Abstract
The purpose of this study was to identify patients of vocal cord paralysis and to establish an etiological diagnosis. Patients with vocal cord paralysis have been followed prospectively at a tertiary referral center. 120 patients identified with vocal cord paralysis by laryngeal endoscopy were evaluated clinically, radiologically and pathologically to make an etiological diagnosis. Those patients in whom no cause was found, a CT scan from base of skull to thorax was done before labeling them as idiopathic. Most of the patients presented in 5th (26.67 %) and 6th (21.67 %) decade. Males out numbered females in the ratio 2.3:1.0. The most common symptom of vocal cord paralysis was change in voice (98.21 %). Bilateral vocal cord palsy was found in 6.67 % patients and unilateral vocal cord palsy was found in 93.33 % patients. Among patients of unilateral vocal cord paralysis left vocal cord was paralyzed in 69.64 % and right cord in 30.36 %. Malignant (34.16 %) causes accounted for largest number of patients followed by central (15.00 %) and idiopathic causes (14.16 %). VCP has got a variable etiology which varies with the laterality of the vocal cord involvement. Malignant causes predominated in our series, occurring in 34.16 %, followed by central and idiopathic causes.
Keywords: Vocal cord paralysis (VCP), Unilateral vocal cord paralysis (UVCP), Bilateral vocal cord paralysis (BVCP), Etiology
Introduction
Vocal cord paralysis (VCP) is a relatively common entity which usually results from a disease process of the vagus nerve or its recurrent laryngeal nerve branch. Although the clinical diagnosis is usually made readily by indirect laryngoscopy, the etiology is more evasive. The cause may be in thorax, neck or cranial cavity. The left recurrent laryngeal nerve branch is more frequently involved, because the longer course of the nerve creates additional vulnerability especially within the mediastinum [1]. Symptoms depend on whether the VCP is unilateral or bilateral. The main presenting symptom in UVCP is hoarseness of voice, the degree of which depends on the position of paralysed vocal cord [2, 3]. Other associated symptoms include weak voice, cough, aspiration and swallowing symptoms [4]. In patients of BVCP most common complaint is breathing difficulty followed by dysphonia and aspiration [5]. The purpose of this study was to identify patients of VCP and to establish an etiological diagnosis.
Materials and Methods
This study was conducted on patients in a tertiary care centre for 1 year. The diagnosis was made in all patients with indirect laryngoscopy or laryngeal endoscopy. Patients with less than 12 years of age or patients with laryngeal malignancies were excluded from the study. Patients selected for the study, after a detailed history and complete ENT, head, neck and systemic examination underwent relevant endoscopic, radiological, hematological, microbiological and pathological examination to make an etiological diagnosis of VCP. Those patients in whom no cause was found, a CT scan from base of skull to thorax was done before labeling them as idiopathic.
Observations
Out of all the patients attending ENT clinic from February 2008 to January 2009, 120 patients were diagnosed as having VCP. The age ranged from 12 to 90 years; mean age ± SD being 51 years ± 5.8. The highest incidence was found in the 5th (26.67 %) and 6th decade (21.67 %). The number of male and female patients were 84 (70 %) and 36 (30.00 %) respectively [M:F = 2.3:1.0]. For patients with UVCP the male to female ratio was 2.7:1.0 and for BVCP male to female ratio was 0.3:1.0. The rural population formed a larger part of our study group, with 75 (62.50 %) patients belonging to rural areas. Majority belonged to upper middle class (37) (30.83 %) and the least number of cases were in the upper class (10) (8.33 %). [As per Kuppuswamy [6] scale 2003]. In patients with UVCP, change in voice was the main complaint in 110 (98.21 %) patients followed by choking on liquids in 43 patients (38.39 %), difficulty in swallowing in 30 patients (26.78 %). However breathing difficulty was the most common complaint in 7 (87.50 %) patients of BVCP followed by dysphonia in 6 (75 %) patients. The duration of change in voice in study cases ranged from <1 week to 2 years with a mean duration of 3.5 months. Out of 14 patients who had a past history of surgery 11 (78.57 %) were post thyroidectomy and 2 (14.28 %) patients had undergone other surgical procedures of neck and only 1 (7.14 %) patient had a past history of chest surgery. BVCP was found in 8 (6.67 %) patients. UVCP was found in 112 (93.33 %) patients. In patients with UVCP 78 (69.64 %) patients had left and 34 (30.36 %) patients had right cord palsy. In most of the patients of UVCP the vocal cord was fixed in paramedian position (89.28 %) followed by intermediate position (6.26 %). In patients with BVCP also, the vocal cords were mostly (87.50 %) fixed in paramedian position. In our study the yield of various diagnostic tests was evaluated as per the formula (Yield = number of diagnosis divided by number of tests ordered). MRI was found to have the highest yield of 85.71 % followed by X ray chest (52.94 %), CT scan (31.81 %) and barium swallow (30 %) (Table 1).
Table 1.
Investigations
| Diagnostic tests | Tests ordered | Diagnosis achieved | Yield (%) |
|---|---|---|---|
| MRI scan | 14 | 12 | 85.71 |
| Chest X ray | 51 | 27 | 52.94 |
| Endoscopya | 53 | 17 | 32.07 |
| CT scanning | 22 | 7 | 31.81 |
| Barium swallow | 10 | 3 | 30.00 |
aBronchoscopy and upper gastrointestinal endoscopy (UGIE)
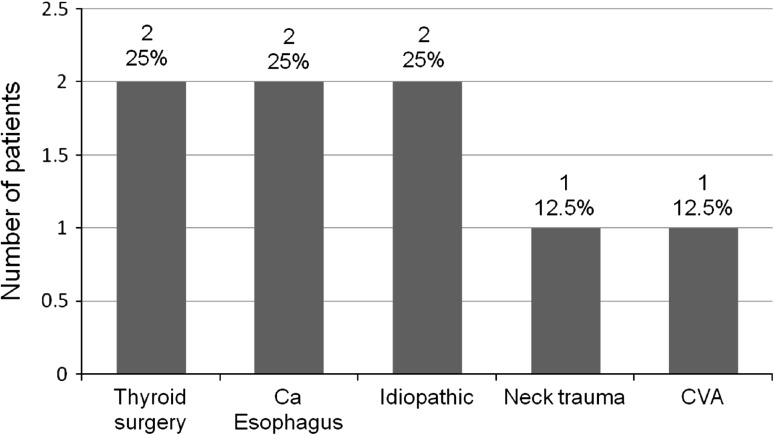
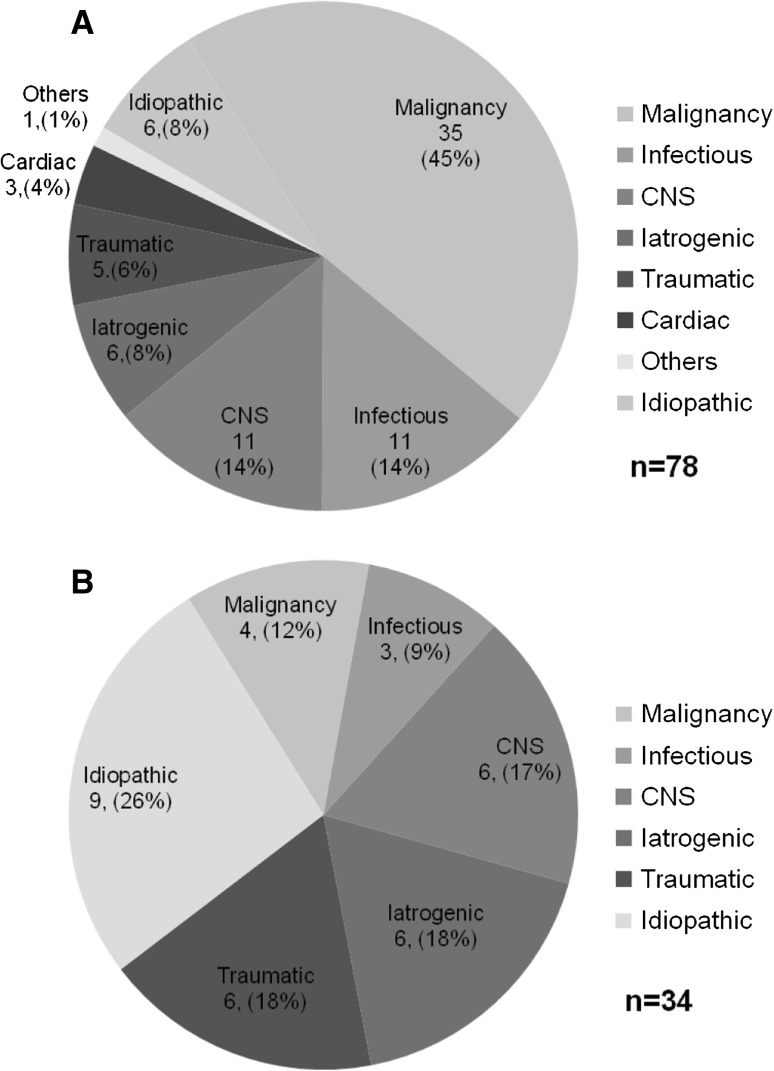
In 17 (14.16 %) patients no apparent cause for VCP was found and thus were grouped as idiopathic. Other etiological factors for UVCP and BVCP are shown in Figs. 1 and 2.
Fig. 1.
Etiology of BVCP (n = 8)
Fig. 2.
a Etiology of left side UVCP. b Etiology of right side UVCP
Discussion
Most of the patients were in the 5th (26.67 %) and 6th decade (21.67 %). The late presentation is due to increased incidence of cancer and cerebovascular accidents among elderly. Our results are in alliance with Merati [4], Havas [7] and Glazer [8] who reported the mean age as 53 years. Ahmed et al. [9] has also reported maximum number of patients in 5th and 6th decade. The male:female was 2.3:1.0. Among patients of UVCP male predominance was seen. The male preponderance could be explained by the fact that in our country, by and large, the attendance of the males in out patient department of hospitals for the treatment of voice complaints is much more than females. The higher prevalence of smoking amongst males also supports the higher male to female ratio. Our results are in accordance with the study of Nerurkar [10] (male:female = 2:1) from Mumbai, India. However in patients with BVCP the male to female ratio was reversed (M:F = 0.3:1). Other studies by Feehery [5] (males 48 %, females 52 %), Benninger [11] (males 52.1 % and females 47.9 %) have reported a much higher prevalence among males for BVCP. Our findings are similar to those reported by Holllinger [12] (male 27.5 %, and females 72.5 %).
In present study 25 % of patients of BVCP were post thyroidectomy as compared to only 8.04 % of post thyroidectomy cases of UVCP. Amongst patients of post thyroidectomy BVCP all the cases were females owing to high incidence of thyroid diseases in females. Most of the patients of UVCP presented with the complaint of change in voice (dysphonia) in 98.21 %. Amongst our patients of UVCP 78 patients (69.64 %) had left and 34 patients (30.36 %) had right side palsy. These findings were in accordance with Yumoto [13] and Ramadan [14]. The left side VCP is more common because left RLN is longer and more vulnerable to injury during its course of intrathoracic injury (Table 2).
Table 2.
Laterality of VCP in various studies
In most patients of UVCP the vocal cord was fixed in paramedian position (89.28 %) followed by intermediate (6.26 %) and median (4.46 %). In patients with BVCP also the vocal cords were mostly fixed in paramedian position (87.50 %).In a study by Siromptong [15] on patients with UVCP, the paralyzed cord was mostly fixed in paramedian position (81 %) followed by median in 12 % and cadaveric position in 7 %. Woodson [16] has proposed that the paramedian position was due to robust reinnervation of the thyroarytenoid muscle in patients with RLN injury.
Table 3 shows the distribution of the various causes of UVCP in few recent studies. Malignancy over all was responsible for VCP in 34.16 % of the patients’. 17.85 % of all UVCP were caused by bronchogenic carcinoma and 11.66 % due to carcinoma esophagus. In the above studies (Table 3) the incidence of malignancy varied from 14 to 30 %. Our study has higher incidence of malignancy than others. The consumption of tobacco and its products is more in this part of the country, contributing as an etiological factor for malignant cases. Surgical causes accounted for 10.71 % compared with 44.27 % of the cases in the study by Nerurkar [10]. In the study by Nerurkar [10] surgical trauma was the main cause of paralysis in 38 (44.27 %) cases out of these 11 (28.95 %) cases were post thyroidectomy and most of them had been referred from other centers for hoarseness of voice and management for the same. With apparent decline of thyroidectomy as the major cause of surgical VCP, other surgical procedures are emerging as causative factors. The proportion of these non thyroid surgical procedures causing VCP has increased from 19 % (3 % overall cases) published in 1970 by Parnell [1] to 85 % (40.47 % overall cases) in a study by Merati [4]. In our study non thyroid procedures accounted for 21.42 % of all surgical causes for VCP (overall 2.5 % of cases). These differences can be explained because such non thyroid surgeries risking vagus or RLN are not preformed very commonly in our institute. Paralysis following trauma is frequently observed. In this series there were 12 (10 %) cases in which trauma was causative factor for VCP. Incidence of traumatic UVCP has been reported between 19 % [11] to 2 % [17]. Our results are in accordance with Terris [18] who found an incidence of 8 % for UVCP. For traumatic BVCP Feehery [5] reported an incidence of 32.6 % from Henry ford hospital and 26.7 % from Jefferson hospital. Tucker et al. [19] and Maisel [20] reported an incidence of 30 and 31.50 % respectively. The incidence of traumatic BVCP in our study (12.5 %) is less as compared to previous studies, possibly due to small sample size of the patients with BVCP. Idiopathic etiologies, by definition have no obvious cause. The adequacy of the work up also determines the incidence of idiopathic causes. This may explain a high incidence of idiopathic etiology in earlier series. Improved imaging, fiberoptic endoscopy have decreased the incidence of so called “idiopathic paralysis” from 29 to 11 % [21, 22]. Our incidence of idiopathic VCP (14.16 %) was also within the same range. Conversely for UVCP, the incidence (13.39 %) was lower than BVCP (25 %). The incidence of idiopathic BVCP is more erratic than for UVCP. In 1973 Bulteau [23] reported a highest incidence of 50 %; just a year later Maisel [20] reported the lowest incidence literature of 3.7 %. Such differences may be partly ascribed to the criteria used for diagnosis.
Table 3.
UVCP etiology
| Etiology | Nerurkar [10] (%) | Chen [21] (%) | Laura [26] (%) | Present study 2009 (%) |
|---|---|---|---|---|
| Malignancy | 14.12 | 29.90 | 18.40 | 34.82 |
| Surgical | 44.27 | 40.20 | 36.50 | 10.71 |
| Trauma | 11.76 | 08.40 | 06.10 | 09.82 |
| Idiopathic | 16.47 | 10.70 | 18.50 | 13.39 |
| CNS | 04.71 | 03.80 | 05.10 | 15.17 |
| Infectious | 08.24 | 00.00 | 02.00 | 12.50 |
| Other | 00.00 | 07.40 | 11.20 | 03.57 |
Conclusion
VCP has got a variable etiology which varies with the laterality of the vocal cord involvement. Malignant causes predominated in our series, occurring in 34.16 % of the total, followed by central and idiopathic causes.
References
- 1.Myssiorek D. Recurrent laryngeal nerve paralysis: anatomy and etiology. Otolaryngol Clin N Am. 2004;37:25–44. doi: 10.1016/S0030-6665(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 2.Tucker HM. Vocal cord paralysis etiology and management. Laryngoscope. 1980;90:585–590. doi: 10.1288/00005537-198004000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Titche LL. Causes of recurrent laryngeal nerve paralysis. Arch Otolaryngol. 1976;102:259–261. doi: 10.1001/archotol.1976.00780100045002. [DOI] [PubMed] [Google Scholar]
- 4.Merati AL, Shermirani N, Smith TL, Toohill RJ. Changing trends in the nature of vocal fold impairment. Am J Otolaryngol Head Neck Med Surg. 2006;27:106–108. doi: 10.1016/j.amjoto.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Feehery JM, Pribitkin EA, Heffelfinger RN, Lacombe VG, Lee D, Lowry LD, Keane WM, Sataloff RT. The evolving etiology of bilateral vocal fold immobility. J Voice. 2003;17(1):76–81. doi: 10.1016/S0892-1997(03)00030-4. [DOI] [PubMed] [Google Scholar]
- 6.Mishra D, Singh HP. Kuppuswamy’s socioeconomic status scale a revision. Indian J Pediatr. 2003;70(3):273–274. doi: 10.1007/BF02725598. [DOI] [PubMed] [Google Scholar]
- 7.Havas T, Lowinger D, Priestly J. Unilateral vocal fold paralysis: causes, options and outcomes. Aust NZ J Surg. 1999;69:509–513. doi: 10.1046/j.1440-1622.1999.01613.x. [DOI] [PubMed] [Google Scholar]
- 8.Glazer HS. Extralaryngeal causes of vocal cord paralysis: CT evaluation. Am J Radiol. 1983;141:527–531. doi: 10.2214/ajr.141.3.527. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad S, Ajaz M, lateef M. A study of incidence and etiopathology of vocal cord paralysis. Indian J Otolaryngol Head Neck Surg. 2002;54:294–296. doi: 10.1007/BF02993746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nerukar N, Tandon S, Kiran K, Joshi A, Gharat P, Bradoo R. Unilateral vocal fold paralysis: an Indian scenario. Bombay Hosp J. 2006;48(4):561–567. [Google Scholar]
- 11.Beninger MS, Gillen JB, Altmann JS. The changing etiology of vocal fold immobility. Laryngoscope. 1998;108:1346–1350. doi: 10.1097/00005537-199809000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Holinger LD, Holinger PC, Holinger PH. Etiology of bilateral abductor vocal cord paralysis. A review of 389 cases. Ann Otol. 1976;85:428–436. doi: 10.1177/000348947608500402. [DOI] [PubMed] [Google Scholar]
- 13.Yumoto E, Minoda R, Hyodo M, Yamagata T. Causes of recurrent laryngeal nerve paralysis. Auris Nausus Larynx. 2002;29:41–45. doi: 10.1016/S0385-8146(01)00122-5. [DOI] [PubMed] [Google Scholar]
- 14.Ramadan HH, Wax MK, Avery S. Outcome and changing cause of UVCP. Otolaryngol Head Neck Surg. 1998;118:199–200. doi: 10.1016/S0194-5998(98)80014-4. [DOI] [PubMed] [Google Scholar]
- 15.Srirompotong S, Sea-Seow P, Srirompotong S. The cause and evaluation of UVCP. J Med Assoc Thai. 2001;84:855–858. [PubMed] [Google Scholar]
- 16.Woodson G. Evolving concepts of laryngeal paralysis. J Laryngol Otol. 2008;122:437–441. doi: 10.1017/S002221510700045X. [DOI] [PubMed] [Google Scholar]
- 17.Willatt DJ, Stell PM. The prognosis and management of idiopathic vocal cord paralysis. Clin Otolaryngol. 1989;14:247–250. doi: 10.1111/j.1365-2273.1989.tb00369.x. [DOI] [PubMed] [Google Scholar]
- 18.Terris DJ, Arnstein DP, Nguyen HH. Contemporary evaluation of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 1992;107:84–90. doi: 10.1177/019459989210700113. [DOI] [PubMed] [Google Scholar]
- 19.Tucker HM. Vocal cord paralysis-1979: aetiology and management. Laryngoscope. 1980;90:585–590. doi: 10.1288/00005537-198004000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Maisel RH, Ogura JH. Evaluation and treatment of vocal cord paralysis. Laryngoscope. 1974;84:302–316. doi: 10.1288/00005537-197402000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Chen HC, Jen YM, Wang CH, Lee JC, Lin YS. Aetiology of vocal cord paralysis. ORL J Otorhinolaryngol Relat Spec. 2007;69:167–171. doi: 10.1159/000099226. [DOI] [PubMed] [Google Scholar]
- 22.Huppler EG, et al. Causes of vocal cord paralysis. Proc Staff Meet Mayo Clin. 1955;30:578–579. [PubMed] [Google Scholar]
- 23.Bulteau V. The aetiology of bilateral recurrent laryngeal nerve paralysis. Med J Aust. 1973;2:776–777. [PubMed] [Google Scholar]
- 24.Parnell FW, Barndenburg JH. Vocal cord paralysis: a review of 100 cases. Laryngoscope. 1970;80(7):1036–1045. doi: 10.1288/00005537-197007000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Leder SB, Ross DA. Incidence of vocal fold immobility in patients with dysphagia. Dysphagia. Spring. 2005;20(2):168–169. doi: 10.1007/s00455-005-0003-3. [DOI] [PubMed] [Google Scholar]
- 26.Laura H, Rosenthal S, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of aetiology over 20 years. Laryngoscope. 2007;117:1864–1870. doi: 10.1097/MLG.0b013e3180de4d49. [DOI] [PubMed] [Google Scholar]