Abstract
This paper examines community-level association between exposure to the reproductive health vouchers programme in Kenya and utilization of services. The data are from a household survey conducted among 2527 women (15–49 years) from voucher and comparable non-voucher sites. Analysis entails cross-tabulations with Chi-square tests and significant tests of proportions as well as estimation of multi-level logit models to predict service utilization by exposure to the programme. The results show that for births occurring after the voucher programme began, women from communities that had been exposed to the programme since 2006 were significantly more likely to have delivered at a health facility and to have received skilled care during delivery compared with those from communities that had not been exposed to the programme at all. There were, however, no significant differences in the timing of first trimester utilization of antenatal care (ANC) and making four or more ANC visits by exposure to the programme. In addition, poor women were significantly less likely to have used safe motherhood services (health facility delivery, skilled delivery care and postnatal care) compared with their non-poor counterparts regardless of exposure to the programme. Nonetheless, a significantly higher proportion of poor women from communities that had been exposed to the programme since 2006 used the services compared with their poor counterparts from communities that had not been exposed to the programme at all. The findings suggest that the programme is associated with increased health facility deliveries and skilled delivery care especially among poor women. However, it has had limited community-level impact on the first trimester timing of antenatal care use and making four or more visits, which remain a challenge despite the high proportion of women in the country that make at least one antenatal care visit during pregnancy.
Keywords: Reproductive health, voucher programme, community-level impact, service utilization, Kenya
KEY MESSAGES.
The reproductive health vouchers programme in Kenya is associated with increased utilization of health facility delivery, skilled delivery care and postnatal care services by poor women from communities exposed to it.
However, there is still a wealth gradient in utilization of services even among women from communities exposed to the voucher programme.
The programme has had limited impact on first trimester timing of first antenatal care visit and making four or more visits, which remain low despite the high proportions of women seeking antenatal care services.
Introduction
In many low-income countries, utilization of health care services is affected by both supply and demand factors. The supply-side factors include the availability and quality of services; the demand side, on the other hand, entails socio-economic and socio-cultural factors that determine the uptake of available services (Makinen et al. 2000; Bingham et al. 2003; Ensor and Cooper 2004; Saye and Raine 2007; Simkhada et al. 2008). With donor support, many governments in low-income countries have financed health care inputs—including infrastructure and stocking and staffing health facilities—with varied success (Ensor and Ronoh 2005; Kruk et al. 2007). Moreover, there is evidence from many of these countries that the poor not only benefit less than the wealthy from collectively funded health services, but also suffer greater disease burden (Castro-Leal et al. 2000; Bustreo et al. 2003; Palmer et al. 2003; Gwatkin et al. 2004; Prata et al. 2005). Given the limitations of the traditional input-based approach, interventions that link new demand-generation strategies with stronger incentives for high quality supply side outputs provide, in theory, an alternative to financing health care services in low-income countries. These approaches—referred to as demand-side financing or output-based approaches (OBA)—condition government or donor subsidies on the service user rather than the provider, and include franchising and contracting, social health insurance, conditional cash transfers and vouchers (Posner et al. 2000; Gorter et al. 2003; Janssen et al. 2004; Bhatia and Gorter 2007; Mumssen et al. 2008).
Vouchers, for instance, limit the bearer to a specific set of goods and services at a fixed reimbursement amount (Steuerle 2000; Janssen et al. 2004). It is assumed that their use in combination with results-based provider contracting will stimulate consumer demand for and increase the supply of competitively contracted health care goods and services. Specifically, the voucher empowers the client to choose the appropriate health care provider, while informed client choice has the potential to induce providers to improve the quality of services they offer. Coupled with accreditation of providers based on proven achievement of a specified level of quality, strong quality assurance and monitoring mechanisms, and negotiated reimbursements for services offered, this should ultimately improve service quality, stimulate utilization of services, target services to high-priority populations (such as the poor, women and children) and contain service costs (Steuerle 2000; Mushi et al. 2003). There is evidence that vouchers and other demand-side financing approaches have been used to influence health care services delivery and uptake in many low-income countries with generally positive results, such as increased service utilization, improved service quality, enhanced access to services by the disadvantaged in society and reduced out-of-pocket costs for beneficiaries (Jacobs and Price 2006; Meuwissen et al. 2006; Lagarde et al. 2007; Bellows et al 2011).
In Kenya, the government has implemented a voucher programme since 2006 with funding from the German Development Bank (KfW). Its objective is to significantly reduce maternal and neonatal mortality by increasing the number of health facility deliveries and improving access to appropriate health services—including reproductive health—for the poor through incentives for increased demand and improved service provision (Hagenmeyer et al. 2005; PricewaterhouseCoopers 2008; RH-OBA Technical Committee 2009). The programme subsidizes comprehensive safe motherhood services (up to four antenatal care visits, delivery, postnatal care up to 6 weeks, Caesarean section, if needed, and treatment of maternal and neonatal complications) and long-term family planning methods (implants, intrauterine contraceptive device [IUCD] and voluntary surgical contraception) to economically disadvantaged women in Kisumu, Kitui and Kiambu districts, and in Korogocho and Viwandani informal settlements in Nairobi. The vouchers are made available through distributors appointed by the voucher management agency at a subsidized cost of KSh. 200 (equivalent US$2.50) for safe motherhood and KSh. 100 (equivalent US$1.25) for family planning services. Additional vouchers are made freely available for all women (poor and non-poor) seeking sexual and gender-based violence recovery services. The distributors use a poverty grading tool consisting of eight items on household assets and amenities, expenditure or income, and access to health services that are unique to each district to identify poor women who qualify for the vouchers (those scoring 8–16 points). The design of the programme is described in detail in Hagenmeyer et al. (2005), Janisch et al. (2010) and RH-OBA Technical Committee (2009).
During the first phase of the programme (2006–08), a total of 54 public and private health facilities (18 in Kisumu, 17 in Kiambu, 12 in Nairobi and 7 in Kitui) were contracted as voucher service providers to offer services at specified standards of quality to voucher clients. During the first 2 years of this phase, distributors from non-governmental organizations (NGOs) were used, who received a commission for each voucher sold. This led to vouchers being sold to non-eligible (non-poor) women. This strategy was abandoned and in the final year of the phase, vouchers were sold through salaried distributors (EPOS Health Management 2011). Up to mid 2011, 25 more health facilities were included in the second phase (2008–11) of the programme (six in Kisumu, five in Kiambu, one in Nairobi and 13 in Kitui) while five facilities left the programme for various reasons including fraud or dissatisfaction with the level of reimbursement. In addition, the programme began contracting health facilities and distributing vouchers in Kilifi and Kaloleni Districts in Coast Province from mid 2011.
There has, however, been no systematic evaluation of the programme to determine the impact of vouchers on the utilization of reproductive health services among communities that are exposed to it. Although evidence from similar programmes indicates positive outcomes, a number of contextual, institutional and design factors may determine the effectiveness of voucher schemes. For instance, the legal and regulatory framework, the prevailing socio-economic and political conditions, administrative and management capacity, as well as the reimbursement process can determine whether the programme achieves the desired outcomes (Gorter et al. 2003; Gauri and Vawda 2004). Moreover, in the Kenya programme, no vouchers were sold between November 2008 and May 2009 because of administrative difficulties in extending the contract with the voucher management agency, and this might limit its effectiveness (EPOS Health Management 2011). This paper examines the community-level association between exposure to the voucher programme in Kenya and utilization of reproductive health services by women. It specifically compares the use of family planning, antenatal care, skilled delivery and postnatal care services by respondents from communities exposed to the voucher programme, against use by respondents from communities without such exposure. Exposure is defined as being from a sub-location (the smallest administrative unit in Kenya) within a 5-km radius of a facility that has implemented the voucher programme since 2006, vs being from an area within similar distance to a comparable facility in the voucher areas that have been in the programme since 2010, or being from an area in the non-voucher sites.
Methods
Study design
The study that provided the data for this paper is part of a project implemented by the Population Council, the aim of which is to evaluate the reproductive health vouchers programmes in five countries (Kenya, Uganda, Tanzania, Cambodia and Bangladesh). The Kenya project has a quasi-experimental design with two rounds of data collection at the facility and household levels in voucher and non-voucher sites for comparison. The design was chosen because there was no random assignment of sites or health facilities to intervention (voucher) or comparison (non-voucher) groups. Rather, the voucher sites were identified by the Government of Kenya (GoK) in collaboration with KfW based on need and the availability of health facilities. Health facilities in the selected sites were then approached to participate in the programme and those that met the accreditation criteria were contracted to provide services to voucher clients.
The comparison sites were, on the other hand, identified by the Population Council in collaboration with the two Ministries of Health (Public Health and Medical Services) based on geographical location, population characteristics and availability of health facilities similar to those in voucher sites. Makueni district was therefore identified as the comparison site for Kitui, Nyandarua district for Kiambu, Uasin Gishu district for Kisumu, while there was no comparison site for Nairobi. Except for Uasin Gishu and Kisumu, which are separated by one district, the other voucher and comparison sites are adjacent to each other. Health facilities in the non-voucher sites were then selected on the basis of how comparable they were to voucher service providers in terms of level (hospital, nursing home, health centre and dispensary) and type of ownership (public, private, faith-based and NGO). The first round of data collection took place between February and November 2010 while the second round is expected in 2012. The analysis of the first round of data involves comparison of three groups of women:
Those from within a 5-km radius of facilities that had been implementing the programme since 2006, hereafter referred to as exposed since 2006;
Those from within similar distance of facilities that were added to the programme in 2010, referred to as not exposed from 2006 to 2010; and
Those from non-voucher sites, referred to as not exposed at all.
Data
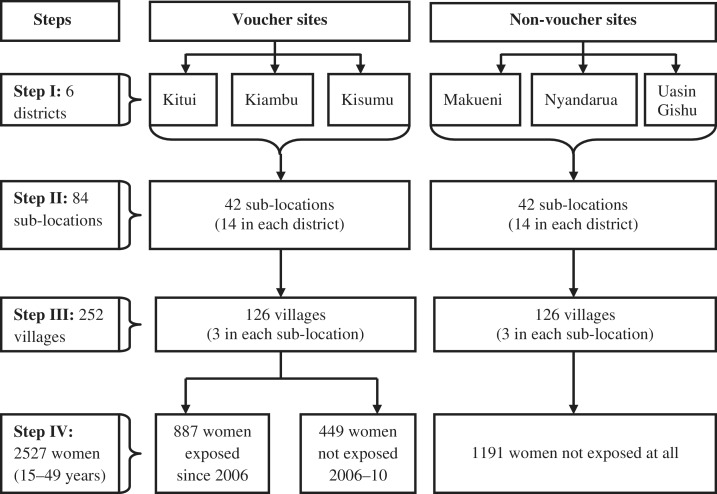
This paper uses data from the household survey that was conducted among women of reproductive age (15–49 years) living within a 5-km radius of contracted and similar non-contracted health facilities in three voucher sites (Kisumu, Kiambu and Kitui) and all the non-voucher sites. The primary sampling unit in the survey was the sub-location. In each district, 14 sub-locations were randomly selected from among those within the stipulated distance to contracted and non-contracted facilities (Figure 1). Three enumeration areas/villages were then randomly selected from each of the sampled sub-locations. Households considered poorest in the enumeration area/village were identified for inclusion in the study with the help of the local administration (Chiefs, Assistant Chiefs and village heads). This approach was informed by the need to capture as many individuals who would qualify for the vouchers as possible given that the vouchers are not randomly assigned to clients. The target sample size in each district in order to detect significant differences between respondents from voucher and comparison sites at 95% confidence level and 80% power was 400 women—about 10 women in each enumeration area/village.
Figure 1.
Steps in sampling and data collection process
In each household, only one member was selected for individual interview. Priority was given to a female member aged between 15 and 49 years who gave birth in the last 12 months or was pregnant at the time of the survey. If a household had more than one such member, the youngest was interviewed since they are likely to be more disadvantaged than older mothers. If the household had no member meeting this criterion, a sexually active female member aged 15–49 years —and therefore a potential family planning client—was interviewed. For households with more than one female sexually active member, only one that was available or willing to be interviewed was included in the study.
A household questionnaire was first administered to the head or, in his/her absence, any responsible member. This captured information on age, sex, relationship to the head and eligibility for individual interview for all members aged 12 years and above. Information was also collected on household assets and amenities, health-related household arrangements, food security and average monthly household expenditures on goods and services. Interviews were conducted in Kiswahili, English or the local language after obtaining written informed consent. Ethical and research clearance was obtained from the Institutional Review Board of the Population Council, the Ethics Review Committee of the Kenya Medical Research Institute (KEMRI), the National Council for Science and Technology (NCST), and the Ministries of Health (Public Health and Medical Services).
Information was collected on background characteristics (age, education level, religious affiliation, marital and employment status); general health status and health care utilization; childbearing experiences and intentions; family planning knowledge and use; awareness and experiences of gender-based violence; and awareness, use and perceptions about reproductive health vouchers. Women who gave birth in the past 5 years before the survey also provided detailed information on each of the births, including antenatal, delivery and postnatal care services as well as experiences and management of any complications. A total of 2352 births were reported by 1992 women over the reference period. Of these, 86% occurred after the voucher programme began (86% in communities exposed since 2006, 83% in communities near facilities added in 2010, and 88% in comparison sites).
Analysis
The analysis focuses on information on women and births occurring after the voucher programme began. The first part involves cross-tabulations with Chi-square tests and significant tests of proportions. The second part entails the estimation of multi-level random-intercept logit models to control for unobserved characteristics of individuals and births identified from the same enumeration area/village and sub-location (Rabe-Hesketh and Skrondal 2008). The basic form of the model is given by Equation (1):
| (1) |
where πijk is the probability of a given outcome for individual or birth i from enumeration area/village j in sub-location k; Xijk is the vector of covariates; β is the associated vector of fixed parameters; and µjk are the unobserved characteristics of individuals or births from the same enumeration area/village and sub-location that might be correlated with the outcomes of interest.
The dependent variables are indicators of utilization of reproductive health services and are measured by nine dichotomous outcomes (Table 1). The independent variable of interest is exposure to the voucher programme with the three categories as described above. The categorization was based on the assumption that most people would walk on average 5 km to a health facility to obtain services. It would thus be expected that in communities exposed to the programme since 2006, most voucher clients would be captured within that radius. In contrast, individuals from communities from within similar radius to facilities that were added in 2010 would have only few voucher clients (those who were able to travel farther than 5 km to seek services), while those from comparison sites would have no voucher clients. The categories were further informed by results from preliminary analysis comparing voucher and non-voucher sites without considering the period of exposure to the programme. This showed no major differences in the use of reproductive health services between the two groups of sites. The number of women interviewed in each category is presented in Figure 1. Other independent variables included in the analysis and their definitions are presented in Table 1.
Table 1.
Definition and measurement of dependent and independent variables
| Variable definition | Measurement |
|---|---|
| Outcome variables | |
| Ever use of any family planning method | 0 = No; 1 = Yes |
| Use of any method in the 12 months preceding survey | 0 = No; 1 = Yes |
| Ever use of LAPM | 0 = No; 1 = Yes |
| Use of LAPM in the 12 months preceding survey | 0 = No; 1 = Yes |
| Making four or more ANC visits | 0 = No; 1 = Yes |
| First trimester ANC visit | 0 = No; 1 = Yes |
| Health facility delivery | 0 = No; 1 = Yes |
| Skilled delivery care | 0 = No; 1 = Yes |
| Postnatal care services for mother and baby | 0 = No; 1 = Yes |
| Independent variables | |
| Exposure to the voucher programme | 1 = Exposed since 2006; 2 = Not exposed from 2006–10; 3 = Not exposed at all |
| Age of respondenta | Single years (ranges from 15 to 49) |
| Education level | 1 = No schooling/pre-unit; 2 = Primary; 3 = Secondary and above |
| Current place of residence | 0 = Urban; 1 = Rural |
| Duration of residence | 1 = Less than 5 years; 2 = 5 years or more; 3 = Always |
| Current marital status | 0 = Never/formerly married; 1 = Married/living together |
| Religious affiliation | 1 = Catholic; 2 = Protestant/other Christian; 3 = Muslim/other/no religion |
| Current employment status | 0 = Unemployed/casual/informal work; 1 = Employed/self-employed |
| Poverty status (according to the poverty grading tool) | 0 = No; 1 = Yes |
| Maternal age at birthb | Single years (ranges from 15 to 48) |
| Woman’s parityb | Ranges from 1 to 11 |
| Sex of childb | 0 = Male; 1 = Female |
| Time since programme began to occurrence of birthb | Single years (ranges from 0 to 4) |
Notes: aNot included in models for antenatal care, health facility delivery and postnatal care services; bIncluded in models for antenatal care, health facility delivery and postnatal care services only. LAPM: long-acting or permanent methods (sterilization, intrauterine contraceptive device or implants); ANC: antenatal care.
The key assumption of the analysis is that the voucher programme had both direct and indirect effects on service utilization. In the first case, individuals from communities exposed to the programme bought and used a voucher to obtain services. In addition, their neighbours who had never bought or used vouchers were encouraged to seek care based on their (voucher users’) positive experiences with services subsidized by the programme or the marketing efforts of the voucher distributors.
Results
Distribution of women by background characteristics
Table 2 presents the distribution of women who were interviewed by various background characteristics and exposure to the voucher programme. The majority of the women were aged 25–34 years, had primary level education, lived in rural areas, had lived at the current place of residence for 5 years or more, were married or living with a man at the time of the survey, and unemployed. There were significant variations in the distribution of women by exposure to the programme in terms of all the background characteristics considered except marital status and household wealth quintile. In addition, 74% of the women were poor according to the poverty grading tool used by the voucher management agency to identify clients. The significant difference in poverty status by exposure to the programme is largely due to the higher proportion of poor women from communities living near facilities that were added to the programme in 2010 compared with those from communities exposed to the programme since 2006 or those from comparison sites.
Table 2.
Percentage distribution of women by various background characteristics according to exposure to the voucher programme
| Characteristics | Exposed since 2006 (%) | Not exposed 2006–10 (%) | Not exposed at all (%) | All women (%) |
|---|---|---|---|---|
| Age group (years) | P < 0.01 | |||
| 15–24 | 38.4 | 25.6 | 28.4 | 31.4 |
| 25–34 | 44.5 | 43.2 | 45.8 | 44.9 |
| 35–44 | 14.7 | 26.7 | 21.6 | 20.1 |
| 45+ | 2.4 | 4.5 | 4.3 | 3.6 |
| Highest education level | P < 0.01 | |||
| No schooling/pre-unit | 1.4 | 4.7 | 3.1 | 2.8 |
| Primary | 66.6 | 76.8 | 67.9 | 69.1 |
| Secondary and above | 32.0 | 18.5 | 29.0 | 28.2 |
| Place of residence | P < 0.01 | |||
| Urban | 26.4 | 9.1 | 13.0 | 17.0 |
| Rural | 73.6 | 90.9 | 87.0 | 83.0 |
| Duration of residence | P < 0.01 | |||
| <5 years | 40.8 | 22.9 | 39.1 | 36.8 |
| ≥5 years | 52.2 | 66.8 | 53.6 | 55.4 |
| Always | 7.0 | 10.2 | 7.3 | 7.7 |
| Current marital status | P = 0.07 | |||
| Never married | 12.3 | 12.3 | 10.3 | 11.4 |
| Married/living together | 79.1 | 77.1 | 82.5 | 80.4 |
| Formerly married | 8.6 | 10.7 | 7.1 | 8.3 |
| Religious affiliation | P < 0.01 | |||
| Catholic | 25.4 | 41.7 | 28.6 | 29.8 |
| Protestant/other Christian | 71.9 | 56.4 | 70.3 | 68.4 |
| Muslim | 1.8 | 0.2 | 0.3 | 0.8 |
| Other/no religion | 0.9 | 1.8 | 0.8 | 1.0 |
| Employment status | P < 0.01 | |||
| Unemployed | 45.8 | 44.3 | 36.1 | 41.0 |
| Employed/self-employed | 30.4 | 39.6 | 41.1 | 37.1 |
| Casual/informal work | 23.8 | 15.8 | 22.8 | 21.9 |
| Missing | 0.0 | 0.2 | 0.1 | 0.1 |
| Household wealth quintile | P = 0.86 | |||
| Poorest | 19.6 | 21.2 | 19.0 | 19.6 |
| Poorer | 19.6 | 22.5 | 19.6 | 20.1 |
| Middle | 19.8 | 18.9 | 20.0 | 19.8 |
| Richer | 20.1 | 18.7 | 20.2 | 19.9 |
| Richest | 20.9 | 18.7 | 21.2 | 20.7 |
| Poverty status | P < 0.01 | |||
| Poor (8–16 points) | 72.2 | 86.2 | 70.9 | 74.1 |
| Non-poor (17–24 points) | 27.8 | 13.8 | 29.1 | 25.9 |
| Number of women | 887 | 449 | 1191 | 2527 |
Note: Percentages may not sum to exactly 100 in some cases due to rounding. P-values are from Chi-square tests for differences by exposure to the voucher programme.
Only 3% of the women from comparison sites had heard about the vouchers compared with 82% in communities exposed to the programme since 2006 and 88% in communities near facilities that were added to the programme in 2010 (Table 3). As expected, none of the women from the comparison sites had ever obtained or used the vouchers. However, similar proportions of women from communities exposed to the programme since 2006 and those from communities not exposed from 2006 to 2010 had ever used the vouchers. Further analysis showed that among those who had ever used vouchers, 10% used them for family planning, 63% for antenatal care, 73% for delivery and 26% for postnatal care services. In communities exposed to the programme since 2006, the proportions of women who used the vouchers for these services were 13% for family planning, 61% for antenatal care, 81% for delivery and 29% for postnatal care. The corresponding proportions for women who had ever used vouchers for the respective services in communities exposed from 2010 were 6%, 66%, 56% and 21%.
Table 3.
Percentage distribution of women by awareness and use of reproductive health services according to exposure to the voucher programme
| Service indicators | Exposed since 2006 (%) | Not exposed 2006–10 (%) | Not exposed at all (%) | All women/ births (%) |
|---|---|---|---|---|
| Reproductive health vouchers | (n = 887) | (n = 449) | (n = 1191) | (n = 2527) |
| Ever heard about the vouchers | 82.3 | 87.8 | 2.7 | 45.8 |
| Ever obtained the voucher | 24.5 | 27.4 | 0.0 | 13.5 |
| Ever used the voucher | 20.5 | 21.4 | 0.0 | 11.0 |
| Family planning services | (n = 887) | (n = 449) | (n = 1191) | (n = 2527) |
| Ever heard about family planning | 98.3 | 94.2 | 97.4 | 97.2 |
| Ever used a method | 73.5 | 45.9 | 75.2 | 69.4 |
| Used a method in the past 12 months | 50.9 | 27.4 | 54.5 | 48.4 |
| Ever used LAPM | 11.5 | 4.0 | 9.6 | 9.3 |
| Used LAPM in the past 12 months | 7.6 | 3.8 | 7.1 | 6.7 |
| Antenatal care servicesa | (n = 715) | (n = 319) | (n = 994) | (n = 2028) |
| Made four or more visits | 60.4 | 56.4 | 60.4 | 59.8 |
| Made first visit in first trimester | 19.6 | 20.4 | 17.9 | 18.9 |
| Delivery and postnatal care servicesa | (n = 715) | (n = 319) | (n = 994) | (n = 2028) |
| Delivered at health facility | 63.4 | 37.0 | 50.4 | 52.9 |
| Received skilled delivery care | 64.1 | 43.0 | 52.2 | 54.9 |
| Obtained postnatal care services | 73.2 | 61.1 | 67.6 | 68.5 |
Notes: aFor births occurring after the voucher programme began. LAPM: long-acting or permanent methods (sterilization, intrauterine contraceptive device or implants).
Use of family planning services
Nearly all the women (97%) had heard about family planning, with no significant difference by exposure to the programme (Table 3). However, the proportion of women who had ever used a family planning method was significantly lower among those from communities near facilities added in 2010 compared with those from communities near facilities that had been in the programme since 2006 or those from comparison sites. A similar pattern is noted for use of a method in the past 12 months preceding the survey, ever use of longer acting or permanent methods (LAPM) and use of LAPM during the 12 months before the survey.
Results from the multi-level logit models predicting the likelihood of family planning use among women by exposure to the voucher programme are presented in Table 4. Although women from communities exposed to the programme since 2006 were 1.4 times more likely to have used LAPM (sterilization, IUCD or implants) in the 12 months before the survey compared with those from comparison sites, the difference is not statistically significant. They were, however, significantly more likely to have ever used these long-term methods compared with their counterparts from the comparison sites. Ever use of LAPM may, however, be affected by prior use before the voucher programme and might not therefore be attributed to the programme.
Table 4.
Odds ratios from the multi-level logit models predicting family planning use among women
| Covariates | Ever use of FP | Use of FP past 12 monthsa | Ever use of LAPMa | Use of LAPM past 12 monthsb |
|---|---|---|---|---|
| Exposure to voucher programme (ref = not exposed at all) | ||||
| Exposed since 2006 | 0.9 (0.6 – 1.4) | 0.8 (0.6 – 1.2) | 1.5* (1.0 – 2.1) | 1.4 (0.9 – 2.2) |
| Not exposed from 2006 to 2010 | 0.3** (0.1 – 0.4) | 0.5** (0.3 – 0.9) | 0.6 (0.3 – 1.1) | 0.9 (0.4 – 1.9) |
| Age (single years) | 1.0** (1.0 – 1.1) | 0.9 (0.9 – 1.0) | 1.1** (1.0 – 1.1) | 1.1** (1.0 – 1.1) |
| Highest education level (ref = no schooling/pre-unit) | ||||
| Primary level | 1.1 (0.6 – 2.0) | 1.3 (0.6 – 2.5) | 1.5 (0.5 – 4.4) | 1.4 (0.4 – 5.1) |
| Secondary and above | 1.1 (0.6 – 2.0) | 1.3 (0.6 – 2.7) | 2.1 (0.7 – 6.3) | 1.8 (0.5 – 7.2) |
| Place of residence (rural = 1) | 0.9 (0.5 – 1.5) | 1.3 (0.9 – 1.9) | 1.1 (0.7 – 1.7) | 1.3 (0.7 – 2.5) |
| Duration of residence (ref = <5 years) | ||||
| 5 years or more | 1.3 (0.9 – 1.6) | 1.1 (0.8 – 1.4) | 1.8** (1.2 – 2.6) | 1.7* (1.1 – 2.6) |
| Always | 0.6* (0.4 – 0.9) | 0.7 (0.4 – 1.2) | 1.3 (0.6 – 2.8) | 1.0 (0.4 – 2.9) |
| Marital status (married/living together = 1) | 1.6** (1.2 – 2.1) | 1.7** (1.3 – 2.4) | 1.5 (0.9 – 2.3) | 0.9 (0.5 – 1.5) |
| Religious affiliation (ref = Catholic) | ||||
| Protestant/other Christian | 0.9 (0.8 – 1.2) | 1.0 (0.8 – 1.3) | 1.4 (0.9 – 2.0) | 1.5 (0.9 – 2.4) |
| Muslim/other/no religion | 1.8 (0.8 – 4.1) | 0.7 (0.3 – 1.5) | 2.5 (0.9 – 6.3) | 3.6* (1.2 – 11.2) |
| Employment status (employed/self-employed = 1) | 1.0 (0.8 – 1.3) | 1.0 (0.8 – 1.3) | 1.2 (0.9 – 1.6) | 1.1 (0.8 – 1.6) |
| Poverty status (poor = 1) | 0.8 (0.6 – 1.0) | 0.7* (0.6 – 0.9) | 1.0 (0.7 – 1.5) | 1.1 (0.7 – 1.6) |
| Children ever born | 0.9 (0.9 – 1.1) | 0.9* (0.8 – 0.9) | 1.0 (0.9 – 1.1) | 1.1 (0.9 – 1.3) |
| Intra- and inter-class correlations | ||||
| Intra-class (within-village) | 0.16 | 0.11 | 0.08 | 0.09 |
| Inter-class (between-village) | 0.14 | 0.02 | 0.03 | 0.07 |
| Number of cases | ||||
| Individuals | 2445 | 1746 | 1746 | 1216 |
| Villages | 252 | 251 | 251 | 236 |
| Sub-locations | 84 | 84 | 84 | 79 |
Notes: aAmong those who ever used a method; bAmong those who ever used LAPM. FP: family planning; LAPM: long-acting or permanent methods (sterilization, intrauterine contraceptive device or implants); ref: reference category. 95% confidence intervals are in parentheses. *P < 0.05; **P < 0.01.
It is also worth noting that compared with unmarried women (never married, divorced, separated and widowed), those who were married or living together with a man at the time of the survey were significantly more likely to have ever used family planning and to have used a method within the 12 months preceding the survey (Table 4). Nonetheless, there was no significant difference in ever or recent use of LAPM by marital status. In addition, older women were significantly more likely to have ever used a family planning method, including LAPM, and to have used LAPM in the past 12 months before the survey compared with younger women.
Use of antenatal care services
There was no significant variation in the proportion of women who made four or more antenatal care visits by exposure to the voucher programme for births occurring after the programme began (Table 3). This applies also to first trimester timing of first antenatal care visit. Results from the multivariate logit models predicting the number of antenatal care visits (four or more) and the timing of the first visit (in the first trimester of pregnancy) show no significant differences in the two indicators of antenatal care utilization by exposure to the programme (Table 5). However, mothers were significantly less likely to have made four or more visits and to have made the first visit in the first trimester for births occurring in later years of the programme (after the programme started) regardless of exposure to the programme. Similarly, women of higher parity were significantly less likely to have made four or more visits and to have made the first visit in the first trimester compared with those of lower parity.
Table 5.
Odds ratios from the multi-level logit models predicting the use of safe motherhood services for births occurring after the voucher programme began
| Covariates | 4+ ANC visits | 1st ANC visit in 1st trimester | Health facility delivery | Skilled delivery care | Received postnatal care |
|---|---|---|---|---|---|
| Exposure to voucher programme (ref = not exposed at all) | |||||
| Exposed since 2006 | 1.1 (0.8 – 1.4) | 1.1 (0.8 – 1.6) | 2.1** (1.5 – 3.1) | 2.0** (1.4 – 2.8) | 1.3 (0.9 – 1.8) |
| Not exposed from 2006 to 2010 | 0.9 (0.7 – 1.4) | 1.3 (0.8 – 2.1) | 0.8 (0.5 – 1.3) | 0.9 (0.6 – 1.5) | 0.8 (0.6 – 1.2) |
| Maternal age at birth (single years) | 1.0** (1.0 – 1.1) | 0.9 (0.8 – 1.0) | 1.0** (1.0 – 1.1) | 1.0** (1.0 – 1.1) | 1.0 (0.9 – 1.0) |
| Highest education level (ref = no schooling/pre-unit) | |||||
| Primary level | 1.2 (0.6 – 2.2) | 0.6 (0.3 – 1.3) | 0.9 (0.4 – 1.8) | 0.7 (0.4 – 1.5) | 1.9 (0.9 – 3.7) |
| Secondary and above | 1.4 (0.7 – 2.8) | 0.8 (0.3 – 1.7) | 1.4 (0.7 – 3.1) | 1.2 (0.6 – 2.6) | 3.0** (1.5 – 6.0) |
| Place of residence (rural = 1) | 1.1 (0.8 – 1.5) | 1.3 (0.8 – 1.9) | 1.2 (0.8 – 1.9) | 1.3 (0.8 – 2.0) | 1.4 (0.9 – 2.1) |
| Duration of residence (ref = <5 years) | |||||
| 5 years or more | 1.1 (0.8 – 1.3) | 1.0 (0.8 – 1.4) | 0.8 (0.7 – 1.1) | 0.9 (0.7 – 1.1) | 1.0 (0.8 – 1.3) |
| Always | 0.9 (0.7 – 1.4) | 1.0 (0.5 – 1.9) | 1.2 (0.7 – 2.1) | 1.3 (0.7 – 2.2) | 1.2 (0.7 – 1.2) |
| Marital status (married/living together = 1) | 0.9 (0.7 – 1.4) | 1.4 (0.9 – 2.1) | 1.2 (0.8 – 1.7) | 1.2 (0.8 – 1.7) | 1.2 (0.9 – 1.7) |
| Religious affiliation (ref = Catholic) | |||||
| Protestant/other Christian | 0.9 (0.8 – 1.3) | 1.1 (0.9 – 1.5) | 0.9 (0.7 – 1.1) | 0.9 (0.7 – 1.1) | 0.9 (0.7 – 1.2) |
| Muslim/other/no religion | 0.6 (0.3 – 1.3) | 0.6 (0.2 – 1.8) | 0.5 (0.2 – 1.2) | 0.5 (0.2 – 1.3) | 1.4 (0.5 – 3.4) |
| Employment status (employed/ self-employed = 1) | 1.1 (0.9 – 1.4) | 1.2 (0.9 – 1.6) | 1.4** (1.1 – 1.8) | 1.4* (1.1 – 1.7) | 1.5** (1.1 – 1.9) |
| Poverty status (poor = 1) | 0.6** (0.5 – 0.8) | 0.9 (0.7 – 1.2) | 0.2** (0.1 – 0.3) | 0.2** (0.1 – 0.3) | 0.4** (0.3 – 0.5) |
| Parity | 0.8** (0.7 – 0.9) | 0.9** (0.8 – 0.9) | 0.7** (0.6 – 0.8) | 0.7** (0.6 – 0.8) | 0.8** (0.7 – 0.9) |
| Sex of child (female = 1) | 1.0 (0.8 – 1.2) | 1.1 (0.9 – 1.3) | 1.1 (0.9 – 1.3) | 0.9 (0.8 – 1.2) | 1.1 (0.9 – 1.4) |
| Time since programme began to birth occurrence (0–4 years) | 0.9* (0.8 – 0.9) | 0.8** (0.8 – 0.9) | 0.9 (0.8 – 1.0) | 0.9 (0.8 – 1.1) | 0.9 (0.8 – 1.1) |
| Intra- and inter-class correlations | |||||
| Intra-class (within-village) | 0.08 | 0.11 | 0.15 | 0.15 | 0.10 |
| Inter-class (between-village) | 0.00 | 0.03 | 0.04 | 0.03 | 0.01 |
| Number of cases | |||||
| Births | 1956 | 1956 | 1956 | 1956 | 1956 |
| Villages | 251 | 251 | 251 | 251 | 251 |
| Sub-locations | 84 | 84 | 84 | 84 | 84 |
Notes: ANC: antenatal care; ref: reference category. 95% confidence intervals are in parentheses. *P < 0.05; **P < 0.01.
Use of delivery and postnatal care services
The proportion of births occurring after the voucher programme began that were delivered at a health facility was significantly higher in communities exposed to the programme since 2006 than in other communities (Table 3). A similar pattern is noted for skilled delivery and postnatal care services. Results from the multivariate logit analysis show that unlike antenatal care utilization, the use of health facility delivery and skilled delivery care services differed significantly by exposure to the voucher programme (Table 5). In particular, births to women from communities exposed to the voucher programme since 2006 were twice as likely to be delivered at a health facility or under skilled care compared with those to women from comparison sites. However, similar to antenatal care utilization, births to women of higher parity were significantly less likely to have been delivered at a health facility or under skilled care compared with births to women of lower parity. This applies to postnatal care utilization as well.
Use of services by poverty status and exposure
Among women from voucher sites, there was no significant difference in the proportion of poor and non-poor women that had used the vouchers (Table 6). A comparison of health service utilization by poverty status shows that there were no significant differences in the proportions of poor and non-poor women who used LAPM in the past 12 months before the survey, or who made the first antenatal care visit within the first trimester of pregnancy, regardless of exposure to the programme. Poor women were, however, significantly less likely to have delivered at a health facility, have been assisted by a skilled provider during delivery, or have received postnatal care services compared with their non-poor counterparts regardless of exposure to the programme (Table 5). Nonetheless, a significantly higher proportion of births to poor women from communities exposed to the programme since 2006 were delivered at a health facility or under skilled care (P < 0.01 in each case) compared with births to poor women from comparison sites (Table 6). The same is noted for postnatal care services (P < 0.05).
Table 6.
Percentage distribution of women using various reproductive health services since the voucher programme started by exposure to the programme and poverty status
| Indicator of service utilization | Exposed since 2006 |
Not exposed 2006–10 |
Not exposed at all |
|||
|---|---|---|---|---|---|---|
| Poor (%) | Non-poor (%) | Poor (%) | Non-poor (%) | Poor (%) | Non-poor (%) | |
| Reproductive health vouchers | (n = 640) | (n = 247) | (n = 387) | (n = 62) | (n = 845) | (n = 346) |
| Ever used the voucher | 20.8 | 19.8 | 20.7 | 25.8 | 0.0 | 0.0 |
| Family planning services | (n = 640) | (n = 247) | (n = 387) | (n = 62) | (n = 845) | (n = 346) |
| Used LAPM past 12 months | 6.9 | 9.3 | 3.9 | 3.2 | 6.6 | 8.1 |
| Antenatal care servicesa | (n = 523) | (n = 192) | (n = 290) | (n = 29) | (n = 712) | (n = 282) |
| Four or more ANC visits | 57.4 | 68.8** | 55.5 | 65.5 | 56.9 | 69.2** |
| First visit in first trimester | 20.3 | 17.7 | 20.0 | 24.1 | 16.4 | 21.6 |
| Delivery/postnatal care servicesa | (n = 523) | (n = 192) | (n = 290) | (n = 29) | (n = 712) | (n = 282) |
| Health facility delivery | 55.1 | 85.9** | 34.1 | 65.5** | 39.5 | 78.0** |
| Skilled delivery care | 55.6 | 87.0** | 40.0 | 72.4** | 42.0 | 78.0** |
| Postnatal care services | 68.3 | 86.5** | 59.0 | 82.8** | 61.7 | 82.6** |
Notes: aFor births occurring after the voucher programme began. LAPM: long-acting or permanent methods (sterilization, intrauterine contraceptive device or implants); ANC: antenatal care. Chi-square tests for differences between poor and non-poor women: *P < 0.05; **P < 0.01.
Discussion
One of the major findings of this paper is that women from communities that had been exposed to the voucher programme since 2006 were significantly more likely to have delivered at a health facility and to have received skilled delivery care for births occurring after the programme started than their counterparts from the comparison sites. It could be that the programme eliminated some of the barriers to accessing these services among women who had been exposed to it, given the generally low levels of utilization—especially of health facility delivery and skilled delivery care—in the country and among women from the comparison sites. For example, only 43% of births in the country are delivered at a health facility, while mothers are assisted by a skilled provider and receive postnatal care services for 44% and 47% of births, respectively (Kenya National Bureau of Statistics [KNBS] and ICF Macro 2010).
There were, however, no significant variations in the utilization of antenatal care services by exposure to the programme. Although the proportion of respondents who sought antenatal care was high, the proportions of births for which mothers made four or more antenatal care visits and for which the first visit was in the first trimester of pregnancy were much lower. This could partly be due to the cost associated with obtaining the vouchers since evidence from other settings where vouchers are free shows increased utilization (Hatt et al. 2010). It could also be a reflection of the general patterns of antenatal care use in Kenya. In particular, although 92% of women in the country seek antenatal care services from skilled providers, only 47% make four or more visits and only 15% make the first visit in the first trimester (KNBS and ICF Macro 2010). The finding suggests that there are still challenges with respect to influencing the timing and number of antenatal care visits, both at the national level and among communities exposed to the voucher programme.
There were also no significant differences in the use of LAPM in the 12 months preceding the survey by exposure to the programme. This could partly reflect the low uptake of these methods in the country, with only 5% of the women using female sterilization, 2% using IUCD and another 2% using implants (KNBS and ICF Macro 2010). It could also be due to low awareness about the family planning vouchers. For instance, only 25% of the women from communities exposed to the programme since 2006 had heard about the family planning vouchers compared with 82% that had heard about the safe motherhood vouchers. This suggests the need to accompany such a voucher scheme with appropriate information, education and communication campaigns given the observed increase in uptake in the recent past as more women became aware of the programme (EPOS Health Management 2011). The lack of significant difference in the use of LAPM by exposure to the programme could further be due to the fact that the study did not evaluate its impact at the community level in the Nairobi sites, where uptake of the family planning vouchers was higher relative to other sites (EPOS Health Management 2011).
The fourth major finding of the paper is that, compared with the comparison sites, a significantly higher proportion of births to poor women from communities exposed to the voucher programme since 2006 were delivered at a health facility, under skilled care and more mothers received postnatal care services. However, poor women were significantly less likely to use these services compared with non-poor women regardless of exposure to the programme. As in many developing countries, the gap between the poor and non-poor in terms of service utilization persists at the national level as well (KNBS and ICF Macro 2010). Thus, although the voucher programme is associated with increased utilization of services by poor women who had been exposed to it since 2006, this has not eliminated the gap between the poor and non-poor. The findings suggest that although financing mechanisms reduce costs of access to services and increase utilization (for example, Kruk et al. 2007), there is need to consider other dimensions of access such as availability and acceptability of services (Say and Raine 2007; Thede et al. 2007). For instance, a poor woman with a voucher might fail to deliver at a contracted health facility because of distance to the facility or negative perceptions about service quality, including provider attitudes.
The importance of distance to care is also evident from the finding that although a similar proportion of women from communities exposed to the programme since 2006 and those from communities not exposed from 2006 to 2010 had ever used the vouchers, the proportion that used the vouchers for delivery was much higher among the former than among the latter group. This could be due to the fact that women from communities not exposed to the programme from 2006 to 2010 had to travel greater distances during this period to facilities in the programme since 2006. In the context of a voucher programme, issues related to distance to care might be addressed by accrediting more facilities that are closer to potential clients and covering transport costs for clients, as is the case in Bangladesh (Hatt et al. 2010; Ahmed and Khan 2011). Negative community perceptions about service quality, on the other hand, could be countered by appropriate information, education and communication campaigns.
However, it is worth noting that the community-level impact of the Kenya vouchers programme on health service utilization might have been under-or over-estimated in the present study due to a number of factors. First, despite the use of a poverty grading tool to identify clients, there was still leakage of vouchers to non-poor women in programme sites, especially during the first 2 years of the programme when distributors worked on commission and sold vouchers to non-poor women. This may have diminished the number of poor women who would have otherwise obtained the vouchers and redeemed them for services from contracted health facilities. It may also have limited the programme’s impact on reducing the gap in the use of services between poor and non-poor women through increased utilization among the non-poor who obtained the vouchers. Moreover, the design of the study may also have resulted in under- or over-estimation of the community-level impact of the programme. In particular, the restriction of the coverage to within 5 km of a voucher facility may have left out those voucher clients who lived beyond the stipulated distance, thereby resulting in under-estimation. In contrast, such restriction might have over-represented voucher clients leading to over-estimation of the impact of the programme especially beyond the 5 km radius. Over-representation of voucher clients could also result from the fact that survey participants were not randomly selected, but were rather identified using an approach similar to that used by the voucher management agency. In addition, the impact of the programme may have been limited by the 7-month lull in voucher sales (November 2008–May 2009) as it took several months after restarting the distribution for the sales to pick up (EPOS Health Management 2011).
The findings might also be affected by other limitations of the study. For instance, it did not determine how much of the increase in service utilization is attributable to vouchers. This is because the survey did not ask detailed questions about use of vouchers for specific services but rather whether respondents had ever used vouchers and for what services. Another limitation is that it does not consider the quality of services received. This is best determined from facility-based data since survey data on quality of care might be affected by recall bias depending on how far back respondents obtained the services. Thirdly, most of the variables included in the models predicting the use of safe motherhood services for births occurring after the programme began—maternal education, place of residence, marital status, religious affiliation, employment status and poverty status—refer to the time of the survey and not the time of the birth. Some of these characteristics might have changed over time in ways that affected exposure to the programme, for example, change of place of residence.
Funding
The evaluation project is funded by the Bill and Melinda Gates Foundation. The reproductive health vouchers programme in Kenya is implemented by the Government with funding from the German Development Bank (KfW).
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The evaluation project of the reproductive health vouchers programme is funded by the Bill and Melinda Gates Foundation and is implemented by the Population Council in collaboration with the National Coordinating Agency for Population and Development (NCAPD), the Ministries of Health, and PricewaterhouseCoopers. Baseline survey data collection received logistical support from the provincial administration (District Commissioners, District Officers, Chiefs, and Assistant Chiefs) and village heads. The project obtained ethical and research clearance from the Institutional Review Board of the Population Council, the Ethics Review Committee of the Kenya Medical Research Institute (KEMRI), the National Council for Science and Technology (NCST), and the Ministries of Health. The views expressed in this paper are solely those of the authors and do not necessarily reflect the views of the funding or implementing agencies.
References
- Ahmed S, Khan MM. A maternal health voucher scheme: what have we learned from the demand-side financing scheme in Bangladesh? Health Policy and Planning. 2011;26:25–32. doi: 10.1093/heapol/czq015. [DOI] [PubMed] [Google Scholar]
- Bellows NM, Bellows BW, Warren C. The use of vouchers for reproductive health services in developing countries: systematic review. Tropical Medicine & International Health. 2011;16:84–96. doi: 10.1111/j.1365-3156.2010.02667.x. [DOI] [PubMed] [Google Scholar]
- Bhatia MR, Gorter AC. Improving access to reproductive and child health services in developing countries: are competitive voucher schemes an option? Journal of International Development. 2007;19:975–81. [Google Scholar]
- Bingham A, Bishop A, Coffey P, et al. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Pública de México. 2003;45:S408–16. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- Bustreo F, Harding A, Axelsson H. Can developing countries achieve adequate improvements in child health outcomes without engaging the private sector? Bulletin of the World Health Organization. 2003;81:886–95. [PMC free article] [PubMed] [Google Scholar]
- Castro-Leal F, Dayton J, Demery L, Mehra K. Public spending on health care in Africa: do the poor benefit? Bulletin of the World Health Organization. 2000;78:66–74. [PMC free article] [PubMed] [Google Scholar]
- Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy and Planning. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- Ensor T, Ronoh J. Impact of organizational change on the delivery of reproductive services: a review of the literature. International Journal of Health Planning and Management. 2005;20:209–25. doi: 10.1002/hpm.810. [DOI] [PubMed] [Google Scholar]
- EPOS Health Management. Bad-Homburg, Germany: EPOS Health Management; 2011. Mid Term Review of the ‘Development of the Health Sector (SWAp) Programme – Reproductive Health Voucher Scheme (Output Based Approach) in Kenya. [Google Scholar]
- Gauri V, Vawda A. Vouchers for basic education in developing economies: an accountability perspective. The World Bank Research Observer. 2004;19:259–80. [Google Scholar]
- Gorter A, Sandiford P, Rojas Z, Salvetto M. Competitive voucher schemes for health: Background paper. Mexico: ICAS; 2003. [Google Scholar]
- Gwatkin D, Bhuiya A, Victora C. Making health systems more equitable. The Lancet. 2004;364:1273–80. doi: 10.1016/S0140-6736(04)17145-6. [DOI] [PubMed] [Google Scholar]
- Hagenmeyer EG, Griffin D, Ahmed R, et al. Berlin: IGES Paper 05-67; 2005. Design study for output-based assistance programme Kenya: Final report. [Google Scholar]
- Hatt L, Nguyen H, Sloan N, et al. Bethesda, MD: Abt Associates Inc; 2010. Economic evaluation of demand-side financing (DSF) for maternal health in Bangladesh. Review, analysis and assessment of issues related to health care financing and health economics in Bangladesh. [Google Scholar]
- Jacobs B, Price N. Improving access for the poorest to public sector health services: insights from Kirivong Operational Health District in Cambodia. Health Policy and Planning. 2006;21:27–39. doi: 10.1093/heapol/czj001. [DOI] [PubMed] [Google Scholar]
- Janisch CP, Albrecht M, Wolfschuetz A, Kundu F, Klein S. Vouchers for health: a demand side output-based aid approach to reproductive health services in Kenya. Global Public Health. 2010;5:578–94. doi: 10.1080/17441690903436573. [DOI] [PubMed] [Google Scholar]
- Janssen M, Maasland E, Mendys-Kamphorst E. The Economics of Demand-side Financing. Rotterdam: SEOR-ECRI; 2004. [Google Scholar]
- Kenya National Bureau of Statistics (KNBS), ICF Macro. Kenya Demographic and Health Survey 2008–09. Calverton, MD: KNBS and ICF Macro; 2010. [Google Scholar]
- Kruk ME, Galea S, Prescott M, Freedman LP. Health care financing and utilization of maternal health services in developing countries. Health Policy and Planning. 2007;22:303–10. doi: 10.1093/heapol/czm027. [DOI] [PubMed] [Google Scholar]
- Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. Journal of the American Medical Association. 2007;298:1900–10. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- Makinen M, Waters H, Rauch M, et al. Inequalities in health care use and expenditures: empirical data from eight developing countries and countries in transition. Bulletin of the World Health Organization. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- Meuwissen LE, Gorter AC, Knottnerus AJA. Impact of accessible sexual and reproductive health care on poor and underserved adolescents in Managua, Nicaragua: a quasi-experimental intervention study. Journal of Adolescent Health. 2006;38:56.e1–56.e9. doi: 10.1016/j.jadohealth.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Mumssen Y, Kumar G, Johannes L. Targeting subsidies through output-based aid. OBApproaches. 2008 No. 22. The Global Partnership on Output-Based Aid. Online at: www.gpoba.org, accessed on 16 December 2008. [Google Scholar]
- Mushi AK, Schellenberg JRA, Mponda H, Lengeler C. Targeted subsidy for malaria control with treated nets using a discount voucher system in Tanzania. Health Policy and Planning. 2003;18:163–71. doi: 10.1093/heapol/czg021. [DOI] [PubMed] [Google Scholar]
- Palmer N, Mills A, Wadee H, Gilson L, Schneider H. A new face for private providers in developing countries: what implications for public health? Bulletin of the World Health Organization. 2003;81:292–97. [PMC free article] [PubMed] [Google Scholar]
- Posner P, Yetvin R, Schneiderman M, Spiro C, Barnett A. A survey of voucher use: variations and common elements. In: Steuerle C, Ooms V, Peterson G, Reischauer R, editors. Vouchers and the Provision of Public Services. Washington, DC: Brookings Institution Press; 2000. pp. 503–37. [Google Scholar]
- Prata N, Montagu D, Jefferys E. Private sector, human resources and health franchising in Africa: policy and practice. Bulletin of the World Health Organization. 2005;83:274–9. [PMC free article] [PubMed] [Google Scholar]
- PricewaterhouseCoopers. Reproductive health output-based aid: end of pilot project report. Vol. 1. Nairobi: PricewaterhouseCoopers; 2008. [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2008. 2nd edn. College Station, TX: Stata Corp LP. [Google Scholar]
- RH-OBA Technical Committee. RH-OBA Review on Quality Assurance: Final Report. Nairobi: RH-OBA Technical Committee; 2009. [Google Scholar]
- Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bulletin of the World Health Organization. 2007;85:812–7. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simkhada B, van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. Journal of Advanced Nursing. 2008;61:244–60. doi: 10.1111/j.1365-2648.2007.04532.x. [DOI] [PubMed] [Google Scholar]
- Steuerle C. Common issues for voucher programs. In: Steuerle C, Ooms V, Peterson G, Reischauer R, editors. Vouchers and the Provision of Public Services. Washington, DC: The Brookings Institution; 2000. pp. 1–37. [Google Scholar]
- Thiede M, Akweongo P, McIntyre D. Exploring the dimensions of access. In: McIntyre D, Mooney G, editors. The Economics of Health Equity. Cambridge: Cambridge University Press; 2007. pp. 103–23. [Google Scholar]