Abstract
Objective To evaluate whether a multifaceted behavioural change programme increases physical activities in patients with Parkinson’s disease.
Design Multicentre randomised controlled trial.
Setting 32 community hospitals in the Netherlands, collaborating in a nationwide network (ParkinsonNet).
Participants 586 sedentary patients with idiopathic Parkinson’s disease aged between 40 and 75 years with mild to moderate disease severity (Hoehn and Yahr stage ≤3).
Intervention Patients were randomly assigned to the ParkFit programme or a matched general physiotherapy intervention. ParkFit is a multifaceted behavioural change programme, designed specifically to achieve an enduring increase in the level of physical activity (coaches using motivational strategies; ambulatory feedback).
Main outcome measures The primary endpoint was the level of physical activity, measured every six months with a standardised seven day recall (LASA physical activity questionnaire—LAPAQ). Secondary endpoints included two other measures of physical activity (activity diary and ambulatory activity monitor), quality of life (Parkinson’s disease questionnaire—PDQ-39), and fitness (six minute walk test).
Results 540 (92.2%) patients completed the primary outcome. During follow-up, overall time spent on physical activities (LAPAQ) was comparable between the groups (adjusted group difference 7%, 95% confidence interval −3 to 17%; P=0.19). Analyses of three secondary outcomes indicated increased physical activity in ParkFit patients, as suggested by the activity diary (difference 30%; P<0.001), the activity monitor (difference 12%; P<0.001), and the six minute walk test (difference 4.8 m; P=0.05). PDQ-39 did not differ between ParkFit patients and controls (difference −0.9 points; P=0.14). The number of fallers was comparable between ParkFit patients (184/299; 62%) and controls (191/287; 67%).
Conclusions The ParkFit behavioural change programme did not increase overall physical activity, as measured with the LAPAQ. The analysis of the secondary endpoints justifies further work into the possible merits of behavioural change programmes to increase physical activities in daily life in Parkinson’s disease.
Trial registration Clinical trials NCT00748488.
Introduction
Parkinson’s disease is a common neurodegenerative disease, characterised by motor symptoms and a wide variety of non-motor symptoms such as depression and apathy.1 2 Despite optimal medical treatment, it remains a progressive disease that negatively affects quality of life. Therefore, allied health interventions are increasingly deployed to treat both the motor and non-motor symptoms of Parkinson’s disease. The evidence to support the merits of these interventions is growing, and treatment guidelines (based partially on evidence and partially on practical clinical experience) for several allied healthcare interventions have been developed.3 4 5
In recent years, several physiotherapy programmes have been tested in patients with Parkinson’s disease.6 7 8 9 10 Reviews and meta-analyses have generally found evidence to support “exercise” as being beneficial with regard to physical functioning, strength, balance, and gait speed.11 12 13 14 15 However, the physiotherapy programmes as tested in these studies were apparently insufficient to achieve an active lifestyle. Because of their combined physical limitations and mental changes, many patients with Parkinson’s disease lead a sedentary lifestyle.16 Reversing this lifestyle could have generic health benefits, including increased survival.17 18 19 Promoting physical activity may also improve specific symptoms of Parkinson’s disease, such as insomnia, depression, or constipation.20 Furthermore, work in rodents suggests that physical activity might counter neurodegeneration in experimental parkinsonism.21 22
An individually tailored, disease specific training programme is needed to improve physical activity in Parkinson’s disease.23 We developed such an intervention (the ParkFit programme24) based on models of behavioural change and containing established behavioural change techniques.25 26 27 28 29 To evaluate this programme, we designed a randomised controlled trial comparing ParkFit with a matched control intervention.24
Methods
The ParkFit trial is a multicentre randomised controlled trial to increase physical activity levels over the course of two years in sedentary patients with Parkinson’s disease. The study design has been detailed elsewhere.24
Study participants
Recruitment ran from September 2008 to January 2010. Patients treated in 32 community hospitals were invited to participate. Eligibility criteria were Parkinson’s disease according to UK Brain Bank criteria1; age 40-75 years; sedentary lifestyle, defined as participation in physical activity of vigorous intensity less than three times a week and for less than 60 minutes in total per week or participation in moderate intensity physical activity less than three times a week and for less than 150 minutes in total per week23; and Hoehn and Yahr stage 3 or lower. Exclusion criteria were mini-mental state examination score less than 24/30, inability to complete Dutch questionnaires, co-morbidity that interfered with daily functioning, daily institutionalised care, and previous deep brain surgery. All participants gave informed consent before the first assessment.
Study outcomes
Baseline characteristics
We scored disease stage according to the modified Hoehn and Yahr scale and assessed motor function by using the unified Parkinson’s disease rating scale (UPDRS part III, motor examination).
Primary endpoint
We made several amendments to the endpoints in the initial phase of the study, at a time when recruitment was under way for only two months. We here report our final selection of endpoints, as specified on ClinicalTrials.gov, in the adapted final research protocol that was accepted by the Ethical Committee (CMO) Arnhem Nijmegen, and in a recent design article.24
The primary endpoint was the LASA physical activity questionnaire (LAPAQ)—a validated, interview based, seven day recall of physical activities. The LAPAQ was highly correlated with a seven day diary (r=0.68; P<0.001) and moderately correlated with a pedometer (r=0.56; P<0.001).30 It asks patients about their daily amount of specific activities, allowing for calculation of total time spent on physical activities (expressed in hours per week). The LAPAQ covers the frequency and duration of the net sum of the following activities: walking outdoors, cycling, gardening, light and heavy household activities, and sport activities.30 Consequently, higher scores on the LAPAQ (in hours per week) indicated more time spent on physical activity. We measured LAPAQ at baseline and after 6, 12, 18, and 24 months. At baseline and after 12 and 24 months, LAPAQ was completed during face to face interviews; after six and 18 months, it was completed by telephone. We assumed that patients would increase their level of physical activity during the first months of the intervention and would then maintain this level. Therefore, the main endpoint was the average of the level of physical activity during the entire follow-up period (that is, the average of 6, 12, 18, and 24 months). This approach has several advantages. Firstly, it provides a global assessment of the results of the intervention. Secondly, it provides maximal power. As the number of assessments taken into account increases, so does the power. We did not compare all individual time points (at 6, 12, 18, and 24 months) separately, because this leads to multiplicity.
Secondary endpoints
We defined four secondary endpoints24: physical fitness, as measured with the six minute walk test at 12 and 24 months (average of all measurements)31; quality of life, as measured with the Parkinson’s disease questionnaire (PDQ-3932) at 6, 12, 18, and 24 months (the average of all measurements); physical activity, measured subjectively every six months with a seven day activity diary (average of all measurements);33 and physical activity, measured objectively every six months with an ambulatory activity monitor (average of all measurements).34
The diary detailed the frequency and total duration (hours/week) spent on five specific activities: walking outdoors for more than 10 contiguous minutes, moderate intensity cycling for more than 10 contiguous minutes, high intensity cycling for more than 10 contiguous minutes, sport activities, and other strenuous activities (such as cutting wood). Participants wore the activity monitor (triaxial accelerometer34) as a necklace, on the belt, or in the pocket. Data were collected during waking hours for 14 days and were stored minute by minute for each axis; output was expressed in kilocalories/minute. We included only completely observed days in the analysis.35 Patients allocated to the ParkFit programme additionally used the monitor as a feedback tool by using light emitting diodes that reflected the amount of actually delivered daily physical activity. Control patients received no feedback from their activity monitor.
Safety and falls
We assessed safety by spontaneous reports of adverse events. We classified serious adverse events as events that caused death, were life threatening, or necessitated admission to hospital. We monitored falls monthly with an automated telephone system.36 Information about adverse events was additionally collected at each physical assessment.
Intervention
After baseline assessment, patients were randomly assigned to either the ParkFit programme or a matched physiotherapy intervention aimed at safety of movements. The investigators logged on to a protected website and entered the region, Hoehn and Yahr stage, age, sex, and current physical activity level of the patients. On the basis of a minimisation algorithm with these factors, the treatment was allocated and registered. Before inclusion, patients were informed that the trial compared two potentially beneficial interventions. We used “active” names for both interventions (the “ParkFit” and “ParkSafe” programmes). To ensure blinding, trained assessors who were unaware of group allocation examined patients. Patients were instructed not to discuss the nature of their physiotherapy with the assessors.
Experienced physiotherapists in the Dutch ParkinsonNet delivered both interventions.37 In total, 154 physiotherapists were trained to deliver both interventions. This ascertained that differences in the personality or style of the physiotherapists could not bias the results. All patients were offered an equal maximum number of treatment sessions (35/year). The full study protocol has been described elsewhere.24
ParkFit programme
We designed the ParkFit programme specifically to achieve a sustained increase in physical activity levels, on the basis of theories and models of behavioural change and on effective behavioural change techniques.25 26 27 28 29 Important elements were activity coaches who guided each patient towards a more active lifestyle during monthly personal coaching sessions; an educational brochure about the benefits of physical activity and suitable activities for patients with Parkinson’s disease; identifying and overcoming any perceived barriers to engaging in physical activity; systematic goal setting, using a health contract and logbook; stimulation to participate in group exercises; and an ambulatory monitor with automated feedback reflecting actually delivered physical activities.34 Ambulatory monitor data were uploaded to a personalised website, where both the patient and coach could monitor progress.
The ParkFit programme also included regular physiotherapy sessions. On the basis of individual disabilities, the therapist and patient jointly formulated individually tailored aims of treatment aims, according to the evidence based guideline for physiotherapy in Parkinson’s disease.3
Control intervention
The control intervention consisted of a general physiotherapy programme aimed at promoting safety of movements, according to the evidence based guideline.3 Patients received an identical brochure to ParkFit patients, but with information about the benefits of physiotherapy and safety of movements. Patients were offered a maximum number of treatment sessions, similar to the ParkFit programme. An active lifestyle was not explicitly stimulated. Treatment aims were jointly formulated by therapist and patient, on the basis of perceived individual disabilities.
Statistical analysis
The main endpoint was the physical activity level during the entire follow-up (6, 12, 18, and 24 months). Because the physical activity level was skewed, we present medians and interquartile ranges and did analyses after logarithmic transformation. We evaluated differences between the two interventions by using a linear mixed model with random nested factors of “patient” and “exercise group.” We included region, Hoehn and Yahr stage, age, sex, and current physical activity level of the patient as covariables. We analysed results according to a modified intention to treat principle, whereby we excluded only patients with no follow-up measurements at all.
Sample size calculation
On the basis of the following power considerations, we aimed to include a total of 700 patients. In a small observational study on physical activity in Parkinson’s disease, patients scored 45% less than controls on the LAPAQ (unpublished data). The coefficient of variation was 110%. On the basis of a difference of 20% in hours per week (with a coefficient of variation of 110%) between the two treatment arms, the mixed model analysis will have at least 80% power (when the correlation between baseline and follow-up measurements is at least 0.50 and when the correlation between the various follow-up measurements is at most 0.75). The decision to define a 20% increase based on the LAPAQ activity as a clinically relevant difference was a pragmatic choice, because no earlier intervention studies had aimed to change activity behaviour in Parkinson’s disease patients. Moreover, previous behavioural change studies in other diseases (such as heart failure, diabetes, and chronic obstructive pulmonary disease) did not include the LAPAQ as an endpoint. In an earlier study by our group,16 we found that patients with Parkinson’s disease were 29% less active than controls (as measured with the LAPAQ): patients spent 12.9 hours per week on physical activity, whereas controls spent more than 17.5 hours. We deemed an increase in physical activity among Parkinson’s disease patients of more than four hours to be unrealistic and reasoned that an increase of two hours per week (that is, an increase of about 20%) would be feasible. We also considered a two hour increase in physical activity to be clinically relevant, for the following reasons. A dose-response relation exists between physical activity and cardiovascular disease or premature mortality.38 Significant risk reductions have been observed with 45-150 minutes a week of brisk walking.39 Additionally, women who walked or exercised vigorously for at least 2.5 hours a week had a 30% lower risk of coronary heart disease.39 Conversely, the risk of cardiovascular disease was higher among women who spent more than 12 hours a day lying down or sleeping.39 This suggests that a two hour increase in physical activities might help to prevent cardiovascular disease. The power is based on two sided 95% confidence intervals. We assumed that the clustering due to the fact that the intervention was carried out in training groups of approximately eight patients leads to an intraclass correlation coefficient of 0.1. On the basis of a previous trial of physical therapy in Parkinson’s disease,37 we expected a dropout rate of 10%.
Results
Baseline characteristics
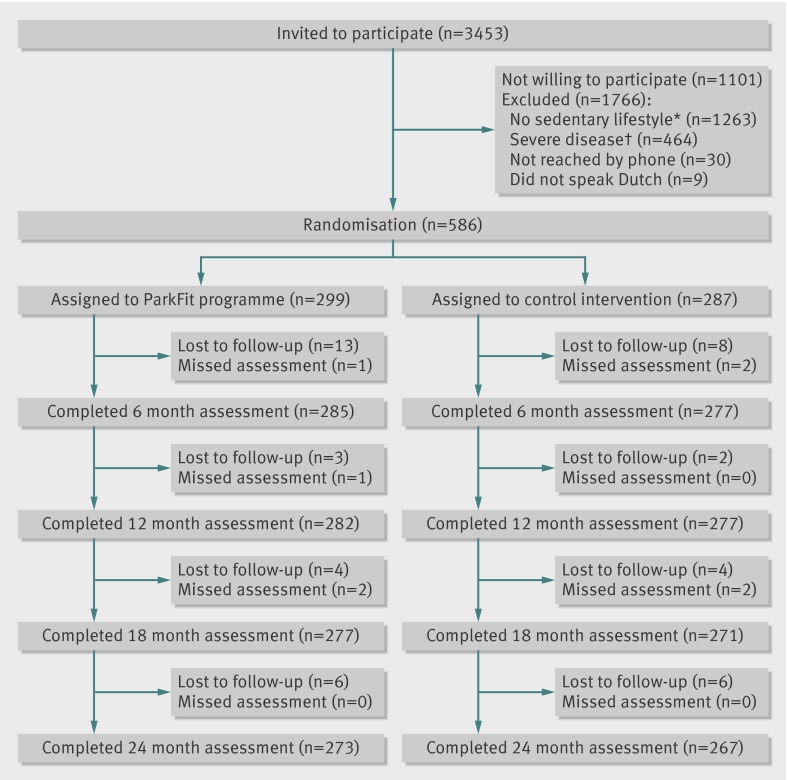
We included 586 patients (figure); 299 patients were randomly assigned to the ParkFit programme and 287 to the control intervention. The groups had comparable demographic and disease characteristics, although ParkFit patients tended to be less active than controls in daily life (that is, spent less time spent on physical activity according to LAPAQ) (table 1).
Screening, randomisation, and completion of primary outcome measure. *Vigorous intensity physical activity >3 times/week and >60 minutes/week or moderate intensity physical activity >3 times/week and >150 minutes/week. †Hoehn and Yahr stage >3, mini-mental state examination <24/30, severe comorbidity interfering with daily functioning, daily care in institution, or deep brain stimulation
Table 1.
Baseline characteristics
| ParkFit (n=299) | Controls (n=287) | |
|---|---|---|
| Demographics and clinical characteristics | ||
| Mean (SD) age (years) | 65.1 (7.9) | 65.9 (7.2) |
| Male sex | 194 (65) | 188 (65) |
| Mean (SD) body mass index | 27.4 (4.5) | 27.6 (4.0) |
| Mean (SD) disease duration (years) | 5.0 (4.5) | 5.5 (4.6) |
| Mean (SD) mini-mental state examination score | 28.1 (1.7) | 28.1 (1.7) |
| Modified Hoehn and Yahr stage (No (%)): | ||
| 1 | 7 (2) | 4 (1) |
| 1.5 | 7 (2) | 10 (3) |
| 2 | 221 (74) | 223 (78) |
| 2.5 | 48 (16) | 36 (13) |
| 3 | 16 (5) | 14 (5) |
| Mean (SD) unified Parkinson’s disease rating scale, part III | 33.1 (11.3) | 32.3 (9.5) |
| Mean (SD) daily levodopa equivalent dose (mg) | 458 (362) | 499 (414) |
| Level of physical activity | ||
| Median (interquartile range) LAPAQ (hours per week) | 12.8 (8.3-20.3) | 13.8 (8.3-23.9) |
LAPAQ = LASA physical activity questionnaire.
Loss to follow-up
In total, 540 (92.2%) of the 586 participants completed the LAPAQ after 24 months. The proportion of patients lost to follow-up was comparable for ParkFit (8.7%) and controls (6.7%). Patients lost to follow-up were similar to those who completed the assessments, except for a higher age.
Compliance
Seventy five (12.8%) of the 586 participants did not complete the two year intervention (ParkFit n=44, control n=31). The main reasons were refusal to change from a regular physiotherapist to a ParkinsonNet physiotherapist, too great a burden, or dissatisfaction with the intervention. Reasons for drop out were similar between the two groups. The mean number of annual individual visits to the physiotherapist did not differ between ParkFit (13.6) and control patients (13.0). Patients in both groups were satisfied with the intervention and would recommend the intervention to others (186 (73%) ParkFit v 182 (71%) controls).
Endpoints
Primary endpoint
Compared with baseline, the overall time spent in physical activities was comparable between the two groups (adjusted group difference 7%, 95% confidence interval −3% to 17%; P=0.19) (table 2).
Table 2.
Effect of intervention (in hours/week) on level of physical activity measured with LASA physical activity questionnaire (LAPAQ; primary outcome)
| Time point | ParkFit | Controls | Estimated difference (95% CI)* | P value | |||
|---|---|---|---|---|---|---|---|
| No | Median (IQR) | No | Median (IQR) | ||||
| Baseline | 299 | 12.8 (8.3-20.3) | 287 | 13.8 (8.3-23.9) | 7% (−3% to 17%) | 0.19 | |
| 6 months | 285 | 13.2 (9.2-20.5) | 277 | 14.2 (8.5-22.0) | |||
| 12 months | 281 | 12.5 (7.2-21.1) | 277 | 12.4 (7.3-17.9) | |||
| 18 months | 277 | 12.3 (7.0-19.0) | 271 | 12.3 (6.8-19.1) | |||
| 24 months | 273 | 12.5 (6.3-18.4) | 267 | 12.0 (7.0-18.3) | |||
IQR=interquartile range.
*Estimated relative difference, based on mixed model analysis.
Secondary endpoints
Both the activity diary and the activity monitor data suggested increased levels of physical activity in ParkFit patients (table 3). Additionally, ParkFit patients increased their physical fitness compared with controls (4.8 m, 0.1 to 9.6; P=0.05). Quality of life did not differ between the groups (−0.9 points, −2.1 to 0.3; P=0.14).
Table 3.
Effect of intervention on secondary outcome measures
| ParkFit | Controls | Estimated difference (95% CI)* | P value | ||||
|---|---|---|---|---|---|---|---|
| No | Effect of intervention | No | Effect of intervention | ||||
| Activity diary—median (interquartile range) hours/week | |||||||
| Baseline | 297 | 5.5 (3.1-10.3) | 282 | 6.3 (3.3-10.5) | |||
| 6 to 24 months | 276 | 7.6 (4.7-12.4) | 276 | 6.9 (4.2-10.8) | |||
| Mean change | 275 | 1.3 | 273 | 0.5 | 30% (17% to 45%) | <0.001 | |
| Activity monitor—median (interquartile range) kcal/day | |||||||
| Baseline | 273 | 453 (368-618) | 269 | 462 (346-604) | |||
| 6 to 24 months | 269 | 504 (390-667) | 269 | 440 (355-582) | |||
| Mean change | 254 | 38.7 | 258 | −14.2 | 12% (7% to 16%) | <0.001 | |
| Quality of life—mean (SD) Parkinson’s disease questionnaire (PDQ-39) | |||||||
| Baseline | 297 | 26.0 (13.7) | 286 | 26.2 (13.1) | |||
| 6 to 24 months | 278 | 26.4 (13.7) | 277 | 27.7 (12.7) | |||
| Mean change | 278 | 0.1 | 276 | 1.7 | −0.9 (−2.1 to 0.3) | 0.14 | |
| Physical fitness—mean (SD) six minute walk test (6MWT) | |||||||
| Baseline (distance in m) | 298 | 391.6 (87.5) | 283 | 392.9 (84.5) | |||
| 12 and 24 months | 256 | 404 (95.1) | 256 | 394.4 (86.5) | |||
| Mean change | 255 | 8.4 | 253 | −1.6 | 4.8 (0.1 to 9.6) | 0.05 | |
*Estimated (relative) difference, based on analysis of covariance.
Safety and falls
Eight patients died during follow-up because of cardiovascular problems, cancer, or medical complications (ParkFit n=5, control n=3). These deaths were unrelated to exercise sessions. Controls reported eight hip fractures, and ParkFit patients reported two. The frequency and severity of all other adverse events were similar in the two groups (ParkFit n=221, control n=242). The number of patients with one or more falls was comparable in the two groups: 184 (62%) in ParkFit and 191 (67%) in controls.
Discussion
This randomised controlled trial showed that a multifaceted behavioural change programme does not promote overall physical activities, as measured with the primary outcome (LASA physical activity questionnaire—LAPAQ), in sedentary patients with Parkinson’s disease. Two of our secondary outcomes focused on other measures of physical activity and did suggest improvements for patients allocated to the ParkFit programme. This was shown both subjectively (with activity diaries) and objectively (with an ambulatory activity monitor). Moreover, physical fitness (an indirect reflection of greater physical activity) increased in ParkFit patients. Quality of life did not differ between the two study arms. The ParkFit group did not have more falls.
Possible explanations for findings
The ParkFit study is therefore a negative trial, showing no difference for the primary outcome (LAPAQ questionnaire) between the study arms. We selected the LAPAQ as primary outcome because it closely reflected the goals of the ParkFit intervention—namely, promotion of physical activities. We regarded an actual increase in physical activity levels as a necessary intermediate and prerequisite to eventually obtain health benefits, including improvements in quality of life. The LAPAQ questionnaire is a validated instrument to measure habitual physical activity in large populations.30 40 LAPAQ covers a wide range of daily life activities, and we previously showed that patients with Parkinson’s disease are 29% less active than controls, as measured with the LAPAQ.16 Our study was powered to defect a 20% increase based on the LAPAQ, which would equate to an increase in physical activities of two hours a week. The ParkFit programme did not achieve this, suggesting that more robust interventions are needed to promote physical activities in daily life.
Our choice of control intervention might have obscured greater differences on the LAPAQ between ParkFit patients and controls. We chose to refer patients in the control arm to a physiotherapist who aimed to improve the safety of movements, but without emphasising the volume of physical activities. This approach helped to maintain blinding of patients with respect to treatment allocation. An additional reason for having a physiotherapy programme as control intervention was that abstaining control patients from physiotherapy for two years was considered unethical, in the light of growing evidence for the effectiveness of specific physiotherapy interventions.11 13 14 15 Furthermore, the ParkFit study took place in the “real world,” and physiotherapy in Parkinson’s disease is “usual care,” not only in the Netherlands (where at least 60% of Parkinson’s disease patients receive physiotherapy annually)4 but also in the United Kingdom.41
Although we found no effect on the primary outcome, two of our secondary outcomes did pick up an increase in physical activities, as measured both subjectively (activity diary) and objectively (activity monitors). According to the diary, ParkFit patients spent almost 1.5 hours a week extra on physical activity, compared with baseline. This differed significantly from controls, who increased their level of physical activity by 30 minutes compared with baseline. This amount of increase in physical activity, as observed with the diary, is comparable to findings in older populations and patients with other chronic conditions.42 43 44 45 For example, behavioural counselling for older patients in primary care yielded a one hour increase in moderate intensity physical activity.42 In addition, pedometer based counselling programmes increased the total physical activity of cardiac patients by almost 1.5 hours a week.43 44 Both the LAPAQ and the diary are subjective instruments, but only the diary showed increased activity levels. One possible explanation for this discrepancy is the fact that the diary merely includes strenuous activities, whereas the LAPAQ questionnaire reflects the net sum of all physical activities (including household activities). Therefore, we cannot exclude that a possible increase in (strenuous) outdoor and sporting activities for ParkFit patients was offset by a concurrent decrease in household activities. The LAPAQ cannot capture such differential effects on specific physical activities, as it merely measures the net sum of all physical activities. We therefore regard our decision to select overall physical activity as primary outcome as a shortcoming in the study design, and this aspect should be included in future research in this area.
Objective assessment of physical activity using a triaxial accelerometer showed an increase in physical activities for ParkFit patients, with a 12% increase in time spent on physical activity after 24 months. Generally, accelerometers underestimate total energy expenditure, because some activities are difficult to detect. This includes upper body movements, specific activities such as cycling, and relatively static movements such as gardening or strength training.33 On the other hand, accelerometers as used in our study can reliably measure activities such as indoor and outdoor walking.34 46 The accelerometers thus measured a different aspect of physical activity than the LAPAQ, and this could explain the difference in outcome from the LAPAQ. Compliance with use of the accelerometers was good, suggesting that it is a feasible surrogate outcome in future studies.
The two remaining secondary outcomes aimed at finding possible health benefits. Physical fitness showed a small but significant difference in favour of ParkFit, but quality of life did not differ between the ParkFit and control intervention. The ParkFit intervention had no major adverse effects. We were concerned about possibly increased fall rates, because amount of physical activity is associated with a greater risk of falling.47 However, the ParkFit programme was not associated with more falls or injuries. In fact, controls reported eight hip fractures, whereas ParkFit patients reported only two. However, these numbers are very small and this finding is coincidental as we did not include hip fractures as a primary or secondary outcome. Therefore, further research should investigate whether this difference in hip fractures is related to the intervention. Another concern was cardiovascular complications due to more strenuous activities. All participants received a sports health assessment before participation. We observed two cardiovascular deaths in the ParkFit group, but these were unrelated to exercise. Other adverse effects were comparable between the groups. Taken together, this suggest that ParkFit was a safe intervention but that the programme needs to be adjusted to achieve more substantial increases in physical activity that translate into tangible health improvements.
Implications for trial design
Our experience with this ParkFit study was a lesson in trial design in this newly emerging field. Although the primary outcome was negative, we have shown the possibility of an exercise based trial in disabled people. Several features set the ParkFit study apart from previous exercise studies: the prolonged follow-up, showing that patients in both arms were able to comply with the intervention for two years; the careful matching of treatment intensity between the study arms; the large sample size, making the ParkFit trial by far the largest study on physical activity in Parkinson’s disease and other chronic diseases11 20 43 44; and the excellent follow-up rate. The feasibility of the study was supported by the ParkinsonNet infrastructure, a nationwide network of allied health professionals who are specialised in Parkinson’s disease.48 A generic challenge for trials aiming to evaluate the merits of allied health treatment is the lack of expertise among therapists who deliver the trial intervention, creating undesirable variability and insufficient contrast with the control arm. Having expert therapists within ParkinsonNet greatly facilitates the delivery of a relatively uniform intervention according to treatment guidelines.37 49
As discussed above, our study also highlights the challenges of selecting the appropriate outcomes for a complex intervention such as a behavioural change programme. Physical activity is a complex behaviour: it includes sports as well as non-sports activities, and it can be characterised by purpose (occupational or leisure), type (cycling, fitness, or soccer), intensity (light, moderate, or vigorous), and duration. Further research should focus on comprehensive, valid, and reliable instruments to accurately measure all these aspects of physical activity behaviour. This is a specific challenge in patients with chronic diseases, as they perform more light and moderate activities that are easily overestimated when using questionnaires and are difficult to detect with activity monitors.
Furthermore, our trial provided new insights in the risk of selection bias. Our participants were on average less sedentary than patients who declined to participate.24 Hence, those who needed to promote their physical activities were most likely to refuse participation. Whether the effects found here can be generalised to more sedentary Parkinson’s disease patients therefore remains unclear. Nor can we extend our findings to patients with severe apathy, severe cognitive impairment, or depression, because these were excluded. Finally, the ParkFit programme was a multifaceted intervention, with coaches using behavioural change techniques, ambulatory feedback devices, and peer pressure from group exercises. Future work should decide which of these components is most effective and if any component is also effective when used alone.
Conclusion
ParkFit, a multifaceted behavioural change programme, did not change the overall volume of physical activities in older, sedentary patients with Parkinson’s disease. However, analysis of the secondary outcomes suggested greater participation in specific elements of physical activity and showed an improved fitness among ParkFit patients. These results for the secondary outcomes suggest that replicating a similar behavioural change study—for example, with the secondary outcomes as primary parameters—may be worthwhile. Such a trial might also put more focus on the quality of life and cost aspects.
What is already known on this topic
Many patients with Parkinson’s disease adopt a sedentary lifestyle because of motor and non-motor disability
Patients with Parkinson’s disease might benefit from physical activity and exercise, but how they can be motivated to change their sedentary lifestyle and persistently increase their level of physical activities remains unclear
What this study adds
The ParkFit behavioural change programme did not increase the overall volume of all physical activities
Greater participation in specific elements of physical activity and an improved fitness were seen among ParkFit patients, without more falls and without a change in quality of life
This study shows the possibility of an exercise based trial in disabled people and highlights several challenges for future studies, in particular with regard to the choice of outcome measures of physical activity
We thank all patients and physiotherapists for participation. We thank T Roordink, M Gerrits, W Trompers, M Weijers, A Vinke, K van Geel, M Post, J Mulder, T Remijn, Y Cornelissen, and I Wijnhoven for their contribution during recruitment and data collection. We thank Mark Massa and Wim Lemmens for their contribution to the data analysis. We thank Bert de Swart and the HAN University of Applied Sciences for organising the temporary participation of many students in the project team of the study. We thank all students for their contribution during the data collection. Furthermore, we thank J W Custers and P J van der Wees (Royal Dutch Society for Physiotherapy), S I Detaille and V Peters (Seneca, Expertise Centre for Sport, Work and Health, HAN University of Applied Sciences), M T Hopman (Department of Physiology, Radboud University Nijmegen Medical Centre), M W A Jongert (TNO Netherlands Organization for Applied Scientific Research), Y P T Kamsma (University Medical Center Groningen), S H J Keus (Departments of Physical Therapy and Neurology, Leiden University Medical Centre; Department of Neurology, Donders Institute for Brain, Cognition and Behavior, Radboud University Nijmegen Medical Centre), G Kwakkel (VU University Medical Center), H Leutscher (Disability Sports Netherlands), W Oerlemans (HAN University of Applied Sciences), C J M van Santen (Society of Exercise Therapists Cesar and Mensendieck), N H M J van Velthoven (Netherlands Olympic Committee; Netherlands Sports Federation), A M J van de Wert (Netherlands Institute for Sport and Physical Activity), and T Wolff (Parkinson Vereniging) for their participation in the ParkFit advisory board.
ParkFit Study Group: A Winogrodzka (Academisch Ziekenhuis Maastricht); J C M Zijlmans (Amphia Ziekenhuis); G J Tissingh (Atrium Medisch Centrum); K Keizer (Catharina-ziekenhuis); H J M M Lohmann (Deventer Ziekenhuis); R van Koningsveld (Elkerliek Ziekenhuis); A J W Boon (Erasmus Medisch Centrum); E van Wensen and F E Strijks (Gelre Ziekenhuizen); G A van Meer (Groene Hart Ziekenhuis); A Mosch (HagaZiekenhuis); J P ter Bruggen (Jeroen Bosch Ziekenhuis); M F Roesdi (Kennemer Gasthuis); E Berger (‘t Lange Land Ziekenhuis and Medisch Centrum Haaglanden); A G G C Korten (Laurentius Ziekenhuis); M Westerink (Maasstad Ziekenhuis); M Aramideh (Medisch Centrum Alkmaar); R Rundervoort (Medisch Centrum Haaglanden); F A Rooyer (Orbis Medisch Centrum); D J Kamphuis (Reinier de Graaf Groep); G J de Jong (Sint Franciscus Gasthuis); L van Hooff (Franciscus Ziekenhuis); K Lemmen (Slingeland Ziekenhuis); Th J M Breuer (St Anna Ziekenhuis); J M J Krul and P M Laboyrie (Tergooiziekenhuizen); F J W Opstelten (VieCuri Medisch Centrum); A M G Sas (Vlietland Ziekenhuis); P J Nederveen (Westfriesgasthuis), J Lion (Ziekenhuis Bernhoven); and C Jansen (Ziekenhuis Gelderse Vallei).
Contributors: MvN and ADS contributed equally to this work. MM, BRB, and FJGB wrote the grant application and supervised all project staff. MvN, ADS, GFB, FJGB, BRB, MM, and members of the ParkFit Study Group contributed to the research design. MvN, ADS, KS, and MM participated in recruitment of patients and data collection. MvN, ADS, and MM contributed to implementation of the intervention and took responsibility for the education of physiotherapists. GFB was responsible for the sample size calculation and devised the statistical analyses and presentation of the results. MvN, ADS, SO, BPvdW, GFB, MM, and BRB took responsibility for data analysis and interpretation. MvN, ADS, SO, and MM wrote first draft of the manuscript. All authors reviewed the final draft. GFB is the guarantor.
Funding: This study was primarily funded by ZonMw (the Netherlands Organization for Health Research and Development (75020012)) and the Michael J Fox Foundation for Parkinson’s research. Additional financial support was provided by VGZ (health insurance company), GlaxoSmithKline, and the National Parkinson Foundation. The study sponsors played no role in study design; in the data collection, analysis, and interpretation; or in the writing of the article and the decision to submit it for publication; all researchers’ activities were independent of the funding source; the research team had full and unrestricted access to all the data.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work (other than those listed under funding); SO is supported by a VIDI grant from the Netherlands Organization for Scientific Research (016.116.371) and has received honorariums for serving on scientific advisory boards for Boehringer Ingelheim, UCB Pharma, and Novartis; GFB received a grant from ZonMw and is a consultant for the pharmaceutical companies Synthon and Panta Rhei; BPW has received research support from the European Union, the Prinses Beatrix Fonds, the Dutch Brain Foundation, Ipsen Pharmaceuticals, the Gossweiler Foundation, and the Royal Dutch Society for Physiotherapy; FJGB has received grants from ZonMw and the Dutch Diabetes Fund; BRB has served as an editorial board member for Movement Disorders, currently serves as an editorial board member for Physiotherapy Canada, is associate editor for the Journal of Parkinson’s Disease, and has received honorariums for serving on scientific advisory boards for Boehringer Ingelheim, Teva, GlaxoSmithKline, and Novartis and research support from the Netherlands Organization for Scientific Research (016.076.352), the Michael J Fox Foundation, the Prinses Beatrix Foundation, the Stichting Internationaal Parkinson Fonds, and the Alkemade Keuls fonds; MM has received grants from ZonMw, the Michael J Fox Foundation, the National Parkinson Foundation, the Dutch Parkinson’s Disease Society, and the Prinses Beatrix Fonds.
Ethical approval: Full ethical approval has been granted for the study (CMO Regio Arnhem-Nijmegen). Written informed consent was given by all patients before enrolment in the trial.
Data sharing: Requests for analyses of de-identified data from this trial should be directed to Marten Munneke (M.Munneke@neuro.umcn.nl).
Cite this as: BMJ 2013;346:f576
References
- 1.Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol 1999;56:33-9. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009;8:464-74. [DOI] [PubMed] [Google Scholar]
- 3.Keus SH, Bloem BR, Hendriks EJ, Bredero-Cohen AB, Munneke M. Evidence-based analysis of physical therapy in Parkinson’s disease with recommendations for practice and research. Mov Disord 2007;22:451-60. [DOI] [PubMed] [Google Scholar]
- 4.Sturkenboom IHWM, Thijssen MCE, Gons-van Elsacker JJ, Jansen IJH, Maasdam A, Schulten M, et al. Ergotherapie bij de ziekte van Parkinson, een richtlijn van Ergotherapie Nederland. Ergotherapie Nederland/Uitgeverij Lemma, 2008.
- 5.Kalf JG, de Swart BJM, Bonnier MWJ, Hofman MFC, Kanters JHM, Kocken JEM, et al. Logopedie bij de ziekte van Parkinson, een richtlijn van de Nederlandse Vereniging voor Logopedie en Foniatrie. NVLF/Uitgeverij Lemma, 2008.
- 6.Hirsch MA, Toole T, Maitland CG, Rider RA. The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson’s disease. Arch Phys Med Rehabil 2003;84:1109-17. [DOI] [PubMed] [Google Scholar]
- 7.Morris ME, Iansek R, Kirkwood B. A randomized controlled trial of movement strategies compared with exercise for people with Parkinson’s disease. Mov Disord 2009;24:64-71. [DOI] [PubMed] [Google Scholar]
- 8.Ridgel AL, Vitek JL, Alberts JL. Forced, not voluntary, exercise improves motor function in Parkinson’s disease patients. Neurorehabil Neural Repair 2009;23:600-8. [DOI] [PubMed] [Google Scholar]
- 9.Ellis T, de Goede CJ, Feldman RG, Wolters EC, Kwakkel G, Wagenaar RC. Efficacy of a physical therapy program in patients with Parkinson’s disease: a randomized controlled trial. Arch Phys Med Rehabil 2005;86:626-32. [DOI] [PubMed] [Google Scholar]
- 10.Toole T, Maitland CG, Warren E, Hubmann MF, Panton L. The effects of loading and unloading treadmill walking on balance, gait, fall risk, and daily function in parkinsonism. NeuroRehabilitation 2005;20:307-22. [PubMed] [Google Scholar]
- 11.Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL. The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2008;23:631-40. [DOI] [PubMed] [Google Scholar]
- 12.Alonso-Frech F, Sanahuja JJ, Rodriguez AM. Exercise and physical therapy in early management of Parkinson disease. Neurologist 2011;17(6 suppl 1):S47-53. [DOI] [PubMed] [Google Scholar]
- 13.Deane KH, Jones D, Playford ED, Ben-Shlomo Y, Clarke CE. Physiotherapy for patients with Parkinson’s Disease: a comparison of techniques. Cochrane Database Syst Rev 2001;(3):CD002817. [DOI] [PubMed] [Google Scholar]
- 14.Mehrholz J, Friis R, Kugler J, Twork S, Storch A, Pohl M. Treadmill training for patients with Parkinson’s disease. Cochrane Database Syst Rev 2010;(1):CD007830. [DOI] [PubMed] [Google Scholar]
- 15.Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, et al. Physiotherapy intervention in Parkinson’s disease: systematic review and meta-analysis. BMJ 2012;345:e5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Nimwegen M, Speelman AD, Hofman-van Rossum EJ, Overeem S, Deeg DJ, Borm GF, et al. Physical inactivity in Parkinson’s disease. J Neurol 2011;258:2214-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997;349:1436-42. [DOI] [PubMed] [Google Scholar]
- 18.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747-57. [DOI] [PubMed] [Google Scholar]
- 19.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ 2006;174:801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Speelman AD, van de Warrenburg BP, van Nimwegen M, Petzinger GM, Munneke M, Bloem BR. How might physical activity benefit patients with Parkinson disease? Nat Rev Neurol 2011;7:528-34. [DOI] [PubMed] [Google Scholar]
- 21.Petzinger GM, Walsh JP, Akopian G, Hogg E, Abernathy A, Arevalo P, et al. Effects of treadmill exercise on dopaminergic transmission in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-lesioned mouse model of basal ganglia injury. J Neurosci 2007;27:5291-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tillerson JL, Caudle WM, Reveron ME, Miller GW. Exercise induces behavioral recovery and attenuates neurochemical deficits in rodent models of Parkinson’s disease. Neuroscience 2003;119:899-911. [DOI] [PubMed] [Google Scholar]
- 23.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1435-45. [DOI] [PubMed] [Google Scholar]
- 24.Van Nimwegen M, Speelman AD, Smulders K, Overeem S, Borm GF, Backx FJ, et al. Design and baseline characteristics of the ParkFit study, a randomized controlled trial evaluating the effectiveness of a multifaceted behavioral program to increase physical activity in Parkinson patients. BMC Neurol 2010;10:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143-64. [DOI] [PubMed] [Google Scholar]
- 26.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38-48. [DOI] [PubMed] [Google Scholar]
- 27.Brodie DA, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. J Adv Nurs 2005;50:518-27. [DOI] [PubMed] [Google Scholar]
- 28.Hospes G, Bossenbroek L, ten Hacken NH, van HP, de Greef MH. Enhancement of daily physical activity increases physical fitness of outclinic COPD patients: results of an exercise counseling program. Patient Educ Couns 2009;75:274-78. [DOI] [PubMed] [Google Scholar]
- 29.Haber D, Rhodes D. Health contract with sedentary older adults. Gerontologist 2004;44:827-35. [DOI] [PubMed] [Google Scholar]
- 30.Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P. Comparison of the LASA physical activity questionnaire with a 7-day diary and pedometer. J Clin Epidemiol 2004;57:252-8. [DOI] [PubMed] [Google Scholar]
- 31.Enright PL, McBurnie MA, Bittner V, Tracy RP, McNamara R, Arnold A, et al. The 6-min walk test: a quick measure of functional status in elderly adults. Chest 2003;123:387-98. [DOI] [PubMed] [Google Scholar]
- 32.Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The Parkinson’s disease questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing 1997;26:353-7. [DOI] [PubMed] [Google Scholar]
- 33.Welk GJ. Physical activity assessments for health-related research. Human Kinetics Publishers, 2002.
- 34.Bonomi AG, Plasqui G, Goris AH, Westerterp KR. Estimation of free-living energy expenditure using a novel activity monitor designed to minimize obtrusiveness. Obesity 2010;18:1845-51. [DOI] [PubMed] [Google Scholar]
- 35.Catellier DJ, Hannan PJ, Murray DM, Addy CL, Conway TL, Yang S, et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc 2005;37(11 suppl):S555-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van der Marck MA, Overeem S, Klok PC, Bloem BR, Munneke M. Evaluation of the falls telephone: an automated system for enduring assessment of falls. J Am Geriatr Soc 2011;59:340-4. [DOI] [PubMed] [Google Scholar]
- 37.Munneke M, Nijkrake MJ, Keus SH, Kwakkel G, Berendse HW, Roos RA, et al. Efficacy of community-based physiotherapy networks for patients with Parkinson’s disease: a cluster-randomised trial. Lancet Neurol 2010;9:46-54. [DOI] [PubMed] [Google Scholar]
- 38.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081-93. [DOI] [PubMed] [Google Scholar]
- 39.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med 2002;347:716-25. [DOI] [PubMed] [Google Scholar]
- 40.Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med 2003;37:197-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parkinson’s disease: national clinical guideline for diagnosis and management in primary and secondary care. Royal College of Physicians of London, 2006. [PubMed]
- 42.Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med 2005;29:247-55. [DOI] [PubMed] [Google Scholar]
- 43.Butler L, Furber S, Phongsavan P, Mark A, Bauman A. Effects of a pedometer-based intervention on physical activity levels after cardiac rehabilitation: a randomized controlled trial. J Cardiopulm Rehabil Prev 2009;29:105-14. [DOI] [PubMed] [Google Scholar]
- 44.Furber S, Butler L, Phongsavan P, Mark A, Bauman A. Randomised controlled trial of a pedometer-based telephone intervention to increase physical activity among cardiac patients not attending cardiac rehabilitation. Patient Educ Couns 2010;80:212-8. [DOI] [PubMed] [Google Scholar]
- 45.Tudor-Locke C, Bell RC, Myers AM, Harris SB, Ecclestone NA, Lauzon N, et al. Controlled outcome evaluation of the first step program: a daily physical activity intervention for individuals with type II diabetes. Int J Obes Relat Metab Disord 2004;28:113-9. [DOI] [PubMed] [Google Scholar]
- 46.Plasqui G, Westerterp KR. Physical activity assessment with accelerometers: an evaluation against doubly labeled water. Obesity 2007;15:2371-9. [DOI] [PubMed] [Google Scholar]
- 47.Wiles CM, Busse ME, Sampson CM, Rogers MT, Fenton-May J, van Deursen R. Falls and stumbles in myotonic dystrophy. J Neurol Neurosurg Psychiatry 2006;77:393-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nijkrake MJ, Keus SH, Overeem S, Oostendorp RA, Vlieland TP, Mulleners W, et al. The ParkinsonNet concept: development, implementation and initial experience. Mov Disord 2010;25:823-29. [DOI] [PubMed] [Google Scholar]
- 49.Sturkenboom IH, Graff MJ, Borm GF, Veenhuizen Y, Bloem BR, Munneke M, et al. The impact of occupational therapy in Parkinson’s disease: a randomized controlled feasibility study. Clin Rehabil 2013;27:99-112. [DOI] [PubMed] [Google Scholar]