Abstract
Background
Pelvic flexion affects orientation of the acetabular cup; however, pelvic position is not static in daily activities. During THA it is difficult to know the degree of pelvic flexion with the patient in the lateral position and that position is static. However, surgeons need to appropriately determine pelvic tilt to properly insert the acetabular component.
Questions/purposes
We investigated the reliability of pelvic flexion angle that was measured by manually identifying the location of the pubic symphysis and bilateral anterior superior iliac spines using synthesized lateral radiographs.
Methods
We synthesized 49 lateral radiographs based on CT data. Each of the 49 radiographs had a unique position: 7° of varying lateral tilt and rotation in each of seven selected pelvic flexion angles. The pelvic flexion angle was measured three times by three independent observers in each position and determined the accuracy (based on the true value from the reconstructions) and reliability of the measures.
Results
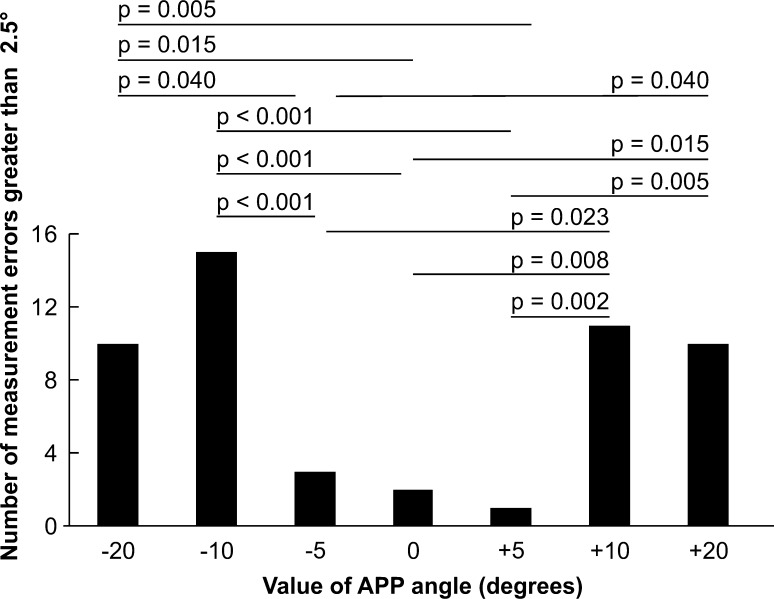
The measurement error was 0.1° (range, −4.8° to 4.0°). There was a tendency for errors when the pelvic flexion angle was 0° or ± 5°; the errors were less when the pelvic flexion angle was ± 10° or ± 20°. Lateral tilt was associated with greater error than rotation. The intraclass correlation coefficient (ICC) of the average value was 0.967. For one observer, more than two measurements are necessary for the ICC to be greater than 0.8, and only one measurement was needed for two of the three observers.
Conclusions
Our data suggest measurement of pelvic flexion angle using lateral radiographs is reliable. We recommend the measurement be performed once by two observers for better reliability.
Introduction
Orientation of the acetabular and femoral components in a THA is important to prevent malpositioning that may cause impingement of these components with subsequent dislocation, acceleration of polyethylene wear, and pain [10, 13, 24].
There is no consensus regarding the safe zone for implantation of a prosthesis in a THA. Some authors consider combined anteversion, the sum of the anteversion of the acetabular and femoral components, important [6, 21, 23]. However, pelvic position is not static; it is dynamic during standing, lying, sitting, and other daily activities and pelvic flexion might affect implantation of the acetabular cup [5, 11, 16, 22]. The same anteversion angle relative to the bony landmark cannot be used universally for all patients because many surgeons, especially those who perform THAs with patients in the decubitus position, use the operative definition of Murray [14]. It is important to know the appropriate pelvic tilt to insert the acetabular component in the best position for a given patient.
Pelvic tilt may be measured from lateral radiographs [3, 7, 11, 12] or by using a software for reconstruction of a three-dimensional (3-D) model from CT scans for planning or simulation of implantation or a CT-based surgical navigation system [2, 15, 17]. Although the various alignment parameters can be calculated with an accuracy of 1° and 1 mm using 3-D CT scans [9], this requires added expense and radiation exposure. Many measurements reflecting pelvic flexion can be measured on lateral radiographs. These include (1) pelvic flexion angle, which is the angle between the line connecting the bilateral anterior superior iliac spine (ASIS) and the pubic symphysis with the vertical line; (2) the pelvic angle, which is the angle between the line connecting the posterior superior corner of vertebra S1 to the bicoxofemoral axis and the vertical line; (3) pelvic tilt, which is the angle between the line connecting the midpoint of the sacral plate and the axis of the femoral heads with the vertical line; and (4) sacral slope, which is the angle between the superior plate of S1 and the horizontal line (Fig. 1).
Fig. 1.
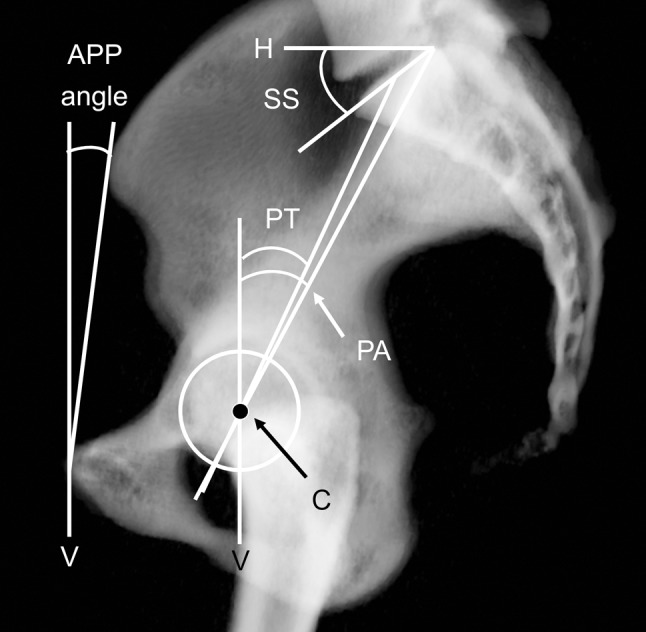
Methods for measuring pelvic flexion angle from a lateral projection radiograph of the pelvis are shown. The anterior pelvic plane (APP) angle is the angle between the line connecting the bilateral ASIS and the pubic symphysis to the vertical line (V); PA is the angle between the line connecting the posterior superior corner of S1 to the center of the femoral heads (C) to V; pelvic tilt (PT) is the angle between the line connecting the midpoint of the sacral plate to C and V; sacral slope (SS) is the angle between the superior plate of S1 and the horizontal line (H).
Measurements from lateral radiographs are easy to acquire and inexpensive [7, 11, 18, 20]. The pelvic flexion angle decreases (ie, is posteriorly tilted) 3° to 5° from the standing to supine positions [2, 15] and before and after THA [15, 17]. Eckman et al. [7] reported similar accuracy when measuring pelvic flexion angle on synthesized lateral radiographs from CT scans. Eckman et al. [7] reported an interobserver reliability of measuring the anterior pelvic plane (APP) angle using synthesized lateral pelvic radiographs from a CT-based surgical navigation system of 0.99. Furthermore, they found an interobserver error of approximately 4° to 6°, although the authors reported a correlation of 0.97 to 0.99. They did not report intraobserver reliability although they did report high interobserver variability.
We therefore investigated: (1) the reliability of single and multiple measurements of pelvic flexion angle; (2) related factors contributing to the measurement errors using a synthesized pelvic model configured from the pelvic flexion angle, lateral tilt, and external rotation of the pelvis; and (3) the number of times the surgeon should make the measurement to obtain a reliable value.
Patients and Methods
We used the CT scan of a 35-year-old woman referred to our institution for evaluation of femoroacetabular impingement. She had no abnormalities in the lumbar spine; in particular, there was no evidence of spondylolisthesis or spondylosis. The acetabula and femoral heads on both sides appeared normal on AP and lateral radiographs. We reconstructed the pelvis model using the Zed Hip® system (Lexi, Tokyo, Japan) (Fig. 1). This was used for 3-D assessment of lower extremity alignment as described previously [1, 9, 18]. One of us (NI) synthesized pelvic models. According to our preliminary study of 3-D measurements, at least 90% of patients with osteoarthritis had an APP angle of −20° to 20° for flexion and extension, respectively, and within 6° lateral tilt when in the standing position. Based on this, we first defined the APP angle in the following seven categories: −20°, −10°, −5°, 0°: parallel to the vertical line, and +5°, +10°, +20°. Next, lateral tilt (Lt) and rotation (R) were assigned to each pelvic model corresponding to each of the seven different APP angles, respectively, in the following seven categories; Lt0°–R0°: parallel to APP, Lt3°–R0°, Lt6°–R0°, Lt0–R3°, Lt0°–R6°, Lt3°–R3°, and Lt6°–R6°. Therefore, we synthesized 49 (seven × seven) 3-D pelvic models. We then synthesized a 2-D lateral radiograph using these 49 pelvis models; all pelvis models were projected to the same sagittal plane; therefore, we synthesized 49 different lateral radiographs of the pelvis.
Because multiple positioning factors might influence reliability, we identified flexion, tilt, and rotation on the synthesized images. All the values of the synthesized APP angle were true values because once we registered the bilateral ASIS and pubic symphysis, we could synthesize flexion, rotation, and lateral tilt of the pelvis digitally. The measurement error was defined as the difference between the true value of the pelvic flexion angle and its measured value.
Three orthopaedic surgeons (HS, RT, YH) measured the APP angle (Observers A, B, and C) on the simulated lateral radiographs [7]. Data collection and analysis were performed by an independent evaluator (NI) who was not one of the observers. The three observers measured 49 shuffled simulated lateral pelvic radiographs; all the images were arranged in random sequences and were assessed three times each by three individuals (ie, 441 measurements). All nine sets of radiographs were arranged in different sequences three times at 1-week intervals. Horizontal and vertical frames were established by using the software that was used for analysis regardless of pelvic flexion, tilt, and rotation; all reference frames were based on the standing position. The origin of the pelvic anatomic coordinate system was defined as the pubic symphysis. The X axis was the transverse axis, defined as a parallel line from the left ASIS to the right ASIS. The Z axis was perpendicular to the X axis in the plane of the APP. The Y axis was perpendicular to the APP. The APP angle was measured as the angle between the line connecting the bilateral ASIS to the pubic symphysis and the vertical line (Fig. 2). If a gap was present between the two ASIS (rather than coincident or overlapping), the observers measured the angle between the lines connecting the midpoint of the two ASIS as reported by Eckman et al. [7]. This was done in 378 of the 441 cases.
Fig. 2.
The relationship between the anterior pelvic plane (APP) angle and the number of measurement errors greater than 2.5° is shown. When the APP angle was within ± 5°, the number of measurement errors was substantially less than when the APP angle was within ± 10° to ± 20°.
To test the intraobserver and interobserver reliabilities, we calculated the intraclass correlation coefficient (ICC) and two-sided 95% CIs for each pairing of assessors using a weighted calculation. We showed the interobserver and intraobserver errors by using the ICC. We used multiple regression analysis to determine which of the following factors contributed to this measurement error: Lt3˚, Lt6˚, R3˚, and R6˚. We calculated how many times the observers might have to repeat the measurement to obtain an ICC greater than 0.8 using the Spearman-Brown formula as follows:
 |
where k is the number of times the observer(s) may have to repeat the measurement, ρ1 is the true value of the ICC, and ρ2 is the target value of the ICC (0.8 in this analysis). Statistical analysis was performed using SPSS software (SPSS, Inc, Chicago, IL, USA).
Results
The mean measurement error between the true and measured values of pelvic flexion was 0.1° (range, −4.8° to 4.0°) (Table 1). The ICC score of the single measurement value for the ICC was 0.767 and the average value was 0.967 (Table 1). According to multiple regression analysis, lateral tilt and rotation were considered to affect measurement error and lateral tilt was associated with greater error than rotation (Table 2). Based on the Spearman-Brown formula, an ICC of 0.80 identifies a highly reliable parameter (see Methods section). Accordingly, we calculated a kappa value that the number of measurements required by each observer to increase the ICC score greater than 0.8 varied between three and nine times for one observer, two to seven times for two observers, and four times for three observers.
Table 1.
Mean values of the anterior pelvic plane as measured by three independent observers
| Measurement | Total | Observer A | Observer B | Observer C |
|---|---|---|---|---|
| Difference from true value* (degrees) | 0.11 ± 1.59 | 0.29 ± 1.42 | −0.03 ± 1.76 | 0.10 ± 1.57 |
| Range (degrees)† | −4.8 to 4.0 | −2.8 to 3.7 | −4.8 to 4.0 | −3.2 to 3.5 |
| ICC (single measure) | 0.767 | 0.803 | 0.705 | 0.829 |
| 95% CI | 0.686–0.841 | 0.707–0.867 | 0.577–0.808 | 0.744–0.893 |
| ICC (average measure) | 0.967 | 0.924 | 0.878 | 0.936 |
| 95% CI | 0.952–0.979 | 0.879–0.955 | 0.804–0.927 | 0.897–0.962 |
| p value | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
* Average ± SD, †minimum value, maximum value; ICC = interclass correlation coefficient; CI = confidence interval.
Table 2.
Multiple regression analysis for lateral tilt and rotation
| Independent variable | Odds ratio | 95% CI |
|---|---|---|
| Lateral tilt of the pelvis | 2.60 | 1.416, 4.786 |
| Rotation of the pelvis | 1.77 | 1.004, 3.130 |
CI = confidence interval.
In the case of one of the observers, more than two measurements were necessary for the ICC to be greater than 0.8, whereas only one measurement was needed for two of the three observers (Table 3).
Table 3.
The number of repeat measurements required of the APP angle
| Observer | A | B | C | A and B | B and C | C and A | All |
|---|---|---|---|---|---|---|---|
| Difference from true value* (degrees) | 0.29 ± 1.42 | −0.03 ± 1.76 | 0.10 ± 1.57 | 0.13 ± 1.58 | 0.04 ± 1.66 | 0.19 ± 1.49 | 0.11 ± 1.59 |
| Range (degrees) | −2.8, 3.7 | −4.8, 4.0 | −3.2, 3.5 | −4.8, 4.0 | −4.8, 4.0 | −3.2, 3.7 | −4.8, 4.0 |
| ICC | 0.803** | 0.705** | 0.829** | 0.883 | 0.872 | 0.808 | 0.897 |
| 95% CI | 0.707, 0.867 | 0.577, 0.808 | 0.744, 0.893 | 0.793, 0.934 | 0.774, 0.928 | 0.649, 0.888 | 0.827–0.940 |
| p value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| k value | – | 1.6 | – | – | – | – | – |
APP = anterior pelvic plane; ICC = intraclass correlation coefficient; CI = confidence interval; k = number of repeat measurements required, * mean ± standard deviation, ** single measurement.
Discussion
Computer-assisted navigation systems decrease the number of outliers regarding positioning of acetabular components [16], whereas mechanical acetabular guides for intraoperative alignment often are insufficient to achieve the desired implant orientation [4]. Ishida et al. [8] reported a reliable way to assess the APP angle on lateral radiographs. Some investigators suggest combined anteversion of the acetabular and femoral components is important to avoid impingement of the components [4, 21, 23]. However, in two of these studies, positions were calculated using computer simulations and mathematical formulae [21, 23]. Subsequently they may be positioned incorrectly if the acetabular component is placed relative to the bony anatomy without considering the pelvic flexion angle of each patient. Surgeons therefore may need to accurately identify the position of the pelvic flexion angle because positioning of the acetabular component relative to the femoral component will change according to the change of pelvic flexion. The assessment of the pelvic flexion angle from lateral projection radiographs is convenient, inexpensive, and widely used [7, 8]. In the current study, we showed that measurement of the pelvic flexion angle from lateral radiographs is clinically reliable.
There were limitations to our study. First, we used synthesized images for the measurements rather than the original images. We frequently had difficulty identifying the ASIS and pubic symphysis owing to low bone density, overlap of the pelvis, image contrast, and soft tissue artifacts. The images used in this study, therefore, may have been easier to measure than the original radiographs, possibly resulting in smaller measurement error. Although Eckman et al. [7] reported the accuracy of lateral radiographs for measuring the pelvic flexion angle, one outlier with an error of 12.4° was observed. We suspect the observers tended to define the ASIS anteriorly when the pelvis was flexed anteriorly; therefore, APP angle seemed to be higher. Similarly, they might have tended to define the ASIS posteriorly when the pelvis was extended posteriorly; therefore, the APP angle seemed to be lower. We observed a tendency of errors greater than ± 2.5° when the APP angle was 0°, +5°, and −5° than when the APP angle was +10°, −10°, +20°, or −20° (Fig. 2). The ASIS was observed twice in almost all the cases when the pelvis was rotated. However, we speculate that when the pelvis was tilted laterally, one of the ASIS may overlap with the iliac crest and it may be difficult to define in some cases. For that reason, we recommend measurement by at least two observers, although we observed high reliability with one of our three observers. Second, it is unclear how large the distance between the two ASIS projected onto a plane is acceptable from our observations. Ishida et al. [8] obtained repeat radiographs when they found a large gap between the two ASIS. Our findings seemed to confirm smaller errors in measurement with smaller gaps between the two ASIS. Third, it is difficult to make any recommendations on the accuracy achievable through this process because we do not know the accuracy required to reduce long-term wear and improve survival.
We observed that the measurement error was 0.1° on average and the ICC was high similar to those reported by Eckman et al. [7]. Therefore, measurement of the pelvic flexion angle using a lateral radiograph of the pelvis was considered a reliable method whereas lateral radiographs can be easily acquired, convenient, and inexpensive [3, 11, 12].
We found the ICC increased to greater than 0.8 when one observer measures twice or more and when two observers measure one time each. Therefore, we believe that the average value of one observer measuring twice or more and two observers measuring once provides a reliable value whereas lateral radiographs can be easily analyzed [7].
We also showed that less pelvic rotation and lateral tilt appear to decrease the measurement error. We believe the measurement error can be decreased to correct pelvic rotation and lateral tilt during radiographic examination. These data suggest that pelvic flexion angle measurements were considered clinically useful.
When surgeons measure the pelvic flexion angle, the measurement may not correspond to the true value. In most cases, we measured the image of the same patient two or more times to determine the intraobserver variability. The intraobserver and interobserver variabilities should be low (high ICC) with a minimal risk of outliers. We found a tendency for less likelihood of errors greater than 2.5° when the APP angle was 0° or ± 5°. Nishihara et al. [15] reported the pelvic flexion angle was within ± 10° in almost 80% of patients undergoing THA. We found that when the APP angle was −10° to +10°, the measurement error was decreased. Since the errors were lower, pelvic flexion angle can be considered clinically useful in many cases. Moreover, lateral tilt and rotation were considered risk factors for measurement errors greater than 2.5° and lateral tilt was associated with greater error than rotation. We may be able to reduce the measurement errors if the rotation is corrected, for example, if the bilateral ASIS is positioned perpendicular to the x-ray film for a lateral radiograph. In standing and sitting positions, lateral tilt may not be corrected. However, in the supine position, we may be able to correct not only lateral tilt, but also rotation. With this method, the measurement errors may be reduced and reliability may be improved.
We found less measurement error with less pelvic rotation and lateral tilt. We believe the measurement is best made once by two observers.
Acknowledgments
We thank Hayato Suzuki MD, Ryota Takubo MD, and Yoji Horigome MD, for their useful input in this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ariumi A, Sato T, Kobayashi K, Koga Y, Omori G, Minato I, Endo N. Three-dimensional lower extremity alignment in the weight-bearing standing position in healthy elderly subjects. J Orthop Sci. 2010;15:64–70. doi: 10.1007/s00776-009-1414-z. [DOI] [PubMed] [Google Scholar]
- 2.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 3.Blondel B, Parratte S, Tropiano O, Pauly V, Aubaniac JM, Argenson JN. Pelvic tilt measurement before and after total hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:568–572. doi: 10.1016/j.otsr.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 4.DiGioia AM, Hafez MA, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, Kischell E, Kanade T. The Otto Aufranc Award: Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;355:8–22. doi: 10.1097/00003086-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 5.DiGioia AM, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 6.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eckman K, Hafez MA, Ed F, Jaramaz B, Levison TJ, Digioia AM., 3rd Accuracy of pelvic flexion measurement from lateral radiographs. Clin Orthop Relat Res. 2006;451:154–160. doi: 10.1097/01.blo.0000238809.72164.54. [DOI] [PubMed] [Google Scholar]
- 8.Ishida T, Inaba Y, Kobayashi N, Iwamoto N, Yukizawa Y, Choe H, Saito T. Changes in pelvic tilt following total hip arthroplasty. J Orthop Sci. 2011;16:682–688. doi: 10.1007/s00776-011-0153-0. [DOI] [PubMed] [Google Scholar]
- 9.Kobayashi K, Sakamoto M, Tanabe Y, Ariumi A, Sato T, Omori G, Koga Y. Automated image registration for assessing three-dimensional alignment of entire lower extremity and implant position using bi-plane radiography. J Biomech. 2009;42:2818–2822. doi: 10.1016/j.jbiomech.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 10.Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999;14:509–513. doi: 10.1016/S0883-5403(99)90110-9. [DOI] [PubMed] [Google Scholar]
- 11.Legaye J. The femoro-sacral posterior angle: an anatomical sagittal pelvic parameter usable with dome-shaped sacrum. Eur Spine J. 2007;16:219–225. doi: 10.1007/s00586-006-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 13.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 14.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 15.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurement of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. doi: 10.1097/01.blo.0000069891.31220.fd. [DOI] [PubMed] [Google Scholar]
- 16.Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty: a prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 17.Parratte S, Pagnano MW, Coleman-Wood K, Kaufman KR, Berry DJ. The 2008 Frank Stinchfield Award: Variation in postoperative pelvic tilt may confound the accuracy of hip navigation systems. Clin Orthop Relat Res. 2009;467:43–49. doi: 10.1007/s11999-008-0521-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sato T, Koga Y, Omori G. Three-dimensional lower extremity alignment assessment system: application to evaluation of component position after total knee arthroplasty. J Arthroplasty. 2004;19:620–628. doi: 10.1016/j.arth.2003.12.063. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki H, Endo K, Mizuochi J, Kobayashi H, Tanaka H, Yamamoto K. Clasped position for measurement of sagittal spinal alignment. Eur Spine J. 2010;19:782–786. doi: 10.1007/s00586-010-1352-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 21.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Wolf A, Digioia AM, 3rd, Mor AB, Jaramaz B. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res. 2005;437:132–137. doi: 10.1097/01.blo.0000164027.06880.3a. [DOI] [PubMed] [Google Scholar]
- 23.Yoshimine F. The safe-zones for combined cup and neck anteversion that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–1323. doi: 10.1016/j.jbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Zhu J, Wan Z, Dorr LD. Quantification of pelvic tilt in total hip arthroplasty. Clin Orthop Relat Res. 2010;468:571–575. doi: 10.1007/s11999-009-1064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]