Abstract
Background
In TKA, soft tissue balance (the joint gap) depends on the amount of resected bone and soft tissue release. Some studies report preoperative bony deformity correlates with soft tissue balance evaluated intraoperatively and that the medial tissues are contracted with varus deformity. However, these studies did not take into account the amount of resected bone and did not describe whether the soft tissue was tight or loose. Therefore, it remains unclear whether in varus deformity the soft tissues on the medial side are contracted.
Questions/purposes
We compared (1) intraoperative joint gap, (2) amount of resected bone, and (3) intraoperative soft tissue laxity on the lateral and medial sides according to severity of preoperative varus deformity.
Methods
We retrospectively reviewed 70 patients with osteoarthritis and varus deformities who underwent 90 TKAs. We retrospectively divided the 90 knees into three groups according to degree of preoperative alignment: mild varus group (< 10°), moderate varus group (10°–20°), and severe varus group (> 20°). To evaluate intraoperative soft tissue tension, we calculated the soft tissue gap by subtracting the thickness of the resected bone from the joint gaps on the medial and lateral sides, respectively. We then explored the relationship between the soft tissue gap and preoperative alignment.
Results
The lateral soft tissue gap was larger in the severe varus group than in the mild and moderate varus groups. The medial soft tissue gap was larger in the severe varus group than in the mild varus group, but there were no differences in the medial joint gaps among the groups.
Conclusions
After the bone is resected, the soft tissue on the lateral side is more lax; however, the soft tissue on the medial side is not shorter with greater preoperative varus deformity.
Introduction
Proper soft tissue balance is reportedly one of the most important factors for postoperative function and implant durability in TKA [10, 13, 17, 24, 26]. Intraoperative soft tissue balance depends on the amount of resected bone and soft tissue release. After the bone is cut, the joint gap is determined by the amount of resected bone and the laxity of the soft tissues [17, 27]. There is no established theory regarding how much bone resection and soft tissue release is required [2, 4, 22]. It is difficult to determine preoperatively the appropriate amount of bone resection and soft tissue release because it is difficult to measure soft tissue tension before surgery [16].
Further, it is unknown whether the tension of the soft tissue on the medial or lateral side will increase or decrease with the progression of preoperative deformity. Therefore, it would be useful for planning if we could know the relationship between intraoperative soft tissue balance and preoperative alignment. Some studies [1, 14, 27] have reported preoperative deformity correlates with soft tissue balance evaluated intraoperatively. Bellemans et al. [1] evaluated the intraoperative alignment of the knee by applying maximal manual varus-valgus stress in extension after removing the osteophytes (but before cutting the bone) while using a computer navigation system. They reported intrinsic shortening of the medial soft tissue and stretching of lateral structures exists when a preoperative varus deformity exceeds 10°. Matsumoto et al. [14] evaluated intraoperative soft tissue balance by using the joint gap after implanting the femoral trial prosthesis and found the intraoperative varus angle was considerably larger if preoperative varus alignment was greater than 20°, compared with those with less preoperative varus alignment. However, these studies did not describe whether the soft tissue was tight or loose because they did not take into account the amount of resected bone.
We therefore compared (1) intraoperative joint gap, (2) amount of resected bone, and (3) intraoperative soft tissue laxity on the lateral and medial sides according to severity of preoperative varus deformity.
Patients and Methods
We retrospectively reviewed 70 patients who underwent 90 TKAs for osteoarthritis with varus deformities. The patient population was comprised of eight men and 82 women with a mean age of 75 years (range, 51–89 years). The average preoperative hip-knee-ankle (HKA) angle, measured on long standing weightbearing AP radiographs, was 14° (range, 3°–30°) in varus. The mean preoperative ROM was 114° (range, 60°–150°), and 13 knees had flexion contracture that was greater than 15°. Three knees had bone defects of the medial tibial plateau that were greater than 11 mm deep (Table 1). This study was approved by the institutional review board of our hospital. To participate in this study, informed consent was obtained from all patients.
Table 1.
Demographic characteristics of enrolled patients
| Variable | Mild varus group (< 10°) | Moderate varus group (10°–20°) | Severe varus group (> 20°) |
|---|---|---|---|
| Number of knees | 17 | 61 | 12 |
| Age (years)* | 74 ± 2 | 75 ± 1 | 76 ± 2 |
| Sex (% male)† | 12 | 7 | 17 |
| Diagnosis (% osteoarthritis) | 100 | 100 | 100 |
| Preoperative ROM (°)* | 114 ± 19 | 116 ± 25 | 103 ± 25 |
| Number of flexion contractures ≥ 15° | 2 | 9 | 2 |
| Bone defects of the medial tibial plateau (mm)*, ‡ | 4.2 ± 3.9 | 6.1 ± 2.9 | 9.0 ± 3.0 |
| Number of bone defects of the medial tibial plateau ≥ 11 mm | 1 | 1 | 1 |
| Postoperative hip-knee-ankle angle (°)* | 0 ± 4 | 1 ± 3 | 1 ± 3 |
* Values are expressed as mean ± SD; †because there were few men, it was not possible to analyze differences between men and women; ‡bone defects of the medial tibial plateau were larger (p = 0.004) in the severe varus group than in the mild varus group.
We retrospectively divided the 90 knees into three groups according to degree of preoperative alignment. This resulted in 17 knees with less than 10° preoperative varus alignment (mild varus group), 61 knees with greater than 10° and less than 20° preoperative varus alignment (moderate varus group), and 12 knees with greater than 20° preoperative varus alignment (severe varus group). The varus alignment was defined as the mechanical axis angle between the femur and the tibia on a preoperative radiograph of a standing, weightbearing patient from the AP view. There were no differences among groups in age, sex, preoperative ROM, number of flexion contractures, or postoperative HKA angle (Table 1).
One experienced surgeon (SM) performed all surgeries using the same prosthesis (NexGen® Complete Knee Solution Legacy® Posterior Stabilized Knee, Zimmer, Inc, Warsaw, IN, USA). All knees were exposed using a standard medial parapatellar approach or midvastus approach. We used a measured resection technique for bone cutting. For the femur, the coronal alignment was set perpendicular to its mechanical axis, according to preoperative long-leg radiographs. In the sagittal plane, the femoral component was aligned to its distal anatomic axis and rotationally aligned to the surgical epicondylar axis. The depth of the distal cut for the femur was set to 9 mm from the most distal lateral articular surface. For the tibia, the coronal alignment was set perpendicular to its mechanical axis, the posterior slope was adjusted to that of the lateral tibial plateau, and the rotational alignment was adjusted to the AP axis, connecting the medial 1/3 of the patellar tendon attachment and the center of the cut surface. The depth of the proximal cut for the tibia was set to 11 mm from the lateral articular surface. The deep medial collateral ligament was carefully liberated from the underlying osteophytes on the medial tibia. All medial and lateral osteophytes of the femoral condyle and tibia were removed. The ACL and PCL were resected and the posterior capsule along the femur was released. Between the proximal tibia and the distal femur, we fitted the offset-type tensor device (ORF-tensor®; Zimmer) on the cut surface to measure the extension gap. Joint distraction force was applied at 176.4 N (40 pounds) [13, 14, 18]. The tension device consisted of three parts: an upper seesaw plate, a lower platform plate, and an extraarticular main body (Fig. 1). The center joint gap and the varus angle between the seesaw plate and the platform plate were measured [13–15]. The measurements with the tensor were obtained three times by one surgeon (SM), and the average was used for data. The average error between repeated measurements for the joint gap and angle were 0.50 mm ± 0.31 mm and 0.38° ± 0.35°. The intraclass correlation coefficients (ICC) for measurements of the joint gap and angle were 0.98 and 0.90 respectively.
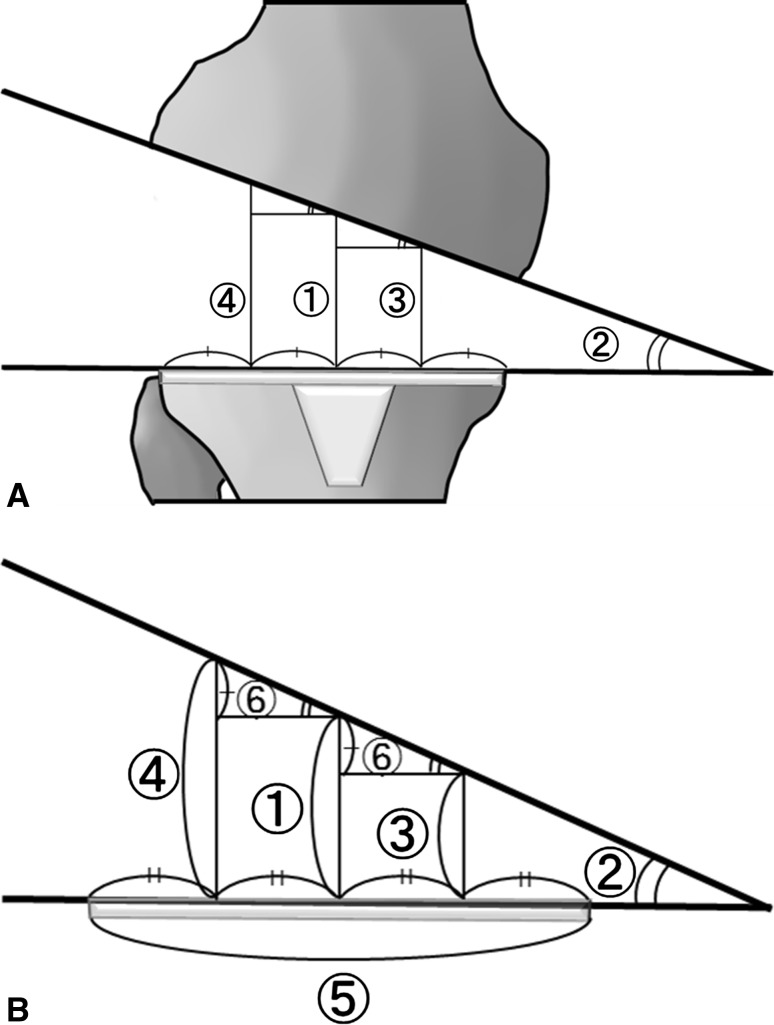
Fig. 1.
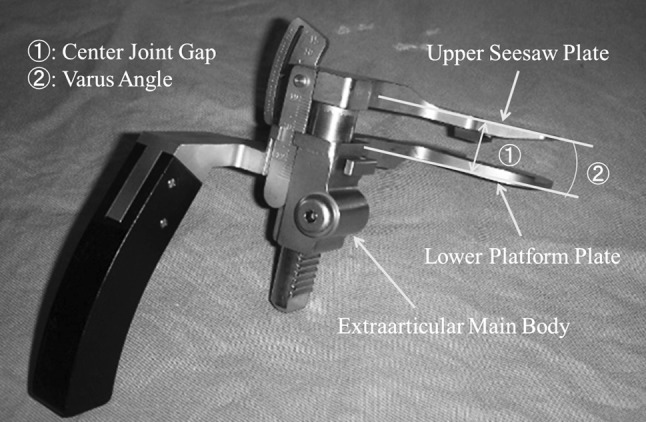
The tension device consists of three parts: an upper seesaw plate, a lower platform plate, and an extraarticular main body. Two measurements were made: (1) the center joint gap and (2) the angle between the seesaw plate and the platform plate.
Using these measurements and the transverse diameter of the tibial component, we could measure the medial and lateral extension joint gaps. The medial joint gap was calculated (center joint gap − 0.25 × diameter of tibial component × tangent of the varus angle), and the lateral joint gap was calculated (center joint gap + 0.25 × diameter of tibial component × tangent of the varus angle) (Fig. 2). To evaluate intraoperative soft tissue tension, we defined a soft tissue gap as the distance calculated by subtracting the thickness of the resected bone with cartilage of the distal femur and proximal tibia from the extension gap on the medial and lateral sides, respectively (Fig. 3). The thickness of the resected bone was measured at the center of the medial and lateral compartments by a caliper. The thickness of the saw blade (1.3 mm) was added to the measured bone thickness to obtain the actual thickness of resected bone.
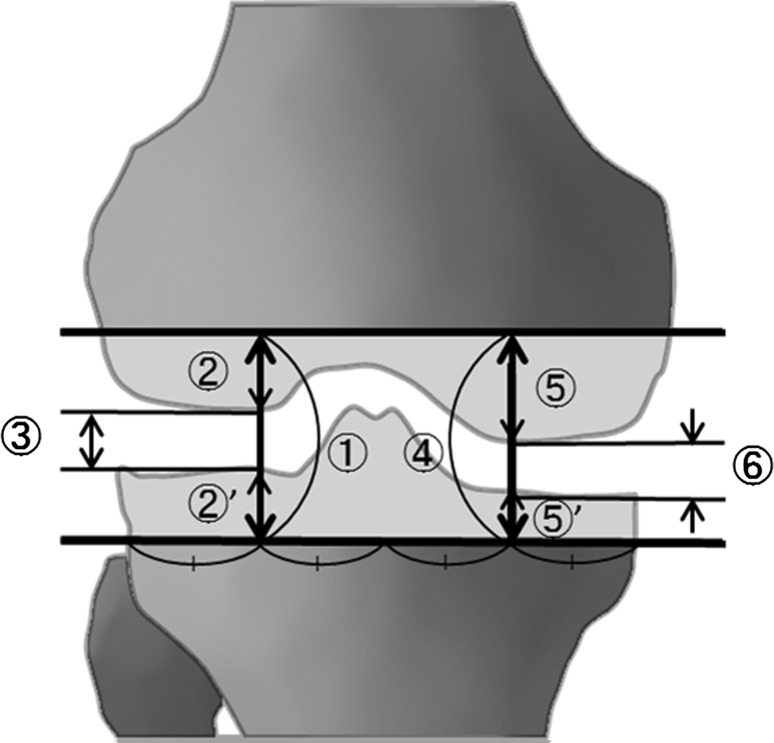
Fig. 2A–B.
(A) A diagram illustrates the: (1) center joint gap, (2) varus angle, (3) medial joint gap, and (4) lateral joint gap. (B) A diagram illustrates the following parameters: (1) center joint gap, (2) varus angle, (3) medial joint gap, (4) lateral joint gap, and (5) transverse diameter of the tibial component. Using these measurements, we calculated the medial and lateral joint gaps as follows: (6) = 0.25 × (5) × tan (2), (3) = (1) − (6), and (4) = (1) + (6).
Fig. 3.
The (1) lateral joint gap, (2) + (2)′ thickness of the lateral resected bone, (3) lateral soft tissue gap, (4) medial joint gap, (5) + (5)′ thickness of the medial resected bone, and (6) medial soft tissue gap are shown.
We determined differences in the joint gap, the thickness of the resected bone, and the soft tissue gap between the groups using ANOVA with a Tukey-Kramer post hoc test. JMP® statistical software (Version 8; SAS Institute, Inc, Cary, NC, USA) was used to analyze the data.
Results
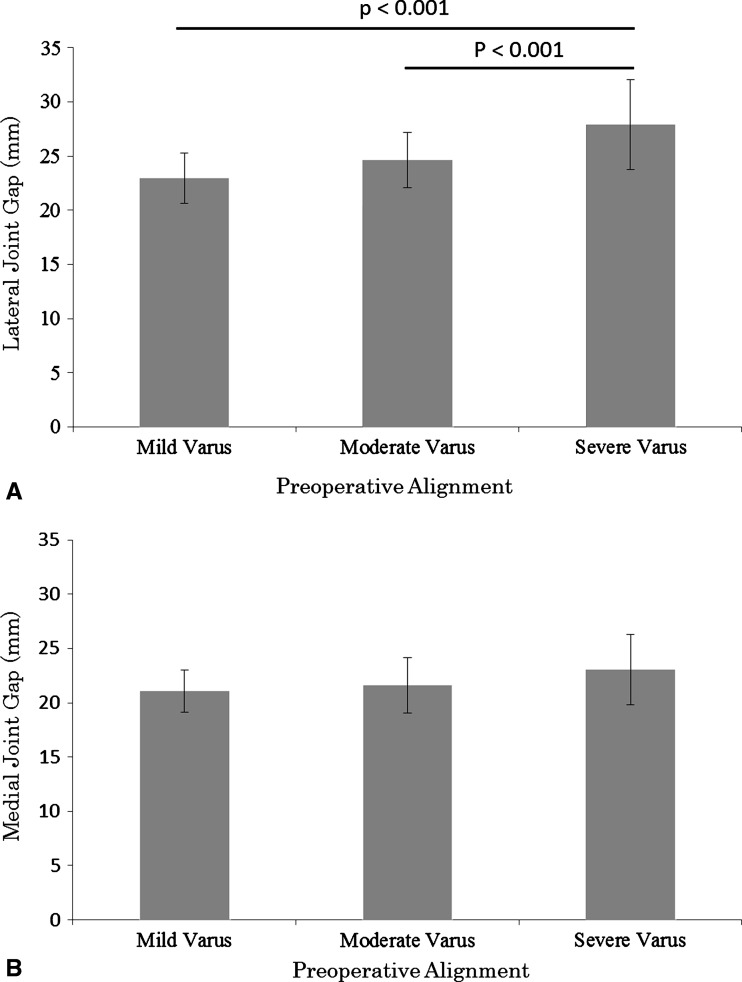
The lateral joint gap was larger (p < 0.001) in the severe varus group than in the mild and moderate varus groups (Fig. 4A). There were no differences in the medial joint gaps among the groups (Fig. 4B).
Fig. 4A–B.
The graphs compare the joint gaps among preoperative alignments. Data are shown as mean ± SD. (A) The lateral joint gap was larger in the severe varus group than in the mild and moderate varus groups. (B) There were no differences in the medial joint gaps among groups.
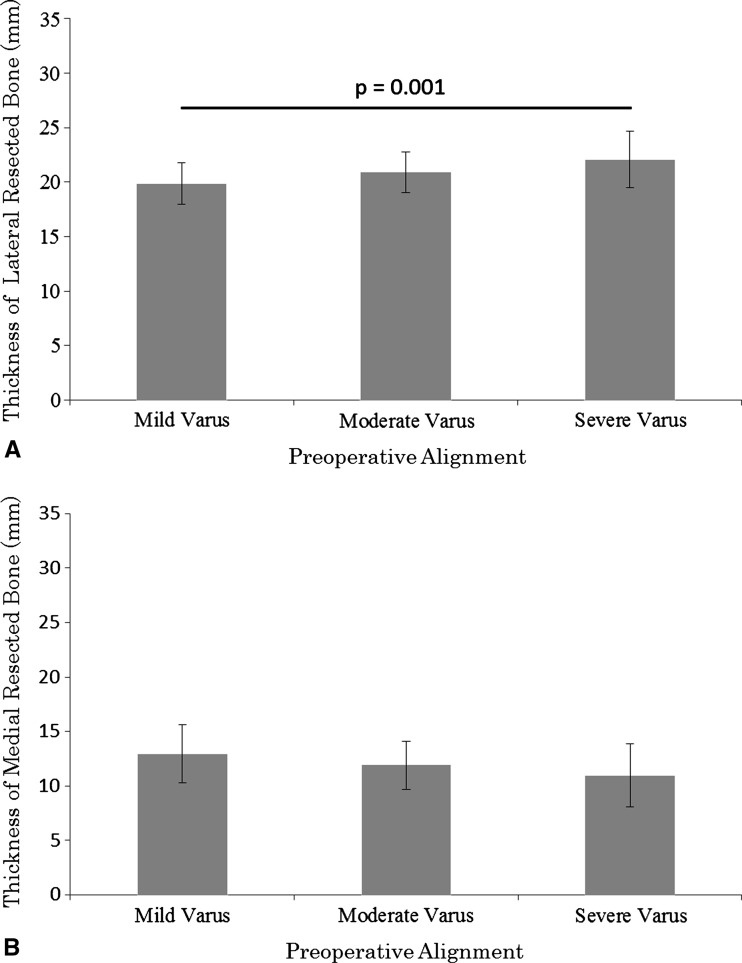
The thickness of the lateral resected bone was larger (p = 0.01) in the severe varus group than in the mild varus group (Fig. 5A). There were no differences in the thickness of the medial resected bone among groups (Fig. 5B).
Fig. 5A–B.
The graphs compare the thicknesses of the resected bone with preoperative alignments. The data are shown as mean ± SD. (A) The thickness of the lateral resected bone was larger in the severe varus group than in the mild varus group. (B) There were no differences in the thickness of the medial resected bone among groups.
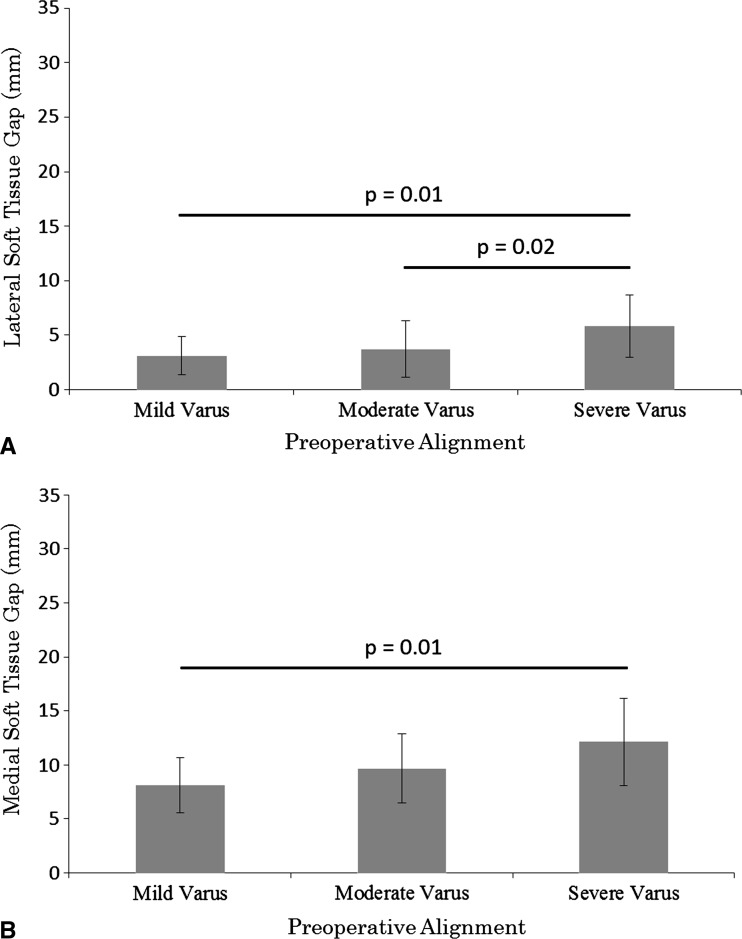
The lateral soft tissue gap was larger (p = 0.01 and 0.02, respectively) in the severe varus group than in the mild and moderate varus groups (Fig. 6A). The medial soft tissue gap was larger (p = 0.01) in the severe varus group than in the mild varus group (Fig. 6B). A comparison of the data is shown (Table 2).
Fig. 6A–B.
Comparison of the soft tissue gaps among preoperative alignments are shown in these graphs. The data are shown as mean ± SD. (A) The lateral soft tissue gap was larger in the severe varus group than in the mild and moderate varus groups. (B) The medial soft tissue gap was larger in the severe varus group than in the mild varus group.
Table 2.
Comparison of results among alignment groups
| Variable | Side | Mild varus group (< 10°) | Moderate varus group (10°–20°) | Severe varus group (> 20°) | p value | ||
|---|---|---|---|---|---|---|---|
| Mild versus moderate varus group | Mild versus severe varus group | Moderate versus severe varus group | |||||
| Joint gap (mm) | Lateral | 23.0 ± 2.3 | 24.6 ± 2.5 | 27.9 ± 4.1 | 0.08 | < 0.001 | < 0.001 |
| Medial | 21.0 ± 2.0 | 21.6 ± 2.5 | 23.1 ± 3.2 | 0.72 | 0.10 | 0.16 | |
| Thickness of the resected bone (mm) | Lateral | 19.9 ± 1.9 | 20.9 ± 1.8 | 22.1 ± 2.6 | 0.13 | 0.01 | 0.15 |
| Medial | 12.9 ± 2.7 | 11.9 ± 2.2 | 10.9 ± 2.9 | 0.27 | 0.08 | 0.41 | |
| Soft tissue gap (mm) | Lateral | 3.1 ± 1.7 | 3.7 ± 2.6 | 5.9 ± 2.8 | 0.63 | 0.01 | 0.02 |
| Medial | 8.1 ± 2.6 | 9.7 ± 3.2 | 12.1 ± 4.0 | 0.19 | 0.01 | 0.14 | |
Values are expressed as mean ± SD.
Discussion
In TKA, soft tissue balancing (the joint gap) depends on the amount of resected bone and soft tissue release. Previous studies have suggested a relationship between preoperative deformity and soft tissue balance evaluated intraoperatively [1, 14]. However, these studies did not take into account the amount of resected bone. Therefore, we addressed the following question: Is there any difference in soft tissue laxity (taking into account the amount of resected bone) on the lateral or medial side depending on the severity of preoperative varus deformity? To answer this question, we compared the following variables among mild, moderate, and severe varus groups: (1) intraoperative extension joint gaps, (2) amount of resected bone on the lateral and medial sides, and (3) intraoperative soft tissue laxity.
We note several limitations. First, multiple factors might have influenced the assessment of the soft tissue balance; factors such as the weight of the thigh, contracture of the quadriceps, or patella baja might have influenced the intraoperative joint gap. However, with the patient under anesthesia, these factors would likely not affect the extension gap. Further, we attempted to evaluate a small number of variables, preoperative varus alignment and intraoperative joint gaps, since it would be helpful for surgeons to predict the intraoperative joint gap simply from the preoperative varus alignment. Second, our study was limited to the medial compartment of osteoarthritic knees and did not include knees with rheumatoid arthritis or the lateral compartment of osteoarthritic knees. Therefore, we cannot generalize our results regarding valgus knees or other diseases. We studied the most common disease for TKA, osteoarthritis with varus deformity. Third, because the amount of resected bone was greater in patients with large medial bone defects, soft tissue releases might have been greater for these patients. However, one experienced surgeon performed the operations and intraoperative measurements and did not release the superficial medial collateral ligament in any patient before measurement. In addition, we encountered only one knee in each group that had a medial bone defect of the medial tibial plateau greater than 11 mm. Therefore, the influence would be small. Fourth, we did not compare nonarthritic knees with osteoarthritic knees. However, it is difficult to obtain normal control of intraoperative gaps, and our data are useful to know the relationship between mild and severe varus deformities.
We found the lateral joint gap was larger in the severe varus group than in the mild and moderate varus groups. By contrast, there were no differences in the medial joint gaps among the groups. These results are similar to those of Matsumoto et al. [13], which showed the lateral joint gap after bone resection was larger in the severe varus group than in the mild and moderate varus groups although they measured the gap after fitting the femoral trial prosthesis (Table 3). However, because they did not take into account the amount of resected bone, the study could not determine whether the cause of the larger joint gap was the increased amount of resected bone or loosening of the soft tissue.
Table 3.
Comparison of our study with other literature
| Study | Variable | Side | Mild varus group (< 10°) | Moderate varus group (10°–20°) | Severe varus group (> 20°) |
|---|---|---|---|---|---|
| Matsumoto et al. [13] | Compartment gap (mm) | Lateral | 11.9 ± 0.8 | 11.7 ± 0.5 | 12.8 ± 0.7 |
| Medial | 10.9 ± 0.6 | 10.3 ± 0.5 | 10.1 ± 0.5 | ||
| Current study | Joint gap (mm) | Lateral | 23.0 ± 2.3 | 24.6 ± 2.5 | 27.9 ± 4.1 |
| Medial | 21.0 ± 2.0 | 21.6 ± 2.5 | 23.1 ± 3.2 | ||
| Current study | Soft tissue gap (mm) | Lateral | 3.1 ± 1.7 | 3.7 ± 2.6 | 5.9 ± 2.8 |
| Medial | 8.1 ± 2.6 | 9.7 ± 3.2 | 12.1 ± 4.0 |
Values are expressed as mean ± SD.
Our observations showed the thickness of the lateral resected bone was larger in knees with greater varus. However, the thickness of the medial resected bone had a tendency to be smaller in knees with more varus. Hunter et al. [8] reported the distal femoral condylar angle and tibial plateau angle vary and increase with greater varus. As the tibial plateau angle increases in knees with severe varus, the surgeon might allow 1 or 2 mm more lateral bone resection to avoid use of bone graft or augmentation block.
The lateral soft tissue gap was larger in the severe varus group, compared with the mild and moderate varus groups, and the medial soft tissue gap was larger in the severe varus group, compared with the mild varus group. This suggests the lateral soft tissue structure is looser with greater preoperative varus deformity, and the contracture of the medial soft tissue structure does not exist even in knees with severe varus. As mentioned above, it is unclear from the study by Matsumoto et al. [14] whether the laxity of the soft tissue increases in knees with severe varus. As we showed, however, expansion of the joint gap on the lateral side in knees with severe varus was caused not only by the increased amount of resected bone but also by loosening of the soft tissue. We believe the reason for loosening of the lateral soft tissue in knees with severe varus is that the lateral thrust movement of the knee during daily weightbearing activities may stretch the lateral soft tissue [11, 28]. In knees with severe varus, this lateral laxity would cause a ligament imbalance after resection of bone in TKA. Our findings for the medial side differed from those of Bellemans et al. [1]. The differences between their study and ours are (1) their measurements were made before the bone was cut, (2) they retained the ACL and PCL; (3) they applied stress manually, and (4) their study did not involve knees with greater than 20° varus. After the bone is cut, removal of the osteophytes might be more complete, especially in the posterior area, loosening the whole articular capsule. Resection of the cruciate ligaments might influence the medial soft tissue tension. As a result, the medial soft tissue is released from pressure of the osteophytes and bone and returns to its original length. Fishkin et al. [7] reported greater stiffness of the ligaments on the lateral and medial sides in osteoarthritic knees with a mean 9° varus deformity than in nonosteoarthritic knees. However, they did not present the relationship between mild and severe varus deformities. We compared osteoarthritic knees with severe, moderate, and mild varus but did not compare nonarthritic with osteoarthritic knees. Additionally, in our study, the deep medial collateral ligament and posteromedial capsule were carefully liberated from the underlying osteophytes on the medial tibia. By contrast, Fishkin et al. [7] did not describe this. We believe osteoarthritic changes might increase stiffness of the capsular ligament along with osteophyte formation; however, contracture of the superficial medial collateral ligament does not exist after releasing the capsular ligaments with complete removal of the osteophytes.
In varus knees, many surgeons assume soft tissues on the medial side contract because such results have been reported in other studies. However, these measurements were performed before surgery or bone resection [1, 3, 9, 16, 20]. Therefore, surgeons try to correct intraoperative imbalance by releasing the medial soft tissues. Because the medial soft tissue does not contract after bone resection and removal of osteophytes, however, an extensive medial release is not necessary to obtain enough extension gap for placement of prosthesis even in severe varus knees. However, as the lateral soft tissue is loose in severe varus knees, ligament imbalance would remain in those knees. There is no consensus regarding how to handle this ligament imbalance caused by loose lateral soft tissue. The extensive medial release to adjust to the morbidly loose lateral soft tissue would result in the use of a thicker insert that may cause elevation of the joint line [25, 27], and the looser soft tissue may create postoperative instability [12, 20]. Some surgeon may consider allowing slight varus postoperative alignment in the safe zone, as described by Fang et al. [5] (2.4°–7.2° valgus in tibiofemoral angle). However, we consider the residual postoperative varus alignment would be a risk to worsen the ligament imbalance. Sekiya et al. [23] suggested that postoperative lateral ligamentous laxity diminished with time, reporting that 8.6° of lateral laxity at extension diminished to 5.1° 3 months after TKA. We think it is unnecessary to release ligaments too much on the medial side to be the same length with the loose lateral side and accept a slight intraoperative lateral laxity as long as a neutral coronal alignment can be achieved after implantation [6, 19, 21]. When taking into account the resected bone, we found the lateral soft tissue was more lax but the medial soft tissue was not shorter with greater varus deformity.
Acknowledgments
We thank Shinya Kawahara MD and Hiroyuki Nakahara MD who crosschecked the data.
Footnotes
The institution of one or more of the authors (KO) received funding, during the study period, from the Japanese Society for the Promotion of Science Grants-in Aid Scientific Research Program (Grant Number 23000011). The study was funded by internal sources from the Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution has approved the human protocol for this investigation, all investigations were conducted in conformity with ethical principles of research, and informed consent for participation in the study was obtained.
This work was performed at Kyushu University, Fukuoka, Japan.
References
- 1.Bellemans J, Vandenneucker H, Vanlauwe J, Victor J. The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc. 2010;18:152–156. doi: 10.1007/s00167-009-0903-0. [DOI] [PubMed] [Google Scholar]
- 2.Berend ME, Small SR, Ritter MA, Buckley CA. The effects of bone resection depth and malalignment on strain in the proximal tibia after total knee arthroplasty. J Arthroplasty. 2010;25:314–318. doi: 10.1016/j.arth.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Brage ME, Draganich LF, Pottenger LA, Curran JJ. Knee laxity in symptomatic osteoarthritis. Clin Orthop Relat Res. 1994;304:184–189. [PubMed] [Google Scholar]
- 4.Brooks P. Seven cuts to the perfect total knee. Orthopedics. 2009;32. pii: orthosupersite.com/view.asp?rID = 42848. DOI: 10.3928/01477447-20090728-27. [DOI] [PubMed]
- 5.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 6.Fehring TK, Valadie AL. Knee instability after total knee arthroplasty. Clin Orthop Relat Res. 1994;299:157–162. [PubMed] [Google Scholar]
- 7.Fishkin Z, Miller D, Ritter C, Ziv I. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res. 2002;20:204–207. doi: 10.1016/S0736-0266(01)00087-0. [DOI] [PubMed] [Google Scholar]
- 8.Hunter DJ, Niu J, Felson DT, Harvey WF, Gross KD, McCree P, Aliabadi P, Sack B, Zhang Y. Knee alignment does not predict incident osteoarthritis: the Framingham osteoarthritis study. Arthritis Rheum. 2007;56:1212–1218. doi: 10.1002/art.22508. [DOI] [PubMed] [Google Scholar]
- 9.Ishii Y, Noguchi H, Matsuda Y, Kiga H, Takeda M, Toyabe S. Preoperative laxity in osteoarthritis patients undergoing total knee arthroplasty. Int Orthop. 2009;33:105–109. doi: 10.1007/s00264-007-0467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y. Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res. 2001;391:210–217. doi: 10.1097/00003086-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Kuroyanagi Y, Nagura T, Kiriyama Y, Matsumoto H, Otani T, Toyama Y, Suda Y. A quantitative assessment of varus thrust in patients with medial knee osteoarthritis. Knee. 2012;19:130–134. doi: 10.1016/j.knee.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Martin JW, Whiteside LA. The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res. 1990;259:146–156. [PubMed] [Google Scholar]
- 13.Matsumoto T, Mizuno K, Muratsu H, Tsumura N, Fukase N, Kubo S, Yoshiya S, Kurosaka M, Kuroda R. Influence of intra-operative joint gap on post-operative flexion angle in osteoarthritis patients undergoing posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:1013–1018. doi: 10.1007/s00167-007-0331-y. [DOI] [PubMed] [Google Scholar]
- 14.Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R. The influence of preoperative deformity on intraoperative soft tissue balance in posterior-stabilized total knee arthroplasty. J Arthroplasty. 2011;26:1291–1298. doi: 10.1016/j.arth.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M. Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng. 2006;128:867–871. doi: 10.1115/1.2354201. [DOI] [PubMed] [Google Scholar]
- 16.Matziolis G, Matziolis D, Perka C. Pre-operative frontal plane malalignment predicts the extension gap asymmetry in knee osteoarthritis. Int Orthop. 2012;36:79–82. doi: 10.1007/s00264-011-1294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA. Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg. 2009;17:766–774. doi: 10.5435/00124635-200912000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Mitsuyasu H, Matsuda S, Fukagawa S, Okazaki K, Tashiro Y, Kawahara S, Nakahara H, Iwamoto Y. Enlarged post-operative posterior condyle tightens extension gap in total knee arthroplasty. J Bone Joint Surg Br. 2011;93:1210–1216. doi: 10.1302/0301-620X.93B9.25822. [DOI] [PubMed] [Google Scholar]
- 19.Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y. Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci. 2006;11:264–266. doi: 10.1007/s00776-006-1009-x. [DOI] [PubMed] [Google Scholar]
- 20.Parratte S, Pagnano MW. Instability after total knee arthroplasty. J Bone Joint Surg Am. 2008;90:184–194. [PubMed] [Google Scholar]
- 21.Sasanuma H, Sekiya H, Takatoku K, Takada H, Sugimoto N. Evaluation of soft-tissue balance during total knee arthroplasty. J Orthop Surg (Hong Kong). 2010;18:26–30. doi: 10.1177/230949901001800106. [DOI] [PubMed] [Google Scholar]
- 22.Schnurr C, Csecsei G, Nessler J, Eysel P, Konig DP. How much tibial resection is required in total knee arthroplasty? Int Orthop. 2011;35:989–994. doi: 10.1007/s00264-010-1025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sekiya H, Takatoku K, Takada H, Sasanuma H, Sugimoto N. Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin Orthop Relat Res. 2009;467:1582–1586. doi: 10.1007/s11999-008-0588-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takayama K, Matsumoto T, Kubo S, Muratsu H, Ishida K, Matsushita T, Kurosaka M, Kuroda R. Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:532–537. doi: 10.1007/s00167-011-1594-x. [DOI] [PubMed] [Google Scholar]
- 25.Teeny SM, Krackow KA, Hungerford DS, Jones M. Primary total knee arthroplasty in patients with severe varus deformity: a comparative study. Clin Orthop Relat Res. 1991;273:19–31. [PubMed] [Google Scholar]
- 26.Whiteside LA, Saeki K, Mihalko WM. Functional medial ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:45–57. doi: 10.1097/00003086-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Yagishita K, Muneta T, Yamamoto H, Shinomiya K. The relationship between postoperative ligament balance and preoperative varus deformity in total knee arthroplasty. Bull Hosp Jt Dis. 2001;60:23–28. [PubMed] [Google Scholar]
- 28.Yoshimura I, Naito M, Hara M, Zhang J. Analysis of the significance of the measurement of acceleration with respect to lateral laxity of the anterior cruciate ligament insufficient knee. Int Orthop. 2000;24:276–278. doi: 10.1007/s002640000171. [DOI] [PMC free article] [PubMed] [Google Scholar]