Abstract
To examine the incidence of haemorrhage following tonsillectomy, to explore the usefulness of antibiotic in preventing postoperative haemorrhage and to examine if the haemorrhage depended on the level of expertise of the surgeon. A retrospective review analysing tonsillectomy method, the rate secondary haemorrhage, the grade of operating surgeon. A χ2 analysis was used to determine the statistical difference between the haemorrhage rates of different tonsillectomy methods. One thousand three hundred and thirty-six tonsillectomies were performed during this period by four different methods: 615 by cold steel dissection, 582 by Coblation, 32 by bipolar dissection and 107 by Helica thermal coagulation. 621 tonsillectomies were performed by Consultant grade and middle grades performed 693 operations. 124 patients (9.3 %) were readmitted with haemorrhage. The secondary haemorrhage requiring surgery for controlling bleeding for cold steel dissection method was 1.5 % compared to 6.7 % for coblation method (P < 0.01 %), 6.3 % for bipolar dissection and 1.9 % for Helica thermal coagulation method. Overall consultants had a post tonsillectomy haemorrhage rate of 5.5 % and middle grades had a rate of 3.7 %. 86.5 % of the patients were already on routine prophylactic oral antibiotics at the time of presentation with haemorrhage needing surgical arrest and 13.5 % were not on antibiotics (P < 0.05 %). There was statistically significant difference in secondary haemorrhage rate between coblation and cold steel dissection methods. Coblation tonsillectomies had an increased need for operative intervention to control secondary haemorrhage. Routine use of antibiotic and expertise of operating surgeon had no bearing on secondary haemorrhage rate.
Keywords: Coblation, Tonsillectomy, Haemorrhage, Helica thermal coagulator
Introduction
Despite strict guidelines for its indication, tonsillectomy still seems to be the frequently performed procedure in an otorhinolaryngology unit. Since the first description of tonsillectomy by Celsus about 2,000 years ago [1], many new techniques have been explored to refine the art of tonsillectomy mainly in the operative speed and achieving haemostasis. The newer techniques include laser [2], microdebridor [3], bipolar cautery [4], ultrasonic [5], coblator [6, 7, 8], are some of the modalities described in the recent English literature. Coblation [6] employs lower temperatures of approximately 60 °C hence expected to cause less collateral damage than standard bipolar diathermy. Helica thermal coagulator is an instrument that combines Helium gas with low AC electrical power. The operational power (4–6 W) is much lower than conventional diathermy. The diathermy ionises helium gas causing tissue fulguration similar to an argon beam coagulator [9]. Low levels of power causes less damage to surrounding tissues and the reported depth of penetration is less than 1.5 mm [10]. In our hospital, apart from cold steel dissection, coblation and Helica methods are routinely used for tonsillectomy.
We report a retrospective analysis of 60 months of tonsillectomy performed on both children and adults in our hospital.
Materials and Methods
This retrospective audit was carried-out at the Princess Royal University Teaching hospital, Farnborough. All patients undergoing tonsillectomy between June 2006 and June 2011, a total of 1,336 patients, were considered for the audit. The patient details were obtained from computer records using F34 as operative-code and all the case notes were individually verified for their accuracy and other data such as grade of surgeon, method of tonsillectomy, post-operative medication including routine post-operative antibiotic prescribed were recorded. Patients undergoing tonsillectomy as part of palatoplasty for snoring and unilateral tonsillectomy for biopsy to exclude malignancy were excluded from the study.
All patients undergoing tonsillectomy at the Princess Royal University Hospital admitted with secondary haemorrhage occurring after 24 h following surgery were included in the study. Those patients with ‘not significant’ haemorrhage seen in accident and emergency department (A & E) and discharged were excluded from the study. Secondary haemorrhage was classified into two groups: those patients requiring a return to theatre for controlling bleeding and those who were managed conservatively. Readmission data was obtained from A & E computer recording, junior doctors’ admission diary records (which are accurately recorded since June 2006) and verified for accuracy from patient’s case notes. Patients with secondary haemorrhage following tonsillectomy performed in other hospitals were excluded from the study. The data obtained were analysed using SPSS statistic software and statistical significance was set at P < 0.05.
Results
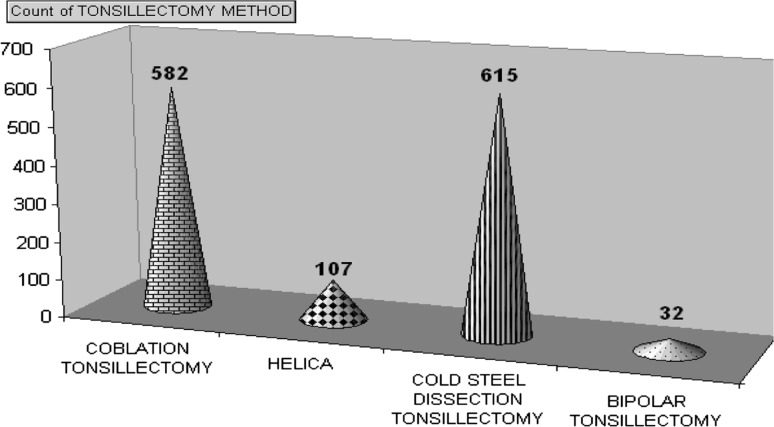
The study evaluated 1,336 tonsillectomies performed during the 60 month period. 783 (58.6 %) patients were female and 553 (41.4 %) were male patients. Mean age was 15.32 years (range 18 months to 85 years). 822 (61.5 %) were children and 514 (38.5 %) adults. Figure 1 shows the method of tonsillectomy.
Fig. 1.
Showing tonsillectomy methods used in past 60 months
Figure 1 shows the methods used for tonsillectomy; 582 patients (43.6 %) had coblation tonsillectomy, 615 (46 %) had cold steel tonsillectomy, Helica Thermal coagulator was performed on 107 (8 %) and bipolar tonsillectomy on 32 patients (2.4 %).
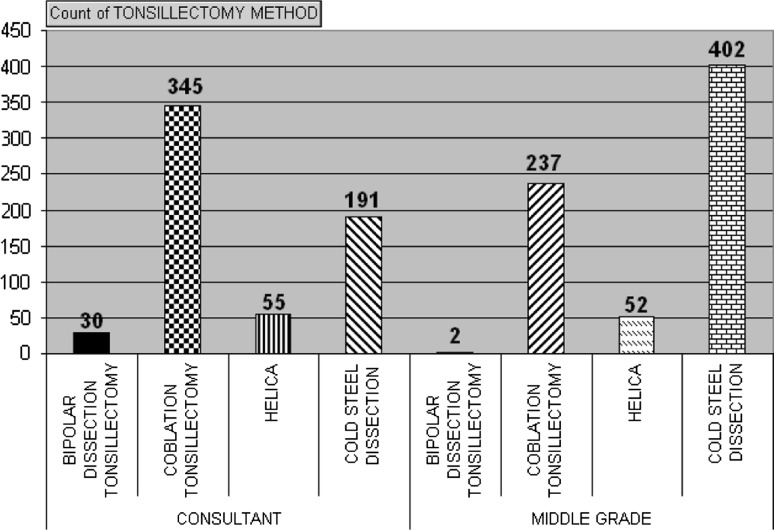
Figure 2 shows the method of tonsillectomy and the grade of surgeon. 693 (52 %) tonsillectomies were performed by middle grade surgeons, 621 (46.5 %) by consultants and 22 (1.6 %) by senior house officers (SHO).
Fig. 2.
Showing the grade of surgeon and method of tonsillectomy performed (operations performed by SHO’s are not shown because of limited number)
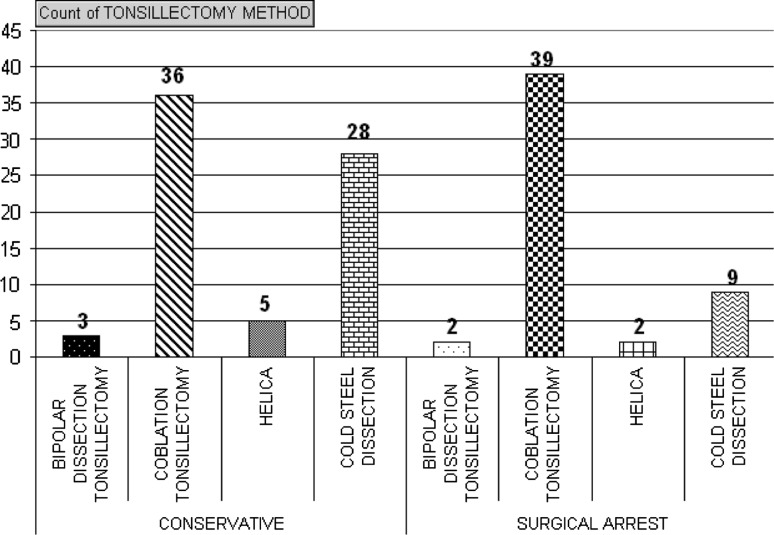
Secondary haemorrhage was classified into those which were managed conservatively and those needing surgical intervention to control the bleeding. 124 (9.3 %) were readmitted with secondary haemorrhage; 72 patients (5.4 %) were managed conservatively and 52 patients (3.9 %) needed surgical intervention to arrest secondary haemorrhage. Table 1 and Fig. 4 show method of tonsillectomy and the type of intervention for secondary haemorrhage.
Table 1.
Showing management of haemorrhage and different tonsillectomy methods
| Complications | Tonsillectomy method | Total |
|---|---|---|
| Conservatively managed | Bilateral dissection tonsillectomy | 28 |
| Bipolar dissection tonsillectomy | 3 | |
| Coblation tonsillectomy | 36 | |
| Helica | 5 | |
| Conservative total | 72 | |
| None | Bilateral dissection tonsillectomy | 578 |
| Bipolar dissection tonsillectomy | 27 | |
| Coblation tonsillectomy | 507 | |
| Helica | 100 | |
| None total | 1,212 | |
| Surgical intervention to arrest haemorrhage | Bilateral dissection tonsillectomy | 9 |
| Bipolar dissection tonsillectomy | 2 | |
| Coblation tonsillectomy | 39 | |
| Helica | 2 | |
| Surgical arrest total | 52 | |
| Grand total | 1,336 |
Fig. 4.
Showing secondary haemorrhage and management
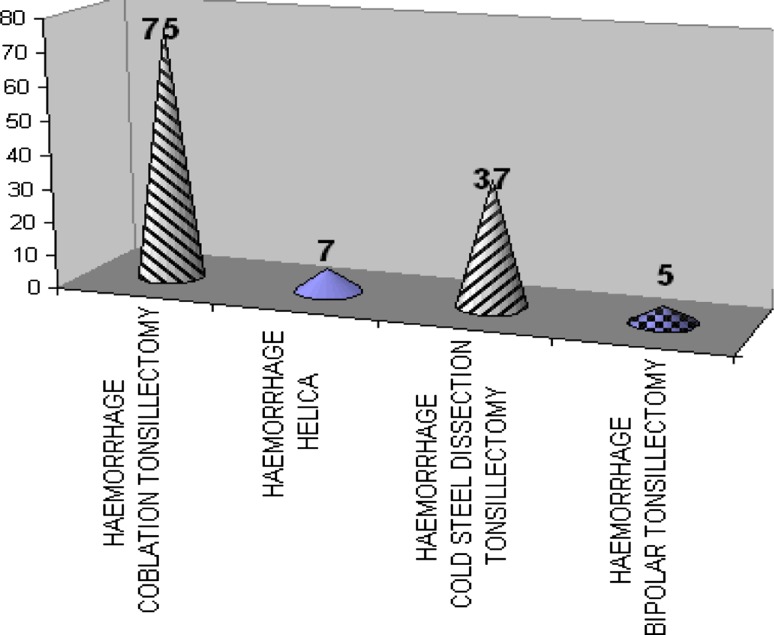
Out of 124 patients readmitted with secondary haemorrhage, 75 (60.8 %) had their tonsillectomy by coblation method, 37 (29.8 %) by cold steel dissection, 5 (4 %) by bipolar dissection and 7 (5.6 %) by Helica thermal coagulation as shown in Fig. 3.
Fig. 3.
Showing overall haemorrhage with three methods of tonsillectomy
Nine patients (1.5 %) who underwent dissection tonsillectomy needed return to theatre to control the haemorrhage where as thirty nine patients (6.7 %) who underwent coblation tonsillectomy needed surgical intervention to arrest the haemorrhage (Fig. 4; Table 1).
Twenty-eight of the 52 patients who needed surgical intervention to control secondary haemorrhage were children and 24 were adults.
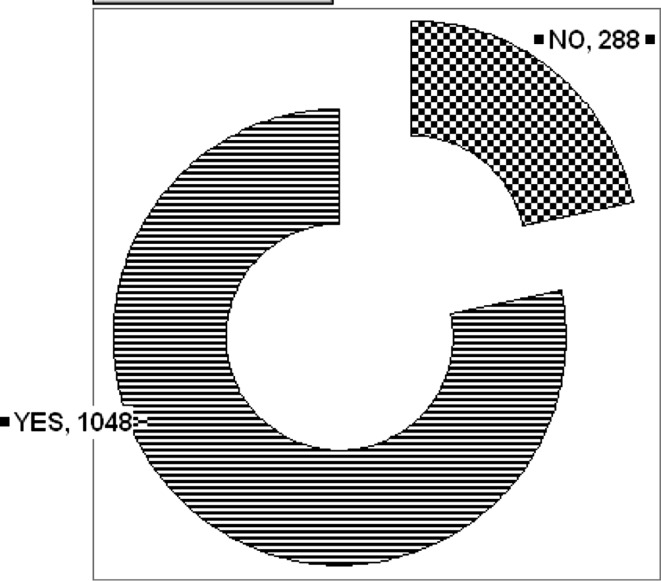
One thousand and forty-eight patients (78.4 %) were discharged on routine prophylactic antibiotics after tonsillectomy and 288 patients (21.6 %) did not have prophylactic antibiotics (Fig. 5). 105 patients (84.7 %) were already on prophylactic antibiotics when they presented with secondary haemorrhage (P < 0.01) and only nineteen patients (15.3 %) were not on routine prophylactic antibiotics. 45 patients (86.5 %) with secondary haemorrhage, were already on prophylactic antibiotics, needed surgical intervention to stem the haemorrhage where as seven (13.5 %) who were not on prophylactic antibiotic.
Fig. 5.
Number of patients on prophylactic antibiotic
Discussion
Despite strict guidelines regarding its’ indications, tonsillectomy is still one of the commonly performed operations especially on children. Until recently the cold steel dissection method has been the standard technique for tonsillectomy. To reduce the intra-operative and post-operative complications, several new techniques such as coblation, laser assisted, harmonic scalpel etc. have been described in the English literature for removal of tonsils.
The coblation technique uses bipolar radio-frequency waves to ablate the target tissue through a conductive saline solution. Coblation uses a bipolar electric system which melts the tissues at only 60 °C and has been around for almost a decade. It has been described for tonsillectomy by Timms and Temple [6]. The basic principle of this technique is passing of radiofrequency bipolar electric current through normal saline resulting in production of sodium ions which break intercellular bonds and melt tissues at low temperature [7]. The surface temperature reached ranges from 40 to 70 °C. Traditional cold steel dissection method uses sharp dissection with a tonsil snare, with or with out bipolar cautery or ligature for haemostasis. Helica-thermocoagulation is a British invention wherein Helium gets ionized when a bipolar current is passed through it. The ionised helium is used to dissect and coagulate the tissues [9].
Clark et al. [11] report a secondary haemorrhage rate of 1.5 % for coblation with no patients returning to theatre for controlling haemorrhage. They report that patients were discharged on oral antibiotics after 24 h of intravenous antibiotics when they presented with bleeding. Clark et al., in their retrospective audit, have not mentioned if patients were on antibiotics or not at the time of presentation. Neither have they mentioned if any bleeding patients were seen in neighbouring hospitals. In our study, we found that nearly 86 % of patients were already on oral antibiotics at the time of presentation with secondary haemorrhage. Belloso et al. [12] in their study report secondary haemorrhage rate of 2.25 % for coblation tonsillectomy compared to 6.19 % for cold dissection.
There are several reports which provide evidence for an increased secondary haemorrhage with coblation tonsillectomy. Amir et al. [13] report life threatening late secondary haemorrhage requiring blood transfusion with coblation tonsillectomies. Divi and Benninger [14] report a secondary haemorrhage rate of 5.4 % in their retrospective study for coblation tonsillectomy.
Windfuhr et al. [15] in their pilot study report a high rate of 9.5 % return to theatre for controlling haemorrhage following coblation tonsillectomy. Javed et al. [16] report a high incidence of secondary haemorrhage following coblation tonsillectomy in their initial audit which forced them to abandon the procedure. In their retrospective audit, they compared coblation with cold steel method and report that 9.1 % patients needed surgical intervention to control secondary haemorrhage. Noon and Hargreaves [17] report a high incidence of secondary haemorrhage following coblation method and have abandoned coblation in their unit. National Prospective Tonsillectomy Audit [18] report 3.6 % as secondary haemorrhage rate following tonsillectomy. In our study, return to theatre for coblation method was high at 6.3 % and overall secondary haemorrhage for coblation was even higher at 12.9 %.
Carney et al. [19] feel that there is a significant learning curve and report high levels of secondary haemorrhage in less experienced surgeons, this totally contrasts our study wherein we found high incidence of secondary haemorrhage in coblation tonsillectomy performed by experienced consultant surgeons compared to middle grades.
O’Reilly et al. [20], Lee et al. [21] found no evidence of reduced secondary haemorrhage rate following routine use of prophylactic antibiotics and question the justification of using prophylactic antibiotic routinely. Dhiwakar et al. [22] in their meta-analysis of ten studies in the Cochrane review found no significant reduction in post-tonsillectomy bleeding and the routine use of prophylactic antibiotic. We found no statistically significant evidence for the use of prophylactic antibiotics in reducing secondary haemorrhage.
Conclusion
This retrospective audit of tonsillectomies in our department has shown increased incidence of post tonsillectomy secondary haemorrhage following coblation tonsillectomy. The routine use of prophylactic antibiotics had no bearing on the rate of secondary haemorrhage. The experience level of the surgeons involved showed no bearing on post tonsillectomy secondary haemorrhage.
References
- 1.Younis RT, Lazar RH. History and current practice of tonsillectomy. Laryngoscope. 2002;112:3–5. doi: 10.1002/lary.5541121403. [DOI] [PubMed] [Google Scholar]
- 2.Martinez SA, Akin DP. Laser tonsillectomy and adenoidectomy. Otolaryngol Clin North Am. 1987;20:371–376. [PubMed] [Google Scholar]
- 3.Koltai PJ, Koltai CA, Mascha ET, et al. Intracapsular partial tonsillectomy for tonsillar hypertrophy in children. Laryngoscope. 2002;112(8):17–19. doi: 10.1097/00005537-200208001-00007. [DOI] [PubMed] [Google Scholar]
- 4.Andrea M. Microsurgical bipolar cautery tonsillectomy. Laryngoscope. 1993;103:1177–1178. doi: 10.1288/00005537-199310000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Weingarten C. Ultrasonic tonsillectomy. Otolaryngol Head Neck Surg. 1997;116:193–196. doi: 10.1016/S0194-5998(97)70324-3. [DOI] [PubMed] [Google Scholar]
- 6.Temple RH, Timms MS. Paediatric coblation tonsillectomy. Int J Paediatr Otolaryngol. 2001;61:195–198. doi: 10.1016/S0165-5876(01)00553-5. [DOI] [PubMed] [Google Scholar]
- 7.Timms MS, Temple RH. Coblation Tonsillectomy: a double blind randomised controlled study. J Laryngol Otol. 2002;116:450–452. doi: 10.1258/0022215021911031. [DOI] [PubMed] [Google Scholar]
- 8.Chang KW. Randomised controlled trail of coblation versus electro cautery. Otolaryngol Head Neck Surg. 2005;132:273–280. doi: 10.1016/j.otohns.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Sutton CJG. Power sources in endoscopic surgery. Curr Opin Obstet Gynaecol. 1995;7:248–256. doi: 10.1097/00001703-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Nduka C, Super P, Monson J, Darzi A. Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg. 1994;179:161–170. [PubMed] [Google Scholar]
- 11.Clark MPA, Smithard A, Jarvis P. How we do it: coblation tonsillectomy complication rates from a single ENT department compared with the National Prospective Tonsillectomy Audit. Clin Otolaryngol. 2006;31:156–159. doi: 10.1111/j.1749-4486.2006.01172.x. [DOI] [PubMed] [Google Scholar]
- 12.Belloso A, Timms MS. Coblation tonsillectomy versus dissection tonsillectomy: postoperative haemorrhage. Laryngoscope. 2003;113:2010–2013. doi: 10.1097/00005537-200311000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Amir J, Belloso A, Broomfield SJ, Morar P. Return to theatre in secondary post-tonsillectomy haemorrhage: a comparison of coblation and dissection techniques. Eur Arch Otorhinolaryngol. 2011;268(6):807–816. doi: 10.1007/s00405-011-1535-9. [DOI] [PubMed] [Google Scholar]
- 14.Divi V, Benninger M. Prospective tonsillectomy bleed: coblation versus non coblation. Laryngoscope. 2005;115:31–33. doi: 10.1097/01.mlg.0000150682.62517.0e. [DOI] [PubMed] [Google Scholar]
- 15.Windfuhr JP, Chen YS, Remmert S. Haemorrhage following coblation tonsillectomy. Ann Otol Rhinol Laryngol. 2005;114:749–756. doi: 10.1177/000348940511401003. [DOI] [PubMed] [Google Scholar]
- 16.Javed F, Sadri M, Uddin J, et al. A complete audit cycle on post tonsillectomy haemorrhage. Acta Otolaryngol. 2007;127:300–304. doi: 10.1080/00016480600895052. [DOI] [PubMed] [Google Scholar]
- 17.Noon AP, Hargreaves S. Increased post-operative haemorrhage seen in adult coblation tonsillectomy. J Laryngol Otol. 2003;117(9):704–706. doi: 10.1258/002221503322334521. [DOI] [PubMed] [Google Scholar]
- 18.Clinical Effectiveness Unit, Royal College, of Surgeons of England. National Prospective Tonsillectomy Audit. Report of an Audit in England and Northern Ireland between July 2003 and September 2004. Available at: http:/www.rcseng.ac.uk/services/publications/publications/pdf/ta-finalreport.pdf. Accessed 9 June 2011
- 19.Carney AS, Harris PK, MacFarlane PL, Nasser S, Esterman A. The coblation tonsillectomy learning curve. Otolaryngol Head Neck Surg. 2008;138:149–152. doi: 10.1016/j.otohns.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 20.O’Reilly BJ, Black S, Fernandes J, Panesar J. Is the routine use of antibiotics justified in adult tonsillectomy? J Laryngol Otol. 2003;117(5):382–385. doi: 10.1258/002221503321626429. [DOI] [PubMed] [Google Scholar]
- 21.Lee WC, Duignan MC, Walsh RM, McRae-Moore JR. An audit of prophylactic antibiotic treatment following tonsillectomy in children. J Laryngol Otol. 1996;110:357–359. doi: 10.1017/s0022215100133614. [DOI] [PubMed] [Google Scholar]
- 22.Dhiwakar M, Clement WA, Supriya M, McKerrow WS. Antibiotics to reduce post-tonsillectomy morbidity. Cochrane Database Syst Rev. 2010;7(7):CD005607. doi: 10.1002/14651858.CD005607.pub3. [DOI] [PubMed] [Google Scholar]