Abstract
Purpose
The aim of this study was to explore the operative technique and effectiveness of triangular osteosynthesis for vertically unstable sacral fractures.
Methods
From January 2009 to December 2010, 25 vertical unstable sacral fractures in 22 patients were treated with triangular osteosynthesis using the combination of universal spine system and iliosacral screw in our institution. Patients were followed up prospectively with routine post-operation visits for clinical and radiographic examination. The reduction quality was evaluated according to Matta criterion. Clinical function outcome, and nerve function outcome was evaluated by Majeed and Gibbons criterion.
Results
All patients were followed up for an average of 14 months (range 8–26 months). Local infection was seen in two patients, and both were healed with debridement and antibiotics. Patients experienced early weight-bearing ability, no fracture reduction loss, and hardware loosening, while all fractures appeared as bone union at the final follow-up. According to Matta criterion for fracture reduction, the results were excellent in 18 sides, good in 6 sides, and fair in 1 side. According to Majeed functional scoring at last follow-up, the results were excellent in 13 cases, good in 6 cases, fair in 2 cases, and poor in 1 case. Neurologic impairment was noted in 13 patients pre-operative, six patients achieved complete recovery, six patients achieved partial improvement, one patient did not have any improvement at the last follow-up.
Conclusion
Triangular osteosynthesis is a relatively new fixation for vertical unstable sacral fractures, the fixation is rigid, permits early full weight-bearing, and nerve decompression can be performed, which facilitates function recovery.
Keywords: Sacral fracture, Pelvic fracture, Triangular osteosynthesis, Spinal-pelvic fixation
Introduction
Sacral fractures often suffers from high-energy trauma: unstable sacral fractures occur in 17–30 % of patients with pelvic trauma [1, 2], and this type fractures represent severe injuries, often associated with a high mortality and morbidity due to pain and malunion [3, 4]. Non-operative treatment had been the first choice for these fractures historically, because of the lack of suitable technique and deficiency in implants. With the development of technique and proper fixation instruments, open or closed reduction and internal fixation have now been recognized as the gold standard for the treatment of these unstable fractures. Operative treatment should reconstruct the fracture anatomy, decompress the nerves, and achieve possibly early mobilization and weight-bearing. Kinds of internal fixation instruments that had been proposed to reconstruct the post pelvic ring include posterior small plates [5], percutaneous iliosacral screws [6, 7], transiliac bars [8–10], and sacral rods [11]. However, none of these fixation instruments can resist vertical shear forces, provide unrestricted weight-bearing, and secure mobilization after operation. Recent studies demonstrated that triangular osteosynthesis is a new option for the treatment of type C pelvic fracture following unstable sacral fractures [12–16]. This fixation combines a lumbopelvic distraction osteosynthesis and a transverse fixation, which provides multiplanar stability. This technique of sacral fracture stabilization facilitates early mobilization, reduces mortality, protects the local neuroanatomy from additional injury which may be caused by progressive deformity, and improves long-term outcomes [12]. The purpose of this article is to show the preliminary results of vertical unstable sacral fractures treated with triangular osteosynthesis.
Materials and methods
Patients
Between January 2009 and December 2010, 22 patients with vertical unstable sacral fractures were treated with triangular osteosynthesis using the combination of Universal Spinal System, USS (Synthes, Bochum, Germany) and iliosacral screw in our institution. There were 13 males and 9 females, with an average age of 30 years (range 21–48 years). The most common modes of injury were motor vehicle accidents (13 cases) and a fall from height (6 cases), with three cases reported being from crushing injuries. All patients combined anterior pelvic ring fractures. All but three patients had ramu fractures, while the remainder had either a symphyseal disruption alone or symphyseal disruption in combination with ramu fractures. 13 patients had neurologic deficits to some extent of the lumbosacral plexus or cauda equina. One had open fracture and four patients suffered internal degloving injuries located in the lumbosacral and flank region. 18 patients combined other fractures, three patients had cervical rib fractures and hemopneumothorax, two patients had bladder rupture, and three patients had brain injuries. Most of the patients had an X-ray trauma series (AP, inlet, and outlet of pelvis) and CT evaluation before operation (Fig. 1). Denis fracture classification was used for the fracture description. Tables 1 and 2 show the fracture distributions.
Fig. 1.
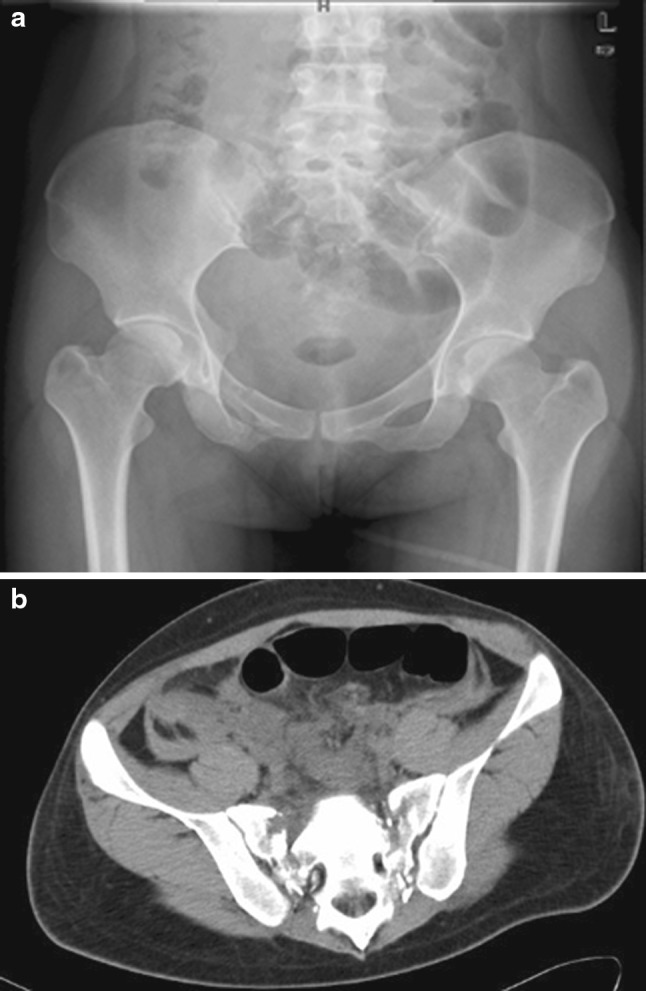
Pre-operative anteroposterior X-ray and CT scan demonstrating bilateral sacral fractures, the fractures being displaced tremendously
Table 1.
Unilateral sacral fractures
| Denis classification | Left side (amount) | Right side (amount) | Total (amount) |
|---|---|---|---|
| Type I | 0 | 3 | 3 |
| Type II | 6 | 4 | 10 |
| Type III | 2 | 1 | 3 |
Table 2.
Bilateral sacral fractures
| Number | Left side | Right side |
|---|---|---|
| 1 | Type I | Type III |
| 2 | Type III | Type III |
| 3 | Type II | Type I |
| 4 | Type III | Type III |
| 5 | Type I | Type III |
| 6 | Type II | Type II |
Operative technique
Patients were initially stabilized hemodynamically and then placed in skeletal traction for fracture reduction. Some bilateral sacral fractures can be temporary fixed with external fixation (Fig. 2). Operation was performed when the patient was stable both hemodynamically and physiologically. The patient was placed in a prone position. An image intensifier or navigation was used. A midline incision from L4 to S3 was made, and the thoracolumbar fascia was dissected approximately 2–2.5 cm lateral to the transverse processes. The intermuscular plane was developed between the erector spinae muscles and multifidus, and this plane leads directly onto the L4/5 facet joint and posterior–superior-iliac-spine (PSIS). The paraspinal muscles were then elevated from the dorsum of the sacrum and reflected medially to expose the sacral fracture and the sacral foramina. Care must be taken to avoid detaching the posterior SI ligaments: as in the case of a sacral fracture, the SI ligaments are intact. If pre-operative physical examination and CT scan confirmed neurologic deficits and sacral canal occlusion, then nerve decompression was performed; formal midline sacral laminectomy could be performed if necessary for decompression completely (Fig. 3). The spinopelvic fixation construct was applied by implanting 6.2-mm Schanz screws into the L5, S1 vertebral body, and a 7-mm Schanz screw into the ipsilateral ilium along the sciatic buttress. Connecting rods were inserted and tightened initially over the proximal pedicle screw of L5 and iliac screw; the screws were used as ‘‘joysticks’’ to achieve reduction. Vertical reduction was obtained using an AO distractor over the pedicle screws, and horizontal reduction was achieved through pelvic reduction clamp. After reducing the displaced fractures satisfactory, iliosacral screw was placed percutaneously initially. In this group, only one IS screw was implanted. Then, the USS connecting rod was locked. For these slightly displaced sacral fractures, which can be reduced by pre-operative traction, the L5/S1 joint capsule was intact, and pre-operative physical examination and CT scan confirmed that there is no need to do nerve decompression. Triangular osteosynthesis can be performed through minimally invasive surgery, for which only S1 pedicle screw and iliac screw are needed, and which can be placed percutaneously. In this group, three patients were treated through this technique. C-arm fluoroscopic X-ray trauma series (AP, inlet, and outlet of pelvis) were used for the confirmation of reduction and placement of implants intraoperative. The surgical wound was closed on two suction drains after copious irrigation. After triangular fixation for the posterior ring, most cases of wide rami displacement or symphyseal diastasis can be reduced spontaneously, and we do not have to deal with it anymore. In this group, only four cases were stabilized with plates (Fig. 4).
Fig. 2.
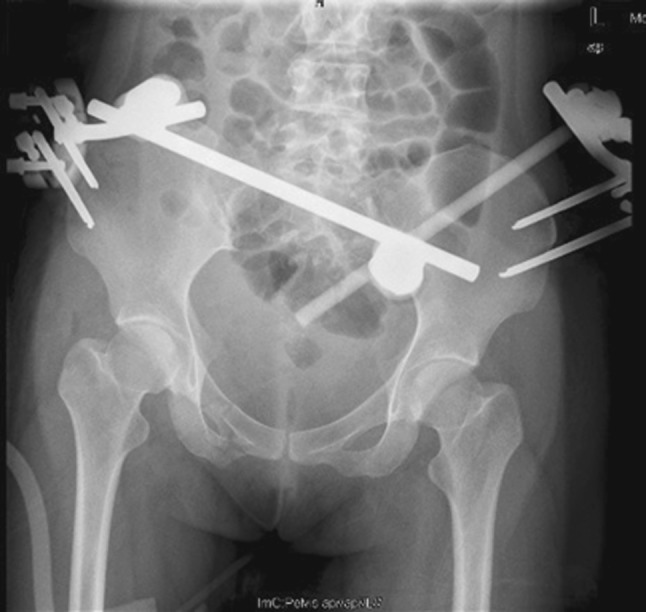
Temporary external fixation for bilateral sacral fractures
Fig. 3.
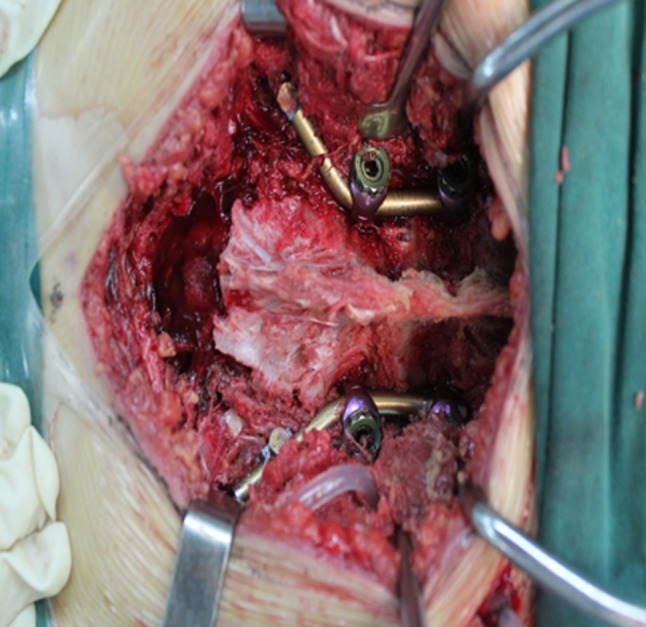
Sacral laminectomy for nerve decompression intraoperative
Fig. 4.
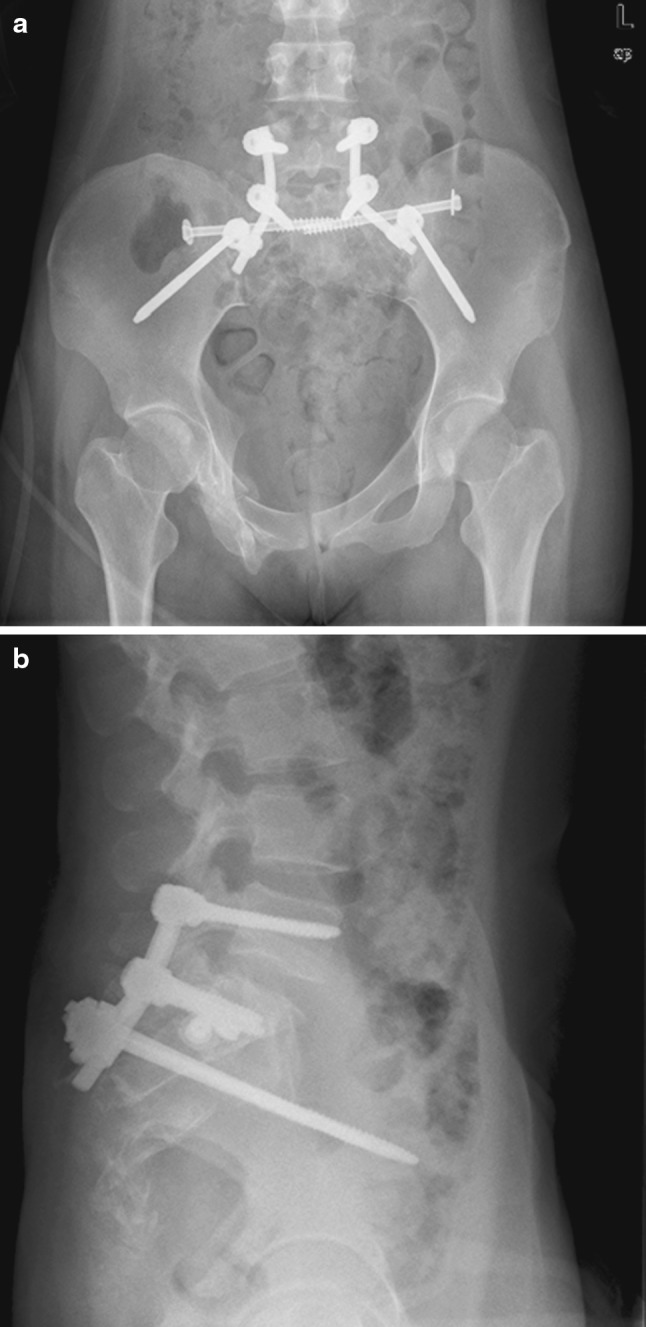
Post-operative radiograph demonstrating triangular osteosynthesis for bilateral sacral fractures
Post-operative care
The suction drains are taken away within 24 h usually. All patients received prophylactic antibiotics for 24–48 h and began to do physical rehabilitation exercises from the first day after operation. Immediate post-operative partial weight-bearing was permitted with the help of a crutch or a walker according to the overall condition of the patients, and advanced to full weight-bearing at 4–6 weeks post operation. The reduction quality was evaluated according to Matta criterion. Clinical function outcome and nerve function outcome were evaluated by Majeed and Gibbons criterion. Patients were followed up prospectively with routine visits at 1 month, 2 months, 3 months, 6 months, and 1 year for clinical and radiographic examination. Follow-up radiographs included X-ray trauma series (AP, inlet, and outlet of pelvis). If the fracture healed at 6–8 months post operation, then the hardware was removed.
Results
The average operating time was 130 min (range 100–230 min). The average blood loss was 450 ml (range 100–800 ml). 16 cases of unilateral vertical unstable sacrum fractures were fixed with unilateral triangular osteosynthesis, three patients with bilateral sacrum fractures were fixed with bilateral triangular osteosynthesis, and the other three bilateral fractures were fixed with unilateral triangular osteosynthesis as one side of the sacrum fracture was stable. Seven side fractures were fixed with only S1 pedicle screw, while 18 side fractures were fixed with L5 and S1 pedicle screws. Five patients were performed sacral laminectomy for cauda equina decompression due to canal occlusion, and another eight patients who suffered sacral plexus impairment were decompressed through fracture reduction or their small fractures were removed. Two cases of wound infection were reported, which was treated with prompt debridement, lavage, and antibiotic. The wound had healed, and the internal fixation implants were not removed before bone union. All patients were followed up for a minimum of 14 months (range 8–26 months). All of the followed up patients demonstrated bone union within 3–6 months (Fig. 5). 16 patients were permitted to handle full weight-bearing 4–6 weeks post-operation; other patients were rejected because of lower limb fracture, polytrauma, or neurologic impairment. No loosening of the hardware occurred, and there is no internal fixation broken. 16 cases of internal fixation have been removed (Fig. 6), and 18 patients have reported back to their original work. No iatrogenic nerve lesion was observed. According to Matta criterion for fracture reduction, the results were excellent in 18 sides, good in 6 sides, and fair in 1 side. According to Majeed functional scoring at last follow-up, the results were excellent in 13 cases, good in 6 cases, fair in 2 cases, and poor in 1 case. Neurologic impairments were noted in 13 patients pre-operative, and these patients underwent nerve decompression through laminectomy. Six patients achieved completely recovery, six patients achieved partial improvement, and one patient did not have any improvement at last follow-up. Table 3 demonstrated nerve function transition between pre-operation and post-operation.
Fig. 5.

Pelvic X-ray demonstrating bone union 6 months after operation
Fig. 6.

Pelvic X-ray demonstrating internal implants that have been removed 8 months after operation
Table 3.
Nerve function transition between pre-operation and post operation in patients who suffered nerve impairment according to Gibbons grading
| Gibbons grading | Pre-operation | Post-operation |
|---|---|---|
| Grade I | 0 | 6 |
| Grade II | 4 | 4 |
| Grade III | 5 | 2 |
| Grade IV | 4 | 1 |
Discussion
Tile C pelvic ring injuries following vertical unstable sacral fractures usually caused by high-energy injuries present a difficult fixation problem for the orthopedic traumatologist. There are both vertical and rotational pelvic instabilities [9]. Different internal fixation implants have been proposed to reconstruct the posterior pelvic ring, but all of these implants have limitations: the difficulty lies in achieving vertical and rotational stabilities simultaneously. Systematic analysis showed that implant failure ranges from 2 to 17.3 % [17]. Kach et al. [18] applied lumbopelvic distraction spondylodesis for the treatment of sacral fractures; this procedure oriented in the vertical direction between the pedicle of L4 or L5 and the crista iliaca, which is a logical protection against cranial migration of the injured half of the pelvic ring. However, Schildhauer et al. [12] pointed out that this kind fixation cannot guarantee rotational stability because it addresses vertical forces only, whereas rotational stability cannot be achieved by the vertical two-point fixation. To solve this problem, triangular osteosynthesis for unstable sacral fractures had been recently introduced [12–16]. This fixation combines a transverse fixation with a lumbopelvic distraction osteosynthesis, providing clinically and biomechanically sufficient multiplanar stability [16, 18]. Biomechanical analysis confirmed that triangular segmental lumbopelvic instrumentation is the most stable fixation method [12, 19]. Such strong fixation allows patients to do early mobilization and carry out progressive weight-bearing activity post-operation [12, 14]. In this series, all patients were treated with iliosacral screw combined with USS fixation, and were permitted to do early physical rehabilitation exercise, to get out of bed with crutches or a walker 3–7 days post-operation, and can have full weight-bearing ability 4–6 weeks post-operation. This confirmed that triangular osteosynthesis allows patients to do early functional exercise and is conducive for function recovery.
Unstable sacral fractures are often combined with nerve injury. Triangular osteosynthesis for the treatment of sacral fractures has the following two advantages: (1) satisfactory reduction can be obtained smoothly, and (2) nerve compression can be decompressed intuitively. Vertical displacement can be reduced by the distraction function of USS system, while horizontal displacement can be reduced through clamp. In this series, and a high quality of fracture reduction was obtained, with the high excellent ratio of 90 % being achieved according to Matta criteria. Sacral plexus impairment was divided into four grades by Gibbons [2]. Nerve impairment always occurred in type II and III sacral fractures according to Denis classification, and was proposed to take nerve decompression [1]. Reilly et al. [20] recognized that crushed nerve injury can be recovered through early surgical intervention. In this group, neurologic impairment was noted in 13 patients pre-operative, after complete nerve decompression, six patients achieved complete recovery, six patients achieved partial improvement, and one patient did not experience any improvement at the last follow-up. This patient suffered sacral plexus rupture. Although anastomosis of the nerve was undertaken, the function could not be restored. We believe that when applying triangular osteosynthesis fixation for sacral fractures associated with nerve injury, there are two reasons accounting for the neurologic function recovery: (1) nerve decompression can be obtained, cauda equina and the nerve root will not be compressed, and suffering due to long-term traction can be avoided, which is conducive for neurologic function recovery; and (2) satisfactory reduction decreased the chances of bone malunion which results in a great number of callus and fibrosis formations that might damage the nerve.
Though triangular osteosynthesis fixed lumbosacral joint, the mobility of lower lumbar segments were destroyed [2]. Thus, it is necessary to select the fixed segment appropriately and to choose as short a segment as possible. The vertical stabilization was achieved through connecting iliac screw and pedicle screw, but L5 pedicle screw is selected if L5/S1 articular capsule is destructive in the initial triangular osteosynthesis [12, 15]. Sometimes, however, the L4 pedicle should be chosen:, (1) when the L5 pedicle is fractured or the avulsion extends to L5 transverse process, which makes the insertion of the L5 pedicle screw difficult or the screw is unstable; and (2) during lumbosacral lordosis or in sacralization of L5, a vertebropelvec fixation between L5 and iliac turns to be a horizontal fixation which cannot resist vertical shear. Mouhsine et al. [14] selected two pedicle screws, L4 and L5, which can provide sufficient stability; however, the lumbar mobilities of L4 and L5 were sacrificed. Sar [21] introduced S1 pediculoiliac screw fixation to a patient with sacral alar fracture (zone 1) and another one with sacroiliac joint instability. This technique requires much less exposure, and there is no lumbosacral fusion, so that the lower lumbar mobility is not affected. The disadvantage is that there is no reduction capability of the vertically displaced fractures, and this technique requires the L5/S1 articular capsule and S1 pedicle intact. Therfore when applying this technique for treating unstable sacral fractures, the vertical displacement should be minimal, which can be reduced through manual traction before operation. In this group, seven side fractures accorded with the above condition, and so we applied both S1 pediculoiliac screw plus iliosacral screw. If the other grossly displaced fractures cannot be reduced with traction or the L5/S1 capsule is not intact, then we inserted two screws, L5 and S1, to achieve reduction and stability. All the patients gained unprotected full weight-bearing ability, no matter whether fixed with one or two pedicle screws, and there were no fixation failure and fracture displacement. However, patients fixed with only one screw resumed normal working much earlier, and the function recovery was better in these patients than those who were fixed with L5 and S1 screws. The reasons for the differences are that the lumbar is not fixed and the lumbosacral activity resumes in the patients fixed with S1 only. Another reason is that the damage is relatively minor compared with those fixed with two screws. The function outcome improved significantly in the last follow up compared to that observed within 3 months after surgery. The main reason might be that the patients fixed with two pedicle screws received implant removal and the function improved obviously. Hence, we strongly recommend routine removal of the implants especially from those fixed with two pedicle screws. Sagi et al. [15] also suggested having the implants removed after bone union.
The choice of horizontal fixation device is still controversial when treating unstable vertical sacral fractures by triangular osteosynthesis: should it be iliosacral screw or transsacral plate? should it be with only one screw or with two screws? There is no biomechanical study to evaluate the difference of stability till now. Schildhauer et al. [12] chose transsacral plate when dealing with bilateral fractures and grossly displaced unilateral fractures. In their opinion, enhanced stability can be obtained in the disrupted pelvic ring through the plate, which is molded in M-shape. This construct acts as tension band and clamp. While two iliosacral screws were implanted in unilateral sacral fractures associated with minor displacement of the anterior pelvis, they believe that at least two iliosacral screws are required when the anterior ring has instability, but one screw is enough, when the anterior pelvis has stability. However, they did not report the difference of complications and stability experienced between the fixations of transsacral plate and iliosacral screws. However, transsacral plate fixation will increase soft damage, while iliosacral screw fixation will increase iatrogenic nerve impairment especially when fixed with two screws, at least, theoretically. Sagi et al. [15] used only one iliosacral screw for horizontal fixation, but the anterior pelvic ring was stabilized in cases of wide rami displacement or symphyseal diastasis. Mouhsine et al. [14] modified triangular osteosynthesis for unstable sacral fractures. In their study, the horizontal fixation was performed with a 6-mm rod used as a crosslink between the two connecting rods. The idea was to reduce striping soft tissue and putting less hardware at the fracture site. However, this method is only applicable to patients with bilateral sacral fractures; otherwise, it requires extensive exposure which will increase soft tissue damage on the contrary. All the studies reported good results, and the patients can have unprotected early weight-bearing ability, yet there are no biomechanical studies so far to analyze which horizontal fixation is the most stable one: only one thing that is certain is that horizontal fixation is necessary, as rotational stability cannot be obtained by vertical fixation. In this consecutive series, we obtained horizontal stability through one percutaneous iliosacral screw, but a plate was used to fix the anterior pelvic ring when it has instability. The result is promising, there is no fixation failure, and the patients can perform early physical rehabilitation exercises. An important phenomenon that should be considered is that patients in this group are very young, and therefore, the bone quality is good which might have influenced the results. Schildhauer et al. [12] reported that in their research, one patient suffered hardware loosening due to osteoporotic defect; hence, when treating patients with poor bone quality, more attention should be paid when performing fracture reduction, and the time to realize full weight-bearing ability might be prolonged.
In conclusion, we found that, triangular osteosynthesis, as described in this article, has advantages in treating unstable sacral fractures: makes the fixation to be rigid, permits achieving early full weight-bearing ability, allows performing nerve decompression, and facilitates faster function recovery. However, there still exists much controversy regarding the technique and the option of implants.
References
- 1.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 2.Gibbons KJ, Soloniuk DS, Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg. 1990;72:889–893. doi: 10.3171/jns.1990.72.6.0889. [DOI] [PubMed] [Google Scholar]
- 3.Court-Brown CM, Gertzbein SD. The management of burst fractures of the fifth lumbar vertebra. Spine. 1987;12:308–312. doi: 10.1097/00007632-198704000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Latenser BA, Gentilello LM, Tarver AA, et al. Improved outcome with early fixation of skeletally unstable pelvic fracture. J Trauma. 1991;31:28–31. doi: 10.1097/00005373-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Pohlemann T, Angst M, Schneider E, et al. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993;7:107–117. doi: 10.1097/00005131-199304000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Griffin DR, Starr AJ, Reinert CM, et al. Vertically unstable pelvic fractures fixed with percutaneous iliosacral crews: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2003;17:399–405. doi: 10.1097/00005131-200307000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Routt ML, Kreqor PJ, Simonian PT, et al. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995;9:207–214. doi: 10.1097/00005131-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Tile M. The management of unstable injuries of the pelvic ring. J Bone Joint Surg Br. 1999;81:941–943. doi: 10.1302/0301-620X.81B6.10474. [DOI] [PubMed] [Google Scholar]
- 9.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Coombs R, Hoeflinger MJ, et al. Anatomical and radiological considerations in compressive bar technique for posterior pelvic disruptions. J Orthop Trauma. 1991;5:434–438. doi: 10.1097/00005131-199112000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Stocks GW, Gabel GT, Noble PC, et al. Anterior and posterior internal fixation of vertical shear fractures of the pelvis. J Orthop Res. 1991;9:237–245. doi: 10.1002/jor.1100090212. [DOI] [PubMed] [Google Scholar]
- 12.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307–314. doi: 10.1097/00005131-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Schildhauer TA, Ledoux WR, Chapman JR, et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Mouhsine E, Wettstein M, Schizas C, et al. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J. 2006;15:857–863. doi: 10.1007/s00586-004-0858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sagi HC, Caron T, Militano U, et al. A comprehensive analysis with minimum one-year follow-up of vertically unstable trans-foraminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma. 2009;23:313–319. doi: 10.1097/BOT.0b013e3181a32b91. [DOI] [PubMed] [Google Scholar]
- 16.Sagi HC. Technical aspects and recommended treatment algorithms in triangular osteosynthesis and spinopelvic fixation for vertical shear transforaminal sacral fractures. J Orthop Trauma. 2009;23:354–360. doi: 10.1097/BOT.0b013e3181a1143a. [DOI] [PubMed] [Google Scholar]
- 17.Papakostidis C, Kanakaris NK, Kontakis G, et al. Pelvic ring disruptions: treatment modalities and analysis of outcomes. Int Orthop. 2009;33:329–338. doi: 10.1007/s00264-008-0555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kach K, Trentz O. Distraction spondylodesis of the sacrum in “vertical shear lesions” of the pelvis. Unfallchirurg. 1994;97:28–38. [PubMed] [Google Scholar]
- 19.Zelle BA, Gruen GS, Hunt T, et al. Sacral fractures with neurological injury: is early decompression beneficial? Int Orthop. 2004;28:244–251. doi: 10.1007/s00264-004-0557-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reilly MC, Zinar DM, Matta JM. Neurologic injuries in pelvic ring fractures. Clin Orthop Relat Res. 1996;329:28–36. doi: 10.1097/00003086-199608000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Sar C, Kilicoglu O. S1 pediculoiliac screw fixation in instabilities of the sacroiliac complex: biomechanical study and report of two cases. J Orthop Trauma. 2003;17:262–270. doi: 10.1097/00005131-200304000-00004. [DOI] [PubMed] [Google Scholar]


