Abstract
Purpose
The percutaneous insertion technique requires surgical skill and experience. However, there have been few clinical reports evaluating the accuracy of minimally invasive pedicle screw placement using the conventional fluoroscopy method. The purpose of this study was to evaluate the accuracy of percutaneous pedicle screw placement in the treatment of thoracic and lumbar spine fractures using two-plane conventional fluoroscopy.
Methods
A prospective clinical trial was performed. A total of 502 percutaneous pedicle screws in 111 patients, all inserted with the assistance of conventional fluoroscopy, were evaluated. The safety and accuracy of pedicle screw placement were based on the evaluation of postoperative axial 3-mm slice computed tomography scans using the scoring system described by Zdichavsky et al. [Eur J Trauma 30:234–240, 2004; Eur J Trauma 30:241–247, 2004].
Results
427/502 pedicle screws (85 %) were classified as good and excellent concerning the best possible screw length and 494/502 (98 %) were found to have good or excellent position. One screw had to be revised due to medial position with a neurological deficit.
Conclusions
This study demonstrates the feasibility of placing percutaneous posterior thoracolumbar pedicle screws with the assistance of conventional fluoroscopy. Minimally invasive transpedicular instrumentation is an accurate, reliable and safe method to treat a variety of spinal disorders, including thoracic and lumbar spine fractures.
Keywords: Thoracolumbar spine fractures, Pedicle screw, Percutaneous technique, Minimally invasive spine surgery, Transpedicular instrumentation
Introduction
In the last two decades, there has been a clear trend in surgery to minimize the injury to normal tissues while abating the same or a better surgical outcome. The idea of percutaneous transpedicular instrumentation for thoracic and lumbar spine fractures has a long history. Percutaneous transpedicular instrumentation was first performed and described by Magerl in 1977 [14]. It was brought into play for temporary external fixation of spinal fractures and in case of infections [14, 15].
The advantage of percutaneous dorsal pedicle screw instrumentation appears to be obvious with respect to the approach. There is no need to remove the spinal muscle from the insertion leading to reduced muscle function, which has been investigated and shown in an electromyophysiological study. Using this technique, significant reduction of blood loss was achieved. Grass et al. [8] showed an average blood loss of 43 ml (10–90 ml) versus the open approach needing 870 ml (570–1,200 ml). A faster rehabilitation due to the less invasive technique has been described by different current publications [3, 5, 6, 22].
The accurate placement of pedicle screws requires surgical skills and experience, especially for the percutaneous insertion technique. Although percutaneous posterior instrumentation has been described in several clinical studies [1, 4, 11, 13, 15, 17, 18, 23, 24], there is lack of data in the literature concerning their use in thoracic and lumbar spine fractures. Traditional open thoracolumbar instrumentation results in significant iatrogenic damage of the vital dorsal musculoligamentous complex [8, 10, 19, 21].
Therefore, the purpose of this prospective study was to investigate the precision, accuracy, and safety of percutaneous pedicle screw insertion for spine fractures in a larger, consecutive number of screws.
Materials and methods
Aiming at a minimum of 500 pedicle screws, 502 consecutively applied screws in a percutaneous technique were included in the study. The operative technique involved a simultaneous double image intensifier. Inclusion criteria were trauma of the thoracic and lumbar spine requiring dorsal instrumentation (±additional ventral fusion or augmentation). After a certain period of training with this technique, the percutaneous screw application was used as a standard procedure in spinal trauma for all patients, if the following criteria were fulfilled:
sufficient X-ray projection in two planes intraoperatively;
sufficient reposition by closed means in a prone position;
no need for additional dorsal open approach (for laminectomy, spinal decompression, fusion or in rotational instability).
All patients in this study underwent a thin-slice CT scan preoperatively for exact evaluation of fracture pattern and preoperative planning for correct pedicle diameter and vertebral lengths. Figure 1 demonstrates a typical example of preoperative CT scan to evaluate the fracture pattern (angle of kyphosis, instability criteria) that allows a classification of the fracture according to Magerl et al. [16] (Fig. 1a, b). For each pedicle screw to be placed percutaneously, a preoperative planning was performed to determine an adequate screw diameter as well as the maximum possible screw length and the adequate convergence angle (Fig. 2a, b, c).
Fig. 1.
Preoperative axial (a) and sagittal (b) CT scan to evaluate fracture pattern (angle of kyphosis) and to classify the fracture (according to Magerl et al. [15])
Fig. 2.
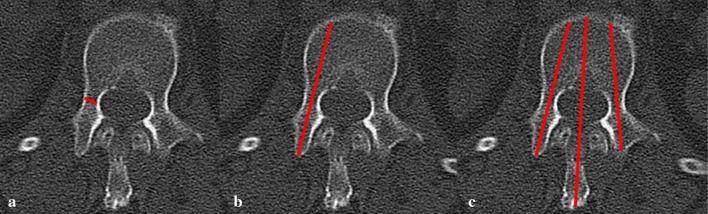
Preoperative CT scan for planning of pedicle screw width, length, and convergence angle (to be performed for each single screw)
Patients were placed in the prone position on a carbon fiber radiolucent operating table with the chest and pelvis supported to gain lordosis. The intraoperative setting is shown in Fig. 3. The repositioning of a traumatic kyphosis is performed percutaneously on the table. The quality of reposition is controlled through the lateral and a.p. image intensifier. A.p. and lateral fluoroscopy projections should be parallel to the end plates nearest the screw to be inserted. An adequate fluoroscopic image of the pedicles should be obtained in both the a.p. and lateral views before proceeding. The spinous process should be midline between the pedicles to ensure a direct a.p. projection. Depending on the depth of the tissue between the skin and pedicle, the skin incision should be made 1–2 cm laterally so that the Jamshidi needle can be angled appropriately when inserting it into the pedicle. After placing the Jamshidi needle at the intersection of the facet and the transverse process, an a.p. image should show the needle tip initially at the lateral margin of the pedicle in the “3 o’clock” (right pedicle) or “9 o’clock position” (left pedicle). While the Jamshidi needle is advanced into the pedicle, a.p. and lateral fluoroscopy should be used intermittently as needed to confirm the direction, making sure that the needle remains lateral to the medial pedicle wall. As the needle advances toward the base of the pedicle on the lateral image, it should approach the pedicle center on the a.p. image. A guidewire is inserted through the cannula and into the pedicle. The cannula is then carefully removed, leaving only the guidewire in place. The fascia and muscle must be dilated (dilatation system) to allow for screw placement. After preparation of the pedicle with a tap, the cannulated pedicle screw is inserted over the guidewire (Fig. 4).
Fig. 3.
Intraoperative setting with image intensifier simultaneously in two planes
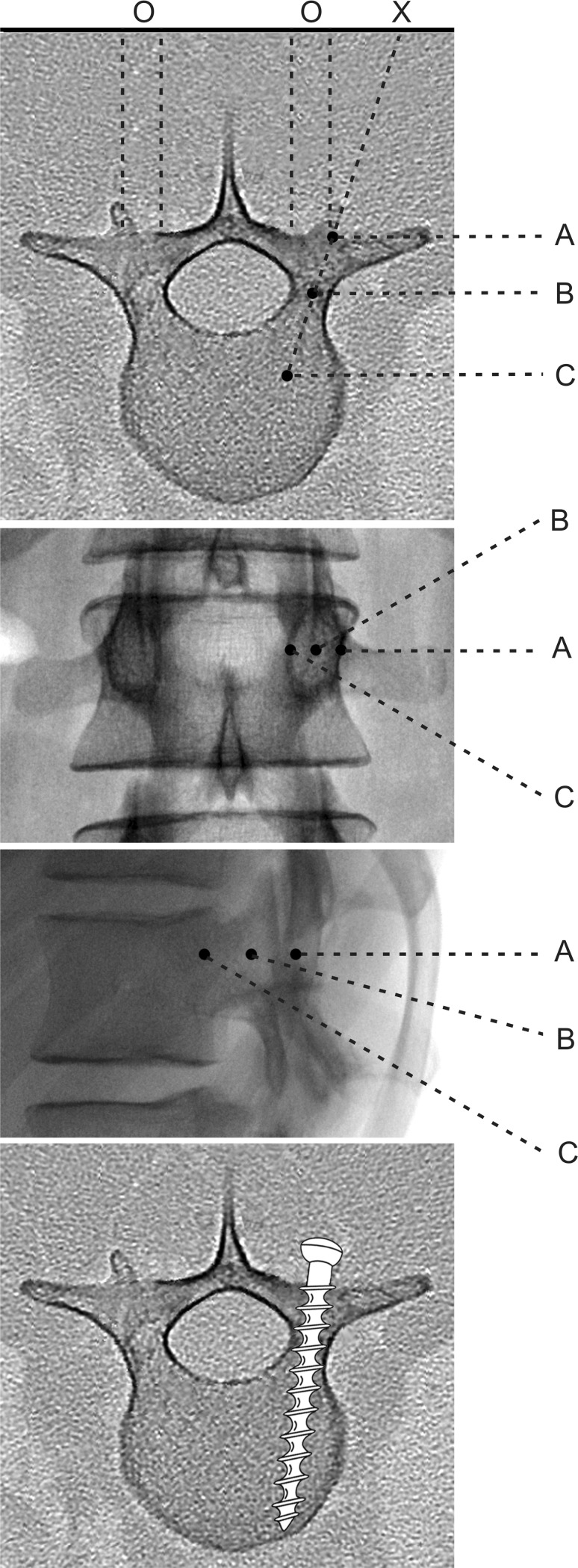
Fig. 4.
Diagrams illustrating the anatomical principles of percutaneous pedicle screw insertion: axial view, a.p. view, lateral view, and axial view (top to bottom). 0: Projection point of the pedicle onto the backskin. X: Incicion point. First, the needle tip is docked onto the lateral margin of the pedicle in three (right pedicle) and nine (left pedicle) o’clock position (position A). As the needle advances toward the base of the pedicle on the lateral image, it should approach the pedicle center on the a.p. image (position B). When the Jamshidi needle exceeds the posterior wall of the vertebra on the lateral image, the tip of the needle has to remain lateral to the medial pedicle wall on the a.p. image (position C)
For stabilization of traumatic thoracic and lumbar spine fractures and other spinal disorders, the CD Horizon Longitude™ multi-level percutaneous fixation system (Medtronic Sofamor Danek) was used between June 2009 and January 2011. Pedicle screws with a diameter between 4.5 and 7.5 mm were inserted, depending on the pedicle width in the preoperative CT scans. The pedicle screws were inserted according to anatomical landmarks using true a.p. and lateral fluoroscopic visualization of the spine.
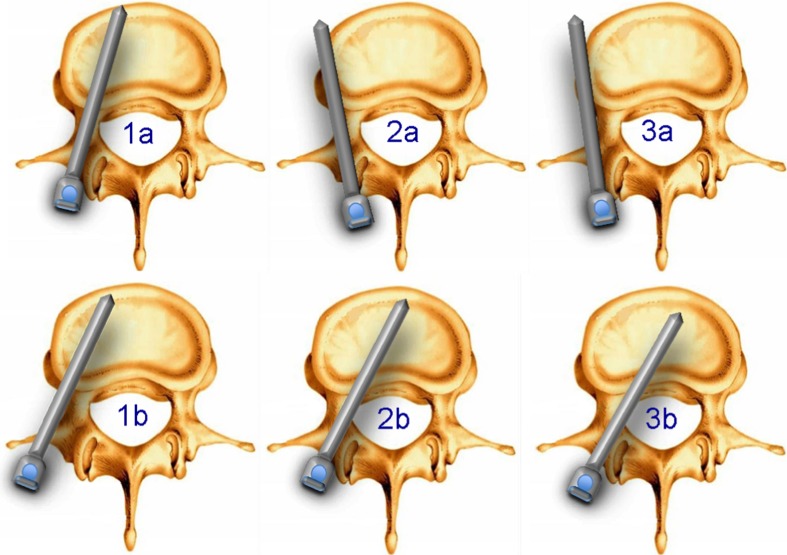
All patients underwent a thin-slice postoperative CT scan to measure and classify the accuracy of pedicle screw placement. The screw length was measured in percent of the maximal possible length of the vertebral body. The accuracy of pedicle screw placement was based on evaluation of postoperative axial 3-mm slice computed tomography scans using the scoring system described by Zdichavsky et al. [27, 28] (compare Fig. 5). The best positioning options are the 1a and the 1b types. The 2a or 2b position must be evaluated for stability, but usually does not require a revision. In a 3a and 3b malposition, depending on stability or the possible neurological irritation, a screw revision must be considered.
Fig. 5.
Evaluation scale to determine precision in percutaneous pedicle screw application. The positioning scale according to Zdichavsky et al. [27, 28] was adopted. Best positioning options are 1a and 1b. A 2a or 2b position must be evaluated for stability, usually do not require revision. A 3a and a 3b malposition might need revision for lack of stability (3a) or neurological irritations (3b)
A total of 111 patients with 502 percutaneous pedicle screw instrumentations in 251 vertebral bodies were included in this study. All patients admitted to our department between July 2009 and January 2011 who required a dorsal instrumentation for stabilization of thoracic or lumbar spine injuries were included to check the study criteria; 34 patients did not fulfill inclusion criteria and underwent open dorsal instrumentation during that time period. The remaining 111 patients (77 %) fulfilled the criteria and were included in the study. The mean age of the patients at the time of surgery was 63 ± 16 years (range 15–88 years).
Of the 111 patients, 40 underwent a dorsal instrumentation without additional procedures, 53 patients in the older age group received an additional percutaneous balloon kyphoplasty, and 18 patients underwent a minimally invasive ventral procedure.
Results
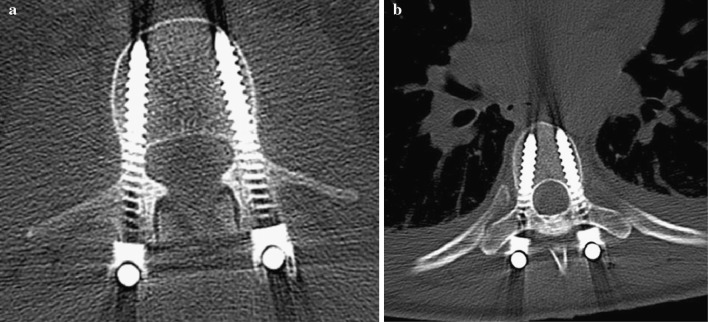
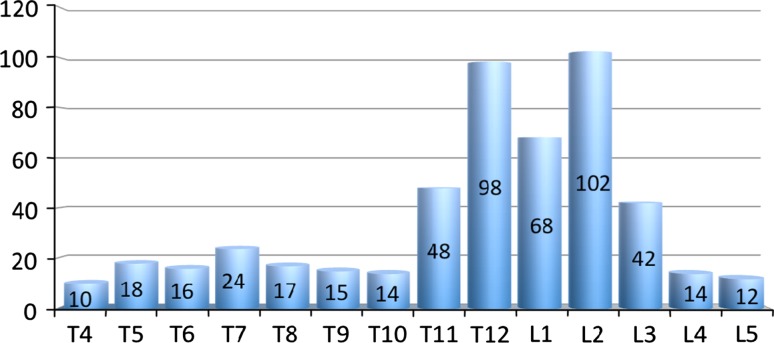
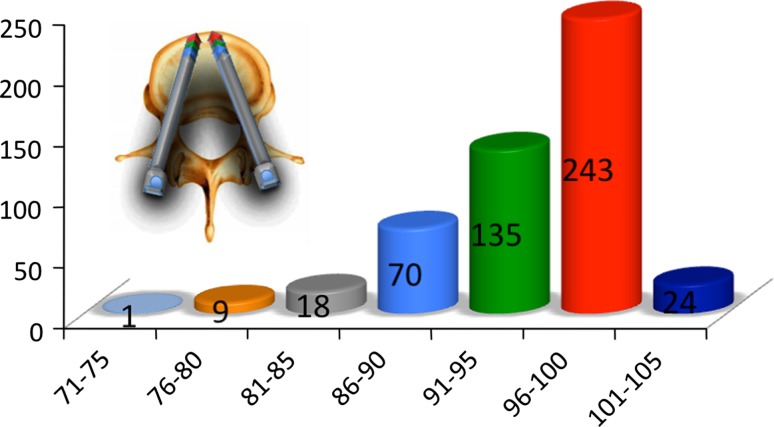
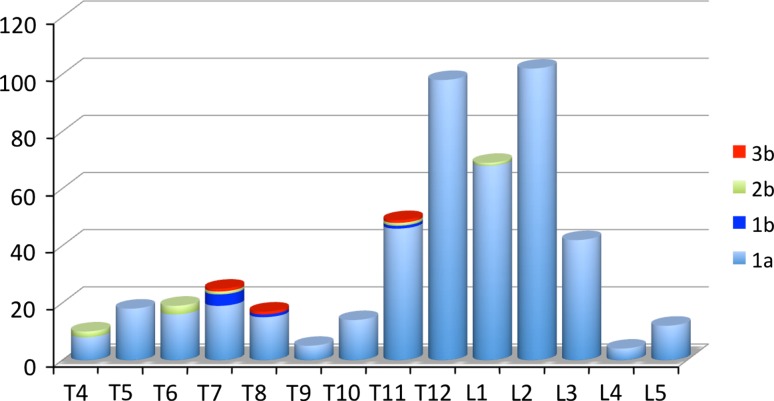
All 111 patients with 502 pedicle screws placed in a percutaneous technique were evaluated according to the above described technique. An excellent position (type Zdichavsky 1a) and an excellent screw length of a 100 % total vertebral body length are shown in Fig. 6a, b. The highest level of percutaneous instrumentation of the series was Th4 and the lowest was L5. Of 502, 316 (63 %) were placed in the thoracolumbar junction (Th11–L2) as typically seen in a trauma group (Fig. 7). The evaluation scale to measure the precision in percutaneous pedicle screw application is shown in Fig. 8. All screws that showed a longer length of 85 % of the total vertebral length were evaluated as good; if 90 % or more of the total possible length was achieved, the length was evaluated as excellent. In 243 screws, the length was close to 100 %, and in 135 screws 91–95 % of the total length was achieved. Seventy screws revealed a length of 86–90 % and 18 screws show a length between 81–85 % of the total possible length. A group of 24 patients had a bicortical screw fixation with the tip of the screw a few millimetres ahead of the ventral cortex of the vertebral body. None of these screws needed revision. Of 502 screws, 427 (85 %) therefore show more than 85 % of the total possible length and are evaluated as good or excellent (Fig. 9). The evaluation scale to determine precision in percutaneous pedicle screw application was adopted from Zdichavsky et al. [27, 28] as shown in Fig. 5. There were three patients with the 3b medial malposition in Th4, Th8, and Th11, respectively. One revision was necessary due to a 3b medial malposition of a pedicle screw at the level Th8 in a patient with ankylosing spondylitis which let to an incomplete spinal cord lesion (Frankel/ASIA C). The neurological symptoms remained until transfer to a rehabilitation center. In the remaining 110 patients, no screw revision was needed. A total of 494–502 (98 %) of screws turned out to have a good or perfect position (Fig. 10). In all patients, we recommended the removal of pedicle screws after non-fusing instrumentation was performed in a percutaneous fashion without the need to open other than in the first operation. Figure 11 shows the easy steps of removal of pedicle screws in a percutaneous fashion.
Fig. 6.
Postop CT scan to measure length and position of pedicle screws. Both show excellent length (=100 %) and positioning (Zdichavsky 1a) [27, 28]
Fig. 7.
Number of applied percutaneous pedicle screws related to the level of insertion (n = 502, highest Th 4, lowest L5)
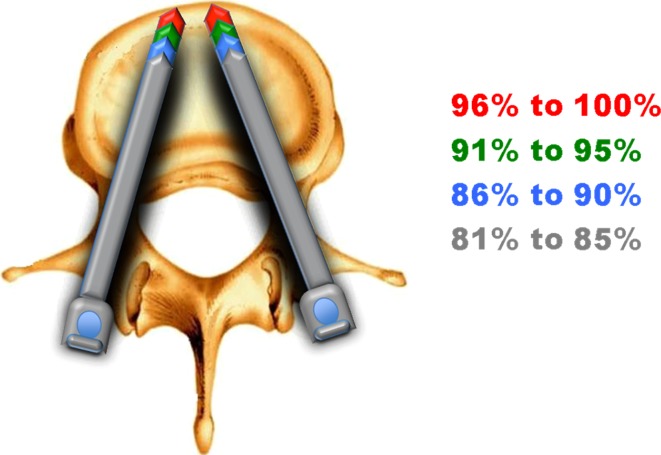
Fig. 8.
Evaluation scale to measure the precision of percutaneous pedicle screw application. Percent screw length of maximal possible length of the instrumented vertebral body (=100 %)
Fig. 9.
Precision of percutaneous pedicle screw application. Percent screw length of maximal possible length (=100 %); 427 of 502 screws (85 %) showed more than 85 % of the total possible length and were evaluated as good and excellent
Fig. 10.
One revision was necessary causing neurological symptoms in a 3b medial malposition of level T8 in a patient with ankylosing spondylitis. No other screw revision was needed; 494 of 502 (98 %) screws turned out to have a good or perfect position
Fig. 11.
Minimally invasive removal of dorsal instrumentation
Discussion
The current trends toward minimally invasive surgical techniques represent an important shift in the practice of contemporary spinal surgery. Accurate placement of pedicle screws will provide optimal mechanical strength and patients’ safety.
For thoracic pedicle screws used in the treatment of spinal deformities, the incidence of screw misplacement ranges from 3 to 44.2 %. The wide variations in the rate of screw misplacement may be attributed to the different method of evaluating the position of the pedicle screws. Gertzbein and Robinsons [7] reported that 15 % of 71 screws inserted using intraoperative fluoroscopy into a non-deformed thoracic spine between T8 and T12 had penetrated the medial pedicle cortex by 2.1–8.0 mm into the spinal canal. Only two patients developed neurologic complaints, which resolved spontaneously after 6 months without screw removal. Liljenqvist et al. [12] reported that 10 screws (8.3 %) out of 126 in idiopathic scoliosis violated the medial pedicle wall by an average of 1.5 mm and a maximum of 3 mm. There were no neurologic complications in any cases. Belmont et al. [2] reported that only 2 screws were out between 2 and 4 mm among 279 thoracic pedicle screws inserted using intraoperative fluoroscopy, which was confirmed by computed axial tomography. Youkilis et al. [26] reported 19 (8.5 %) cortical violations, which included 8 (3.6 %) violations more than 2 mm out of 224 image-guided thoracic pedicle screws confirmed by postoperative CT scan. Transgression of the medial thoracic pedicle wall up to 4 mm is not necessarily associated with neurologic complications, because medial breach up to 4 mm by a thoracic pedicle screw causes similar loss of spinal canal cross-sectional area as one or two intracanalicular hooks [20].
The accuracy of minimally invasive screw placement in such a large group of trauma patients has not been reported yet. An accurate screw placement concerning the positioning of 98 % is at least as high as an open dorsal instrumentation. There was one critical medial malposition of the screw (Zdichavsky type 3b) leading to a neurological deficit. This happened in a 78-year-old adipose patient with ankylosing spondylitis. We have underestimated the risk of bad visualization using image intensifier in contrast to an open technique in these patients; however, the risk of malposition of pedicle screws in these patients is also high in the open technique. Furthermore in over 95 % of our patients, we achieved more than 85 % of the maximal possible length of the pedicle screw due to exact preoperative planning.
Approximately, 60 % of the fixation strength of thoracic and lumbar pedicle screws is in the pedicle itself. The cancellous bone in the vertebral body adds another 15–20 % of strength, whereas purchase in the anterior cortex offers 20–25 % increase [9, 25]. In normal healthy bone, it is not necessary to routinely engage the anterior cortex, which also avoids the potential danger of injuring the anterior vascular structures. In cases of osteoporosis or problematic fracture type, adequate screw diameters as well as the maximum possible screw length offer the maximum available fixation strength. In cyclic load tests, deeper-inserted screws were found to withstand a greater number of cycles before loosening [29].
There are certain limitations and disadvantages in the percutaneous technique of fracture instrumentation. Additional reposition by the device is highly limited compared to the open Schanz screw technique. Therefore, we did not use this device, unless an anatomical reduction was achieve in a closed manner in a prone position.
We still do not know if the lordotic pretension used in a Schanz screw technique might result in a better retention of the fracture. This needs to be analyzed in further studies. In a percutaneous technique, a dorsal fusion or an additional fixation between the longitudinal fractures with rotational instabilities is not possible. We therefore did not use a percutaneous instrumentation in these fractures. In all fractures that need an additional ventral fusion, we do not see a problem for a non-fusing percutaneous technique on the dorsal side. In cases of navigation, we think percutaneous screw application technique is very limited and we therefore do not use navigation in combination with percutaneous screw application.
Conclusion
This study evaluated the radiographic results in 502 pedicle screws in 111 patients who underwent minimally invasive transpedicular instrumentation for thoracic and lumbar spine injuries. The accurate placement of pedicle screws will provide optimal mechanical strength and ensure patients’ safety.
According to the results presented here, we feel that percutaneous screw application for dorsal pedicle instrumentation in fracture patients is a safe treatment and may be recommended.
Conflict of interest
None
References
- 1.Bednar DA, Raducan V. External spinal skeletal fixation in the management of back pain. Clin Orthop. 1996;322:131–145. [PubMed] [Google Scholar]
- 2.Belmont PJ, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 3.Blattert TR, Katscher S, Josten C. Percutaneous techniques in the thoracic and lumbar spine. Unfallchirurg. 2011;114(1):17–25. doi: 10.1007/s00113-010-1939-9. [DOI] [PubMed] [Google Scholar]
- 4.Esses SI, Botsford DJ, Kostuik JP. The role of external spinal skeletal fixation in the assessment of low-back disorders. Spine. 1989;14:594–601. doi: 10.1097/00007632-198906000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J. 2010;19(2):316–324. doi: 10.1007/s00586-009-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan SW, Hu ZJ, Fang XQ, Zhao FD, Huang Y, Yu HJ. Comparison of paraspinal muscle injury in one-level lumbar posterior inter-body fusion: modified minimally invasive and traditional open approaches. Orthop Surg. 2010;2(3):194–200. doi: 10.1111/j.1757-7861.2010.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Grass R, Biewener A, Dickopf A. Perkutane dorsale versus offene Instrumentation bei Fraktu-ren des thorakolumbalen Über-gangs: Eine vergleichende prospective Untersuchung. Unfallchirurg. 2006;109:297–305. doi: 10.1007/s00113-005-1037-6. [DOI] [PubMed] [Google Scholar]
- 9.Hirano T, Hasegawa K, Takahashi HE, Uchiyama S, Hara T, Washio T, Sugiura T, Yokaichiya M, Ikeda M. Structural characteristics of the pedicle and its role in screw stability. Spine. 1997;22:2504–2509. doi: 10.1097/00007632-199711010-00007. [DOI] [PubMed] [Google Scholar]
- 10.Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique and complications. Neurosurg Focus. 2006;20:1–5. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 11.Jeanneret B, Jovanovic M, Magerl F. Percutaneous diagnostic stabilization for low back pain: correlation with results after fusion operations. Clin Orthop. 1994;304:130–138. [PubMed] [Google Scholar]
- 12.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lyon DW, Hall DJ, Mulholland RC, Webb JK. The role of external fixation as a predictor of fusion success. In: Ono K, Takemitsu Y, Yonenobu K, editors. Lumbar fusion and stabilization. Tokyo: Springer; 1993. pp. 25–34. [Google Scholar]
- 14.Magerl F. Verletzungen der Burst- und Lendenwirbelsäule. Langenbecks Arch Chir. 1980;352:428–433. doi: 10.1007/BF01292083. [DOI] [Google Scholar]
- 15.Magerl F. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop. 1984;189:125–141. [PubMed] [Google Scholar]
- 16.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 17.Nakashima H, Sato K, Ando T, Inoh H, Nakamura H. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. J Spinal Disord Tech. 2009;22(7):468–472. doi: 10.1097/BSD.0b013e31819877c8. [DOI] [PubMed] [Google Scholar]
- 18.Olerud S, Sjöström L, Karlström G, Hamberg M. Spontaneous effect of increased stability of the lower lumbar spine in cases of severe chronic back pain: the answer of an external transpeduncular fixation test. Clin Orthop. 1986;203:67–74. [PubMed] [Google Scholar]
- 19.Park Y, Ha JW. Comparison of one level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007;32:537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 20.Polly DW, Jr, Potter BK, Kuklo T, Young S, Johnson C, Klemme WR. Volumetric spinal canal intrusion: a comparison between thoracic pedicle screws and thoracic hooks. Spine. 2004;29(1):63–69. doi: 10.1097/01.BRS.0000105525.06564.56. [DOI] [PubMed] [Google Scholar]
- 21.Prokop A, Löhlein F, Chmielnicki M, Volbracht J. Minimally invasive percutaneous instrumentation for spine fractures. Unfallchirurg. 2009;112:621–628. doi: 10.1007/s00113-008-1556-z. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez-Vela J, Lobo-Escolar A, Joven-Aliaga E, Herrera A, Vicente J, Sunen E, Loste A, Tabuenca A. Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur Spine J. 2009;18(8):1194–1201. doi: 10.1007/s00586-009-1010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soini J, Seitsalo S. The external fixation test of the lumbar spine: 30 complications in 25 of 100 consecutive patients. Acta Orthop Scand. 1993;64:147–149. doi: 10.3109/17453679308994556. [DOI] [PubMed] [Google Scholar]
- 24.Tiusanen H, Seitsalo S, Östermann K, Soini J. The role of external transpedicular fixation in anterior interbody lumbar fusion. J Spinal Disord. 1996;9:433–438. doi: 10.1097/00002517-199610000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein JN, Rydevik BL, Rausching WR. Anatomical and technical considerations of pedicle screw fixation. Clin Orthop. 1992;284:34–46. [PubMed] [Google Scholar]
- 26.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48:771–779. doi: 10.1097/00006123-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Zdichavsky M, Blauth M, Knop C, Graessner M, Herrmann H, Krettek C, Bastian L. Accuracy of pedicle screw placement in thoracic spine fractures. Part I: inter- and intra-observer reliability of the scoring system. Eur J Trauma. 2004;30:234–240. doi: 10.1007/s00068-004-1422-9. [DOI] [Google Scholar]
- 28.Zdichavsky M, Blauth M, Knop C, Lotz J, Krettek C, Bastian L. Accuracy of pedicle screw placement in thoracic spine fractures. Part II: a retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma. 2004;30:241–247. doi: 10.1007/s00068-004-1423-8. [DOI] [Google Scholar]
- 29.Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, Spencer CW. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99–112. [PubMed] [Google Scholar]