Abstract
Background
Early diagnosis and successful treatment of juvenile osteochondritis dissecans (JOCD) is essential in preventing articular degeneration at a young age. Surgical treatment of stable JOCD lesions failing nonoperative treatment involves retroarticular or transarticular drilling to induce revascularization and healing. Multiple case series report high healing rates and infrequent complications for both retroarticular and transarticular drilling modalities; however, it is unclear from these individual reports whether one mode of drilling provides higher healing rates.
Questions/purposes
We asked whether transarticular or retroarticular drilling of stable JOCD lesions results in differing patient-oriented outcomes, rates of radiographic healing, time to radiographic healing, and complication rates.
Methods
We systematically reviewed the short-term clinical outcomes of retroarticular and transarticular drilling of stable OCD lesions. PubMed and additional sources identified 65 studies; 12 studies met inclusion criteria.
Results
Heterogeneity and quality of studies limited review to qualitative analysis. No clear differences were seen in patient-oriented outcomes after treatment with either drilling modality. Radiographic healing for JOCD lesions drilled retroarticularly occurred in 96 of 111 (86%) lesions in an average of 5.6 months. Transarticular drilling of JOCD lesions resulted in 86 of 94 (91%) lesions healing by radiography in an average of 4.5 months. No complications were reported for either drilling modality.
Conclusions
Retroarticular and transarticular drilling of stable lesions results in comparable short-term patient-oriented outcomes and radiographic healing. Further high-quality comparative studies are required to adequately compare drilling modalities, clearly define radiographic healing, and patient-oriented outcomes after nonoperative treatment.
Introduction
Osteochondritis dissecans (OCD) of the knee is a rare, localized pathologic process in which subchondral bone and adjacent articular cartilage separate from the femoral condyle. First described as “quiet necrosis” by Paget in 1870 [28] and later coined OCD by Konig in 1888 [21], its true etiology remains speculative. Various theories involve ischemic, genetic, and traumatic processes; however, its increasing incidence in skeletally immature patients most supports a theory of repetitive microtrauma as youth participation in sports increases [6, 9, 11].
Although OCD was first described more than a century ago [28], its natural history remains unclear; OCD likely manifests along a pathologic spectrum from softening of the overlying articular cartilage to osteochondral separation with loose body formation over months to years [17]. Furthermore, few high-quality studies exist to guide clinicians on most diagnostic, prognostic, and therapeutic decisions [8].
Juvenile OCD (JOCD) is differentiated from adult OCD (AOCD) by open femoral physes. In contrast to AOCD lesions, AOCD lesions with intact overlying cartilage may respond well to nonoperative measures including activity modifications, restricted weightbearing, and knee immobilization. Controversy exists over specific methods or required duration of nonoperative treatment and there is considerable uncertainty regarding its effectiveness. Some series quote a high rate of radiographic healing of more than 90% [23, 32], whereas others share less optimistic figures of less than 60% [6, 7, 30, 34]. Many authors acknowledge a frequent requirement of 6 to 18 months of nonoperative treatment to achieve healing, leading to concerns of atrophy, stiffness, and poor treatment adherence [2, 6, 16, 17].
Commonly accepted operative indications in stable JOCD lesions include failed nonoperative measures of 3 to 6 months or approaching physeal closure [11]. Arthroscopically confirmed stable JOCD lesions are drilled by one of two general modalities, transarticular or retroarticular, to create channels into subchondral bone for revascularization and bony union of the osteochondral fragment. Transarticular drilling penetrates the articular cartilage through at least one site to create multiple subchondral penetrations. Concerns with this technique involve the uncertain long-term implications for cartilage health created by articular cartilage drill sites. By contrast, retroarticular drilling spares the articular surface and physes by drilling through the side of the affected condyle or intercondylar notch. Comparatively, it necessitates fluoroscopic guidance and its technical difficulty raises the risk of incomplete lesion drilling, displacement of the OCD fragment, and inadvertent soft tissue injury around the knee.
Multiple case series [2, 18, 19] report a high rate of healing and low complication rates using either transarticular or retroarticular drilling modalities. These studies demonstrate improved clinical outcomes using a variety of patient-oriented outcome measures and high rates of radiographic healing. Kawasaki et al. [18] reported a Lysholm score of 97.7 and 100% of 15 lesions healed radiographically 16 months after retroarticular drilling. Other transarticular studies report Lysholm scores in the mid- to high 90s and radiographic healing approaching 100% [2, 19].
No high-quality studies or systematic reviews exist to guide the treating physician on the best drilling modality to optimize patient-oriented outcomes and rates of radiographic healing. We therefore asked whether retroarticular drilling for stable JOCD lesions or transarticular drilling results in differing (1) patient-oriented outcome measures; (2) radiographic healing; (3) time to healing on radiography; and (4) complications.
Search Strategy and Criteria
We searched the electronic databases Medline, Embase, and the Cochrane Collaboration July 2011 for relevant literature on drilling for stable JOCD lesions. The search of the Medline and Embase databases was limited to the title and abstract. Key words we used in combination were (1) “osteochondritis dissecans”; (2) “drilling”; and (3) “knee”. Abstracts indicating a possibility of clinical outcomes from therapeutic drilling prompted retrieval of the full-text article for detailed evaluation. The reference lists for all relevant articles were hand-searched for additional relevant articles.
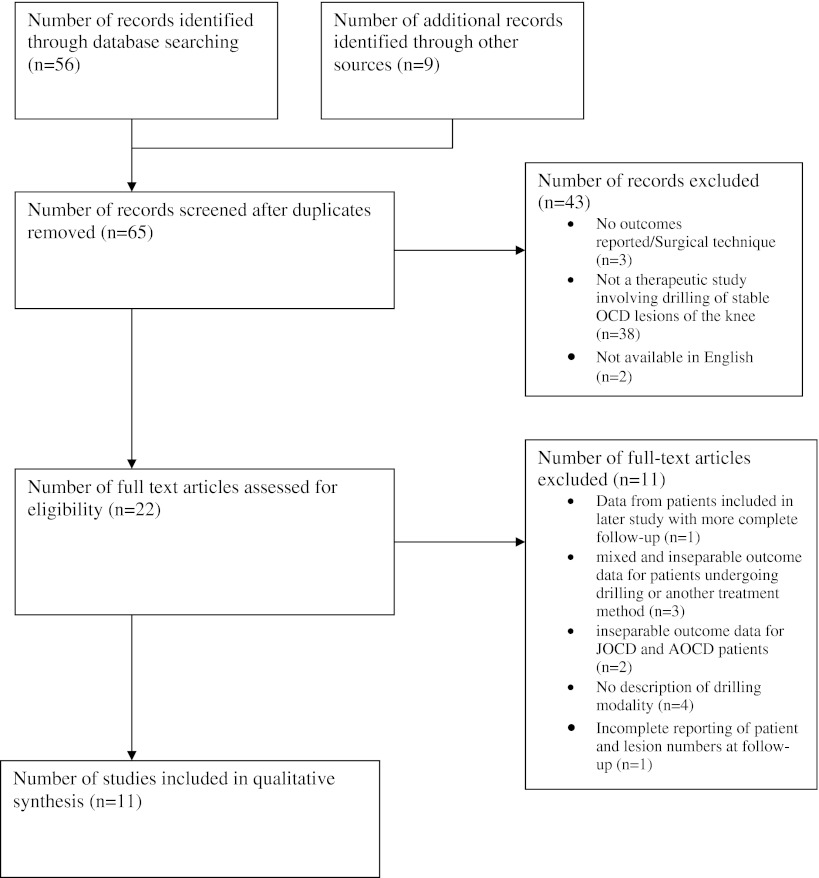
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1) depicts the number of articles identified and screened, included, and excluded with reasons for exclusion. The initial search identified 65 potentially relevant studies; 56 studies were identified through a computerized database search with an additional nine studies identified through hand-searching of article references. Subsequent review of abstracts produced 22 articles for more detailed full-text evaluation. One study was excluded as a result of inclusion of patients from a later study with more complete followup [12]. Three studies reported on mixed and inseparable outcome data for patients undergoing either drilling or another form of treatment method [16, 17, 26]. Two studies were excluded as a result of inseparable outcomes data for patients with JOCD or AOCD lesions [13, 15]. Four studies did not describe the type of drilling modality used [3, 24, 29, 33]. One study did not describe the number of patients at followup and was therefore excluded [7]. These exclusions left 11 studies (Table 1).
Fig. 1.
The review was performed systematically and qualitatively analyzed 11 studies.
Table 1.
Study and patient characteristics
| Study | Year | Level of evidence | Study design | Number of JOCD lesions at followup | Duration of followup (months)* | Age at time of surgery (years)* | Lesion location |
|---|---|---|---|---|---|---|---|
| Lee and Mercurio [22] | 1981 | IV | Retrospective case series | 1 | 7 (6–7) | 18 (12–26) | 1 MFC |
| Bradley and Dandy [5] | 1989 | IV | Retrospective case series | 11 | 24 (12–60) | 12 (11–13) | 11 MFC |
| Aglietti et al. [2] | 1994 | IV | Retrospective case series | 16 | 56 (34–104) | 12.8 (10–14) | 16 MFC |
| Anderson et al. [4] | 1997 | IV | Retrospective case series | 20 | 60 (24–108) | 13.5 (9–23) | 15 MFC |
| 5 LFC | |||||||
| Kocher et al. [19] | 2001 | IV | Prospective case series | 30 | 45 (24–86) | 12.3 (8.5–16.1) | 30 MFC |
| Louisia et al. [25] | 2003 | IV | Retrospective case series | 17 | 141 (36–312) | 13.8 (11–29) | 17 MFC |
| Kawasaki et al. [18] | 2003 | IV | Retrospective case series | 15 | 16 (12–24) | 12.5 (9–18) | 7 MFC |
| 8 LFC | |||||||
| Donaldson and Wojtys [9] | 2008 | IV | Retrospective case series | 16 | 21 (8–38) | 12.3 (9–15) | 12 MFC |
| 4 LFC | |||||||
| Adachi et al. [1] | 2009 | IV | Retrospective case series | 20 | 32 (13–62) | 12 (9–15) | 8 MFC |
| 12 LFC | |||||||
| Edmonds et al. [10] | 2010 | IV | Retrospective case series | 59 | 36.3 (1.3–72) | 13.4 (8–18.6) | 42 MFC |
| 17 LFC | |||||||
| Ojala et al. [27] | 2011 | IV | Prospective case series | 5 | 36.6 (4–79) | 15 (7–21) | 3 MFC |
| 2 LFC |
* Values expressed as means with ranges in parentheses; NR = not reported; MFC = medial femoral condyle; LFC = lateral femoral condyle; JOCD = juvenile osteochondritis dissecans.
Study characteristics determining eligibility were either published prospective or retrospective studies reporting on outcomes for patients undergoing drilling for stable JOCD lesions. We considered lesions stable if they were described as stable by the study author. Additionally, inclusion was dependent on involvement of human subjects and availability in English language. We excluded studies if they reported on patients from another study with more complete followup or did not report basic data. Specifically, studies were excluded if they did not report the skeletal maturity of patients, the stability of the OCD lesion, or the type of drilling modality used. Outcome data were required for patients with JOCD lesions undergoing drilling treatment in isolation from other treatment modalities. Additionally, studies reporting on both JOCD and AOCD lesions were excluded if separate outcomes data for JOCD lesions were not reported.
Independent data extraction and collation into a table format were performed by three reviewers (MJG, MLM, JLC). Decisions regarding table format and type of data for extraction were made by consensus among reviewers. Extracted data included first author, publication date, level of evidence, study design, number of lesions at followup, duration of followup, age at the time of surgery, lesion location, lesion type, duration of conservative management, drilling technique, diameter of wire, number of drill holes, use of fluoroscopy, postoperative weightbearing status, patient-oriented outcomes, complications, number of lesions healed by radiography, and time to healing on radiographs. The collated data from each reviewer were compared for accuracy and any inconsistencies were corrected by consensus discussions.
Three reviewers (MJG, MLM, JLC) independently assessed methodological quality, assigned level of evidence, and determined study design. A study was considered prospective if it was started before the first patient was enrolled.
The risk of bias across studies and for individual studies was assessed and reported on by the independent reviewers. A consensus was reached among the reviewers as to the importance of each bias and need for inclusion of bias in the reporting of results.
A variety of patient-oriented outcomes or composite scales was used throughout the included studies; all studies reported at least one measure of patient-oriented outcome. Four studies reported results using pain reports [2, 5, 10, 22] and two studies defined their own patient-oriented outcome scales [9, 13]. Validated composite scores were used in the remaining studies; five studies used the Hughston clinical score [1, 4, 18, 25, 27], one study used the International Knee Documentation Committee form (IKDC) [4], and three studies used the Lysholm score [1, 18, 19]. The remainder of the studies typically defined healing on radiographs as resolution of the lesion’s sclerotic rim and/or resolution of the radiolucent zone behind the OCD lesion.
Results
Patient-oriented outcome scores were comparable in all studies using either drilling modality. Five studies used a Hughston score to report patient-oriented outcome data [1, 4, 18, 25, 27]. Three of these studies used a retroarticular technique (40 juvenile OCD lesions) [1, 18, 27] and two used a transarticular technique (37 juvenile OCD lesions) [4, 25] (Table 2). Studies using a retroarticular technique reported a total of two poor outcomes and one failure. The two studies using a transarticular technique reported one poor result. Lysholm scores were used to evaluate outcomes for JOCD lesions in two studies using retroarticular techniques (35 lesions) [1, 18] and one study using a transarticular technique (30 lesions) [19]. All three studies reported high final Lysholm scores.
Table 2.
Treatment
| Study | Preoperative | Operation | Postoperative | |||
|---|---|---|---|---|---|---|
| Duration of conservative treatment (months)* | Approach | Diameter of drill or wire (mm) | Number of lesion perforations | Radiographic guidance | Weightbearing status | |
| Lee and Mercurio [22] | NR | Retroarticular | NR | 1 | Yes | NWB, duration NR |
| Bradley and Dandy [5] | 6 | Transarticular | 1.5 | ≥ 6 | No | WBAT Day 1 |
| Aglietti et al. [2] | 16 (6–48) | Transarticular | 2.0 | 1 | No | Protected WB 1 months |
| Anderson et al. [4] | > 3 | Transarticular | 0.62 | Multiple | Yes | Touch WB 6 weeks |
| Kocher et al. [19] | 6 | Transarticular | 1.6 | 6–10 | No | NWB 1 months |
| Louisia et al. [25] | 22 (12–36) | Transarticular | 1.5 or 2.0 | 4–6 | Yes | NWB 2 months |
| Kawasaki et al. [18] | 6 (3–8) | Retroarticular | 1.5 | > 3 | Yes | NWB 1 week |
| Donaldson and Wojtys [9] | NR | Retroarticular | < 1.0 | 4–8 | Yes | Touch WB 6 weeks |
| Adachi et al. [1] | > 6 | Retroarticular | 1.2 | 5–10 | Yes | NWB for 1 week |
| Edmonds et al. [10] | 6 | Retroarticular | 1.5 or 2.0 | 15–20 | Yes | Touch WB 6 weeks |
| Ojala et al. [27] | > 6 | Retroarticular | 3.0 | 1–3 | Yes (MRI) | Protected WB, duration NR |
* Values expressed as means with ranges in parentheses; NR = not reported; NWB = nonweightbearing.
We found no major differences in rates of radiographic healing for JOCD lesions drilled by retroarticular or transarticular techniques with respective healing rates of 86% and 91% (Table 4). One study used MRI in isolation to evaluate lesion healing and was therefore not included in this analysis [27].
Table 4.
Radiographic healing of juvenile osteochondritis dissecans lesions after retroarticular and transarticular drilling
| Parameter | Retroarticular drilling studies [1, 9, 10, 18, 22]* | Transarticular drilling studies [2, 4, 5, 19, 25]* |
|---|---|---|
| Number of lesions at followup | 111 | 94 |
| Duration of followup (months)† | 30.3 (7.0–36.3) | 65.0 (24–141) |
| Average age at surgery (years)† | 12.8 (12.0–13.4) | 13.2 (12.0–14.8) |
| Lesion locations | ||
| MFC (%) | 70 (63.1) | 89 (94.7) |
| LFC (%) | 41 (36.9) | 5 (5.3) |
| Lesions healed on radiographs (%) | 86 | 91 |
* Analysis restricted to studies reporting on specific outcome data for juvenile osteochondritis dissecans lesions; †values are a weighted average of studies reporting on juvenile osteochondritis dissecans outcomes with ranges in parentheses; MFC = medial femoral condyle; LFC = lateral femoral condyle.
An apparent difference was seen in time to healing by radiographic examination of JOCD lesions drilled by transarticular or retroarticular techniques (Table 5). Of the 11 studies using radiographs to examine for lesion healing, seven studies reported results on time to healing by radiography [1, 2, 4, 9, 10, 18, 19]. One study using a retroarticular approach was excluded from the time to healing analysis as a result of a unique interpretation of healing on radiography [10]. This article reported healing as a percentage by comparison of preoperative and postoperative studies; by this interpretation, lesions would require considerably more time to achieve 100% healing. Within the remaining six studies, JOCD lesions drilled transarticularly took an average of 4.5 months to heal compared with 5.6 months for JOCD lesions drilled retroarticularly.
Table 5.
Time to healing of juvenile osteochondritis dissecans lesions after retroarticular and transarticular drilling
| Parameter | Retroarticular drilling studies [1, 9, 18]* | Transarticular drilling studies [2, 4, 19]* |
|---|---|---|
| Number of lesions at followup | 50 | 64 |
| Duration of followup (months)† | 23.7 (16.0–32.0) | 52.0 (45.0–60.0) |
| Average age at surgery (years)† | 12.2 (12.0–12.3) | 13.1 (12.3–14.8) |
| Lesion locations | ||
| MFC (%) | 26 (52.0) | 60 (93.7) |
| LFC (%) | 24 (48.0) | 4 (6.3) |
| Time to healing on radiographs (months)† | 5.6 (4.0–8.5) | 4.5 (4.4–4.9) |
* Analysis restricted to studies reporting on specific outcome data for juvenile osteochondritis dissecans lesions; †values are a weighted average of studies reporting on juvenile osteochondritis dissecans outcomes with ranges in parentheses; MFC = medial femoral condyle; LFC = lateral femoral condyle.
There were no reports of complications from retroarticular and transarticular drilling in any of the included studies (Table 3). Of the 13 included studies, seven reported no perioperative complications and six did not report on complications.
Table 3.
Juvenile osteochondritis dissecans drilling outcomes
| Study | Patient-oriented outcomes | Complications | Number of lesions healed on radiographs | Time to healing on radiographs (months)* |
|---|---|---|---|---|
| Bradley and Dandy [5] | Pain report: 9 no pain, 2 less pain | None | 10 of 11 | NR |
| Lee and Mercurio [22] | Pain-free | NR | Healed | NR |
| Aglietti et al. [2] | All pain-free | None | 16 of 16 | 4.9 (2–8) |
| Anderson et al. [4] | IKDC: NL: 14, NN: 4, Abn: 1, severely abn: 1 Hughston: 15 excellent, 4 good, 1 poor | None | 18 of 20 healed | 4.4 (1–9) |
| Kocher et al. [19] | Lysholm: 92.8 (58–100) | NR | 30 of 30 | 4.4 (1–11) |
| Louisia et al. [25] | Hughston: 12 excellent, 2 good, 1 fair, 1 poor | NR | 12 of 17 healed | NR |
| Kawasaki et al. [18] | Lysholm: 97.6 (87–100) Hughston: 11 excellent, 4 good | NR | 15 of 15 healed | 4 (3–5) |
| Donaldson and Wojtys [9] | 11 excellent (asymptomatic, full activities), 1 fair | None | 16 of 16 | 8.5 (5–14.5) |
| Adachi et al. [1] | Lysholm: 95.8 (89–100) Hughston: 16 excellent, 1 good, 1 poor | None | 19 of 20 | 4.4 (2–8) |
| Edmonds et al. [10] | All pain-free | None | 49 of 59 | 11.8 (1.3–47.3) |
| Ojala et al. [27] | Hughston: 3 excellent, 1 good, 1 failure | None | N/A | NR |
* Values expressed as means with ranges in parentheses; NR = not reported; IKDC = International Knee Documentation Committee; NL = normal; NN = near normal; Abn = abnormal.
Discussion
Early diagnosis and successful treatment of OCD are essential in preventing the long-term sequelae of articular degeneration at a young age. Stable JOCD lesions frequently fail nonoperative treatment [6, 7, 30, 34] and are treated with surgical intervention in the form of drilling to promote osteochondral fragment revascularization and healing. Multiple case series [2, 18, 19] report high rates of healing and low morbidity using both transarticular and retroarticular drilling for stable JOCD lesions. However, no high-quality studies or systematic reviews exist to guide treating physicians to decide which drilling modality is best for their patient. We therefore asked whether retroarticular drilling for stable JOCD lesions or transarticular result in differing (1) patient-oriented outcome measures; (2) radiographic healing; (3) time to healing on radiography; and (4) complications.
There are major limitations of this review and the literature: (1) an assumption was made regarding the accuracy of assessment of OCD lesion stability in studies that did not use common classification systems or detailed descriptions of lesion appearance; (2) lesions were assumed to be of relatively equal sizes across studies because this parameter was infrequently reported by the studies included in this review. A variety of studies suggest this parameter is an important predictor of lesion healing [6, 10, 17, 30, 34, 35]; (3) notwithstanding inconsistent and nonvalidated definitions of radiographic healing of OCD lesions within the literature, this review assumed correct assessment of OCD lesion healing on radiography by study authors. Heterogeneity among authors’ diagnoses of lesion healing on radiographs was highlighted by one article [10] that uniquely reported healing as a percentage by comparison of preoperative and postoperative radiographs; (4) time to healing on radiographs is in turn influenced by each study’s definition of radiographic healing and dependent on varying postoperative followup schedules; (5) there was considerable heterogeneity in the type of patient-oriented outcome used across the studies resulting in restriction to qualitative analysis of outcomes; (6) analysis was further limited by multiple studies using nonvalidated patient-oriented outcome measures for juveniles/adolescents; and (7) the short-term clinical outcomes reported by this review would conceivably miss long-term complications, most notably articular cartilage changes after multiple transarticular drill sites. Interestingly, a transarticular study included in this review [5] reported slight drill site depression and fibrillation after a second-look arthroscopy 5 years after the index procedure. Nevertheless, the long-term effect of transarticular drilling remains unquantified.
Given the single cohorts of the included studies, there is a particularly high risk of referral or selection bias in the included studies. Additionally, there is a substantial risk of overestimated treatment effect through measurement bias in the studies. This systematic error would conceivably occur through an expectation of treatment effect by the investigators and potentially more favorable patient responses. Risk of measurement bias is further enhanced by possible inaccuracies in the assessment of healing with radiographs [14, 31].
Comparable patient-oriented outcome measures were found in studies using either drilling modality. Recognizing the limitations of qualitative analysis of patient-oriented outcomes from the included studies, it is apparent that neither drilling modality demonstrated clearly superior patient-oriented outcomes. This may serve to reassure the treating surgeon of relatively equal short-term symptomatic and functional improvement regardless of drilling modality used.
Using nonstandardized radiographic assessment, neither drilling modality demonstrated clearly superior rates of radiographic healing. Included retroarticular and transarticular studies demonstrated an average healing rate of 86% and 91% healing, respectively. Importantly, this suggests a favorable long-term prognosis and suggests no clear advantage of either drilling modality in the prevention of the sequelae of osteoarthritis from a nonhealing JOCD lesion.
Neither drilling modality demonstrated superiority over the other with regard to time to radiographic healing. Average time to healing was 5.6 and 4.5 months for retroarticular and transarticular drilling, respectively. Both modalities appear to offer patients relatively equal opportunity to return to activity in a relatively short period of time and avoid the effects of prolonged immobilization or activity restrictions.
No complications were reported in any other included studies of this review. The low short-term morbidity of retroarticular and transarticular drilling found in this study is consistent with current opinions regarding the safety of these techniques in the literature. This lends further credence to the current standard of care for the management of stable JOCD lesions [8].
True comparative patient-oriented outcomes and rates of radiographic healing between transarticular and retroarticular drilling for JOCD lesions remain unanswered. These questions are most ideally evaluated by high-quality prospective comparative trials, which clearly distinguish between JOCD and AOCD lesions.
Comparative studies of transarticular and retroarticular drilling require reproducible reference standards for defining OCD lesion healing by radiographs or MRI. Studies on inter- and intraobserver reliability should be performed on specific radiographic criteria for the evaluation of lesion healing. This first step would be essential before further evaluation of a nonoperative or operative treatment effect.
Additionally, future comparative studies must address patient-oriented outcomes and radiographic healing rates after nonoperative treatment. This has been inadequately addressed through retrospective studies [6, 16, 23, 30, 32, 35]. Evaluation of specific nonoperative treatment protocols through high-quality clinical trials would provide context and a benchmark for comparison to drilling techniques.
Further OCD drilling studies require standardization of nomenclature and patient-oriented outcomes to enhance comparability. This review has used the terms transarticular and retroarticular to distinguish the two general drilling techniques on the basis of articular cartilage involvement. This is in contrast to myriad of potentially confusing terms used in the existing literature such as retrograde or antegrade. Additionally, standardized measurement of patient-oriented outcomes with an instrument that is reliable, validated, and responsive [36] would further enhance the quality of future trials. The pedi-IKDC form is modified from the IKDC and is reportedly reliable, valid, and responsive in pediatric populations with knee disorders [20].
Available evidence from 11 studies suggested a high rate of healing on radiography and comparable times to healing on radiographs for JOCD lesions drilled either retroarticularly or transarticularly. Further studies are required to clearly define radiographic healing of a OCD lesion and the efficacy of nonoperative treatment. Future investigations should aim to use standardized nomenclature and validated patient-oriented outcome measures.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at the University of Toronto, Toronto, Ontario, Canada; and the University of Pennsylvania School of Medicine, Philadelphia, PA, USA.
References
- 1.Adachi N, Deie M, Nakamae A, Ishikawa M, Motoyama M, Ochi M. Functional and radiographic outcome of stable juvenile osteochondritis dissecans of the knee treated with retroarticular drilling without bone grafting. Arthroscopy. 2009;25:145–152. doi: 10.1016/j.arthro.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Aglietti P, Buzzi R, Bassi P, Fioriti M. Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy. 1994;10:286–291. doi: 10.1016/S0749-8063(05)80113-6. [DOI] [PubMed] [Google Scholar]
- 3.Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg Br. 1971;53:440–447. [PubMed] [Google Scholar]
- 4.Anderson A, Richards D, Pagnani M, Hovis D. Antegrade drilling for osteochondritis dissecans of the knee. Arthroscopy. 1997;13:319–324. doi: 10.1016/S0749-8063(97)90028-1. [DOI] [PubMed] [Google Scholar]
- 5.Bradley J, Dandy D. Results of drilling osteochondritis dissecans before skeletal maturity. J Bone Joint Surg Br. 1989;71:642–644. doi: 10.1302/0301-620X.71B4.2768313. [DOI] [PubMed] [Google Scholar]
- 6.Cahill BR, Phillips MR, Navarro R. The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy: a prospective study. Am J Sports Med. 1989;17:601–606. doi: 10.1177/036354658901700502. [DOI] [PubMed] [Google Scholar]
- 7.Cepero S, Ullot R, Sastre S. Osteochondritis of the femoral condyles in children and adolescents: our experience over the last 28 years. J Pediatr Orthop B. 2005;14:24–29. doi: 10.1097/01202412-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Chambers HG, Shea KG, Anderson AF, Brunelle TJ, Carey JL, Ganley TJ, Paterno MV, Weiss JM, Sanders JO, Watters WC, 3rd, Goldberg MJ, Keith MW, Turkelson CM, Wies JL, Raymond L, Boyer KM, Hitchock K, Anderson S, Sluka P, Boone C, Patel N. American Academy of Orthopedic Surgeons. Diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg. 2011;19:297–306. doi: 10.5435/00124635-201105000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Donaldson L, Wojtys E. Extraarticular drilling for stable osteochondritis dissecans in the skeletally immature knee. J Pediatr Orthop. 2008;28:831–835. doi: 10.1097/BPO.0b013e31818ee248. [DOI] [PubMed] [Google Scholar]
- 10.Edmonds E, Albright J, Bastrom T, Chambers H. Outcomes of extra-articular, intra-epiphyseal drilling for osteochondritis dissecans of the knee. J Pediatr Orthop. 2010;30:870–878. doi: 10.1097/BPO.0b013e3181f5a216. [DOI] [PubMed] [Google Scholar]
- 11.Flynn JM, Kocher MS, Ganley TJ. Osteochondritis dissecans of the knee. J Pediatr Orthop. 2004;24:434–443. doi: 10.1097/01241398-200407000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Guhl J. Arthroscopic treatment of osteochondritis dissecans: a preliminary report. Orthop Clin North Am. 1979;10:671–683. [PubMed] [Google Scholar]
- 13.Guhl J. Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res. 1982;167:65–74. [PubMed] [Google Scholar]
- 14.Hartman JM, Forsen JW, Jr, Wallace MS, Neely JG. Tutorials in clinical research: part IV: recognizing and controlling bias. Laryngoscope. 2002;112:23–31. doi: 10.1097/00005537-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Hayan R, Phillipe G, Ludovic S, Claude K, Jean-Michel C. Juvenile osteochondritis of femoral condyles: treatment with transchondral drilling. Analysis of 40 cases. J Child Orthop. 2009 Dec 18 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 16.Hefti F, Berguiristain J, Krauspe R, Möller-Madsen B, Riccio V, Tschauner C, Wetzel R, Zeller R. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231–245. [PubMed] [Google Scholar]
- 17.Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984;66:1340–1348. [PubMed] [Google Scholar]
- 18.Kawasaki K, Uchio Y, Adachi N, Iwasa J, Ochi M. Drilling from the intercondylar area for treatment of osteochondritis dissecans of the knee joint. Knee. 2003;10:257–263. doi: 10.1016/S0968-0160(02)00104-7. [DOI] [PubMed] [Google Scholar]
- 19.Kocher M, Micheli L, Yaniv M, Zurakowski D, Ames A, Adrignolo A. Functional and Radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med. 2001;29:562–566. doi: 10.1177/03635465010290050701. [DOI] [PubMed] [Google Scholar]
- 20.Kocher MS, Smith JT, Iversen MD, Brustowicz K, Ogunwole O, Andersen J, Yoo WJ, McFeely ED, Anderson AF, Zurakowski D. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39:933–939. doi: 10.1177/0363546510383002. [DOI] [PubMed] [Google Scholar]
- 21.Konig F. [Regarding free bodies in joints] [in German]. Dtsch Z Chir. 1887–1888;27:90–109.
- 22.Lee C, Mercurio C. Operative treatment of osteochondritis dissecans in situ by retrograde drilling and cancellous bone graft: a preliminary report. Clin Orthop Relat Res. 1981;158:129–136. [PubMed] [Google Scholar]
- 23.Linden B. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1977;59:769–776. [PubMed] [Google Scholar]
- 24.Lindholm TS, Osterman K. Treatment of juvenile osteochondritis dissecans in the knee. Acta Orthop Belg. 1979;45:633–640. [PubMed] [Google Scholar]
- 25.Louisia S, Beaufils P, Katabi M, Robert H. Transchondral drilling for osteochondritis dissecans of the medial condyle of the knee. Knee Surg Sports Traumatol Arthrosc. 2003;11:33–39. doi: 10.1007/s00167-002-0320-0. [DOI] [PubMed] [Google Scholar]
- 26.Mitsuoka T, Shino K, Hamada M, Horibe S. Osteochondritis dissecans of the lateral femoral condyle of the knee joint. Arthroscopy. 1999;15:20–26. doi: 10.1053/ar.1999.v15.015002. [DOI] [PubMed] [Google Scholar]
- 27.Ojala R, Kerimaa P, Lakovaara M, Hyvönen P, Lehenkari P, Tervonen O, Blanco-Segueiros R. MRI-guided percutaneous retrograde drilling of osteochondritis dissecans of the knee. Skeletal Radiol. 2011;40:765–770. doi: 10.1007/s00256-011-1118-2. [DOI] [PubMed] [Google Scholar]
- 28.Paget J. On the production of some of the loose bodies and joints. St Bartholomew’s Hosp Rep. 1870;6:1–4. [Google Scholar]
- 29.Pascual-Garrido C, Friel NA, Kirk SS, McNickle AG, Bach BR, Jr, Bush-Joseph CA, Verma NN, Cole BJ. Midterm results of surgical treatment for adult osteochondritis dissecans of the knee. Am J Sports Med. 2009;37(Suppl 1):125S–130S. doi: 10.1177/0363546509350833. [DOI] [PubMed] [Google Scholar]
- 30.Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM. Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop. 2003;23:102–108. [PubMed] [Google Scholar]
- 31.Sackett DL. Bias in analytic research. J Chronic Dis. 1979;32:51–63. doi: 10.1016/0021-9681(79)90012-2. [DOI] [PubMed] [Google Scholar]
- 32.Sales de Gauzy J, Mansat C, Darodes PH, Cahuzac JP. Natural course of osteochondritis dissecans in children. J Pediatr Orthop B. 1999;8:26–28. [PubMed] [Google Scholar]
- 33.Smillie I. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39:248–260. doi: 10.1302/0301-620X.39B2.248. [DOI] [PubMed] [Google Scholar]
- 34.Wall E, Von Stein D. Juvenile osteochondritis dissecans. Orthop Clin North Am. 2003;34:341–353. doi: 10.1016/S0030-5898(03)00038-5. [DOI] [PubMed] [Google Scholar]
- 35.Wall EJ, Vourazeris J, Myer GD, Emery KH, Divine JG, Nick TG, Hewett TE. The healing potential of stable juvenile osteochondritis dissecans knee lesions. J Bone Joint Surg Am. 2008;90:2655–2664. doi: 10.2106/JBJS.G.01103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17:31–39. doi: 10.5435/00124635-200901000-00005. [DOI] [PubMed] [Google Scholar]