History and Physical Examination
A 55-year-old woman presented with a painless, palpable, slow-growing mass in the right knee of 10 years’ duration. She denied any recent traumatic event or preceding infection. Her medical history was unremarkable. On physical examination, a soft, freely movable, nontender, palpable mass without surrounding warmth was located in the anterolateral aspect of the knee. She had no limitation to her ROM. The remainder of the musculoskeletal examination was normal. Laboratory analyses were within normal limits.
After initial AP and lateral radiographic evaluation (Fig. 1), the patient underwent MRI of the right knee (Figs. 2, 3).
Fig. 1A–B.

(A) AP and (B) lateral radiographs of the right knee show a radiolucent soft tissue lesion with fat attenuation in the anterolateral aspect of the knee.
Fig. 2A–D.
(A) Axial T1-weighted, (B) coronal T-1 weighted, and (C) axial T2-weighted MR images show the large soft tissue mass in the suprapatellar pouch having the same signal intensity as the subcutaneous fat and a thin fibrous internal septum with low signal intensity on T1- and T2-weighted images. (D) On an axial proton density fat saturation MR image, the lesion appears hypointense and has the same signal intensity as the subcutaneous fat. Minimal joint effusion outlining the capsule was observed.
Fig. 3.
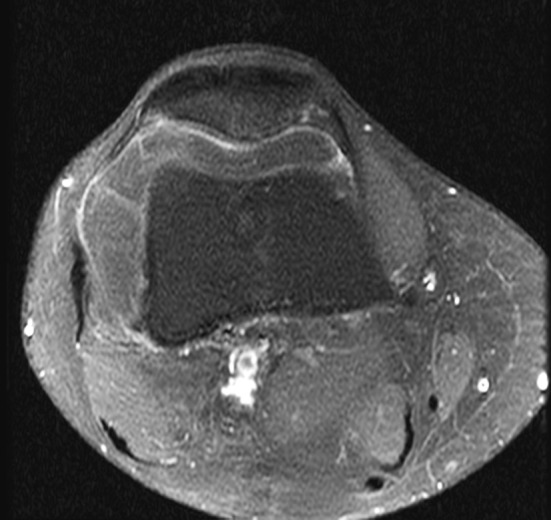
An axial T1-weighted MR image shows mild peripheral enhancement of the soft tissue mass after intravenous administration of gadolinium contrast.
Based on the history, physical examination, laboratory studies, and imaging studies, what is the differential diagnosis at this point?
Imaging Interpretation
AP (Fig. 1A) and lateral (Fig. 1B) radiographs of the right knee showed a radiolucent soft tissue mass in the anterolateral aspect of the knee. There was no visible bone destruction or other lesion identified. MRI revealed one large soft tissue mass in the suprapatellar pouch that had the same signal intensity as the subcutaneous fat and an internal septum with low signal intensity on T1- and T2-weighted sequences within it (Fig. 2A–C). Minimal joint effusion outlining the joint capsule also was seen on an axial proton density fat saturation image (Fig. 2D). The soft tissue lesion also showed mild peripheral enhancement pattern on postgadolinium T1-weighted MRI (Fig. 3).
Differential Diagnosis
Intraarticular lipoma
Lipoma arborescens
Intraarticular liposarcoma
Pigmented villonodular synovitis
Hoffa’s disease
The patient underwent arthrotomy by means of a medial parapatellar incision. The specimen was excised completely, and a fibrous stalk was ligated. The entire specimen was submitted for routine pathohistologic examination (Fig. 4).
Fig. 4A–B.

The histologic specimen examined in (A) a low-power field (Stain, hematoxylin and eosin; original magnification, ×40) and (B) a high-power field (Stain, hematoxylin and eosin; original magnification, ×200) had mature fat cells with no atypical nuclei and thin fibrous septa between lobules of adipocytes. No atypical cells or thick septa were found.
Based on the history, physical examination, laboratory studies, imaging studies, and histologic picture, what is the diagnosis and how should the patient be treated?
Histology Interpretation
Arthrotomy revealed an encapsulated, soft, yellowish, movable, and decalcified mass. After dissection, a fibrous vascular stalk attachment of the medial wall of the knee was ligated, and a 6- × 10-cm mass lesion then was excised. For pathohistologic examination, the specimen was cut and stained with hematoxylin and eosin. Histologic sections showed abundant mature adipocytes with thin fibrous septa, suggestive of typical characteristics of an intraarticular lipoma (Fig. 4). No atypical cells or thick septae were found.
Diagnosis
Intraarticular lipoma
Discussion and Treatment
Clinical and radiologic features showed the painless, palpable, slow-growing mass in the patient’s right knee for 10 years and the large soft tissue mass in the suprapatellar pouch had the same signal intensity as the subcutaneous fat on T1- and T2-weighted sequences. The lesion also showed a mild peripheral enhancement pattern with a thin internal septum. These features characterize an intraarticular, well-defined, and pure lipomatous lesion of the knee, highly suggestive of an intraarticular lipoma. We considered the primary differential considerations to be lipoma arborescens, well-differentiated liposarcoma, pigmented villonodular synovitis, and Hoffa’s disease. Macroscopically, lipoma arborescens has a frondlike appearance with numerous villous synovial proliferations of fatty yellow tissue. Villous lipomatous proliferation of the synovial membrane is characteristic of lipoma arborescens [16, 25]. In addition, lipoma arborescens usually is associated with some clinical conditions, such as trauma, osteoarthritis, or other chronic inflammatory conditions [16, 25], whereas a true intraarticular lipoma usually occurs de novo without a prior event. The characteristic finding of lipoma arborescens observed on MR images is villous-like projections in the synovial lining with high signal intensity on T1- and T2-weighted images, which will saturate on fat-suppressed sequences [25], whereas intraarticular lipomas usually present as a diffuse or nodular lipomatous lesion in the knee.
A well-differentiated liposarcoma is a low-grade sarcoma affecting predominantly middle-aged patients. It often present as a painless, slow-growing mass which may by locally aggressive but it rarely metastasizes [1, 8]. The primary intraarticular liposarcoma is rare [14]. The characteristic features of a well-differentiated liposarcoma on MR images are large lesion size, presence of thick septa, and presence of nonlipomatous soft tissue components with decreased percentage of fat composition [1, 8]. However, contrary to a well-differentiated liposarcoma, an intraarticular lipoma manifests as a purely lipomatous lesion.
Pigmented villonodular synovitis (PVNS) is a rare intraarticular lesion characterized by a proliferative disorder of the synovial lining that may affect the joints or tendon sheaths. MRI reveals a lesion with low signal intensity on T1- and T2-weighted images with “blooming” artifact attributable to the hemosiderin deposition. The lesions also show a well-enhanced pattern on postgadolinium T1-weighted MRI, whereas intraarticular lipomas usually present as a diffuse or nodular lipomatous lesion with a mild peripheral enhancement pattern [4, 5].
Hoffa’s disease is a syndrome of infrapatellar fat pad impingement, first described by Hoffa in 1904 [11]. The infrapatellar fat pad is hypertrophied owing to previous trauma [12]. MRI shows a mass or nodule with low signal intensity on T1- and T2-weighted images attributable to fibrosis in the subacute or chronic stage. MRI also may show high signal intensity on T2-weighted images because of tissue swelling or hemorrhage. Hoffa’s disease occasionally may be associated with ossification [10, 12]. However, in contrast, an intraarticular lipoma usually manifests as a nodular or diffuse lipomatous tumor in the suprapatellar pouch, and rarely is located in the infrapatellar fat or intercondylar notch region.
A lipoma is a benign tumor composed of adipose tissue and most commonly occurs in the subcutaneous region [2]. However, an intraarticular lipoma is rare. All of the differential diagnoses can have similar clinical presentations, which adds to the difficulty of making an accurate diagnosis. The English-language literature has 16 case reports of intraarticular lipomas [3, 7, 9, 10, 13, 15, 17, 19–22, 24, 26–29]. An intraarticular lipoma usually occurs in middle-aged patients, but some cases have been reported in adolescents [19, 29]. Subcutaneous lipomas are reportedly more common in women than in men [23]. No clear sex predilection for intraarticular lipomas has been described. In the 17 cases of intraarticular lipomas in the knee, 16 published cases plus our patient, there is female-to-male ratio of 10:7.
The knee is the most common location for an intraarticular lipoma, and the hip and facet joint of the spine also have been reported as locations [6, 18]. Intraarticular lipomas usually present with a painless enlarged knee mass, locked knee, joint swelling, or a painful knee caused by strangulation of the intraarticular lipoma [10, 27, 28]. A true intraarticular lipoma typically is a solitary yellowish, variable-sized, solitary polyp-like mass, round to oval, with a short stalk connecting the joint capsule grossly. Histopathologically, an intraarticular lipoma contains mature adipocytes covered by synovial tissue and may have a vascular pedicle and fibrous septa. Intraarticular lipomas with osteochondroid metaplasia or osseous metaplasia have been reported and have a possible association with repeated trauma [17, 24]. Therefore, an intraarticular lipoma is a true neoplastic tumor of unknown etiology [24, 28]. The indolent slow-growing clinical courses of an intraarticular lipoma without metastasis similar to a subcutaneous lipoma were observed clinically. However, the natural history of an intraarticular lipoma has not been well studied.
Typically, MRI findings of an intraarticular lipoma are high signal intensity on T1- and T2-weighted images that is isointense relative to subcutaneous fat tissue and contains thin delicate thin fibrous septa.
The standard treatment of an intraarticular lipoma of the knee has not been established. Either open excision or arthroscopic excision has been performed [7]. There were no local tumor recurrences of an intraarticular lipoma after arthroscopic excision in previous studies [3, 10, 19, 27], which seems to be a reliable treatment for some intraarticular lipomas. Open excision or arthroscopic excision depends on the tumor size. Arthroscopic treatment may not be acceptable for an intraarticular lipoma as large as that seen in our patient, where arthrotomy would constitute a more reliable approach. Thus, preoperative MRI is useful not only in the differential diagnosis but also in preoperative planning.
We report the case of a 55-year-old woman who presented with a painless, palpable, slow-growing mass in her right knee for 10 years. She had successful complete excision of the mass by arthrotomy with a medial parapatellar incision, good postoperative recovery with full ROM of the knee, and no recurrence 3 months after the surgery.
An intraarticular lipoma is an uncommon lesion and can be challenging to diagnose at initial presentation, as it was in our patient. The presentation of an intraarticular lipoma is similar to that of many other intraarticular lesions, such as lipoma arborescens, PVNS, liposarcoma, and Hoffa’s disease. Characteristic MRI findings can help in differentiating an intraarticular lipoma from other intraarticular lesions and in preoperative planning.
Acknowledgments
We thank Yih-Chau Lu MD for contributions to the discussion and management for this patient. We also thank Meng-Yuan Tsai MD and Clement Kuen-Huang Chen MD for their contributions and advice on the radiologic-pathologic correlations and findings.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Arkun R, Memis A, Akalin T, Ustun EE, Sabah D, Kandiloglu G. Liposarcoma of soft tissue: MRI findings with pathologic correlation. Skeletal Radiol. 1997;26:167–172. doi: 10.1007/s002560050214. [DOI] [PubMed] [Google Scholar]
- 2.Bancroft LW, Kransdorf MJ, Peterson JJ, O’Connor MI. Benign fatty tumors: classification, clinical course, imaging appearance, and treatment. Skeletal Radiol. 2006;35:719–733. doi: 10.1007/s00256-006-0189-y. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein AD, Jazrawi LM, Rose DJ. Arthroscopic treatment of an intra-articular lipoma of the knee joint. Arthroscopy. 2001;17:539–541. doi: 10.1053/jars.2001.22414. [DOI] [PubMed] [Google Scholar]
- 4.Bouali H, Deppert EJ, Leventhal LJ, Reeves B, Pope T. Pigmented villonodular synovitis: a disease in evolution. J Rheumatol. 2004;31:1659–1662. [PubMed] [Google Scholar]
- 5.Bravo SM, Winalski CS, Weissman BN. Pigmented villonodular synovitis. Radiol Clin North Am. 1996;34:311–326. [PubMed] [Google Scholar]
- 6.Dietemann JL, Bonneville JF, Runge M, Jeung MY, Weintraub A, Wackenheim A. Computed tomography of lumbar apophyseal joint lipoma: report of three cases. Neuroradiology. 1989;31:60–62. doi: 10.1007/BF00342032. [DOI] [PubMed] [Google Scholar]
- 7.Ehlinger M, Adam P, Bierry G, Dosch J, Taglang G, Bonnomet F. Supra-patellar swelling and knee instability. Skeletal Radiol. 2010;39:1047–1048. doi: 10.1007/s00256-010-0881-9. [DOI] [PubMed] [Google Scholar]
- 8.Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182:733–739. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 9.Hill JA, Martin WR, 3rd, Milgram JW. Unusual arthroscopic knee lesions: case report of an intra-articular lipoma. J Natl Med Assoc. 1993;85:697–699. [PMC free article] [PubMed] [Google Scholar]
- 10.Hirano K, Deguchi M, Kanamono T. Intra-articular synovial lipoma of the knee joint (located in the lateral recess): a case report and review of the literature. Knee. 2007;14:63–67. doi: 10.1016/j.knee.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 11.Hoffa A. Influence of adipose tissue with regard to the pathology of the knee joint. JAMA. 1904;43:795–796. doi: 10.1001/jama.1904.92500120002h. [DOI] [Google Scholar]
- 12.Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997;17:675–691. doi: 10.1148/radiographics.17.3.9153705. [DOI] [PubMed] [Google Scholar]
- 13.Keser S, Bayar A, Numanoğlu G. An unusual cause for anterior knee pain: strangulated intra-articular lipoma. Knee Surg Sports Traumatol Arthrosc. 2005;13:585–588. doi: 10.1007/s00167-004-0595-4. [DOI] [PubMed] [Google Scholar]
- 14.Khan AM, Cannon S, Levack B. Primary intra-articular liposarcoma of the knee: case report. J Knee Surg. 2003;16:107–109. [PubMed] [Google Scholar]
- 15.Kidwai AS, Klassen C, Hemphill S, Griffiths HJ. Radiologic case study: intra-articular synovial lipoma. Orthopedics. 2005;28(522):611–613. doi: 10.3928/0147-7447-20050601-01. [DOI] [PubMed] [Google Scholar]
- 16.Kloen P, Keel SB, Chandler HP, Geiger RH, Zarins B, Rosenberg AE. Lipoma arborescens of the knee. J Bone Joint Surg Br. 1998;80:298–301. doi: 10.1302/0301-620X.80B2.8244. [DOI] [PubMed] [Google Scholar]
- 17.Lee F, Keel SB, Gebhardt MC, Rosenthal DI. Intra-articular lipoma with osteochondroid metaplasia in the knee joint. Skeletal Radiol. 2001;30:230–233. doi: 10.1007/s002560100339. [DOI] [PubMed] [Google Scholar]
- 18.Margheritini F, Villar RN, Rees D. Intra-articular lipoma of the hip: a case report. Int Orthop. 1998;22:328–329. doi: 10.1007/s002640050271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marui T, Yamamoto T, Kimura T, Akisue T, Nagira K, Nakatani T, Hitora T, Kurosaka M. A true intra-articular lipoma of the knee in a girl. Arthroscopy. 2002;18:E24. doi: 10.1016/S0749-8063(07)60029-2. [DOI] [PubMed] [Google Scholar]
- 20.Matsumoto K, Okabe H, Ishizawa M, Hiraoka S. Intra-articular lipoma of the knee joint: a case report. J Bone Joint Surg Am. 2001;83:101–105. doi: 10.2106/00004623-200101000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Min KD, Yoo JH, Song HS, Lee BI. A case of intra-articular synovial lipoma of the knee joint causing patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2010;18:1094–1097. doi: 10.1007/s00167-009-1005-8. [DOI] [PubMed] [Google Scholar]
- 22.Motsis E, Vasiliadis HS, Xenakis TA. Intraarticular synovial lipoma of the knee located in the intercondylar notch, between ACL and PCL: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2005;13:683–688. doi: 10.1007/s00167-004-0600-y. [DOI] [PubMed] [Google Scholar]
- 23.Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433–1466. doi: 10.1148/rg.245045120. [DOI] [PubMed] [Google Scholar]
- 24.Pudlowski RM, Gilula LA, Kyriakos M. Intraarticular lipoma with osseous metaplasia: radiographic-pathologic correlation. AJR Am J Roentgenol. 1979;132:471–473. doi: 10.2214/ajr.132.3.471. [DOI] [PubMed] [Google Scholar]
- 25.Ryu KN, Jaovisidha S, Schweitzer M, Motta AO, Resnick D. MR imaging of lipoma arborescens of the knee joint. AJR Am J Roentgenol. 1996;167:1229–1232. doi: 10.2214/ajr.167.5.8911186. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi S, Yamamoto T, Matsushima S, Yoshiya S, Matsubara N, Matsumoto T. Solitary intraarticular lipoma causing sudden locking of the knee: a case report and review of the literature. Am J Sports Med. 2003;31:297–299. doi: 10.1177/03635465030310022401. [DOI] [PubMed] [Google Scholar]
- 27.Tudisco C, Farsetti P, Febo A. Solitary intra-articular lipoma locking the knee in a young boy. J Pediatr Orthop B. 2008;17:131–133. doi: 10.1097/BPB.0b013e3280e12a83. [DOI] [PubMed] [Google Scholar]
- 28.Yeomans NP, Robertson A, Calder SJ. Torsion of an intra-articular lipoma as a cause of pseudo locking of the knee. Arthroscopy. 2003;19:E27. doi: 10.1053/jars.2003.50078. [DOI] [PubMed] [Google Scholar]
- 29.Yilmaz E, Karakurt L, Akpolat N, Özdemir H, Belhan O, İncesu M. Intra-articular lipoma of the knee joint in a girl. Arthroscopy. 2005;21:98–102. doi: 10.1016/j.arthro.2004.09.004. [DOI] [PubMed] [Google Scholar]



