Abstract:
Fungus cerebri is a relatively rare disease. The various reasons attributed to such pathology are, long standing mastoiditis, previous temporal lobe fracture, spontaneous herniation and most important common cause is post operative to mastoidectomy. The diagnosis is mainly clinical and supplemented by imaging studies. The commonly herniated part is the temporal lobe, but cerebellar herniation are also reported Different surgical modalities are used in managing this condition. Surgical approaches in the treatment of brain herniation into the mastoid or middle ear are, neurosurgical, otosurgical and combined. A case of fungus cerebri complicating mastoidectomy is presented and the pathogenesis is discussed
Keywords: Brain fungus, Fungus cerebri, Masoidectomy
Introduction
Fungus cerebri is protrusion of brain and dura out of the cranial cavity into the mastoid and middle ear. Fungus cerebri or cerebral herniation is a rare complication of modern otology. Earlier, it used to occur when a brain abscess complicating mastoiditis was drained through a mastoidectomy. In these cases the cerebral or cerebellar herniation developed either behind the ear or in the external auditory meatus, depending on the approach to the mastoid. The threat of this complication was an important factor for advocating the drainage of a brain abscess associated with mastoiditis through a clean, separate, burr hole rather than via the mastoid cavity [1]. Caboche first described the herniation of brain into the temporal bone in the French literature in 1902. Since then, a variety of terms such as brain hernia, brain fungus, brain prolapse, cerebral hernia, fungus cerebri, meningoencephalocoele or encephalocoele have evolved to describe this pathology [2]. Due to its declining incidence, the diagnosis may be delayed and result in the development of serious complications such as cerebrospinal fluid leak, meningitis, epidural or subdural abscess. Dural herniation and encephalocoele are uncommon entities that are encountered in less than 1 % of revision otologic operations [3]. The predisposing factors include: prior ear surgery such as mastoidectomy (radical or modified radical), meningitis, cholesteatoma and active chronic otitis media. Defect in the tegmen tympani and or tegmen antri are the most common sites of occurrence [4]. This condition develops as a sequel to defects in duraand skull combining with any of the forms of brains welling or increased intracranial pressure, or both. The brain protrudes through the dural opening into the mastoid cavity and may present at the scalp incision. The herniation may be accompanied by a leakage of cerebrospinal fluid(CSF).Management consists of wide surgical exposure, amputation of necrotic, herniated brain tissue, watertight dural closure, and closure in layers of the overlying soft tissues. The underlying cause of the increased intracranial pressure needs to be removed [1].
Case Report
On 15 February 2012 a 14-year-old male patient presented with complaint of right ear discharge and decreased hearing–6 years, mass in right ear- 1 year, with history of right ear surgery (modified radical mastoidectomy) performed one year back under general anaesthesia. Postoperatively the patient had high grade fever for 3 days with vomiting. He had dry ear for about a month post operatively when patient had discharge, intermittent, scanty, occasionally blood stained and mass in right ear canal. When the child was admitted to the ENT Department, patient was afebrile, pulse and blood pressure were normal
Examination of the right ear revealed evidence of modified radical mastoidectomy (post aural scar) with a pink, nonpulsatile, soft, insensitive mass, which did not bleed on touch filling the external auditory canal (Fig. 2) with mucopurulent discharge. There was no sign suggestive of intracranial complication. Patient had right ear conductive deafness on tuning fork tests with negative fistula test. The left ear was normal. Bilateral facial nerve were intact. Rest of the E.N.T. and head-neck examination was normal. Pure tone audiometry showed moderate- severe conductive hearing loss right ear. Radiographical examination CECT right temporal bone with 2 mm contiguous axial and 3 mm coronal sections of the temporal fossa and posterior fossa region before and after I/V contrast administration was suggestive of heterogeneously enhancing mass involving the right EAC, middle ear and mastoid part of temporal bone with destruction of tegmen tympani, and middle ear ossicle (Fig. 1a, b). Biopsy of the mass showed chronic inflammation. Multiplanar MR imaging (MRI) of the cranium was done on a 1.5 Tesla magnet using a dedicated head coil. T1, T2 weighted images were obtained in axial, sagittal and coronal planes using SE & GE sequences. Post Gadolinium enhanced T1 weighted images were subsequently acquired–T2 weighted axial and sagittal images demonstrate evidence of a heterogeneous signal intensity in the EAC and middle ear on the right side. Middle ear ossicles were not seen. There was evidence of defect in the tegmen tympani through which temporal lobe was seen bulging. Hence, a diagnosis of Fungus cerebri was made. The sequence of events was surmised to be as follows: post operative the patient developed otogenic meningitis which increased intracranial pressure and the dural defect (probablya surgical error), resulted in herniation i.e. Fungus cerebri (Brain fungus).
Fig. 2.

Mass filling EAC (right side)
Fig. 1.
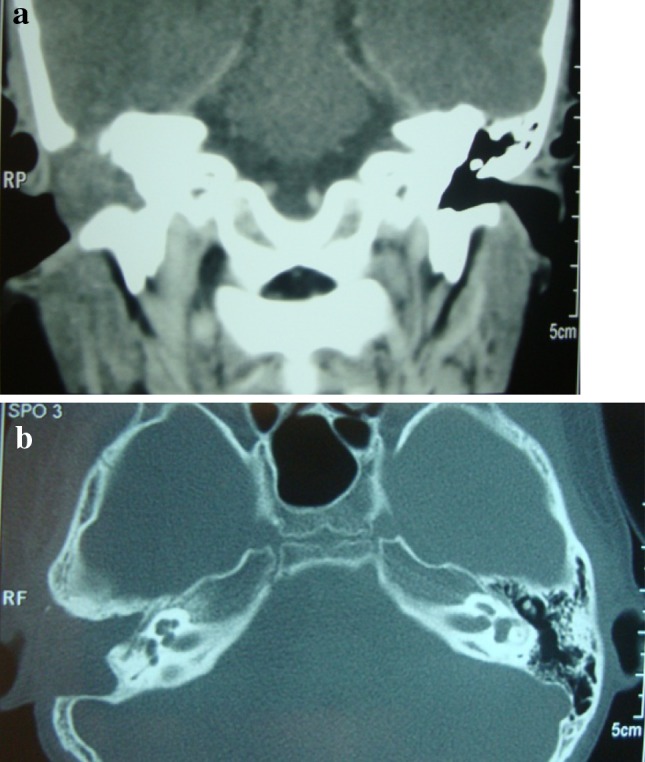
a CT scan coronalsection showing brain herniation through tegmen tympani (right side). b CT scan axial section showing brain herniation through tegmen tympani (right side)
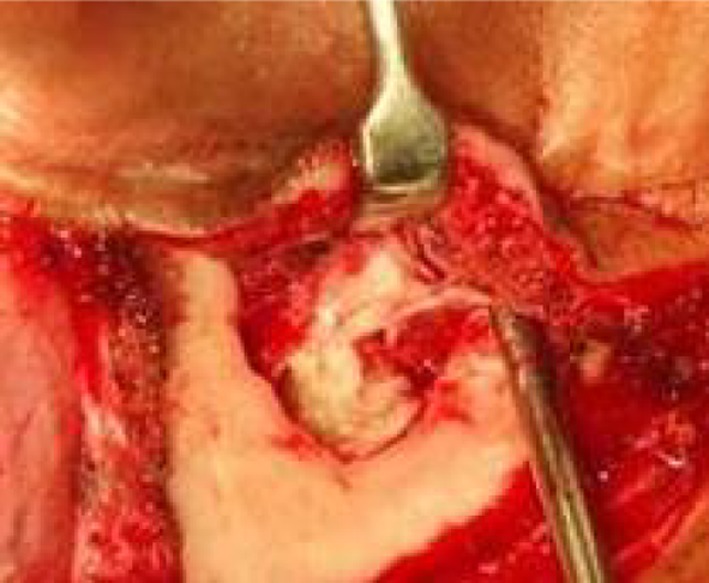
Patient was taken up for surgery after informed consent under general anaesthesia by transmastoid postaural approach. Mastoid cavity and middle ear were found to be filled with cholesteatoma, medial to EAC mass (Figs. 3, 4). Brain tissue (pulsatile and compressible) along with meninges was seen herniating from the tegen tympani defect (2 × 1.5 cm size) filling the EAC (Fig. 2). Cholesteatoma sac was removed from mastoid cavity and middle ear, ossicles were missing. Dura adherent to the meatal skin, was separated, without damaging the dura. Herniating brain tissue was cauterized at site of herniation using bipolar cautery (Fig. 5). Tegmen defect was sealed using temporalis facia graft and auto calvarial bone graft (Fig. 6a, b). Palisade was formed over the stapes footplate and sealed with temporalis facia; with wide meatoplasty. Post operative period was uneventful patient made a successful recovery and was discharged on 4th day of surgery. The canal pack was removed on 10th day. Histopathology of excised tissue came as glial tissue. Patient is symptom free without recurrence on 6 months of follow up.
Fig. 3.
Cholesteatoma medial to herniated brain in mastoid cavity and middle ear (right side)
Fig. 4.

Brain fungus in EAC, through defect in tegmen tympani (right side)
Fig. 5.

Herniated brain tissue after removal with bipolar cautery (right side)
Fig. 6.

a Site for auto calvarial graft. b Tegmen tympani defect sealed with temporalis fascia and auto calvarial graft (right side)
Discussion
Not many cases have been reported of herniation of Dura (meningocoele) and/or Brain, (meningoencephlocoele), into the mastoid and the middle ear. The aetiological factors are felt to be, chronic otomastoiditis, congenital dehiscence, fracture of skull base, spontaneous and most common, post mastoidectomy surgery. In the study by Spiros Manolidis, the predisposing factors for dural herniation include: prior ear surgery such as mastoidectomy (radical or modified radical), meningitis, cholesteatoma and active chronic otitis media [2, 4]. Iatrogenic injuries incurred during radical and modified radical mastoidectomy account for more than 59 to 77 % of the causes of encephalocoele [2, 5]. Dural defect can be due to various causes such as spontaneous- congenital and idiopathic [6], traumatic [7], iatrogenic and inflammatory [8]. The most common site of the dural defect is the tegmen plate [4]. Herniations are classified as pedenculated or sessile. They are associated with infection, CSF leak, and neurological complications. They are also associated with otological problems such as hearing loss, and trapped squamous epithelium. The commonly herniated part is the temporal lobe, but cerebellar herniation are also reported. The cases and literature reported, support that, dural injury is necessary for herniation, and if the arachnoid remains intact, a meningoencephalocoele results. The potential of CSF leak into the ear and recurrent meningitis is common. If the arachnoid is not intact, an encephalocoele results which predominantly presents as a mass without a CSF leak. Diagnosis is based on a high index of suspicion and clinical evaluation. High resolution computed tomography and Magnetic resonance imaging (MRI) could be used as preoperative evaluation modalities to confirm the diagnosis and assess the extent of lesion [5]. Brain herniation into a post-mastoidectomy cavity is rare and can be radiologically confused with cholesteatoma on the high resolution CT scan. MRI is essential to differentiate between cholesteatoma, brain herniation and inflammatory tissue. Surgery is the primary modality of treatment and different techniques and approaches are described for the repair of dural defect. Surgical approaches in the treatment of brain herniation into the mastoid or middle ear are, neurological, otological and combined [6].
Otological—mainly transmastoid, done in very small defects. Cartilage, bone chips or temporalis fascia is used to repair the defect.
Neurological—by middle cranial fossa approach or temporoparietal craniotomy. Combined-advocated in very large herniation [9, 10].
The herniated brain tissue is non functional and is thus usually removed after shrinkage with diathermy [5, 11]. Various materials can be used to seal the defect in different combinations such as temporalis fascia, conchal cartilage, titanium mesh, cadaveric dura, muscle, bone, proplast, and fibrin glue [2].
Conclusion
Fungus cerebri occurs as a complication of mastoid surgery and is an entirely preventable complication if care is taken not to injure the dura with burrs or diathermy. High index of clinical suspicion is needed to diagnose this condition. Surgical management remains the mainstay and early diagnosis and intervention will prevent further complication.
References:
- 1.Gluckman J. Fungus cerebri: an unusual complication of mastoidectomy. S Afr Med J. 1975;49(46):1933–1934. [PubMed] [Google Scholar]
- 2.Jackson CG, Pappas DG Jr, Manolidis S, Glasscock ME, Von Doersten PG, Carl R Hampf CR, et al. Brain herniation into the middle ear and mastoid: concepts in diagnosis and surgical management. Am J Otolaryngol. 1997;18:198–206. [PubMed] [Google Scholar]
- 3.Ramalingam KK, RaviRamalingam, Sreenivasa Murthy TM, Chandrakala GR, UttamAgarwal An unusual case of brain fungus. Orissa J Otolaryngol Head & Neck Surg. 2007;1(1):42–43. [Google Scholar]
- 4.Kizilay A, AladagI, Cokkeser Y, Ozturan O (2002) Dural bone defects and encephalocele associated with chronic otitis media or its surgery. Kulak BurunBogazIhtisDerg Nov–Dec, 9 (6):403–9 [PubMed]
- 5.Aristequi M, Falcioni M, Saleh E, Taibah A, Russo A, Landolfi M, Sanna M. Meningoencephalic herniation into the middle ear: a report of 27 cases. Laryngoscope. 1995;105(5 Pt 1):512–518. doi: 10.1288/00005537-199505000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Fenstra L, Sanna M, Zini C. Surgical treatment of brain herniation. Am J Otolaryngol. 1985;6(4):311–315. [PubMed] [Google Scholar]
- 7.Kariyattil R, Muthukuttiparambil U. Traumatic acute brain herniation through the ear in a child. Sultan Qaboos Univ Med J. 2012;12(3):352–356. doi: 10.12816/0003150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Escada P, Vital JP, Capucho C, Lima C, da Silva JM, Penha RS. Meningoencephalic herniation into the middle ear. Rev Laryngol Otol Rhinol (Bord) 1999;120(1):47–52. [PubMed] [Google Scholar]
- 9.Soubere C, Langman AW. Combined mastoid/middle cranial fossa approach. Skull base Surg. 1998;8:185–189. doi: 10.1055/s-2008-1058181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iurato S, Ettorre GC, Selvini C. Brain herniation into the middle ear: two idiopathic cases treated by a combined intracranial-mastoid approach. Laryngoscope. 1989;99(9):950–954. doi: 10.1288/00005537-198909000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Lundy LB, Graham MD, Kartush JM, LaRouere MJ. Temporal bone encephalocele and cerebrospinal fluid leaks. Am J Otolaryngol. 1996;17(3):461–469. [PubMed] [Google Scholar]


