Abstract
Background
The stability of an osteochondritis dissecans (OCD) lesion of the humeral capitellum may be determined by intraoperative probing with unstable lesions being displaceable. Although preoperative imaging is used to diagnose and determine treatment of these lesions, it is unclear whether unstable lesions on imaging correspond to those found intraoperatively.
Questions/Purposes
We therefore examined the concordance between preoperative imaging and intraoperative instability and examined the imaging features of the patients who healed without surgery.
Methods
We retrospectively reviewed 61 patients who underwent OCD of the humeral capitellum surgery or nonoperative treatment. All patients had plain radiography, MRI, and/or CT scans. The presence or absence of stability was determined intraoperatively by the International Cartilage Repair Society OCD classification. We determined the sensitivity, specificity, and predictive value of various imaging findings to predict instability.
Results
The following preoperative imaging features were associated with intraoperative instability: a displaced fragment, epiphyseal closure of the capitellum, or a lateral epicondyle observed on radiographs; irregular contours of the articular surface or a high signal interface on T2-weighted MRI; and a displaced fragment observed on CT. Unstable lesions were more common when the epiphysis of the capitellum was closed. Intralesional segmentation was sensitive for detecting an unstable lesion, whereas displaced type on the radiographs and displaced fragment on the CT were specific. The following imaging findings were not seen in nonoperative patients: displaced type and closure of the epiphyseal line on radiographs, irregular contours of the articular surface, articular defects, and T2 high signal intensity interface between the fragments and their bed on the MRI or a displaced fragment on the CT.
Conclusions
Although we found high sensitivity for some preoperative findings on imaging, none reached 100% of sensitivity. Preoperative MRI related to the intraoperative assessment of stability.
Level of Evidence
Level III, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
For determining the best treatment for osteochondritis dissecans (OCD) of the humeral capitellum, it is important to clarify whether the lesions are stable or unstable. We define unstable OCD lesions as those with fragments that can be displaced by intraoperative probing. MRI is commonly used to assess the stability of OCD lesions of the knee [4]. In a retrospective study of 106 patients, Takahara et al. [9, 10] suggested a stable lesion was likely with an open capitellar growth plate, radiolucency-type OCD as observed on plain radiographs, and < 20° restriction of elbow motion, whereas they presumed the lesion was likely unstable if one of these three conditions was not satisfied.
Minami et al. [7] classified OCD of the humeral capitellum into three radiographic grades: Grade I, radiolucency; Grade II, a nondisplaced fragment; and Grade III, a displaced or detached fragment. Kijowski and De Smet [5] detected OCD of the capitellum on anterior and lateral plain radiographs of the elbow in only seven of 15 patients. Because OCD lesions may be underdiagnosed on the basis of AP radiographs of the elbow in extension, Takahara et al. [10] recommended using an anterior image of the elbow in 45° flexion and an oblique image of the same in 30° external rotation. T2-weighted MRI findings indicate instability is a high signal intensity line through the articular cartilage, articular defects, and high signal intensity interface between the fragments and their beds [2, 6, 8, 11]; these high signal intensity areas reflect the interposition of synovial fluid. MRI can also reveal cartilage lesions that are indistinct on plain radiographic images. CT is useful in ascertaining the properties of bone fragments, the location of loose bodies, and whether there is sclerosis of the joint base. It can also detect incarcerated intraarticular loose bodies [13]. Jans et al. [3] found 100% consistency of preoperative MRI and CT findings and surgical findings in 11 patients who underwent surgery. Among the patients who undergo surgical treatment, it is important for the choice of treatment whether the OCD lesion is stable or unstable; if the lesions are unstable, we plan for resection or reconstruction of the articular surface rather than fixation.
Given the limited literature and few patients on which conclusions have been reached, we examined the concordance between preoperative imaging and intraoperative instability and examined the imaging features of the patients who healed without surgery and presumably had stable lesions.
Patients and Methods
We retrospectively reviewed 78 patients (76 males, two females) who had OCD of the humeral capitellum and had plain radiography, MRI, and/or CT between 2000 and 2011. We excluded 17 patients for whom imaging data were not available. CTs were performed on 1 mm sliced (Aquilion 64; Toshiba, Tochigi, Japan) and MRIs on a 1.5-T system (Achieva Release 3.2; Philips, Eindhoven, The Netherlands). We used both a PACS system and nondigital evaluation. We divided our patients who had OCD of the humeral capitellum into two groups: operative and nonoperative. The ages of the patients at the time of the operation ranged from 9 to 17 years with an average age of 13.3 years. Nonoperative treatment was used in 11 patients who had an open capitellar growth plate on plain radiographs, radiolucent or nondisplaced lesions, and less than a 20° restriction of elbow motion [9]. The average age at the time of examination was 11.2 years (range, 10–12 years) among nonoperative patients. The indications for surgery were: (1) Minami classification Grade I [7] and T2-weighted MRI findings that indicate instability [2, 6, 8, 11]; and (2) Minami classification Grade II or III [7] and/or T2-weighted MRI findings that indicate instability [2, 6, 8, 11]. The contraindications were: (1) Minami classification Grade I or II [7] with open capitellar growth plate and not enough for the T2-weighted MRI findings that indicate instability [2, 6, 8, 11]; and (2) lack of symptoms. All patients were involved in sports: 54 baseball players; two dodgeball players; and one player each of softball, table tennis, shot put, gymnastics, and kendo.
All 50 operative patients had plain radiography. One of us (HS) classified the OCD lesions by the Minami classification as described before [7]. The reviewer was blinded to the surgical findings. However, it left the possibility of some interobserver variability for all classifications used. The patency of the epiphyseal line in the lateral epicondyle and capitellum of the humerus was examined. Among the operative group, there were eight patients with Grade I, 24 patients with Grade II, and 17 patients with Grade III. Patency of the epiphyseal line in the capitellum of the humerus was observed in 11 patients and closure was observed in 39 patients. Patency of the epiphyseal line in the lateral epicondyle of the humerus was observed in 21 patients and closure was observed in 29 patients (Table 1). On the other hand, there were seven patients with Grade I, four patients with Grade II, and none with Grade III among the nonoperative patients. Patency of the epiphyseal line in the capitellum was observed in 10 patients and closure was observed in one patient. Patency of the epiphyseal line in the lateral epicondyle of the humerus was observed in all nonoperative patients.
Table 1.
Radiographic findings and ICRS classification
| ICRS |
Minami classification grade | Epiphyseal line (humerus) | |||||
|---|---|---|---|---|---|---|---|
| I | II | III | Capitellum | Lateral epicondyle | |||
| Radiolucency | Nondisplaced | Displaced | Open | Close | Open | Close | |
| I | 0 | 1 | 0 | 1 | 0 | 1 | 0 |
| II | 3 | 6 | 0 | 4 | 5 | 7 | 2 |
| III | 3 | 14 | 6 | 4 | 19 | 8 | 15 |
| IV | 2 | 4 | 11 | 2 | 15 | 5 | 12 |
| Total | 8 | 24 | 17 | 11 | 39 | 21 | 29 |
ICRS = International Cartilage Repair Society.
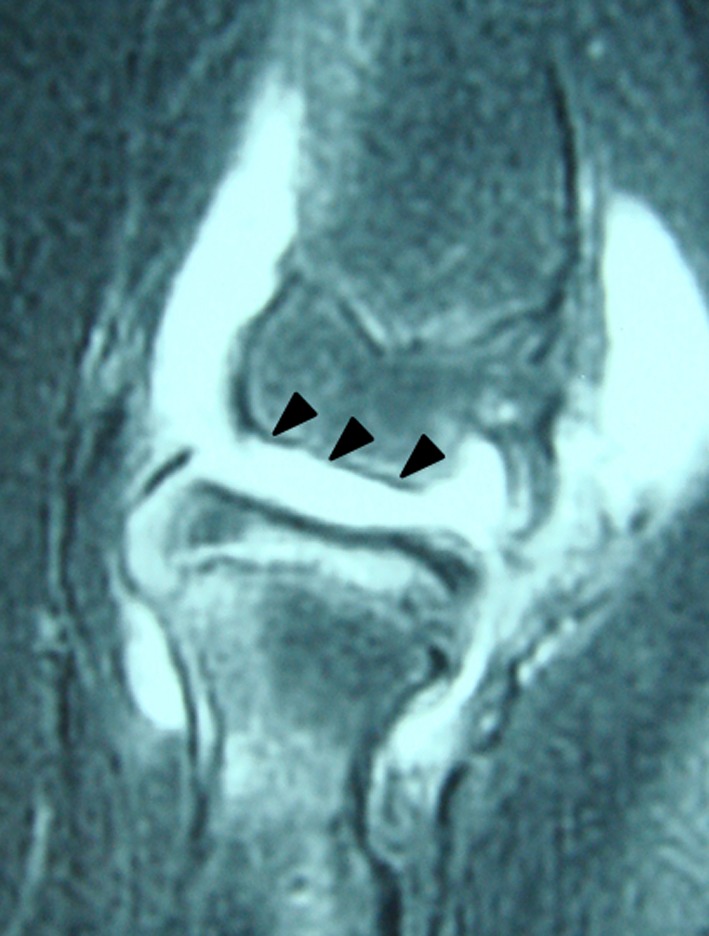
Forty-seven of the operative patients had MRI with one or more of the following findings: irregular contours of the articular surface (Fig. 1), articular defects (Fig. 2), T2 high (compared with bone) signal intensity interface (Fig. 3), and high signal intensity line through the articular cartilage (Fig. 4). For analysis, patients with no findings were designated with a minus (−) symbol and patients with findings with a plus (+) symbol. Among the operative group, irregular contours of the articular surface were observed in 29 of the patients and no irregularities were observed in 18 patients. Articular defects were observed in 20 patients and were not observed in 26 patients. T2 high signal intensity interface between the fragments and their bed was − in 23 of the patients and + in 24 patients. A T2 high signal intensity line through the articular cartilage was observed in 15 patients and was not present in 32 patients (Table 2). On the other hand, all nonoperative patients had MRI. No incidence of irregular contours of the articular surface, articular defects, and T2 high signal intensity interface between the fragments and their bed was observed in any of the nonoperative patients. A T2 high signal intensity line through the articular cartilage was observed in one patient and was not observed in 10 patients.
Fig. 1.
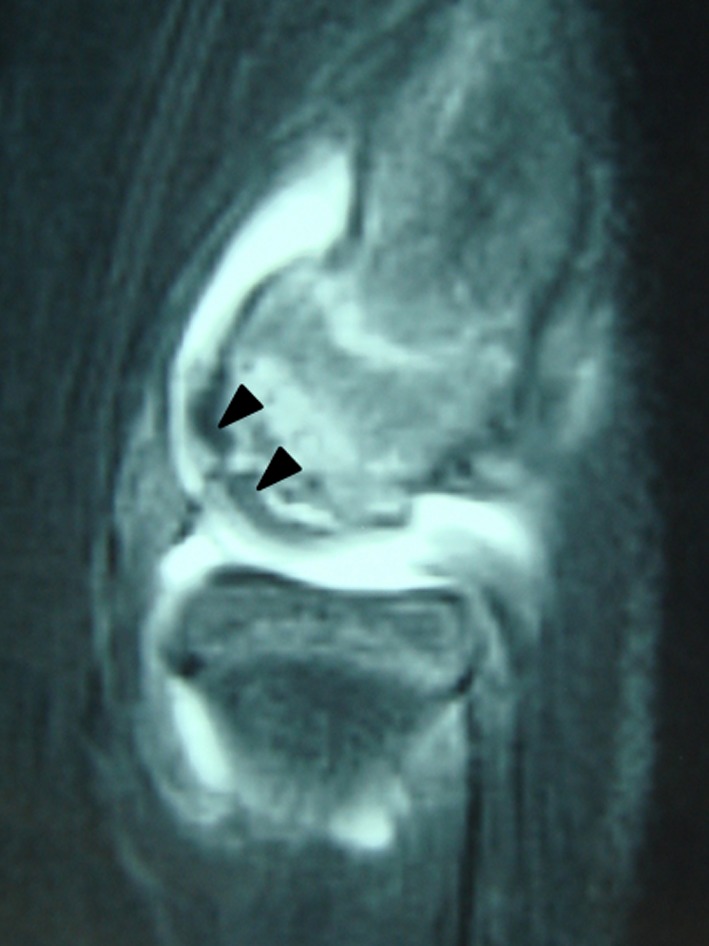
Irregular contours of the articular surface. MRI T2 fat-suppression sagittal image demonstrates articular surface irregularity of the humeral capitellum as a low signal abnormality (black arrowheads).
Fig. 2.
Articular defect. MRI T2 fat-suppression sagittal image demonstrates articular defect of the humeral capitellum as high signal abnormality (black arrowheads).
Fig. 3.
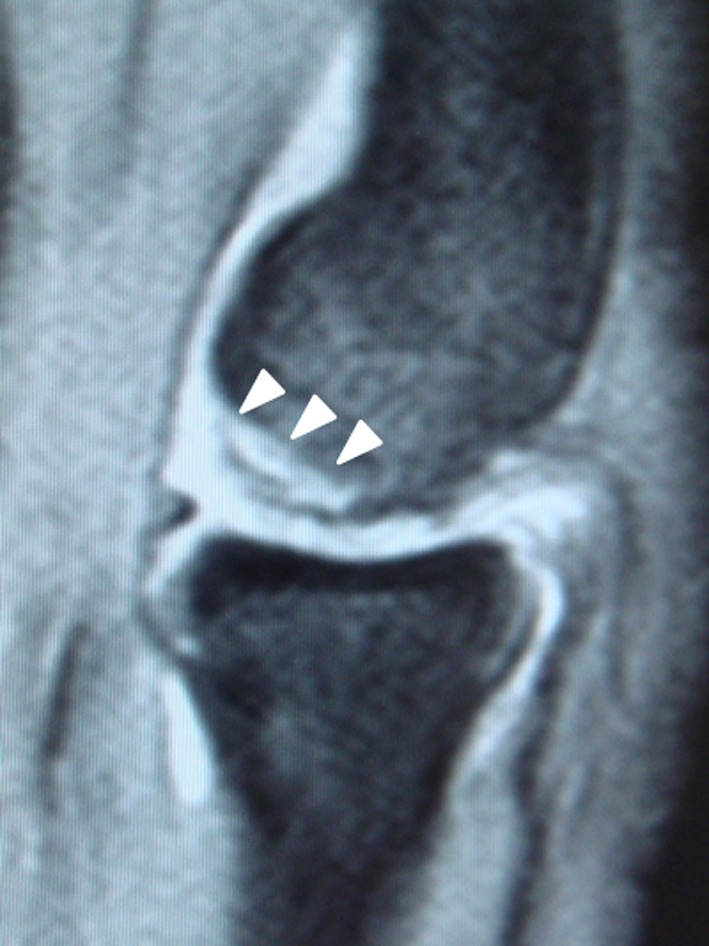
T2 high signal intensity interface. MRI T2 fat-suppression sagittal image demonstrates a linear high signal intensity interface compared with bone as indicated by the white arrowheads between the fragments and their bed.
Fig. 4.

High signal intensity line through the articular cartilage. MRI T2 fat-suppression sagittal image demonstrates a high signal intensity line through the articular cartilage of the humeral capitellum as indicated by the black arrowheads on the lesion.
Table 2.
MRI findings and ICRS classification
| ICRS |
Articular | T2 high signal intensity | ||||||
|---|---|---|---|---|---|---|---|---|
| Irregularity | Defect | Interface | Line through the articular cartilage | |||||
| − | + | − | + | − | + | − | + | |
| I | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 |
| II | 7 | 2 | 7 | 3 | 7 | 2 | 7 | 2 |
| III | 8 | 14 | 13 | 7 | 10 | 12 | 15 | 7 |
| IV | 2 | 13 | 5 | 10 | 5 | 10 | 9 | 6 |
| Total | 18 | 29 | 26 | 20 | 23 | 24 | 32 | 15 |
ICRS = International Cartilage Repair Society.
Forty-six operative patients had CT with one or more of the following findings examined: bone defects, intralesional segmentation, and displaced fragment (Fig. 5). We defined segmentation as multiple fragments of the capitellum and displaced fragment if any of the fragments had displacement on CT. Among the operative group, focal bone defects were observed in 34 patients but not in 12 patients. OCD segmentation was observed in 35 patients and but not in 10 patients, and a displaced fragment was observed in 12 patients but not in 34 patients (Table 3). On the other hand, nine of the nonoperative patients had CT. Focal bone defects were observed in eight patients but not in one patient. OCD segmentation was observed in one patient but not in eight patients. No incidence of a displaced fragment was observed in any of the nonoperative patients.
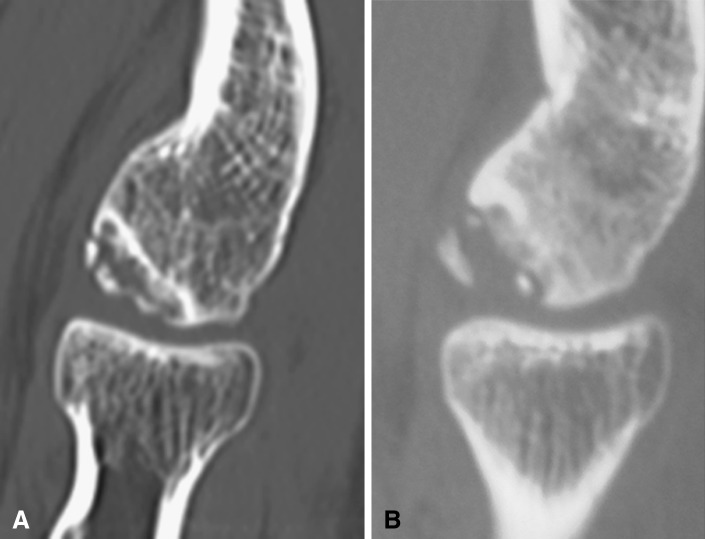
Fig. 5A–B.
Sagittal CT images demonstrate intralesional segmentation (A) and a displaced fragment (B).
Table 3.
CT findings and ICRS classification
| ICRS | Bone defect | Segmentation | Displaced fragment | |||
|---|---|---|---|---|---|---|
| − | + | − | + | − | + | |
| I | 1 | 0 | 0 | 1 | 1 | 0 |
| II | 3 | 6 | 4 | 5 | 9 | 0 |
| III | 6 | 16 | 2 | 20 | 15 | 7 |
| IV | 2 | 12 | 4 | 10 | 9 | 5 |
| Total | 12 | 34 | 10 | 35 | 34 | 12 |
ICRS = International Cartilage Repair Society.
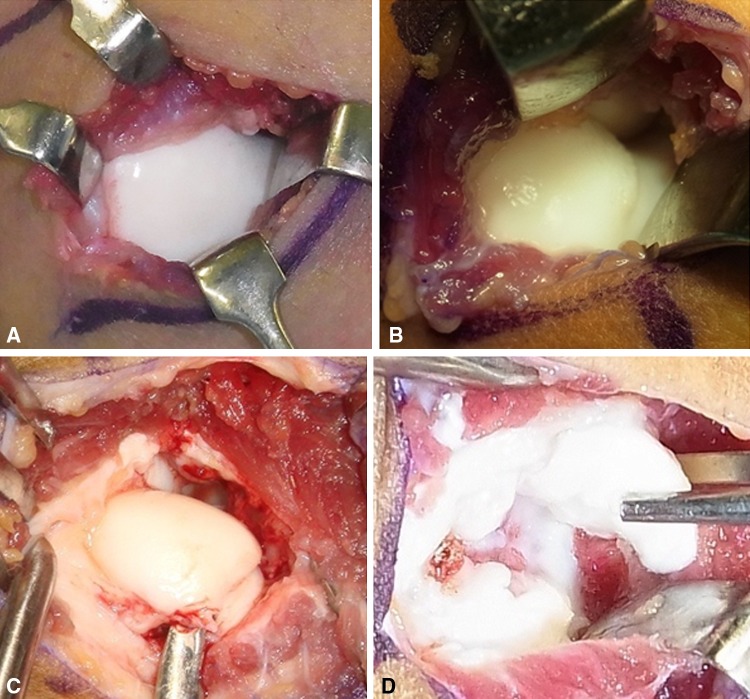
Intraoperative diagnosis was made on the basis of the International Cartilage Repair Society (ICRS) classification. The ICRS has divided OCD into four categories based on arthroscopic findings [1]. They are as follows: ICRS OCD I: stable lesions with a continuous but softened area covered by intact cartilage; II: lesions with partial discontinuity that are stable when probed; III: lesions with a complete discontinuity that are not yet dislocated (dead in situ) but are unstable when probed; and IV: empty defects as well as defects with a dislocated fragment or a loose fragment within the bed (Fig. 6). One patient with ICRS OCD I, nine patients with ICRS OCD II, 23 patients with ICRS OCD III, and 17 patients with ICRS OCD IV were evaluated intraoperatively. In the comparison, we divided ICRS OCD classification into two: stable (I and II) and unstable (III and IV). ICRS OCD III is dead in situ and unstable when probed; we were readily able to recognize such lesions as a result of their instability. We also divided Minami’s classification into two: displaced (Grade III) or not (Grade I and II) to simplify the further analysis.
Fig. 6A–D.
ICRS classification. The ICRS divides OCD into four categories as follows: ICRS OCD I: stable lesions with a continuous but softened area covered by intact cartilage (A), ICRS OCD II: lesions with partial discontinuity that are stable when probed (B), ICRS OCD III: lesions with a complete discontinuity that are not yet dislocated but are unstable when probed (dead in situ) (C), and ICRS OCD IV: empty defects as well as defects with a dislocated fragment or a loose fragment within the bed (D).
We performed bone peg fixation for an ICRS OCD II lesion. When a patient had an ICRS OCD III or IV, the fragment was removed and reconstruction of the articular surface was considered if the osteochondral defect was > 50% of the capitellar width [10].
We examined the concordance among preoperative radiographs, MRI, CT findings, and intraoperative instability (ICRS OCD III and IV) using Fisher’s exact probability test for independence. We then determined the respective sensitivity, specificity, and predictive value of preoperative imaging.
Results
At surgery, 10 patients had stable OCD and 40 patients had unstable OCD. The following preoperative findings corresponded to the intraoperative diagnosis based on the ICRS classification: displaced fragment (p = 0.010), closure of the epiphyseal line in the capitellum (p = 0.030) and lateral epicondyle (p = 0.011), MRI irregular contours of the articular surface (p = 0.004), high signal intensity interface (p = 0.036), and displaced fragment on CT (p = 0.044) (Tables 4, 5). We found no correspondence between the following findings and intraoperative instability: the presence of a high signal intensity line through the articular cartilage in the lesion (p = 0.289) or articular defects on MRI (p = 0.154), focal bone defects seen on CT (p = 0.416), and intralesional segmentation (p = 0.189). A sensitivity higher than 80% to detect an unstable lesion was obtained in the following preoperative findings: epiphyseal closure of the capitellum (85%) on radiographs and segmentation (83%) on CT. The higher specificity than 80% was obtained in the following preoperative findings: Grade III (100%) and epiphyseal closure of the lateral epicondyle (80%) on radiographs, articular irregularity (80%) and defect (80%), T2 high signal intensity interface (80%) and high signal intensity line through the articular cartilage (80%) on MRI, and displaced fragment on CT (100%). The higher predictive value than 80% was obtained in all of the preoperative findings evaluated in this study. Grade III on radiographs and displaced fragment on CT had the greatest predictive value (100%). If the preoperative MRI showed any of the mentioned unstable findings, we evaluated the lesion as unstable. Preoperative MRI correlated with intraoperative diagnosis (p = 0.002, sensitivity 84%, specificity 70%, predictive value 91%).
Table 4.
Statistical analysis of preoperative radiographic and intraoperative findings
| ICRS | Minami classification grade | Epiphyseal line (humerus) | ||||
|---|---|---|---|---|---|---|
| Capitellum | Lateral epicondyle | |||||
| I + II | III (displaced) | Open | Close | Open | Close | |
| I + II (stable) | 9 | 0 | 5 | 5 | 8 | 2 |
| III + IV (unstable) | 19 | 15 | 6 | 34 | 13 | 27 |
| p values* | 0.010 | 0.030 | 0.011 | |||
| Sensitivity | 44 | 88 | 68 | |||
| Specificity | 100 | 50 | 78 | |||
| Predictive values | 100 | 85 | 92 | |||
* Fisher’s exact probability test; ICRS = International Cartilage Repair Society.
Table 5.
Statistical analysis of preoperative imaging and intraoperative findings
| Analysis | MRI | CT | |||||
|---|---|---|---|---|---|---|---|
| Articular | T2 high signal intensity | Bone defect | Segmentation | Displaced fragment | |||
| Irregularity | Defect | Interface | Through the articular cartilage | ||||
| p values* | 0.004 | 0.154 | 0.036 | 0.289 | 0.416 | 0.189 | 0.044 |
| Sensitivity | 73 | 49 | 73 | 41 | 78 | 83 | 33 |
| Specificity | 80 | 80 | 80 | 80 | 40 | 40 | 100 |
| Predictive values | 93 | 90 | 92 | 88 | 82 | 83 | 100 |
* Fisher’s exact probability test.
Among nonoperative patients, the following imaging findings were not seen: Minami Grade III lesions and closure of the epiphyseal line on radiographs, irregular contours of the articular surface, articular defects, and T2 high signal intensity interface between the fragments and their bed on the MRI or a displaced fragment on the CT.
Discussion
A high signal rim and a high signal interface on T2 MR images of OCD lesions in the humeral capitellum reportedly suggest that the lesion is unstable [3, 12]. Takahara et al. [12] reported that MR assessment agreed with the surgical findings in six of the six cases. Because few previous studies have attempted to compare the findings of preoperative imaging modalities such as radiography, MRI, and CT with surgical findings in patients with unstable OCD of the humeral capitellum, we examined the concordance between preoperative imaging and intraoperative instability.
We acknowledge limitations to our study. First, we restricted the comparison study to patients who underwent surgery. Because no ICRS classification could be obtained for patients who underwent nonoperative treatment, the accuracy of imaging findings could not be evaluated in those patients. Second, the accuracy of imaging evaluation targeting all cases of OCD including nonoperative cases is unknown. Third, we did not record physical findings such as tenderness or ROM of the elbow. Because our nonoperative group did not include any patients with restricted elbow motion, stable OCD lesions should be measured in terms of not only imaging, but also range of elbow motion. Fourth, we reviewed retrospectively and the classification systems were not validated.
We found closure of the capitellar growth plate was sensitive for detecting instability and displacement of the fragment was specific. Articular irregularity and defects, T2 high signal intensity interface, and high signal intensity line through the articular cartilage had great specificity. The patients with nondisplaced-type OCD consisted of both stable and unstable types, and the patients with displaced-type OCD were all unstable (Table 1). Five of eight patients with radiolucency-type OCD were unstable (Table 1). In addition, segmentation on CT had high sensitivity to detect the lesion’s instability. The area can be viewed three-dimensionally with a three-dimensional CT reconstruction, which is useful in planning surgery. However, CT cannot detect loose bodies with many cartilaginous components. Preoperative diagnosis by MRI had a sensitivity of 84%. Preoperative MRI correlated with intraoperative diagnosis (Table 5) similar to the reports of Takahara et al. [12] and Jans et al. [3]. Jans et al. [3] reported that the surgical findings of instability correlated with the MRI criteria as applied to the knee [4]: high T2 signal rim, surrounding cysts, high T2 signal fracture line, and fluid-filled osteochondral defect. They also described that these MRI criteria were 100% sensitive for instability of OCD lesions of the elbow in all 11 patients who had surgery. In the current study, the following preoperative imaging was a substantial indication of lesion instability (ICRS OCD III and IV): Grade III, closure of the epiphyseal line in the capitellum and lateral epicondyle, MRI irregular contours of the articular surface, high signal intensity interface, and a displaced fragment on CT (Table 5).
None of the patients in our nonoperative group had Grade III lesions and closure of the epiphyseal line on radiographs, evidence of irregular contours of the articular surface, articular defects, and T2 high signal intensity interface between the fragments and their bed on MRI or a displaced fragment on CT. When a patient does not have any these findings, nonoperative treatment may be able to make a choice. However, no ICRS classification could be derived for these patients and the presence of a stable or unstable lesion could not be established.
We classified lesions with ICRS OCD I and II as stable and ICRS III and IV as unstable. We recommend the use of radiographs, MRI, and CT to assess the stability of the OCD lesion. The stability of such lesions should be comprehensively examined using these modalities.
Acknowledgments
We thank Dr Hitoshi Ishikawa, Department of Health Information Management, Yamagata Saisei Hospital, for his assistance and support.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85(Suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 2.Fritz RC, Steinbach LS, Tirman PF, Martinez S. MR imaging of the elbow. An update. Radiol Clin North Am. 1997;35:117–144. [PubMed] [Google Scholar]
- 3.Jans LB, Ditchfield M, Anna G, Jaremko JL, Verstraete KL. MR imaging findings and MR criteria for instability in osteochondritis dissecans of the elbow in children. Eur J Radiol. 2012;81:1306–1310. doi: 10.1016/j.ejrad.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Kijowski R, Blankenbaker DG, Shinki K, Fine JP, Graf BK, De Smet AA. Juvenile versus adult osteochondritis dissecans of the knee. Radiology. 2008;248:571–578. doi: 10.1148/radiol.2482071234. [DOI] [PubMed] [Google Scholar]
- 5.Kijowski R, De Smet A. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34:266–271. doi: 10.1007/s00256-005-0899-6. [DOI] [PubMed] [Google Scholar]
- 6.Kijowski R, De Smet A. MRI findings of osteochondritis dissecans of the capitellum with surgical correlation. AJR Am J Roentgenol. 2005;185:1453–1459. doi: 10.2214/AJR.04.1570. [DOI] [PubMed] [Google Scholar]
- 7.Minami M, Nakashita K, Ishii S, Usui M, Muramatsu I, Ogino T, Fukuda K, Sugawara M. Twenty-five cases of osteochondritis dissecans of the elbow] [in Japanese. Clin Orthop Surg. 1979;14:805–810. [Google Scholar]
- 8.Murphy BJ. MR imaging of the elbow. Radiology. 1992;184:525–529. doi: 10.1148/radiology.184.2.1620859. [DOI] [PubMed] [Google Scholar]
- 9.Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205–1214. doi: 10.2106/JBJS.F.00622. [DOI] [PubMed] [Google Scholar]
- 10.Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2008;90(Suppl 2):47–62. doi: 10.2106/JBJS.G.01135. [DOI] [PubMed] [Google Scholar]
- 11.Takahara M, Ogino T, Takagi M, Tsuchida H, Orui H, Nambu T. The natural progression of osteochondritis dissecans of the humeral capitellum. Radiology. 2000;216:207–212. doi: 10.1148/radiology.216.1.r00jl29207. [DOI] [PubMed] [Google Scholar]
- 12.Takahara M, Ogino T, Tsuchida H, Takagi M, Kashiwa H, Nambu T. Sonographic assessment of osteochondritis dissecans of the humeral capitellum. AJR Am J Roentgenol. 2000;174:411–415. doi: 10.2214/ajr.174.2.1740411. [DOI] [PubMed] [Google Scholar]
- 13.Van den Ende KI, McIntosh AL, Adams JE, Steinmann SP. Osteochondritis dissecans of the capitellum: a review of the literature and a distal ulnar portal. Arthroscopy. 2011;27:122–128. doi: 10.1016/j.arthro.2010.08.008. [DOI] [PubMed] [Google Scholar]