Abstract
In Uganda, as in many parts of Africa, the majority of the population seek treatment for malaria in drug shops as their first point of care; however, parasitological diagnosis is not usually offered in these outlets. Rapid diagnostic tests (RDTs) for malaria have attracted interest in recent years as a tool to improve malaria diagnosis, since they have proved accurate and easy to perform with minimal training. Although RDTs could feasibly be performed by drug shop vendors, it is not known how much customers would be willing to pay for an RDT if offered in these settings. We conducted a contingent valuation survey among drug shop customers in Mukono District, Uganda. Exit interviews were undertaken with customers aged 15 years and above after leaving a drug shop having purchased an antimalarial and/or paracetamol. The bidding game technique was used to elicit the willingness-to-pay (WTP) for an RDT and a course of artemisinin-based combination therapy (ACT) with and without RDT confirmation. Factors associated with WTP were investigated using linear regression. The geometric mean WTP for an RDT was US$0.53, US$1.82 for a course of ACT and US$2.05 for a course of ACT after a positive RDT. Factors strongly associated with a higher WTP for these commodities included having a higher socio-economic status, no fever/malaria in the household in the past 2 weeks and if a malaria diagnosis had been obtained from a qualified health worker prior to visiting the drug shop. The findings further suggest that the WTP for an RDT and a course of ACT among drug shop customers is considerably lower than prevailing and estimated end-user prices for these commodities. Increasing the uptake of ACTs in drug shops and restricting the sale of ACTs to parasitologically confirmed malaria will therefore require additional measures.
Keywords: Willingness-to-pay, contingent valuation, drug shop, malaria, rapid diagnostic test, artemisinin-based combination therapy, Uganda
JEL codes: D12, I11
KEY MESSAGES.
The willingness-to-pay for a rapid diagnostic test (RDT) performed in a drug shop was for the majority of drug shop customers lower than the expected end-user price.
The average willingness-to-pay for a course of artemisinin-based combination therapy (ACT) among drug shop customers was considerably higher than for an RDT but still lower than the current price of an ACT in drug shops.
Increasing the uptake of ACTs in drug shops and restricting the sale of ACTs to parasitologically confirmed malaria will most likely require additional measures.
Further research is required to explore mechanisms to increase demand for RDT diagnosis prior to sale of ACTs in drug shops.
Background
The most recent treatment guidelines for malaria from the World Health Organization recommend prompt parasitological confirmation of suspected malaria illness in all patients before treatment where testing facilities are available (World Health Organization 2010). Rapid diagnostic tests (RDTs) have attracted interest in recent years as a tool to improve malaria diagnosis since they have generally proved accurate (Abba et al. 2011), affordable, quick and relatively easy to perform with minimal training. Proper use of RDTs may also contribute to reduced drug wastage, improved treatment of non-malarial fevers and reduce the risk of development of drug resistance (Hopkins et al. 2009). Economic evaluations have suggested that the use of RDTs can be cost-effective in some settings (Lubell et al. 2008; Shillcutt et al. 2008). There has been a rapid increase in the roll-out of RDTs in public health facilities, although evidence suggests that some providers do not always adhere to the test results, continuing to prescribe antimalarials despite negative results (Hamer et al. 2007; Reyburn et al. 2008; Ansah et al. 2010).
In most countries of Africa, large proportions of the population utilize the private sector, and in particular drug shops, as their first option for treatment of fever and malaria (Amexo et al. 2004; Mota et al. 2009). Similar treatment-seeking behaviour is seen in Uganda, where it is estimated that around 50% of all distribution of antimalarials to end users is through drug shops (ACTWatch 2009), yet surveys in early 2009 found that the first-line malaria treatment, artemisinin-based combination therapies (ACTs), was in stock in only 8% of private sector providers and that the sale of a range of older, less effective antimalarials was still common (ACTWatch 2009; O’Connell et al. 2011). In addition, malaria diagnosis in Ugandan drug shops is rarely based on a parasitological diagnosis since microscopes are typically not available (ACTWatch 2009) and RDTs have not yet been included in the list of commodities that registered drug shops are allowed to sell.
Given that a large proportion of Ugandans visit drug shops as their first option for treatment, there is increasing interest in improving malaria case management in these outlets. Uganda is one of the eight countries piloting the Affordable Medicines Facility – malaria (AMFm), which aims to increase access to good quality affordable ACTs in the public, non-government organization (NGO) and private sectors in malaria-endemic countries through a manufacturer-level subsidy (Arrow et al. 2004; Laxminarayan and Gelband 2009). In this context the possibility of introducing RDTs in drug shops in order to improve the targeting of ACTs is also being considered. However, it is not known whether the community would be willing to pay for RDTs, and if so how much. RDTs are a relatively new commodity in Uganda, being first introduced into government health facilities in 2008. In contrast, ACTs have been in use in government facilities since 2005.
In the only published ‘willingness-to-pay’ (WTP) study for an RDT we could identify in an African setting (Uzochukwu et al. 2010), customers in Nigeria reported a WTP of 431 Naira (US$3.32). However, no similar studies have been conducted elsewhere in sub-Saharan Africa. The main objective of this study was to determine the willingness-to-pay for an RDT for malaria among customers in registered drug shops in Mukono District, central Uganda, and to identify factors influencing the price that customers are willing to pay. In addition, this study explored the WTP for a course of ACT with and without confirmation with an RDT. This study is nested within an ongoing randomized community trial investigating the feasibility, acceptability and cost-effectiveness of introducing RDTs in drug shops in Mukono District, Central Uganda.
Methods
Study site and population
The study was conducted in Mukono District in Central Uganda over a period of 5 weeks in June–July 2009 during the peak of the rainy season. Mukono District had an estimated population of 808 000 in 2002 and is predominantly rural, with only 5% of the population living in urban areas and 50% of the working population classified as subsistence farmers (Uganda Bureau of Statistics 2006).
Malaria, predominantly due to Plasmodium falciparum, is the leading cause of morbidity and mortality in the district. The area is considered hyper-endemic for malaria. An exit survey conducted in 65 registered drug shops in Mukono District, after the present study, between June and September 2010 estimated a slide positivity rate of 27% amongst customers with fever (unpublished survey data). In contrast to earlier studies in Uganda in 2009 (ACTWatch 2009; O’Connell et al. 2011), the survey in 2010 revealed that 71% of these drug shops reported having ACTs in stock on the day of the survey. Almost two-thirds (64%) of the drug shop employees visited knew that the first-line malaria drug for uncomplicated malaria is an ACT, but less than one-third (29%) knew what an RDT was for. Parasitological diagnosis was possible in only a minority of drug shops since only 4 out 65 shops reported having a functioning microscope and none stocked RDTs. Focus group discussions conducted with community members and in-depth interviews with drug shop vendors in Mukono in 2009 likewise found a widespread awareness of ACTs, which were universally perceived as being highly effective (unpublished data), but less familiarity with RDTs (Mbonye et al. 2010; Chandler et al. 2011).
Survey methods
The general approach chosen was a contingent valuation survey with a willingness-to-pay format. This approach was considered appropriate for this study as RDTs were not well-known goods at the time of the study. Contingent valuation is a method designed to establish preferences among a group of individuals for a commodity not presently available on the market, or for commodities where the current price does not reflect its value to individuals. A monetary value is captured from individuals by asking them to imagine that the commodity in question is available on the market and how much they would be ‘willing-to-pay’ (WTP) as a maximum to have the good, or alternatively the minimum value they would be ‘willing-to-accept’ (WTA) for being deprived of the commodity (Klose 1999; Smith 2003). Contingent valuation has been particularly popular for valuing environmental interventions since in this field the problem of missing or non-functioning markets is pervasive (Hanley et al. 2003), but this method has also been increasingly used for valuing health services both in developed and in developing countries in recent years (Whittington 1998; Smith 2003). Contingent valuation surveys have been conducted for a wide range of health services including an AIDS vaccine (Bishai et al. 2004), a malaria vaccine (Sauerborn et al. 2005), improved child survival (Weaver et al. 1996), insecticide-treated mosquito nets (Onwujekwe et al. 2008) and ACT (Wiseman et al. 2005). While there is some empirical evidence supporting the ability of contingent valuation to yield WTP figures which are good predictors of actual WTP (Blumenschein et al. 2001; Onwujekwe et al. 2001; Onwujekwe 2004), there is continuous debate on various aspects such as the best elicitation techniques and a range of possible biases (Klose 1999; Smith and Sach 2010).
An important component of contingent valuation is the format for eliciting WTP. A range of different formats has been used including open-ended questions, closed questions (‘take it or leave it’) and the bidding game (Russell et al. 1995; Klose 1999; Smith 2000), but there is no consensus regarding a gold standard for WTP elicitation in the literature (Klose 1999; Onwujekwe 2004). For this study, a bidding game technique was chosen because it was expected to have content validity in the setting of Mukono where there is some room for negotiating the price of most goods. In addition, a few empirical studies have found the bidding game to be very reliable (Whittington et al. 1992; Cho et al. 2000) and more reliable than closed questions (Dong et al. 2003a; Onwujekwe et al. 2005).
Following the general advice that the hypothetical choice must be presented to a respondent as a realistic and plausible situation as far as possible (Russell et al. 1995; Whittington 1998; Smith 2003), the survey was conducted as exit interviews among drug shop customers seeking treatment for fever or malaria.
The interviews were conducted by five field assistants who had at least 7 years of schooling and undertook 5 days of training in general interviewing skills, understanding and performing an RDT and learning about the difference between ACTs and other antimalarials. Two days were dedicated to training on the bidding game technique, where interviewers participated in role plays followed by discussions and agreement on the best ways of presenting the scenarios and conducting the bidding games. This ensured standardization of bidding game elicitation among interviewers. They also participated in the pretesting and revision of the tools before actual field work.
The trained interviewers were placed near drug shops where they observed all trades in drug shops. Customers who had purchased an antimalarial and/or paracetamol for fever were approached by the interviewers once the drug shop trade had finished, and interviews were conducted in a quiet place near the shop.
Data collection instrument
The contingent valuation questionnaire comprised three main categories of questions. The first section described the purpose of the study, sought verbal consent and established eligibility through a set of screening questions. Individuals eligible for an interview were customers of 15 years and above and who were either a head of household, a spouse of the head of household or respondents who in their own opinion ‘participated in the decision on what to do if a member of the household is suffering from fever’. If the customer was a child below 15 years, interviewers accompanied the child to his/her home to perform the interview with an eligible family member.
The second category of questions captured information on factors believed to influence the willingness-to-pay for an RDT and treatment with ACT. These included questions on the demographic and socio-economic background of the individual as well as factors that had been found to influence willingness-to-pay for different malaria preventive and treatment services in previous studies. These included the presence of fever/malaria among family members in the previous 2 weeks, distance from home to a provider, travel time to a provider and whether a diagnosis had been obtained prior to the visit to the drug shop (Cho et al. 2000; Onwujekwe et al. 2004a; Wiseman et al. 2005; Chase et al. 2009). Socio-economic status was assessed through a list of questions about ownership of assets taken from the 2006 Uganda Demographic and Health Survey (Uganda Bureau of Statistics and Macro International Inc. 2007). Responses were used to develop a socio-economic status index using principal component analysis (Filmer and Pritchett 2001; Vyas and Kumarayanake 2006). Individuals were ranked according to the index and grouped into quintiles.
The third section consisted of the willingness-to-pay elicitation. Three hypothetical scenarios were described to the respondent which involved them coming to a drug shop as a patient with suspected malaria and being offered diagnostic and/or treatment services. Respondents were asked to state their willingness-to-pay for: (1) a course of ACT for an adult, (2) an RDT performed by the drug shop employee and (3) a course of ACT for an adult after having purchased an RDT which turned out to be positive. More details on the scenarios are provided in the appendix. Scenarios 1 and 3 were introduced in order to examine if there were systematic differences in willingness-to-pay for a course of ACT according to whether malaria had been confirmed by an RDT or not.
Interviewers were instructed to simulate an auction process: first they presented the respondent with the starting offer and asked her/him whether s/he was willing to pay that amount. Respondents who were willing to pay the initial amount were then asked about a higher offer. Bidding continued as long as the response was still “yes”. If the respondent said “no” to an offer, the bidding process was stopped and respondents were asked for the maximum they were willing to pay as an open-ended question. The amount stated in the open-ended question should logically lie between the last two offers and interviewers were instructed to remind the respondents about the last two offers. The starting offers were the same for all respondents and set at a low level as judged by WTP answers from the pilot test of the questionnaire [UGX500 (US$0.25) for an RDT and UGX2000 (US$1.00) for a course of ACT]. After each bidding game for eliciting WTP for the goods for an adult, an open-ended question was posed to obtain the WTP for the same goods for a child.
Sampling
A multi-stage sampling procedure was used to select the drug shops. A list of all 17 census enumeration areas (EAs) for Mukono district was obtained from the Uganda Bureau of Statistics. All EAs with a health centre II were selected resulting in 14 eligible EAs.1 For logistical convenience, five EAs were randomly selected from this list. Using a list of drug shops registered by the National Drug Authority, 25 drug shops were randomly selected from the five EAs.
We calculated that a sample size of 500 exit interviews (20 per drug shop) would be needed to estimate the mean willingness-to-pay for an RDT with a 95% confidence interval of ±15%, assuming a mean of UGX1600 (US$0.80), a standard deviation of UGX1400 (US$0.70) and an intra-cluster correlation of 0.15.
Ethical clearance
Ethical clearance for the study was obtained from the institutional review board of the Uganda National Council for Science and Technology, Kampala, in March 2009 (reference number HS 546) and the Ethics Committee of the London School of Hygiene and Tropical Medicine (application number 5709).
Statistical methods
Data were entered and verified in EpiData Entry version 3 (The EpiData Association, Odense, Denmark) and analysed using STATA version 10 (StataCorp, Texas, USA). Linear regression was used to examine factors influencing customers’ WTP for an RDT, a course of ACT and a course of ACT after a positive RDT, respectively. Factors associated with WTP in the univariate analyses (P ≤ 0.10) were included in a multivariable model. All factors that remained significantly associated (P ≤ 0.10) and with geometric mean ratios above 1.2 or below 0.8 in this multivariable model were retained. These models were fitted to the natural logarithm of the WTP values due to the distributions being right-skewed. The distributions of log transformed WTP values were normally distributed. Results have been transformed back onto the original scale, and geometric means or ratios of geometric means are presented. Log-likelihood ratio tests were used to compare the goodness of fit of the different multivariable models. A paired t-test on log transformed WTP answers was used for comparing the WTP for a course of ACT and a course of ACT after a positive RDT.
Results
Demographic characteristics of respondents
Interviews were conducted with 519 customers visiting a licensed drug shop. Sixteen per cent of interviews were conducted in the respondent’s home. A similar number of males (53%) and females (47%) participated in the interviews, and two-thirds (68%) of customers were aged below 40 years. Over half (52%) were educated up to primary school level and the main occupation of the head of household was farming (44%). The majority of respondents (95%) reported that it would be useful if a test for malaria could be performed at drug shops. Drug stock-outs at public facilities are a common occurrence and thus approximately one-quarter (24%) of those interviewed attended a drug shop with a prior diagnosis of malaria determined by a laboratory test or presumptively by a health worker. Most of the customers (87%) reported having purchased at least one antimalarial during the present visit to the drug shop, including quinine (32%), amodiaquine (21%), sulphadoxine-pyrimethamine (18%) and chloroquine (18%), but only 21 customers (4%) had purchased an antimalarial drug containing artemisinin. The geometric mean of the expenditure by drug shop customers on all drugs including antimalarials, analgesics etc. was UGX1758 (US$0.87) on the day of the interview.
Willingness-to-pay for an RDT and a course of ACT
Bidding games were completed by the majority of drug shop customers to elicit their WTP for an RDT (99%), a course of ACT (97%) and a course of ACT after a positive RDT (96%), and all stated WTP replies were above zero. The geometric mean WTP for an RDT was UGX1067 (US$0.53), with a considerably higher WTP for a course of ACT of UGX3661 (US$1.82), increasing to UGX4128 (US$2.05) for RDT-confirmed malaria (Table 1). Almost two-thirds (63%) of the drug shop customers stated that that they would be willing to pay the same for an RDT for a child as for an adult. The majority of customers said that they were willing to pay less for a course of ACT for a child both without an RDT (85%) and with a prior RDT (82%).
Table 1.
Willingness-to-pay (WTP) in UGX (UGX2010 = US$1)a among 519 drug shop customers for an RDT, a course of ACT and a course of ACT following a positive RDT, Mukono District, Uganda, June–July 2009
| WTP for: | No. of responsesb | Geometric mean (UGX)c | 95% CI | Geometric mean (US$)c | 95% CI |
|---|---|---|---|---|---|
| RDT | 514 | 1067 | [1006; 1132] | 0.53 | [0.50; 0.56] |
| ACT | 502 | 3661 | [3431; 3906] | 1.82 | [1.71; 1.94] |
| ACT after pos. RDT | 500 | 4128 | [3870; 4403] | 2.05 | [1.93; 2.19] |
Notes: aAverage exchange rate during 2009 (www.oanda.com).
b5, 17 and 19 out of 519 drug shop customers had missing values or refused to state a WTP for an RDT, a course of ACT and a course of ACT after a positive RDT, respectively.
cAntilog of the mean of log transformed WTP values.
CI = Confidence Interval
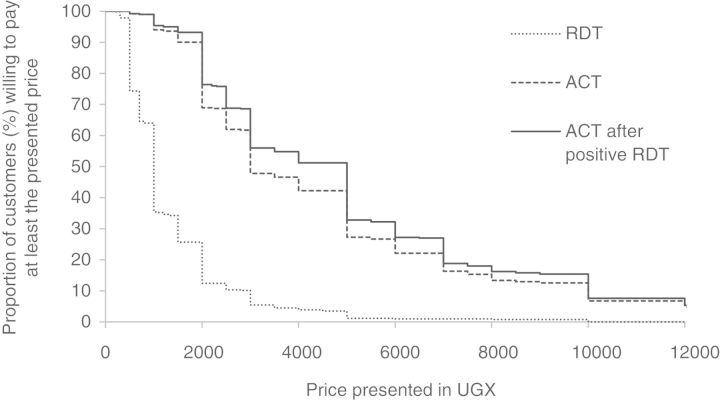
Figure 1 displays the proportion of drug shop customers willing to pay a given price or more for the proposed services. The hypothetical demand for an RDT falls quickly as price increases. For example, 64% of the drug shop customers have a WTP of UGX1000 (US$0.50) or above, while only 26% of customers have a WTP of UGX2000 (US$1.00) or above. The hypothetical demand for ACTs falls more gradually and there is considerable overlap between the two curves for WTP for a course of ACT with or without malaria confirmed by an RDT. Among drug shop customers, 90% were willing to pay UGX2000 (US$1.00) or more for a course of ACT, while 93% were willing to pay this amount or more for an ACT if malaria had been confirmed by an RDT first. Similarly, 27% of customers were willing to pay UGX6000 (US$2.99) or more for a course of ACT and 32% were willing to pay this amount for an ACT after confirmation of malaria by an RDT.
Figure 1.
Relationship between price and the proportion of drug shop customersa willing to pay at least the presented price in UGX (UGX2010 = US$1)b for an RDT, a course of ACT and a course of ACT after a positive RDT, Mukono District, June–July 2009 Notes: a5, 17 and 19 out of 519 drug shop customers had missing values or refused to state a WTP for an RDT, a course of ACT and a course of ACT after a positive RDT, respectively. bAverage exchange rate during 2009 (www.oanda.com).
On average, the WTP for a course of ACT after a confirmation of malaria was significantly higher than the WTP for an ACT course without RDT confirmation (P < 0.001). However, only 33% of the drug shop customers reported a higher WTP for an ACT if malaria had been confirmed by an RDT, with more than half (58%) of customers stating the same WTP for a course of ACT whether or not malaria was RDT-confirmed.
Factors affecting willingness-to-pay
Table 2 shows the univariate associations of demographic and malaria factors with WTP for the three scenarios. A higher WTP for an RDT was associated (P ≤ 0.10) with respondents who were of younger age, female, had a higher level of schooling, occupations other than farming and with higher socio-economic status of the household. Customers with no fever/malaria in the household in the previous 2 weeks and those who had a prior malaria diagnosis given by a health worker or a parasitological test before coming to the drug shop were also more willing to pay a higher price for an RDT. All factors, except gender and education, remained independently associated with the same direction of association in the multivariable analysis (Table 3).
Table 2.
Univariate associations of demographic and malaria factors with the willingness-to-pay for malaria diagnosis and treatment, Mukono District, 2009
| RDT (N = 514) |
Course of ACT (N = 502) |
Course of ACT after positive RDT (N = 500) |
||||
|---|---|---|---|---|---|---|
| na | GMRb [95% CI] | na | GMRb [95% CI] | na | GMRb [95% CI] | |
| Age group (years) | ||||||
| 15–24 | 115 | 1.00** | 114 | 1.00*** | 115 | 1.00*** |
| 25–29 | 81 | 0.83 [0.68; 1.01] | 77 | 0.90 [0.73; 1.11] | 76 | 0.91 [0.73; 1.12] |
| 30–34 | 77 | 0.82 [0.68; 1.00] | 77 | 0.75 [0.60; 0.92] | 75 | 0.85 [0.69; 1.04] |
| 35–39 | 74 | 0.76 [0.63; 0.93] | 73 | 0.76 [0.62; 0.94] | 73 | 0.74 [0.60; 0.91] |
| 40–49 | 81 | 0.79 [0.65; 0.96] | 78 | 0.69 [0.56; 0.86] | 78 | 0.72 [0.58; 0.88] |
| 50+ | 85 | 0.72 [0.60; 0.88] | 82 | 0.67 [0.54; 0.82] | 82 | 0.66 [0.54; 0.81] |
| Gender | ||||||
| Male | 274 | 1.00* | 268 | 1.00** | 267 | 1.00** |
| Female | 240 | 1.12 [0.99; 1.26] | 234 | 1.19 [1.04; 1.35] | 233 | 1.21 [1.06; 1.38] |
| Marital status | ||||||
| Married/cohabiting | 386 | 1.00 | 375 | 1.00 | 373 | 1.00 |
| Not in relationship | 120 | 0.94 [0.82; 1.08] | 119 | 0.92 [0.79; 1.07] | 119 | 0.92 [0.79; 1.08] |
| Level of education | ||||||
| Primary | 271 | 1.00** | 268 | 1.00** | 267 | 1.00** |
| O level | 143 | 1.25 [1.09; 1.44] | 140 | 1.26 [1.09; 1.47] | 138 | 1.28 [1.10; 1.48] |
| A level and above | 51 | 1.27 [1.04; 1.56] | 48 | 1.20 [0.95; 1.50] | 49 | 1.24 [0.99; 1.55] |
| None | 49 | 1.11 [0.90; 1.36] | 46 | 1.17 [0.93; 1.47] | 46 | 1.20 [0.96; 1.51] |
| Occupationc | ||||||
| Farmer | 224 | 1.00*** | 219 | 1.00*** | 219 | 1.00*** |
| Labourer, craftsman | 71 | 1.49 [1.25; 1.79] | 70 | 1.61 [1.33; 1.96] | 69 | 1.60 [1.32; 1.95] |
| Sales | 99 | 1.13 [0.97; 1.33] | 98 | 1.15 [0.97; 1.36] | 97 | 1.15 [0.97; 1.37] |
| Services | 80 | 1.23 [1.04; 1.46] | 76 | 1.38 [1.14; 1.67] | 75 | 1.30 [1.08; 1.57] |
| Unemployed, other | 23 | 1.34 [1.01; 1.78] | 22 | 1.79 [1.31; 2.45] | 23 | 1.55 [1.14; 2.11] |
| Socio-economic status | ||||||
| Lowest | 104 | 1.00*** | 101 | 1.00*** | 101 | 1.00*** |
| Lower middle | 102 | 1.07 [0.89; 1.29] | 99 | 1.22 [1.00; 1.49] | 100 | 1.14 [0.93; 1.39] |
| Middle | 101 | 1.17 [0.97; 1.41] | 101 | 1.16 [0.95; 1.42] | 101 | 1.17 [0.96; 1.42] |
| Upper middle | 103 | 1.28 [1.07; 1.54] | 100 | 1.44 [1.18; 1.77] | 100 | 1.46 [1.20; 1.78] |
| Highest | 102 | 1.48 [1.23; 1.78] | 99 | 1.63 [1.33; 1.99] | 96 | 1.63 [1.34; 2.00] |
| Malaria in household in the past 2 weeks | ||||||
| Presence of malaria | 433 | 1.00*** | 427 | 1.00*** | 425 | 1.00*** |
| No malaria | 28 | 1.61 [1.25; 2.08] | 26 | 1.77 [1.33; 2.35] | 26 | 1.78 [1.34; 2.36] |
| Malaria diagnosis prior to drug shop visitd | ||||||
| No | 388 | 1.00*** | 379 | 1.00** | 377 | 1.00** |
| Yes | 126 | 1.46 [1.27; 1.66] | 123 | 1.28 [1.10; 1.48] | 123 | 1.24 [1.06; 1.43] |
| Travel time to drug shop | ||||||
| Less than 1 hour | 330 | 1.00 | 324 | 1.00** | 322 | 1.00* |
| 1 hour or above | 118 | 1.12 [0.97; 1.29] | 113 | 1.20 [1.02; 1.40] | 113 | 1.17 [1.00; 1.36] |
| Travel distance to drug shop | ||||||
| Less than 1 km | 137 | 1.00 | 136 | 1.00 | 134 | 1.00 |
| 1–3 km | 139 | 0.94 [0.80; 1.10] | 138 | 1.01 [0.85; 1.20] | 138 | 1.07 [0.90; 1.27] |
| 3 km or more | 181 | 1.04 [0.90; 1.21] | 173 | 1.09 [0.93; 1.29] | 173 | 1.07 [0.91; 1.25] |
Notes: *P ≤ 0.10; **P ≤ 0.05; ***P ≤ 0.001.
aThe number of respondents by category in each variable may not add to N due to non-responses.
bGMR stands for geometric mean ratio.
cSales included shopkeeper, retail, wholesale, market vendor. Services included civil servant, driver, security guard, boda boda rider.
d‘No’ indicates patient self-diagnosis or diagnosis without a test by drug seller during the drug shop visit; ‘Yes’ indicates laboratory test or presumptive diagnosis by health worker prior to the drug shop visit.
Table 3.
Multivariable linear regression analysis between willingness-to-pay among drug shop customers for malaria diagnosis and treatment and selected factors, Mukono District, 2009
| RDT | Course of ACT | Course of ACT after positive RDT | |
|---|---|---|---|
| GMRa [95% CI] | GMRa [95% CI] | GMRa [95% CI] | |
| Age group (years) | |||
| 15–24 | 1.00** | 1.00* | 1.00** |
| 25–29 | 0.79 [0.65; 0.96] | 0.87 [0.70; 1.08] | 0.88 [0.71; 1.10] |
| 30–34 | 0.88 [0.72; 1.07] | 0.86 [0.68; 1.08] | 0.95 [0.75; 1.19] |
| 35–39 | 0.74 [0.60; 0.90] | 0.85 [0.68; 1.06] | 0.72 [0.58; 0.90] |
| 40–49 | 0.79 [0.65; 0.96] | 0.75 [0.59; 0.95] | 0.75 [0.60; 0.94] |
| 50+ | 0.76 [0.62; 0.92] | 0.73 [0.59; 0.92] | 0.68 [0.55; 0.84] |
| Level of education | |||
| Primary | 1.00* | ||
| O level | 1.07 [0.91; 1.27] | ||
| A level and above | 1.01 [0.80; 1.29] | ||
| None | 1.38 [1.08; 1.77] | ||
| Occupationb | |||
| Farmer | 1.00** | 1.00** | |
| Labourer, craftsman | 1.28 [1.06; 1.54] | 1.33 [1.07; 1.65] | |
| Sales | 0.94 [0.79; 1.10] | 1.02 [0.84; 1.23] | |
| Services | 0.97 [0.81; 1.16] | 1.09 [0.89; 1.35] | |
| Unemployed, other | 1.09 [0.81; 1.47] | 1.62 [1.13; 2.33] | |
| Socio-economic status | |||
| Lowest | 1.00** | 1.00** | 1.00** |
| Lower middle | 1.04 [0.86; 1.24] | 1.10 [0.89; 1.37] | 1.08 [0.88; 1.34] |
| Middle | 1.11 [0.91; 1.34] | 1.12 [0.89; 1.40] | 1.11 [0.89; 1.38] |
| Upper middle | 1.20 [0.99; 1.45] | 1.33 [1.06; 1.67] | 1.29 [1.03; 1.63] |
| Highest | 1.38 [1.14; 1.68] | 1.53 [1.21; 1.93] | 1.53 [1.20; 1.96] |
| Malaria in household in the past 2 weeks | |||
| Presence of malaria | 1.00*** | 1.00*** | 1.00*** |
| No malaria | 1.67 [1.31; 2.13] | 1.80 [1.35; 2.40] | 1.99 [1.50; 2.64] |
| Malaria diagnosis prior to drug shop visitc | |||
| No | 1.00*** | 1.00** | 1.00** |
| Yes | 1.42 [1.24; 1.63] | 1.24 [1.07; 1.45] | 1.19 [1.02; 1.39] |
| Travel time to drug shop | |||
| Less than 1 hour | 1.00*** | 1.00** | |
| 1 hour or above | 1.38 [1.17; 1.63] | 1.30 [1.10; 1.53] | |
Notes: *P ≤ 0.10; **P ≤ 0.05; ***P ≤ 0.001.
aGMR stands for geometric mean ratio.
bSales included shopkeeper, retail, wholesale, market vendor. Services included civil servant, driver, security guard, boda boda rider.
c‘No’ indicates patient self-diagnosis or diagnosis without a test by drug seller during the drug shop visit; ‘Yes’ indicates laboratory test or presumptive diagnosis by health worker prior to the drug shop visit.
Similar patterns of univariate associations were observed for the WTP for a course of ACT with and without confirmation with an RDT, with the addition of travel time such that customers who travelled longer to a drug shop were more willing to pay a higher price for an ACT. All factors, with the exception of gender and education, remained independently associated with the WTP for a course of ACT in the multivariable analysis. For the WTP for a course of ACT after a positive RDT, gender and occupation were no longer associated after adjusting for the other demographic and malaria factors.
Discussion
The present contingent valuation survey was designed to elicit the willingness-to-pay for an RDT and a course of ACT among individuals choosing to visit drug shops for malaria treatment in Uganda. The results may help to set the initial prices in the private sector for their present customers. While it must be emphasized that the WTP values found in this study may not be generalizable to the population as a whole, the findings may nevertheless be used to draw some general recommendations on public health policy related to the RDTs and ACTs supplied through drug shops in Uganda.
The results of our study suggest that the WTP for an RDT and the WTP for a course of ACT are low and likely to be considerably lower than unsubsidized end-user prices of these commodities. Currently the unsubsidized price of an RDT in drug shops is likely to be in the range of UGX5220–5800 (US$2.54–2.83). This estimate is based on the price offered to both the public and the private sectors by one large Ugandan supplier (Joint Medical Stores 2009) of UGX2900 (US$1.41) including value added tax (VAT) and costs of insurance and freight at the time of the study, and assuming a mark-up of 80–100% as suggested by a survey among drug shops in nine districts (Medicines for Malaria Venture 2008) and in Mukono District (unpublished data). This price was considerably higher than the WTP for an RDT found among most customers in our study where only 4% of the respondents were willing to pay UGX5000 (US$2.49) or more. In order to ensure that many more drug shop customers would be willing to buy an RDT, the price would need to be much lower. Theoretically the price of an RDT should be as low as UGX700 (US$0.35) to ensure that three-quarters of our study participants would be willing to purchase an RDT. Similarly, the average price of an adult course of ACT was UGX15000 (US$7.46) in drug shops in Mukono District at the time of the study (unpublished data), while a country-wide survey found a median price of UGX9000 (US$4.48) (O’Connell et al. 2011). Our results indicate that only 4% and 13% of customers would purchase a course of ACT at these prices and that the price of a course of ACT needed to be as low as UGX2500 (US$1.24) to ensure that 69% of the respondents would purchase this antimalarial. ACTs through the AMFm facility will be made available to customers at a recommended retail price printed on the package of UGX800 (US$0.40) for an adult course. This is double the price of US$0.18 for an adult course of sulphadoxine-pyrimethamine, the most popular antimalarial in Uganda at the time of the study (ACTWatch 2009). Our results suggest that a price of UGX800 for an adult course of ACT would nevertheless still ensure that almost all drug shop customers (99%) in the present survey would purchase this treatment.
The results from our survey suggest that the WTP for both an RDT and a course of ACT is much lower than likely market prices. With the implementation of the AMFm, good quality ACTs should be available in drug shops at low prices (Sabot et al. 2009). However, there are concerns that this will give rise to a marked increase in the use of ACTs by those who do not need them. If the uptake of RDTs in drug shops is to be encouraged in order to improve the targeting of the subsidized ACTs then they too will need to be subsidized; our results indicate that the subsidy will need to be at a level that will ensure that the price of RDTs is substantially lower than that of the ACTs. In Cambodia, where there has been a nationwide programme of subsidized, socially marketed RDTs and ACTs for almost 10 years, the subsidized wholesale price of RDTs was recently reduced to US$0.05 per test, with a recommended retail price (RRP) of US$0.24, in order to incentivize the use of RDTs. This compares with a wholesale price of US$0.42 and RRP of US0.61 for an adult course of recommended ACT (Yeung et al. 2011).
The WTP for an RDT was found to be much lower than the WTP for a course of ACT. In addition, the WTP for a course of ACT after having purchased an RDT confirming malaria was not much higher than the WTP for ACT without parasitological confirmation. A number of factors may have contributed to the lower expressed WTP for an RDT. In contrast to ACTs which were well known and perceived to be highly efficacious and superior to other antimalarials by the local community (unpublished report), RDTs were generally not well known (Mbonye et al. 2010; Chandler et al. 2011) and it may have been more difficult for interviewees to place a value on a commodity that was unfamiliar. In addition, ACTs are currently priced much higher than other antimalarials and thus the customer may expect that all of the funds they have available may be needed for the drug purchase. As the RDT represents a cost in addition to the cost of medication, it may be perceived as unaffordable if the customer believes that the fever is probably due to malaria or that the best way to diagnose a disease is by trying different drugs until one of these removes symptoms (Chandler et al. 2011). Should these beliefs change, or the price of ACT drop, the WTP for an RDT might change.
Nonetheless, the findings of our study suggest that drug shop customers currently place a very low value on seeking parasitological confirmation from an RDT before purchasing an antimalarial and additional measures may be necessary to encourage use of RDTs. Further research is thus needed to investigate and develop specific mechanisms to increase demand for RDT diagnosis prior to sale of ACTs in drug shops. Possible approaches include the use of targeted subsidies and/or offering the RDT and ensuing treatment as a single bundled commodity rather than two separate commodities. For instance, a possible package of diagnosis and treatment could incorporate a proposal to a customer to purchase an RDT after which the customer will be offered a course of ACT for free or at a low price if the test is positive, and another appropriate treatment or advice to seek treatment at a health centre if the test is negative. As this type of package or ‘conditional sale’ of an antimalarial is not normally offered in drug shops, a specific system would need to be set up. A recent study in Kenya explored the use of a voucher system through which the study population could access RDTs and ACTs at different prices (Cohen et al. 2011). One of the packages offered a full refund of the RDT if it was positive and the customer purchased an ACT. Our findings lend support to the need to develop novel interventional mechanisms in order to promote diagnosis in drug shops, and to investigate their feasibility and cost-effectiveness.
The analysis of factors influencing the WTP for malaria diagnosis and treatment showed some variation across different groups in this study. Most notably the WTP increased with the socio-economic quintiles. The implication of this is that relatively low prices of an RDT and a course of ACT are needed to ensure that the poorest sections of drug shop customers will purchase diagnosis and treatment at drug shops. This may be achieved through a high subsidy. Experience of fever or malaria in the household in the previous 2 weeks resulted in a lower WTP for malaria diagnosis and treatment than if no fever or malaria had been experienced. Similar findings regarding a negative association between experience with malaria and WTP for malaria services have been reported in other studies (Onwujekwe et al. 2004b; Udezi et al. 2010). Possible explanations for the association in our study could be that households with a recent experience with fever or malaria still had leftover medication or the fevers experienced were mild or self-resolving. Finally, the associations found in this study could be used for identifying groups to be targeted for an information campaign on the benefits of parasitological diagnosis and ACT. The focus could be on groups which currently have low valuations of RDT diagnosis and ACT such as older age groups and certain occupational groups.
The present contingent valuation survey resulted in plausible WTP values for an RDT and a course of ACT among drug shop customers in Uganda. For instance, the stated WTP for an ACT was not unrealistically higher than the actual expenditure on drugs purchased on the day of the interview (geometric mean of US$1.82 vs US$0.87). It would be expected that the WTP for an ACT is higher than for other antimalarials as the former was described to the respondents as being the most effective. In addition, the WTP for an adult course of ACT was much lower than the actual price of an ACT at the time of the study when a country-wide survey found a median price of UGX9000 (US$4.48) (O’Connell et al. 2011), while a more recent survey found a median price of US$1.92 for an adult course of ACT (Health Action International 2011). Nevertheless, a number of potential limitations of the study should be mentioned.
The validity of the contingent valuation technique has been the subject of much discussion and possible biases have been identified which may drive a wedge between hypothetical and actual WTP (Klose 1999). Hypothetical bias may arise if respondents feel that the scenarios described to them are too hypothetical and therefore they may not take the task presented to them seriously (Onwujekwe et al. 2005). However, it is not clear if hypothetical bias would lead to an underestimate or overestimate of the stated WTPs in this study. In order to minimize this kind of bias, this study tried to simulate as much as possible a realistic and plausible choice situation, for instance by conducting WTP interviews with customers just exiting a drug shop after the purchase of treatment for fever. Starting-point bias refers to the phenomenon whereby respondents’ WTP is influenced by the opening offer and is typically measured by giving different opening offers to different sub-samples of respondents (Dong et al. 2003b). While the extent of starting-point bias was not measured as part of the present study, there are some indications that this might not have been a serious problem. The opening offers in the bidding games were the same for all respondents and set at low values of UGX500 (US$0.25) for an RDT and UGX2000 (US$1.00) for a course of ACT. It was observed during the bidding games that the number of additional offers accepted after the opening bid varied a lot among the respondents, suggesting a deliberate thought process on one’s WTP rather than applying some mechanical process such as accepting the first 2–3 bids and then declining. However, if starting-point bias was a problem, the WTP values obtained might be underestimates of actual WTP since the opening bid was low. Contingent valuation exercises with valuation of several different commodities may experience order-effect bias whereby the order of presentation of commodities to be valued has an influence on the valuation of individual goods. As recommended by several authors (Bateman and Langford 1997; Clark and Friesen 2008), we attempted to minimize the order-effect bias by explaining the full range of goods to be valued during the interview before any elicitation started.
Conclusions
The findings of the present study suggest that the willingness-to-pay for an RDT and an ACT among drug shop customers is considerably lower than prevailing and estimated prices for these goods. If the dual objectives of increasing the uptake of ACTs in drug shops and restricting the prescription of ACTs to parasitologically confirmed malaria are to be achieved, additional interventions will therefore be necessary. The AMFm initiative aims to provide ACTs at low prices through a subsidy. Increased utilization of RDTs may likewise be encouraged through a subsidy large enough to ensure a price considerably lower than the price of a course of ACT. Other approaches such as the introduction of diagnosis and treatment as a single bundled commodity rather than two separate commodities could be a relevant topic for further research.
Funding
This research is supported by the ACT Consortium, which is funded through a grant from the Bill & Melinda Gates Foundation to the London School of Hygiene and Tropical Medicine [grant number 39640]. Sian Clarke is supported by the Wellcome Trust, London, UK through a Career Development Fellowship [084933].
Conflict of interest
The authors hereby state that during the study and article writing they had no conflict of interest whatsoever.
Acknowledgements
We thank Dr Katherine Fielding and Dr Daniela Manno for statistical advice and Ms Mary Beth Thoren for help with the design of the questionnaire. We would also like to thank all participating customers, drug shop vendors and in particular our interviewers: Steven Kalake, Denise Kasenene, Joseph Mugisha, Deborah Namisango and Charity Wamala.
Appendix
Hypothetical scenarios presented to respondents before asking their willingness-to-pay, Mukono District, 2009
Scenario 1: A course of ACT
Assume that you have come to a drug shop today because you think that you may have malaria although you have not taken a test.
I will now give you some additional information on some new malaria drugs.
The Ministry of Health of Uganda now recommends drugs called artemisinin combination therapies or ‘ACTs’, for example Co-artem, for treating malaria. This is because it is a combination of two drugs and cures people more quickly and more effectively than the older antimalarials like chloroquine and fansidar. (Interviewer: show package of Co-artem.)
The Ministry of Health wishes to make ACTs such as Co-artem widely available to the population of Uganda. Private drug sellers cannot offer services for free—they have to charge a price. For this study, it is important to know how valuable Co-artem is for potential customers like yourself.
I will now ask you some questions on what you might do if Co-artem had been available in drug shops today. I want to know if you would consider buying Co-artem from drug sellers, and if yes, how much you would value this drug. I will give different examples of prices for Coartem and then ask you if you would buy a full dose of Co-artem at that price.
If drug shops had Co-artem available today—would you be willing to pay UGX2000 for a course of Co-artem to treat one attack of malaria?
Scenario 2: Rapid diagnostic test (RDT)
Assume that you have come to a drug shop today because you think that you may have malaria although you have not taken a test.
Diagnosis of malaria can be difficult. If you suffer from fever or headache, this may be a sign of malaria which should be treated with antimalarial drugs. However, these symptoms may just as well be another health problem which should be treated with something else. Malaria is caused by parasites in your blood so the best way of finding out if you have malaria is to examine your blood for parasites. In the past this could only be done by using a microscope and was therefore only done in hospitals and some health centres. However, now there is a new simple test to look for malaria parasites which can be performed anywhere and takes about 15 minutes to get the result. This test requires only a drop of blood taken from the finger so this is similar to the way it is done at a health facility when blood is taken for examination using a microscope. Since the test kit will only be used once there is no risk of transmission of diseases during the taking of a drop of blood. In addition, the test can only be used to diagnose malaria and no other disease. The test must be performed by a trained drug seller or a trained health worker. Therefore, an ill person must travel from home to a drug seller or health facility if he/she wants this test for malaria. I will demonstrate a rapid malaria test to you now.
Interviewer: Demonstrate an RDT—explain what will happen if there are malaria parasites in the blood.
The benefits of doing a malaria test before treatment is that the ill person can get the right treatment for his/her illness. If the test shows malaria, the ill person should be treated with an ACT such as Co-artem which will likely cure a patient. If the test does not show malaria, then they do not need an ACT such as Co-artem and an alternative diagnosis and treatment must be determined.
If a malaria test is not performed then nobody can be sure whether or not a fever is malaria and whether or not the antimalarial treatment is necessary or not.
You have come today to a drug seller to buy antimalarial drugs. The drug seller recommends you to buy and carry out a rapid malaria test which will tell you if you actually have malaria. The drug seller explains that he/she will recommend different treatments depending on the result of the rapid malaria test. These are the following:
(A) If the rapid malaria test shows malaria, then he/she will recommend a course of Co-artem which is available at 15000 Shillings, or
(B) If the rapid malaria test shows that your illness is not malaria, then depending on how sick you are, the drug seller will suggest either a course of paracetamol available at 1000 shillings for a simple fever or refer to a health centre/unit for a serious fever.
If drug shops had rapid malaria tests available today—would you be willing to pay UGX500 for a rapid diagnostic test?
Scenario 3: A course of ACT after a positive RDT
Assume that you have come to a drug shop today because you think that you may have malaria but you are not sure. You are therefore considering buying drugs against malaria. You buy a rapid malaria test at the price of 1000 Shillings. The test shows that you have malaria. The drug seller offers you to buy a course of Co-artem explaining that this is the best drug at the market at present.
If you know that you have malaria after taking a rapid malaria test and drug shops had Co-artem available today—would you be willing to pay UGX2000 for a course of Co-artem to treat one attack of malaria?
Endnote
1 The presence of a health centre in an EA was not required for the present contingent valuation survey, but this was an important component for the main trial investigating the feasibility, acceptability and cost-effectiveness of introducing RDTs in drug shops in Mukono District.
References
- Abba K, Deeks JJ, Olliaro PL, et al. Rapid diagnostic tests for diagnosing uncomplicated P. falciparum malaria in endemic countries. Cochrane Database of Systematic Reviews. 2011;7:CD008122. doi: 10.1002/14651858.CD008122.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACTWatch. Washington, DC: Population Services International; 2009. Outlet Survey Report (Baseline), Republic of Uganda, 09/08, 10/08. [Google Scholar]
- Amexo M, Tolhurst R, Barnish G, Bates I. Malaria misdiagnosis: effects on the poor and vulnerable. The Lancet. 2004;364:1896–8. doi: 10.1016/S0140-6736(04)17446-1. [DOI] [PubMed] [Google Scholar]
- Ansah EK, Narh-Bana S, Epokor M, et al. Rapid testing for malaria in settings where microscopy is available and peripheral clinics where only presumptive treatment is available: a randomised controlled trial in Ghana. British Medical Journal. 2010;340:c930. doi: 10.1136/bmj.c930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrow K, Panosian C, Gelband H, editors. Saving Lives, Buying Time: Economics of Malaria Drugs in an Age of Resistance. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Bateman IJ, Langford IH. Budget-constraint, temporal, and question-ordering effects in contingent valuation studies. Environment and Planning A. 1997;29:1215–28. [Google Scholar]
- Bishai D, Pariyo G, Ainsworth M, Hill K. Determinants of personal demand for an AIDS vaccine in Uganda: contingent valuation survey. Bulletin of the World Health Organization. 2004;82:652–60. [PMC free article] [PubMed] [Google Scholar]
- Blumenschein K, Johannesson M, Yokoyama KK, Freeman PR. Hypothetical versus real willingness to pay in the health care sector: results from a field experiment. Journal of Health Economics. 2001;20:441–57. doi: 10.1016/s0167-6296(01)00075-3. [DOI] [PubMed] [Google Scholar]
- Chandler CI, Hall-Clifford R, Asaph T, et al. Introducing malaria rapid diagnostic tests at registered drug shops in Uganda: limitations of diagnostic testing in the reality of diagnosis. Social Science & Medicine. 2011;72:937–44. doi: 10.1016/j.socscimed.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase C, Sicuri E, Sacoor C, et al. Determinants of household demand for bed nets in a rural area of southern Mozambique. Malaria Journal. 2009;8:132. doi: 10.1186/1475-2875-8-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho-Min-Naing, Lertmaharit S, Kamol-Ratanakul P, Saul AJ. Ex post and ex ante willingness to pay (WTP) for the ICT Malaria Pf/Pv test kit in Myanmar. Southeast Asian Journal of Tropical Medicine and Public Health. 2000;31:104–11. [PubMed] [Google Scholar]
- Clark J, Friesen L. The causes of order effects in contingent valuation surveys: an experimental investigation. Journal of Environmental Economics and Management. 2008;58:195–206. [Google Scholar]
- Cohen J, Dupas P, Schaner S. Boston, MA: Harvard School of Public Health. Mimeo; 2011. Prices, diagnostic tests and the demand for malaria treatment: evidence from a randomized trial. [Google Scholar]
- Dong H, Kouyate B, Cairns J, Sauerborn R. A comparison of the reliability of the take-it-or-leave-it and the bidding game approaches to estimating willingness-to-pay in a rural population in West Africa. Social Science & Medicine. 2003a;56:2181–9. doi: 10.1016/s0277-9536(02)00234-4. [DOI] [PubMed] [Google Scholar]
- Dong H, Kouyate B, Cairns J, Mugisha F, Sauerborn R. Willingness-to-pay for community-based insurance in Burkina Faso. Health Economics. 2003b;12:849–62. doi: 10.1002/hec.771. [DOI] [PubMed] [Google Scholar]
- Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Hamer DH, Ndhlovu M, Zurovac D, et al. Improved diagnostic testing and malaria treatment practices in Zambia. Journal of the American Medical Association. 2007;297:2227–31. doi: 10.1001/jama.297.20.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley N, Ryan M, Wright R. Estimating the monetary value of health care: lessons from environmental economics. Health Economics. 2003;12:3–16. doi: 10.1002/hec.763. [DOI] [PubMed] [Google Scholar]
- Health Action International. Retail prices of ACTs co-paid by the AMFm and other antimalarial medicines: Ghana, Kenya, Madagascar, Nigeria, Tanzania and Uganda. 2011 Online at: http://www.theglobalfund.org/documents/amfm/AMFm_PriceTrackingByHAIAugust2011Survey_Report_en, accessed 26 April 2012. [Google Scholar]
- Hopkins H, Asiimwe C, Bell D. Access to antimalarial therapy: accurate diagnosis is essential to achieving long term goals. British Medical Journal. 2009;339:b2606. doi: 10.1136/bmj.b2606. [DOI] [PubMed] [Google Scholar]
- Joint Medical Stores. Catalogue and Price Indicator, August 2009. Kampala: Print Innovations & Publishers Ltd, Kampala; 2009. [Google Scholar]
- Klose T. The contingent valuation method in health care. Health Policy. 1999;47:97–123. doi: 10.1016/s0168-8510(99)00010-x. [DOI] [PubMed] [Google Scholar]
- Laxminarayan R, Gelband H. A global subsidy: key to affordable drugs for malaria? Health Affairs. 2009;28:949–61. doi: 10.1377/hlthaff.28.4.949. [DOI] [PubMed] [Google Scholar]
- Lubell Y, Reyburn H, Mbakilwa H, et al. The impact of response to the results of diagnostic tests for malaria: cost-benefit analysis. British Medical Journal. 2008;336:202–5. doi: 10.1136/bmj.39395.696065.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbonye AK, Ndyomugyenyi R, Turinde A, et al. The feasibility of introducing rapid diagnostic tests for malaria in drug shops in Uganda. Malaria Journal. 2010;9:367. doi: 10.1186/1475-2875-9-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicines for Malaria Venture. Understanding the Antimalarials Market: Uganda 007 – An overview of the supply side. Geneva: Medicines for Malaria Venture; 2008. [Google Scholar]
- Mota RE, Lara AM, Kunkwenzu ED, Lalloo DG. Health seeking behavior after fever onset in a malaria-endemic area of Malawi. American Journal of Tropical Medicine and Hygiene. 2009;81:935–43. doi: 10.4269/ajtmh.2009.08-0361. [DOI] [PubMed] [Google Scholar]
- O’Connell KA, Gatakaa H, Poyer S, et al. Got ACTs? Availability, price, market share and provider knowledge of antimalarial medicines in public and private sector outlets in six malaria-endemic countries. Malaria Journal. 2011;10:326. doi: 10.1186/1475-2875-10-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onwujekwe O, Chima R, Shu E, Nwagbo D, Okonkwo P. Hypothetical and actual willingness to pay for insecticide-treated nets in five Nigerian communities. Tropical Medicine & International Health. 2001;6:545–53. doi: 10.1046/j.1365-3156.2001.00745.x. [DOI] [PubMed] [Google Scholar]
- Onwujekwe O. Criterion and content validity of a novel structured haggling contingent valuation question format versus the bidding game and binary with follow-up format. Social Science & Medicine. 2004;58:525–37. doi: 10.1016/s0277-9536(03)00214-4. [DOI] [PubMed] [Google Scholar]
- Onwujekwe O, Uzochukwu B, Shu E, Ibeh C, Okonkwo P. Is combination therapy for malaria based on user-fees worthwhile and equitable to consumers? Assessment of costs and willingness to pay in Southeast Nigeria. Acta Tropica. 2004a;91:101–15. doi: 10.1016/j.actatropica.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Onwujekwe O, Fox-Rushby J, Hanson K. Valuing the benefits of a health intervention using three different approaches to contingent valuation: re-treatment of mosquito bed-nets in Nigeria. Journal of Health Services Research & Policy. 2004b;9:67–75. doi: 10.1258/135581904322987472. [DOI] [PubMed] [Google Scholar]
- Onwujekwe O, Fox-Rushby J, Hanson K. Inter-rater and test-retest reliability of three contingent valuation question formats in south-east Nigeria. Health Economics. 2005;14:529–36. doi: 10.1002/hec.928. [DOI] [PubMed] [Google Scholar]
- Onwujekwe O, Fox-Rushby J, Hanson K. Construct validity of the bidding game, binary with follow-up, and a novel structured haggling question format in determining willingness to pay for insecticide-treated mosquito nets. Medical Decision Making. 2008;28:90–101. doi: 10.1177/0272989X07308748. [DOI] [PubMed] [Google Scholar]
- Reyburn H, Mbakilwa H, Mwangi R, et al. Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: randomised trial. British Medical Journal. 2008;334:403. doi: 10.1136/bmj.39073.496829.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S, Fox-Rushby J, Arhin D. Willingness and ability to pay for health care: a selection of methods and issues. Health Policy and Planning. 1995;10:94–101. doi: 10.1093/heapol/10.1.94. [DOI] [PubMed] [Google Scholar]
- Sabot OJ, Mwita A, Cohen JM, et al. Piloting the global subsidy: the impact of subsidized artemisinin-based combination therapies distributed through private drug shops in rural Tanzania. PLoS One. 2009;4:e6857. doi: 10.1371/journal.pone.0006857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauerborn R, Gbangou A, Dong H, Przyborski JM, Lanzer M. Willingness to pay for hypothetical malaria vaccines in rural Burkina Faso. Scandinavian Journal of Public Health. 2005;33:146–50. doi: 10.1080/14034940510005743. [DOI] [PubMed] [Google Scholar]
- Shillcutt S, Morel C, Goodman C, et al. Cost-effectiveness of malaria diagnostic methods in sub-Saharan Africa in an era of combination therapy. Bulletin of the World Health Organization. 2008;86:101–10. doi: 10.2471/BLT.07.042259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RD. The discrete-choice willingness-to-pay question format in health economics: should we adopt environmental guidelines? Medical Decision Making. 2000;20:194–206. doi: 10.1177/0272989X0002000205. [DOI] [PubMed] [Google Scholar]
- Smith RD. Construction of the contingent valuation market in health care: a critical assessment. Health Economics. 2003;12:609–28. doi: 10.1002/hec.755. [DOI] [PubMed] [Google Scholar]
- Smith RD, Sach TH. Contingent valuation: what needs to be done? Health Economics, Policy and Law. 2010;5:91–111. doi: 10.1017/S1744133109990016. [DOI] [PubMed] [Google Scholar]
- Udezi WA, Usifoh CO, Ihimekpen OO. Willingness to pay for three hypothetical malaria vaccines in Nigeria. Clinical Therapeutics. 2010;32:1533–44. doi: 10.1016/j.clinthera.2010.07.018. [DOI] [PubMed] [Google Scholar]
- Uzochukwu BS, Onwujekwe OE, Uguru NP, Ughasoro MD, Ezeoke OP. Willingness to pay for rapid diagnostic tests for the diagnosis and treatment of malaria in southeast Nigeria: ex post and ex ante. International Journal for Equity in Health. 2010;9:1. doi: 10.1186/1475-9276-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uganda Bureau of Statistics. The 2002 Uganda Population and Housing Census, Economic Characteristics. Kampala: Uganda Bureau of Statistics; 2006. [Google Scholar]
- Uganda Bureau of Statistics, Macro International Inc. Uganda Demographic and Health Survey 2006. Calverton, MD: UBOS and Macro International Inc; 2007. [Google Scholar]
- Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy and Planning. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- Weaver M, Ndamobissi R, Kornfield R, et al. Willingness to pay for child survival: results of a national survey in Central African Republic. Social Science & Medicine. 1996;43:985–98. doi: 10.1016/0277-9536(96)00015-9. [DOI] [PubMed] [Google Scholar]
- Wiseman V, Onwujekwe O, Matovu F, Mutabingwa TK, Whitty CJ. Differences in willingness to pay for artemisinin-based combinations or monotherapy: experiences from the United Republic of Tanzania. Bulletin of the World Health Organization. 2005;83:845–52. [PMC free article] [PubMed] [Google Scholar]
- Whittington D. Administering contingent valuation surveys in developing countries. World Development. 1998;26:21–30. [Google Scholar]
- Whittington D, Smith VK, Okorafor A, et al. Giving respondents time to think in contingent valuation studies: a developing country application. Journal of Environmental Economics & Management. 1992;22:205–25. [Google Scholar]
- World Health Organization. Guidelines for the Treatment of Malaria, 2nd edition. Geneva: World Health Organization; 2010. [Google Scholar]
- Yeung S, Patouillard E, Allen H, Socheat D. Socially-marketed rapid diagnostic tests and ACT in the private sector: ten years of experience in Cambodia. Malaria Journal. 2011;10:243. doi: 10.1186/1475-2875-10-243. [DOI] [PMC free article] [PubMed] [Google Scholar]