Abstract
Background
The incidence of heterotopic ossification (HO) after hip arthroscopy reportedly ranges from less than 1.0% to 6.3%. Although open debridement has been described and a few series mention arthroscopic debridement, the techniques for arthroscopic excision of HO have not been described in detail. We describe the arthroscopic treatment of this complication.
Description of Technique
Revision arthroscopy was completed in the central and peripheral compartments using prior portals and fluoroscopy was used to identify the HO. Spinal needle localization was used to triangulate onto the HO. Cannulas were inserted over the spinal needle. Once the HO was clearly identified with the arthroscope, it was excised using a burr and confirmed on fluoroscopy.
Methods
We retrospectively reviewed 66 patients who underwent arthroscopic treatment of femoroacetabular impingement between July 2008 and June 2010. There were 36 females and 30 males with an average age of 38 years (range, 15–68 years). Eight of the 66 (12%) patients had HO develop. Using the grading of Brooker et al., six patients had Grade 1, one had Grade 2, and one had Grade 3 HO. Three patients with HO were symptomatic and underwent arthroscopic resection. We obtained modified Harris hip scores (HHS) and radiographs at followup. The minimum followup for the three patients with revision surgery was 2 years (mean, 2 years 2 months; range, 2 years–2 years 8 months).
Results
The three patients who underwent arthroscopic resection had HHS ranging from 85 to 96 at last followup. No patient had recurrence of HO.
Conclusions
Our data suggest HO is not uncommon after hip arthroscopy for the treatment of femoroacetabular impingement but most patients have minor degrees and no symptoms. In symptomatic patients, arthroscopic excision appears to relieve pain and restore function.
Introduction
The concept of femoroacetabular impingement (FAI) is increasingly recognized as a cause of hip pain in young adults [1, 14, 15]. With advances in arthroscopic technique and instrumentation, hip arthroscopy has become an increasingly common method of treatment [5, 7, 10, 11]. Despite its increasing use, numerous clinical studies have described complications with hip arthroscopy, including nerve injury related to traction, extraabdominal fluid extravasation, avascular necrosis, infection, femoral neck fracture, hip instability, and heterotopic ossification (HO) [2, 5, 7, 9–11, 15, 16].
A range of HO after hip arthroscopy from less than 1.0% to 6.3% has been reported in series ranging from 96 to 616 patients [2, 5, 7, 9–11, 15, 16]. Furthermore, the incidence of HO was reported as much as 8.3% to 33% in subsets of two series in which patients received limited or no prophylaxis with NSAIDs [2, 16]. These series briefly mention treating patients with arthroscopic and open debridement, but arthroscopic excision of HO is not described in detail [2, 10–13, 16].
Bedi et al. reported that of the 29 hips that had HO develop postoperatively, seven underwent revision surgery for excision of HO at a mean duration of 11.6 months after the index procedure [2]. Three hips with Grade 1 or 2 HO underwent arthroscopic HO excision and four hips with Grade 3 or 4 HO underwent open HO excision. The surgical technique was not described and the followup and improvement were not quantified. Larson and Giveans compared arthroscopic labral debridement and refixation in patients with FAI and found three patients with symptomatic HO in the debridement group and none in the labral refixation group [10]. Two of these patients underwent revision hip arthroscopy and postoperative radiation to remove the symptomatic HO. The surgical technique, indications, efficacy, and followup were not described [10].
The purpose of our study is to describe the arthroscopic treatment of three patients with symptomatic HO and report postoperative pain and function.
Surgical Technique
The indications for revision hip arthroscopy for HO are: (1) symptoms sufficient to cause pain and dysfunction in the hip which are different than the patient’s preoperative labral or intraarticular symptoms, (2) limitation in active or passive ROM compared with the nonsurgical side, (3) identifiable HO on radiographs, and (4) concomitant intraarticular hip disorder such as unaddressed FAI or retears of the labrum. The contraindications are: (1) Grade 4 HO with extensive bone formation, (2) posterior location of HO, (3) immature HO, (4) substantial arthritis of the hip, and (5) an obese patient where access may be difficult. For patients with symptomatic HO, revision hip arthroscopy was performed. Imaging was obtained after the index procedure to determine if there was any unaddressed labral, cartilaginous, ligamentous, bony disorder or any sequelae associated with FAI.
The senior author (TY) performed all procedures with the patient in the supine position and under general anesthesia [4]. Traction was achieved with a Smith & Nephew Hip Distractor (Andover, MA, USA) and confirmed with C-arm fluoroscopy. Prior portal incisions were used to perform a diagnostic arthroscopy of the central compartment. In all three cases, a second look at the labral repairs showed intact labral repairs with reconstituted chondrolabral junctions. In one case (Patient 3), the HO bridged with the acetabular rim. A burr was used to perform further acetabuloplasty without disrupting the labral repair. Once we completed arthroscopy of the central compartment, the traction was released and the peripheral compartment was entered. Any unaddressed cam disorder was addressed at this time. The peritrochanteric space also can be entered at this time if there is any gluteus medius or minimus disorder causing lateral-sided symptoms. After arthroscopy was completed in the central and peripheral compartments, fluoroscopy was used to identify the HO. Spinal needle localization was used to triangulate onto the HO. Cannulas were inserted over the spinal needle. Once the HO was clearly identified with the scope, it was excised using a burr (Fig. 1) and larger fragments were extracted using a grasper. Fluoroscopy was used at the end of the case to confirm excision of HO.
Fig. 1.
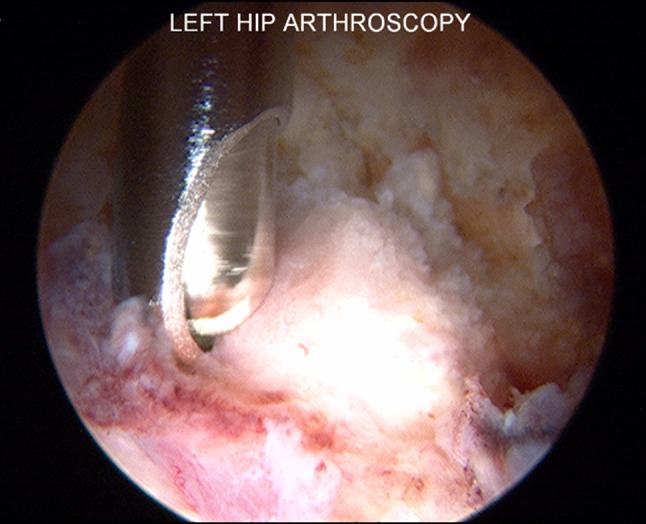
This is an arthroscopic image of the excision of HO in the hip capsule with an arthroscopic burr after needle localization.
Postoperatively, patients were partial weightbearing with crutches for 4 weeks. A cryotherapy pad was used for 2 weeks and a hinged hip brace was used for the first week. Formal physiotherapy was begun 4 weeks after surgery and continued twice a week for approximately 3 months until the patient achieved full ROM and strength. Return to all activities without restriction was allowed at 6 months. Postoperative HO prophylaxis with NSAIDs versus radiation was discussed with each patient. Patients were given the option of 2 weeks of indomethacin 50 mg or radiation therapy performed shortly after surgery or receiving NSAIDs and radiation. Risks, benefits, and alternatives of each treatment option were discussed.
Patients and Methods
We retrospectively reviewed all 66 patients who underwent arthroscopic treatment of FAI by the senior author (TY) between July 2008 and June 2010. There were 36 females and 30 males with an average age of 38 years (range, 15–68 years). Each patient’s HO was classified using the grading system of Brooker et al. [3]; six had Grade 1, one had Grade 2, and one had Grade 3 HO. Eight of the 66 patients (12%) had HO confirmed radiographically (Table 1). Three of the eight patients had arthroscopic excision of HO at the time of this report. The minimum followup for all 66 patients was 24 months (mean, 28 months; range, 24–36 months) and the minimum followup for the three patients after revision surgery was 24 months (mean, 26 months; range, 24–32 months).
Table 1.
Patients with HO
| Patient number | Sex | Age (years) | Weight (kg) | BMI (kg/m2) | Resection | Brooker grade | Preoperative/postoperative Harris hip scores—index procedure | Preoperative/ postoperative Harris hip scores after HO excision | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 19 | 80.3 | 27.1 | Cam | 2 | 56/96 | N/A | None |
| 2 | M | 53 | 92.1 | 29.1 | Cam/pincer | 1 | 44/93 | N/A | None |
| 3 | F | 48 | 68.0 | 25.8 | Pincer | 1 | 52/70 | 70/85 | Arthroscopic resection, indomethacin, radiation therapy |
| 4 | F | 53 | 55.8 | 21.1 | Pincer | 1 | 52/85 | N/A | None |
| 5 | M | 34 | 90.0 | 26.9 | Cam/pincer | 1 | 63/85 | N/A | None |
| 6 | M | 29 | 73.5 | 23.2 | Cam/pincer | 1 | 59/78 | 78/96 | Indomethacin, arthroscopic resection, radiation therapy |
| 7 | M | 29 | 59.9 | 21.3 | Pincer | 1 | 56/92 | N/A | None |
| 8 | F | 22 | 75.0 | 26.7 | Pincer | 3 | 45/70 | 70/96 | Indomethacin, arthroscopic resection |
HO = heterotopic ossification; BMI = body mass index; M = male; F = female; N/A = not applicable.
Patients were evaluated at regular intervals (1 week, 1 month, 3 months, 6 months, and 1 year) or more frequently if necessary. At each visit we obtained modified Harris hip scores (HHS [8]). The modification as described by Byrd and Jones includes pain (44 points) and function (47 points), with a multiplier of 1.1, for a total possible score of 100 [6]. Followup radiographs after revision surgery were obtained at 1 week, 6 months, and 1 year or more often if necessary. Demographic data for all patients including age, sex, diagnosis, weight, height, BMI, and intraoperative findings were recorded (Table 2). All data collection was approved by our institutional review board. Postrevision radiographs were evaluated by the senior author (TY) and a radiologist (CP) for recurrence of HO. There were no differences in radiographic evaluations between the senior author (TY) and the radiologist (CP).
Table 2.
Demographic data
| Patient parameter | Data |
|---|---|
| Average age | 38 years (range, 15–68 years) |
| Sex | 30 males 36 females |
| Average weight | 77.2 kg (range, 45.3–113.4 kg) |
| Average BMI | 26.1 kg/m2 (range, 17.8–40.4 kg/m2) |
| Intraoperative findings | 6 hips with cam 18 hips with pincer 42 hips with cam/pincer |
| Preoperative/postoperative average Harris hip score for a patient without HO | 55/90 |
BMI = body mass index; HO = heterotopic ossification.
Results
The mean modified HHS at last followup were 90 for patients without HO after surgery and 83 for those with HO. For the three patients who had revision surgery for HO, their mean modified HHS was 73 (range, 70–78) after the index procedure but improved to 92 (range, 85–96) after arthroscopic excision of HO. Two of the three patients who underwent arthroscopic excision of HO had Brooker Grade 1 HO and one had Grade 3 HO. Each patient presented after the index procedure with either pain or stiffness that was different from their initial chief complaint and had radiographic evidence of HO.
One patient (Patient 3 in Table 1), a 48-year-old woman who had Grade 1 HO after labral repair and pincer resection, underwent revision surgery and intraoperatively it was discovered that she had a large anterolateral spur that was confluent with the area of HO and this was removed with a burr. She was sent home with 2 weeks of 50 mg indomethacin twice a day. The next day the patient underwent radiation therapy for HO prophylaxis with 700 cGy in one fraction. At latest followup (24 months), the patient was doing well with painless, full hip ROM and her lateral pain has completely resolved. Her HHS improved from 70 to 85. She has returned to playing soccer.
Another patient (Patient 6 in Table 1), a 29-year-old man, presented for 3-month followup and reported resolution of his original symptoms after arthroscopic labral debridement, acetabuloplasty, and femoral neck osteochondroplasty, but reported new stiffness and discomfort, which he had not felt before with abduction of the hip. His radiograph showed Brooker Grade 1 HO (Fig. 2). He was prescribed indomethacin but continued to have stiffness and followup radiographs showed continued HO. Seven months after his initial procedure, the patient underwent arthroscopic excision of HO measuring 1.0 × 1.0 × 0.3 cm. Postoperatively, he was treated with 50 mg indomethacin twice a day for 2 weeks. The next day the patient underwent radiation therapy for HO prophylaxis with 700 cGy in one fraction. At last followup (28 months), the patient reported substantial relief of his lateral pain compared with his preoperative symptoms. On examination he had full ROM and no signs of impingement and his HHS improved from 78 to 96. He has returned to running.
Fig. 2.

This AP radiograph shows the hips of a 29-year-old man who had Brooker Grade 1 HO develop after left hip arthroscopy. The patient subsequently underwent revision surgery.
The third patient (Patient 8 in Table 1) who underwent arthroscopic excision of HO is a 22-year-old woman who 3 months after acetabuloplasty, pincer resection, and labral repair with two anchors, noted pain with flexion to 70° and minimal internal and external rotation owing to pain. A radiograph of her hip taken at the 3-month visit showed Brooker Grade 3 HO (Fig. 3). She was prescribed indomethacin but continued to have hip pain. Eight months after her initial surgery she underwent excision of HO measuring 1.5 × 0.5 × 0.3 cm. At latest followup (26 months) she is substantially improved and her HHS improved from 70 to 96. All three patients were given the option of postoperative HO prophylaxis with indomethacin for 2 weeks or a one-time dose of radiation or both. The third patient was apprehensive about receiving radiation and therefore chose chemoprophylaxis only.
Fig. 3.

This AP radiograph shows the hips of a 22-year-old woman who had Brooker Grade 3 HO develop after right hip arthroscopy. She subsequently underwent revision surgery.
Discussion
Arthroscopic excision of HO provides a minimally invasive technique for removal of symptomatic ectopic bone around the hip. Most of the literature on HO surrounding the hip comes from the arthroplasty research which describes open surgical excision [16]. Although no comparison of open versus arthroscopic HO excision has been published, we believe arthroscopic excision, by its minimally invasive nature, is associated with less morbidity than open excision. Our purpose was to describe the arthroscopic treatment of three patients with symptomatic HO and report postoperative pain and function.
There are several important limitations associated this study. First, our study is a small retrospective review of three patients without a comparison group of patients treated either nonoperatively or with an alternate treatment. Furthermore, patients had varying procedures depending on the nature of their disorder. Second, we did not investigate the role of HO prophylaxis in this study. Our focus was to determine our incidence of HO after hip arthroscopy and describe its arthroscopic excision. Future studies should address the prevention of this complication by investigating the role of chemical prophylaxis or radiation therapy. Third we have limited followup (mean, 26 months) for the three patients in our study. Fourth, although patients’ symptoms correlated with the development of HO and were relieved with its excision, there may be confounding variables that influenced their symptoms and resolution of symptoms after revision surgery that we have not identified.
In our series we found a 12.1% (eight of 66) incidence of patients having HO develop after hip arthroscopy. Three patients were symptomatic and have elected arthroscopic excision at this time. None of the patients in our series received HO prophylaxis (medication or radiation) and this likely contributed to our higher incidence than the range of HO after hip arthroscopy of less than 1.0% to 6.3% cited in the current literature [2, 5, 7, 9–11, 15, 16]. The incidence of HO has been reported as much as 8.3% to 33% in the subset of two series where patients received limited or no prophylaxis with NSAIDs [2, 16]. Other investigators have had lower incidences of HO. Laude et al. reported one patient with HO in their series of 100 hips treated for FAI using a miniopen anterior Hueter approach with arthroscopic assistance [13]. This patient had Brooker Type 2 HO and underwent revision for excision of HO 33 months postoperatively [13]. Byrd and Jones reported only one patient with HO in their series of 207 hips with cam-type FAI treated with arthroscopic femoroplasty [5]. This patient had HO develop in the hip capsule but did not preclude a high HHS and warranted no treatment [5].
The treatment of HO after arthroscopic surgery for FAI has not been well described in the literature. Treatment has varied from benign neglect to open and arthroscopic debridement. Larson and Giveans reported six hips (6.0%) with postoperative heterotopic bone formation in their series of 100 hip arthroscopies; one of these patients had substantial motion limitation resulting from ossification of the iliopsoas tendon [10]. However, this motion deficit resolved at 1 year without additional treatment [10]. They did not mention treatment for the remaining five patients with HO in their study. In another series, Larson and Giveans examined arthroscopic debridement versus refixation of the acetabular labrum associated with FAI [11]. Heterotopic bone developed postoperatively in three (8.3%) of 36 patients in the débridement group. Two of these patients subsequently had revision hip arthroscopy and postoperative irradiation to remove symptomatic heterotopic bone. None of the patients in the refixation group had HO develop [11]. After this complication, they treated subsequent patients with naproxen (500 mg twice daily) for 3 weeks postoperatively. Gedouin et al. also cited the development of HO as a complication in their multicenter series on the assessment of arthroscopic management of FAI [7]. Of the seven complications (6%) they observed, HO developed in three patients: two with Brooker Grade 2 and one with Grade 3. The patient with Grade 3 HO had a preoperatively osteoarthritic hip and was treated with a THA. One patient with Grade 2 HO had flexion limited to 100° at latest followup but had substantial pain relief.
Since the last arthroscopic resection of HO, we have focused on HO prophylaxis. We have implemented a protocol of 50 mg indomethacin twice a day for 2 weeks postoperatively and have not had another patient (356 consecutive patients) with this complication. The use of NSAIDS for HO prophylaxis is well documented for THA but there are only two studies examining its use for prevention of HO after hip arthroscopy [2, 16]. Randelli et al. reported on the prevalence of HO in a series of 300 patients undergoing arthroscopic management of FAI [16]. Their study looked at two groups, one that received NSAID prophylaxis after surgery and another that did not receive any prophylaxis. All of the patients who had HO develop were in the group that did not receive prophylaxis with NSAIDs [16]. Bedi et al. examined the addition of indomethacin during the acute postoperative period to an existing HO prophylactic protocol of naproxen administered for 30 days postoperatively and found a reduction in the development of HO [2].
The development of HO after hip arthroscopy for treatment of FAI is not an infrequent complication and can be symptomatic for some patients. To our knowledge, this is the first series describing arthroscopic excision of HO. Although we have a small series of patients, arthroscopic excision of HO is an important treatment option for dealing with this complication. With arthroscopic excision as we have described our three patients had pain relief and improved function.
Acknowledgments
We thank Catherine N. Petchprapa MD, musculoskeletal radiologist at NYU Hospital for Joint Diseases, for evaluation of the radiographs reported in this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med. 2012;40:854–863. doi: 10.1177/0363546511434285. [DOI] [PubMed] [Google Scholar]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 4.Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/S0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 5.Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2010;468:741–746. doi: 10.1007/s11999-009-0841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gedouin JE, May O, Bonin N, Nogier A, Boyer T, Sadri H, Villar RN, Laude F. Assessment of arthroscopic management of femoroacetabular impingement: a prospective multicenter study. Orthop Traumatol Surg Res. 2010;96(8 suppl):S59–67. doi: 10.1016/j.otsr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Ilizaliturri VM., Jr Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res. 2009;467:760–768. doi: 10.1007/s11999-008-0618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–546. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 13.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. doi: 10.1007/s00167-007-0332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Randelli F, Pierannunzii L, Banci L, Ragone V, Aliprandi A, Buly R. Heterotopic ossifications after arthroscopic management of femoroacetabular impingement: the role of NSAID prophylaxis. J Orthop Traumatol. 2010;11:245–250. doi: 10.1007/s10195-010-0121-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


