Abstract
Tailgut cysts are rare congenital anomalies, believed to be remnants of the primitive embryonic hindgut. In addition to causing genitourinary and bowel obstructive symptoms, they have been reported to harbour occult adenocarcinoma. Varying positions of a tailgut cyst with respect to the rectum have also been reported in literature. We present a rare presentation of this disease vis a vis obstipation and acute urinary retention in a 70 year old man.
Keywords: Congenital, Tailgut cyst, Urinary retention, Obstipation
Introduction
Believed to be remnants of the embryonic hindgut, Tailgut cysts have rarely presented with urinary tract and bowel obstruction. These cysts are predominantly retrorectal but varied positions like prerectal, perirenal and perianal have been reported. Tumor markers shown to be positive for tailgut cyst adenocarcinomas are CEA and CA19.9 and these markers have a valuable role in the monitoring of tumor recurrence and response to treatment. Surgical treatment is the rule for diagnosis as well as to circumvent malignant transformation.
Case History
A 70 year old diabetic gentleman presented with constipation for 4 months, dysuria, sensation of incomplete voiding, increased frequency, and dribbling for 10–12 days. There was no history of recent weight loss or rectal bleeding. His constipation progressed to obstipation just prior to admission.
Physical examination revealed mild tenderness on deep palpation in the right iliac fossa. Digital rectal examination suggested an 8cm x 6.5cm, firm, tender, immobile extra-rectal mass compressing the rectum. The overlying mucosa seemed free.
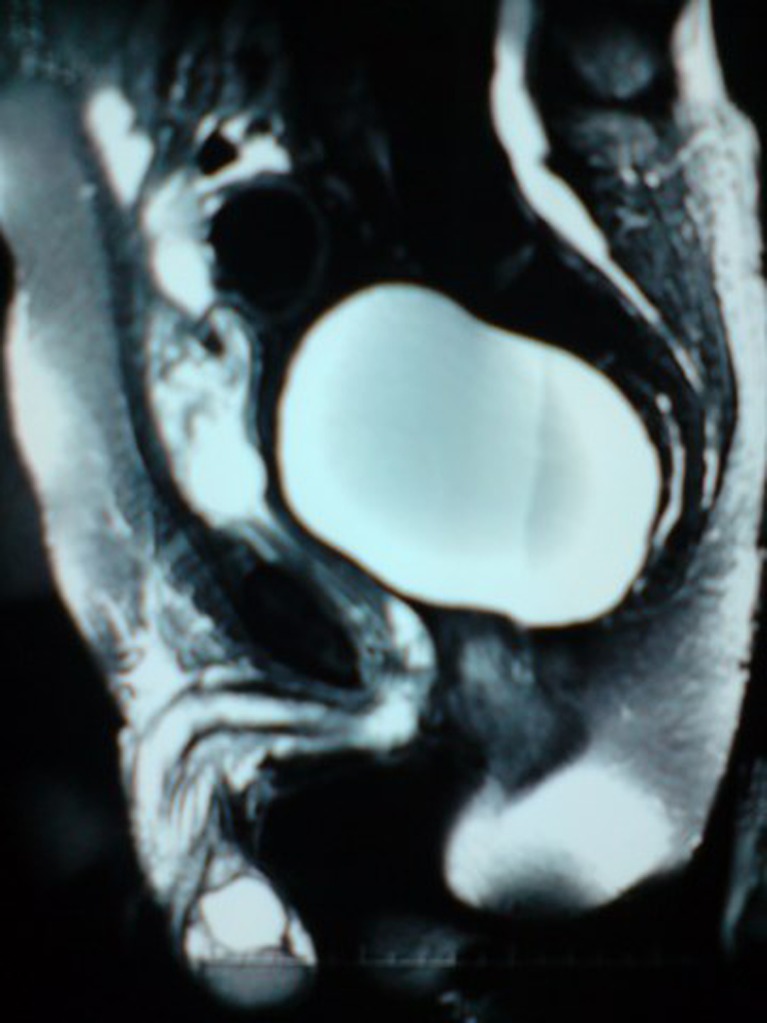
Contrast tomography of the abdomen was suggestive of a pelvic cyst posterior to the urinary bladder and anterior to the sacrum and coccyx displacing the rectum and anal canal to the left. MRI showed a large, ovoid, well defined collection measuring 10cm (CC) x 8.2cm (T) x 11cm (AP) posterior to the urinary bladder (Fig. 1). The contents of the collection appeared hemorrhagic and a layering effect was seen in the posterior aspect of the collection. The urinary bladder was found to be displaced anteriorly. The collection was in close apposition to the right rectal wall (perirectal region), displacing it to the left.
Fig. 1.
MRI Picture showing a large, ovoid, well defined collection measuring 10 cms [CC] x 8.2 cm [T] x 11 cm [AP] displacing the urinary bladder anteriorly
With the provisional diagnoses of a tail gut cyst, rectal duplication cyst and a rectal hamartoma, the patient underwent laparoscopic sigmoid mobilization, laparotomy and excision of the pelvic cyst. Operative findings included (Fig. 2):
10 × 15 cm cystic globular mass in the right pararectal region extending till the pelvic floor.
800ml of dark green odourless fluid drained from the cyst.
Dense adhesions between the cyst and the neighboring rectum and sigmoid colon.
No communication between the rectum and the cyst.
Fig. 2.

Intra-operative picture showing a 10 x 15 cm cystic, globular mass in the right para-rectal region
Discussion
Embryology and Clinical Features
Tail gut cysts arise due to the persistence of the postanal gut which usually regresses by the eighth week of development. Symptoms include bleeding and pain on defecation, lower abdominal and back pain and occasionally genitourinary obstructive symptoms. Tailgut cysts are predominantly retrorectal but varied positions like prerectal, perirenal and perianal have been reported [1].
Malignancy
There are p53 gene mutations similar to colonic adenocarcinoma. Tumor markers shown to be positive for tailgut cyst adenocarcinomas are CEA and CA19.9 and these markers have a valuable role in the monitoring of tumor recurrence and response to treatment [2].
Diagnosis
Transrectal ultrasound, can precisely locate the cyst as well as delineate the integrity of the rectal walls and rule out the presence of invasion. CT shows a thin walled, well-circumscribed mass with septations, with or without calcifications and signs of local inflammation. MRI is said to be more sensitive than CT at differentiating unilocular and multilocular masses. The wall and septae are found to enhance with contrast. A definitive diagnosis rests only on the specimen obtained from surgical resection. On histopathology, the cyst walls have been said to be lined with a variety of epithelia. Scattered bundles of smooth muscle fibres are usually present in cyst walls separated from the epithelium by a thin layer of fibrous tissue [3].
Management
Surgical resection, regarded as the mainstay of treatment, provides a definitive diagnosis, relieves symptoms, prevents subsequent infection as well as circumvents malignant transformation [4].
Contributor Information
Viju Joseph Abraham, Phone: +91-9872208382.
Mark Peacock, Phone: +91-9815277792.
Kim J. Mammen, Phone: +91-9814034185, Email: kjmammen@gmail.com
References
- 1.Jang SH, Jang KS, Song YS, Min KW, Han HX, Lee KG, Paik SS. Unusual prerectal location of a tailgut cyst: a case report. World J Gastroenterol. 2006;12(31):5081–5083. doi: 10.3748/wjg.v12.i31.5081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gonul II, Baglan T, Pala I, Mentes B. Tailgut cysts: diagnostic challenge for both pathologists and clinicians. Int J Colorectal Dis. 2007;22:1283–1285. doi: 10.1007/s00384-006-0153-2. [DOI] [PubMed] [Google Scholar]
- 3.Liang JJ, Alrawi S, Fuller GN, Tan D. Carcinoid tumors arising in tailgut cysts may be associated with estrogen receptor status: case report and review of the literature. Int J Clin Exp Pathol. 2008;1:539–543. [PMC free article] [PubMed] [Google Scholar]
- 4.Au E, Anderson O, Morgan B, Alarcon L, George ML. Tailgut cysts: report of two cases. Int J Colorectal Dis. 2009;24:345–350. doi: 10.1007/s00384-008-0598-6. [DOI] [PubMed] [Google Scholar]