 [DOI] [PubMed] [Google Scholar]
- 16. Perez-Gutierrez C, Llobet E, Llompart CM, Reines M, Bengoechea JA. 2010. Role of lipid A acylation in Yersinia enterocolitica virulence. Infect. Immun. 78: 2768– 2781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Knirel YA, Lindner B, Vinogradov EV, Kocharova NA, Senchenkova SN, Shaikhutdinova RZ, Dentovskaya SV, Fursova NK, Bakhteeva IV, Titareva GM, Balakhonov SV, Holst O, Gremyakova TA, Pier GB, Anisimov AP. 2005. Temperature-dependent variations and intraspecies diversity of the structure of the lipopolysaccharide of Yersinia pestis. Biochemistry 44: 1731– 1743 [DOI] [PubMed] [Google Scholar]
- 18. Rebeil R, Ernst RK, Gowen BB, Miller SI, Hinnebusch BJ. 2004. Variation in lipid A structure in the pathogenic yersiniae. Mol. Microbiol. 52: 1363– 1373 [DOI] [PubMed] [Google Scholar]
- 19. Kawahara K, Tsukano H, Watanabe H, Lindner B, Matsuura M. 2002. Modification of the structure and activity of lipid A in Yersinia pestis lipopolysaccharide by growth temperature. Infect. Immun. 70: 4092– 4098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Montminy SW, Khan N, McGrath S, Walkowicz MJ, Sharp F, Conlon JE, Fukase K, Kusumoto S, Sweet C, Miyake K, Akira S, Cotter RJ, Goguen JD, Lien E. 2006. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 7: 1066– 1073 [DOI] [PubMed] [Google Scholar]
- 21. Parkhill J, Wren BW, Thomson NR, Titball RW, Holden MT, Prentice MB, Sebaihia M, James KD, Churcher C, Mungall KL, Baker S, Basham D, Bentley SD, Brooks K, Cerdeno-Tarraga AM, Chillingworth T, Cronin A, Davies RM, Davis P, Dougan G, Feltwell T, Hamlin N, Holroyd S, Jagels K, Karlyshev AV, Leather S, Moule S, Oyston PC, Quail M, Rutherford K, Simmonds M, Skelton J, Stevens K, Whitehead S, Barrell BG. 2001. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 413: 523– 527 [DOI] [PubMed] [Google Scholar]
- 22. Perry RD, Straley SC, Fetherston JD, Rose DJ, Gregor J, Blattner FR. 1998. DNA sequencing and analysis of the low-Ca2+-response plasmid pCD1 of Yersinia pestis KIM5. Infect. Immun. 66: 4611– 4623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Deng W, Burland V, Plunkett G, 3rd, Boutin A, Mayhew GF, Liss P, Perna NT, Rose DJ, Mau B, Zhou S, Schwartz DC, Fetherston JD, Lindler LE, Brubaker RR, Plano GV, Straley SC, McDonough KA, Nilles ML, Matson JS, Blattner FR, Perry RD. 2002. Genome sequence of Yersinia pestis KIM. J. Bacteriol. 184: 4601– 4611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bashir A, Banday MZ, Haq E. 2011. Lipopolysaccharide, mediator of sepsis enigma: recognition and signaling. Int. J. Biochem. Res. Rev. 1: 1– 13 [Google Scholar]
- 25. Pernerstorfer T, Stohlawetz P, Hollenstein U, Dzirlo L, Eichler HG, Kapiotis S, Jilma B, Speiser W. 1999. Endotoxin-induced activation of the coagulation cascade in humans: effect of acetylsalicylic acid and acetaminophen. Arterioscler. Thromb. Vasc. Biol. 19: 2517– 2523 [DOI] [PubMed] [Google Scholar]
- 26. Jacob A, Hensley LK, Safratowich BD, Quigg RJ, Alexander JJ. 2007. The role of the complement cascade in endotoxin-induced septic encephalopathy. Lab. Invest. 87: 1186– 1194 [DOI] [PubMed] [Google Scholar]
- 27. Neilsen PO, Zimmerman GA, McIntyre TM. 2001. Escherichia coli Braun lipoprotein induces a lipopolysaccharide-like endotoxic response from primary human endothelial cells. J. Immunol. 167: 5231– 5239 [DOI] [PubMed] [Google Scholar]
- 28. Zhang H, Peterson JW, Niesel DW, Klimpel GR. 1997. Bacterial lipoprotein and lipopolysaccharide act synergistically to induce lethal shock and proinflammatory cytokine production. J. Immunol. 159: 4868– 4878 [PubMed] [Google Scholar]
- 29. Aliprantis AO, Yang RB, Mark MR, Suggett S, Devaux B, Radolf JD, Klimpel GR, Godowski P, Zychlinsky A. 1999. Cell activation and apoptosis by bacterial lipoproteins through Toll-like receptor-2. Science 285: 736– 739 [DOI] [PubMed] [Google Scholar]
- 30. Miyake K. 2004. Innate recognition of lipopolysaccharide by Toll-like receptor 4–MD-2. Trends Microbiol. 12: 186– 192 [DOI] [PubMed] [Google Scholar]
- 31. Shimazu R, Akashi S, Ogata H, Nagai Y, Fukudome K, Miyake K, Kimoto M. 1999. MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4. J. Exp. Med. 189: 1777– 1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Raetz CR, Whitfield C. 2002. Lipopolysaccharide endotoxins. Annu. Rev. Biochem. 71: 635– 700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B. 1998. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282: 2085– 2088 [DOI] [PubMed] [Google Scholar]
- 34. Lien E, Means TK, Heine H, Yoshimura A, Kusumoto S, Fukase K, Fenton MJ, Oikawa M, Qureshi N, Monks B, Finberg RW, Ingalls RR, Golenbock DT. 2000. Toll-like receptor 4 imparts ligand-specific recognition of bacterial lipopolysaccharide. J. Clin. Invest. 105: 497– 504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoshino K, Takeuchi O, Kawai T, Sanjo H, Ogawa T, Takeda Y, Takeda K, Akira S. 1999. Cutting edge: Toll-like receptor 4 (TLR4)-deficient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J. Immunol. 162: 3749– 3752 [PubMed] [Google Scholar]
- 36. Rosenzweig JA, Jejelowo O, Sha J, Erova TE, Brackman SM, Kirtley ML, van Lier CJ, Chopra AK. 2011. Progress on plague vaccine development. Appl. Microbiol. Biotechnol. 91: 265– 286 [DOI] [PubMed] [Google Scholar]
- 37. Naumov AV, Ledvanov MY, Drozdov IG. 1992. Plague immunology. Russian Research Anti-Plague Institute, Saratov, Russia: [Google Scholar]
- 38. Titball RW, Williamson ED. 2001. Vaccination against bubonic and pneumonic plague. Vaccine 19: 4175– 4184 [DOI] [PubMed] [Google Scholar]
- 39. Feodorova VA, Pan'kina LN, Savostina EP, Kuznetsov OS, Konnov NP, Sayapina LV, Dentovskaya SV, Shaikhutdinova RZ, Ageev SA, Lindner B, Kondakova AN, Bystrova OV, Kocharova NA, Senchenkova SN, Holst O, Pier GB, Knirel YA, Anisimov AP, Motin VL. 2009. Pleiotropic effects of the lpxM mutation in Yersinia pestis resulting in modification of the biosynthesis of major immunoreactive antigens. Vaccine 27: 2240– 2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Szaba FM, Kummer LW, Wilhelm LB, Lin JS, Parent MA, Montminy-Paquette SW, Lien E, Johnson LL, Smiley ST. 2009. D27-pLpxL, an avirulent strain of Yersinia pestis, primes T cells that protect against pneumonic plague. Infect. Immun. 77: 4295– 4304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sun W, Six D, Kuang X, Roland KL, Raetz CR, Curtiss R., 3rd 2011. A live attenuated strain of Yersinia pestis KIM as a vaccine against plague. Vaccine 29: 2986– 2998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Loppnow H, Brade H, Durrbaum I, Dinarello CA, Kusumoto S, Rietschel ET, Flad HD. 1989. IL-1 induction-capacity of defined lipopolysaccharide partial structures. J. Immunol. 142: 3229– 3238 [PubMed] [Google Scholar]
- 43. Golenbock DT, Hampton RY, Qureshi N, Takayama K, Raetz CR. 1991. Lipid A-like molecules that antagonize the effects of endotoxins on human monocytes. J. Biol. Chem. 266: 19490– 19498 [PubMed] [Google Scholar]
- 44. Sha J, Agar SL, Baze WB, Olano JP, Fadl AA, Erova TE, Wang S, Foltz SM, Suarez G, Motin VL, Chauhan S, Klimpel GR, Peterson JW, Chopra AK. 2008. Braun lipoprotein (Lpp) contributes to virulence of yersiniae: potential role of Lpp in inducing bubonic and pneumonic plague. Infect. Immun. 76: 1390– 1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Edwards RA, Keller LH, Schifferli DM. 1998. Improved allelic exchange vectors and their use to analyze 987P fimbria gene expression. Gene 207: 149– 157 [DOI] [PubMed] [Google Scholar]
- 46. Sha J, Endsley JJ, Kirtley ML, Foltz SM, Huante MB, Erova TE, Kozlova EV, Popov VL, Yeager LA, Zudina IV, Motin VL, Peterson JW, DeBord KL, Chopra AK. 2011. Characterization of an F1 deletion mutant of Yersinia pestis CO92, pathogenic role of F1 antigen in bubonic and pneumonic plague, and evaluation of sensitivity and specificity of F1 antigen capture-based dipsticks. J. Clin. Microbiol. 49: 1708– 1715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fadl AA, Sha J, Klimpel GR, Olano JP, Galindo CL, Chopra AK. 2005. Attenuation of Salmonella enterica serovar Typhimurium by altering biological functions of murein lipoprotein and lipopolysaccharide. Infect. Immun. 73: 8433– 8436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Fadl AA, Sha J, Klimpel GR, Olano JP, Niesel DW, Chopra AK. 2005. Murein lipoprotein is a critical outer membrane component involved in Salmonella enterica serovar Typhimurium systemic infection. Infect. Immun. 73: 1081– 1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sha J, Fadl AA, Klimpel GR, Niesel DW, Popov VL, Chopra AK. 2004. The two murein lipoproteins of Salmonella enterica serovar Typhimurium contribute to the virulence of the organism. Infect. Immun. 72: 3987– 4003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bartra SS, Styer KL, O'Bryant DM, Nilles ML, Hinnebusch BJ, Aballay A, Plano GV. 2008. Resistance of Yersinia pestis to complement-dependent killing is mediated by the Ail outer membrane protein. Infect. Immun. 76: 612– 622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Peterson JW, Comer JE, Baze WB, Noffsinger DM, Wenglikowski A, Walberg KG, Hardcastle J, Pawlik J, Bush K, Taormina J, Moen S, Thomas J, Chatuev BM, Sower L, Chopra AK, Stanberry LR, Sawada R, Scholz WW, Sircar J. 2007. Human monoclonal antibody AVP-21D9 to protective antigen reduces dissemination of the Bacillus anthracis Ames strain from the lungs in a rabbit model. Infect. Immun. 75: 3414– 3424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Peterson JW, Comer JE, Noffsinger DM, Wenglikowski A, Walberg KG, Chatuev BM, Chopra AK, Stanberry LR, Kang AS, Scholz WW, Sircar J. 2006. Human monoclonal anti-protective antigen antibody completely protects rabbits and is synergistic with ciprofloxacin in protecting mice and guinea pigs against inhalation anthrax. Infect. Immun. 74: 1016– 1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Agar SL, Sha J, Foltz SM, Erova TE, Walberg KG, Baze WB, Suarez G, Peterson JW, Chopra AK. 2009. Characterization of the rat pneumonic plague model: infection kinetics following aerosolization of Yersinia pestis CO92. Microbes Infect. 11: 205– 214 [DOI] [PubMed] [Google Scholar]
- 54. Ranallo RT, Kaminski RW, George T, Kordis AA, Chen Q, Szabo K, Venkatesan MM. 2010. Virulence, inflammatory potential, and adaptive immunity induced by Shigella flexneri msbB mutants. Infect. Immun. 78: 400– 412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Liu T, Konig R, Sha J, Agar SL, Tseng CT, Klimpel GR, Chopra AK. 2008. Immunological responses against Salmonella enterica serovar Typhimurium Braun lipoprotein and lipid A mutant strains in Swiss-Webster mice: potential use as live-attenuated vaccines. Microb. Pathog. 44: 224– 237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Toso JF, Gill VJ, Hwu P, Marincola FM, Restifo NP, Schwartzentruber DJ, Sherry RM, Topalian SL, Yang JC, Stock F, Freezer LJ, Morton KE, Seipp C, Haworth L, Mavroukakis S, White D, MacDonald S, Mao J, Sznol M, Rosenberg SA. 2002. Phase I study of the intravenous administration of attenuated Salmonella typhimurium to patients with metastatic melanoma. J. Clin. Oncol. 20: 142– 152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Feodorova VA, Pan'kina LN, Savostina EP, Sayapina LV, Motin VL, Dentovskaya SV, Shaikhutdinova RZ, Ivanov SA, Lindner B, Kondakova AN, Bystrova OV, Kocharova NA, Senchenkova SN, Holst O, Pier GB, Knirel YA, Anisimov AP. 2007. A Yersinia pestis lpxM-mutant live vaccine induces enhanced immunity against bubonic plague in mice and guinea pigs. Vaccine 25: 7620– 7628 [DOI] [PubMed] [Google Scholar]
- 58. Post DM, Ketterer MR, Phillips NJ, Gibson BW, Apicella MA. 2003. The msbB mutant of Neisseria meningitidis strain NMB has a defect in lipooligosaccharide assembly and transport to the outer membrane. Infect. Immun. 71: 647– 655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hajjar AM, Ernst RK, Tsai JH, Wilson CB, Miller SI. 2002. Human Toll-like receptor 4 recognizes host-specific LPS modifications. Nat. Immunol. 3: 354– 359 [DOI] [PubMed] [Google Scholar]
- 60. Kalupahana R, Emilianus AR, Maskell D, Blacklaws B. 2003. Salmonella enterica serovar Typhimurium expressing mutant lipid A with decreased endotoxicity causes maturation of murine dendritic cells. Infect. Immun. 71: 6132– 6140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Galindo CL, Sha J, Moen ST, Agar SL, Kirtley ML, Foltz SM, McIver LJ, Kozlova EV, Garner HR, Chopra AK. 2010. Comparative global gene expression profiles of wild-type Yersinia pestis CO92 and its Braun lipoprotein mutant at flea and human body temperatures. Comp. Funct. Genomics 2010: 342168 doi:10.1155/2010/342168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Li B, Yang R. 2008. Interaction between Yersinia pestis and the host immune system. Infect. Immun. 76:1804– 1811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Feodorova VA, Golova AB. 2005. Antigenic and phenotypic modifications of Yersinia pestis under calcium and glucose concentrations simulating the mammalian bloodstream environment. J. Med. Microbiol. 54: 435– 441 [DOI] [PubMed] [Google Scholar]
- 64. Murray SR, Bermudes D, de Felipe KS, Low KB. 2001. Extragenic suppressors of growth defects in msbB Salmonella. J. Bacteriol. 183: 5554– 5561 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.