Attention-deficit hyperactivity disorder (ADHD) is characterized by inattention, hyperactivity, and impulsivity.[2] Globally, ADHD affects approximately 5–10% of children[3] and persists into adolescence in up to 85% of affected individuals.[4] Psychostimulants, such as methylphenidate and amfetamine, are the mainstay of treatment in ADHD.[2]
A patch that delivers methylphenidate transdermally (methylphenidate transdermal system; Daytrana®) has been developed for the treatment of ADHD. The patch comprises a backing layer, an adhesive formulation that incorporates methylphenidate and uses DOT Matrix™ technology, and a protective liner, which is removed prior to application.[5] The features and properties of methylphenidate transdermal system (including available patch sizes and the nominal methylphenidate dose delivered by each patch size) are shown in table I. Once applied to the skin, methylphenidate transdermal system releases methylphenidate continuously. A potential advantage of this patch technology is that it allows the duration of the effect to be tailored to the individual by varying the duration of the application (‘wear time’).[6]
Table I.
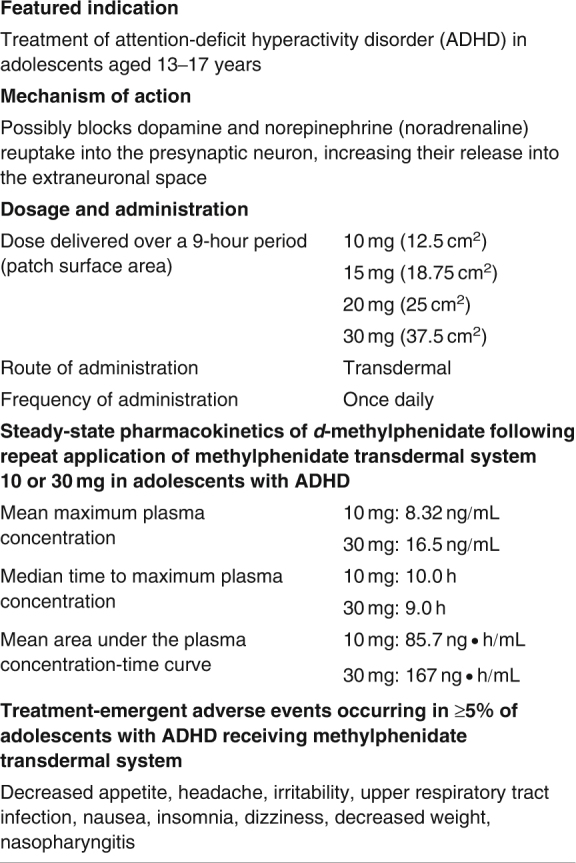
Features and properties of methylphenidate transdermal system (Daytrana®)[1]
Methylphenidate transdermal system is approved in the US for the treatment of ADHD,[5] and its use in children aged 6–12 years with ADHD has been reviewed previously.[7] This profile report examines the use of methylphenidate transdermal system in adolescents aged 13–17 years with ADHD.
Adolescents aged 13–17 years with ADHD were randomized to receive methylphenidate transdermal system or placebo transdermal system in a double-blind, multicenter, 7-week trial (core trial).[8] During a 5-week dose-optimization period, patients were titrated to their optimal methylphenidate transdermal system dosage (10, 15, 20, or 30 mg); the dose-optimization period was followed by a 2-week maintenance period, during which patients continued treatment at their optimal dosage. Patches were applied to the hip each morning and worn for 9 hours per day.[8] Following the core trial, eligible patients could receive longer-term therapy with methylphenidate transdermal system 10–30 mg in a noncomparative extension study of ≈6 months duration.[9]
According to the results of the core trial, methylphenidate transdermal system 10–30 mg was effective in adolescents aged 13–17 years with ADHD.[8] The mean ADHD-Rating Scale-IV (ADHD-RS-IV) total score (primary endpoint) decreased to a significantly (p < 0.001) greater extent in adolescents receiving methylphenidate transdermal system (n = 143) than in those receiving placebo transdermal system (n = 72), with a least squares mean between-group difference of -9.96 (95% CI -13.39, -6.53). The mean ADHD-RS-IV total score at study end was 17.7 in methylphenidate transdermal system recipients and 27.7 in placebo transdermal system recipients; the mean baseline scores were 36.4 and 36.6 in the corresponding treatment groups.[8]
In the extension study, methylphenidate transdermal system recipients experienced a significant (p < 0.001) reduction from the start of the core trial in the mean ADHD-RS-IV total score of 23.0.[9]
Methylphenidate transdermal system was generally well tolerated in adolescents with ADHD. The vast majority of treatment-emergent adverse events were of mild to moderate severity in both the short-term core trial[8] and the longer-term extension study.[9] In the core trial, the most frequently reported treatment-emergent adverse events (occurring in ≥5% of methylphenidate transdermal system recipients and in numerically more methylphenidate transdermal system than placebo transdermal system recipients) included decreased appetite, irritability, upper respiratory tract infection, nausea, insomnia, dizziness, and decreased weight.[8] A similar tolerability profile was seen during the extension study.[9]
In the core trial, most of the skin reactions to methylphenidate transdermal system comprised mild erythema, and adherence of the methylphenidate transdermal system patch to the skin was rated at ≥90% overall.[8] Changes in the blood pressure and pulse rate observed in the core[8] and extension[9] studies were typical of those seen in patients receiving stimulants.
Acknowledgements and Disclosures
The full text article[1] from which this profile report was derived was reviewed by A.C. Childress, Center for Psychiatry and Behavioral Medicine Inc., Las Vegas, NV, USA; J. Elia, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
The manufacturer of the agent under review was also offered an opportunity to comment on the original article[1] during the peer review process; changes resulting from comments received were made on the basis of scientific and editorial merit. The preparation of the original article and this profile report was not supported by any external funding.
Footnotes
Adapted and reproduced from the original article published in CNS Drugs 2011; 25 (4): 333–342.[1]
References
- 1.Keating G.M. Methylphenidate transdermal system in attention-deficit hyperactivity disorder in adolescents. CNS Drugs. 2011;25(4):333–42. doi: 10.2165/11206730-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- 3.Biederman J. Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry. 2005;57(11):1215–20. doi: 10.1016/j.biopsych.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 4.Biederman J., Faraone S., Milberger S., et al. Predictors of persistence and remission of ADHD into adolescence: results from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1996;35(3):343–51. doi: 10.1097/00004583-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Noven Pharmaceuticals, Inc. Daytrana© (methylphenidate transdermal system): US prescribing information [online]. Available from URL: http://www.daytrana.com/downloads/novenPI.pdf [Accessed 2010 Nov 29]
- 6.Wilens T.E., Boellner S.W., López F.A., et al. Varying the wear time of the methylphenidate transdermal system in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2008;47(6):700–8. doi: 10.1097/CHI.0b013e31816bffdf. [DOI] [PubMed] [Google Scholar]
- 7.Anderson V.R., Scott L.J. Methylphenidate transdermal system in attention-deficit hyperactivity disorder in children. Drugs. 2006;66(8):1117–26. doi: 10.2165/00003495-200666080-00007. [DOI] [PubMed] [Google Scholar]
- 8.Findling R.L., Turnbow J., Burnside J., et al. A randomized, double-blind, multicenter, parallel-group, placebo-controlled, dose-optimization study of the methylphenidate transdermal system for the treatment of ADHD in adolescents. CNS Spectr. 2010;15(7):419–30. doi: 10.1017/s1092852900000353. [DOI] [PubMed] [Google Scholar]
- 9.Findling R.L., Katic A., Rubin R., et al. A 6-month, open-label, extension study of the tolerability and effectiveness of the methylphenidate transdermal system in adolescents diagnosed with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2010;20(5):365–75. doi: 10.1089/cap.2009.0122. [DOI] [PubMed] [Google Scholar]


