Abstract
Objective
To investigate the determinants of specialty choice among graduating medical students in Spain, a country that entered into a severe, ongoing economic crisis in 2008.
Setting
Since 2008, the percentage of Spanish medical school graduates electing Family and Community Medicine (FCM) has experienced a reversal after more than a decade of decline.
Design
A nationwide cross-sectional survey conducted online in April 2011.
Participants
We invited all students in their final year before graduation from each of Spain's 27 public and private medical schools to participate.
Main outcome measures
Respondents’ preferred specialty in relation to their perceptions of: (1) the probability of obtaining employment; (2) lifestyle and work hours; (3) recognition by patients; (4) prestige among colleagues; (5) opportunity for professional development; (6) annual remuneration and (7) the proportion of the physician's compensation from private practice.
Results
978 medical students (25% of the nationwide population of students in their final year) participated. Perceived job availability had the largest impact on specialty preference. Each 10% increment in the probability of obtaining employment increased the odds of preferring a specialty by 33.7% (95% CI 27.2% to 40.5%). Job availability was four times as important as compensation from private practice in determining specialty choice (95% CI 1.7 to 6.8). We observed considerable heterogeneity in the influence of lifestyle and work hours, with students who preferred such specialties as Cardiovascular Surgery and Obstetrics and Gynaecology valuing longer rather than shorter workdays.
Conclusions
In the midst of an ongoing economic crisis, job availability has assumed critical importance as a determinant of specialty preference among Spanish medical students. In view of the shortage of practitioners of FCM, public policies that take advantage of the enhanced perceived job availability of FCM may help steer medical school graduates into this specialty.
Keywords: Medical Education & Training, Primary Care
Article summary.
Article focus
Ours is the first comprehensive study of the determinants of physician specialty choice in Spain, a country whose healthcare system is dominated by the public sector.
Since 2008, when Spain entered into a severe, ongoing economic crisis, the percentage of Spanish medical school graduates electing Family and Community Medicine (FCM) has experienced a reversal after more than a decade of decline.
In an April 2011 nationwide cross-sectional survey of graduating students from all Spanish medical schools, we focused on the likelihood of obtaining employment as a determinant of physician specialty choice.
Key messages
We find that job availability has assumed a key role in determining specialty choice.
We confirm the importance of factors such as prestige, opportunity for professional development and private sector remuneration.
In contrast to prior studies, we find wide variation in the importance that Spanish medical students attach to a controllable lifestyle and reduced work hours.
Strengths and limitations of this study
In the present study, we use online survey methods to achieve wide coverage of all 27 of Spain's medical schools at the expense of a reduced response rate. Moreover, we do not report longitudinal follow-up data on our respondents’ specialty preferences over time.
Our findings suggest policy levers that may take advantage of the high level of perceived job security of FCM and thus increase the flow of medical school graduates into the field.
Introduction
During the past two decades, researchers have carried out numerous studies of the determinants of specialty choice.1–37 While most have been conducted in the USA,1–13 16 18 19 22 24 25 others have addressed the determinants of specialisation in Canada,14 17 21 23 32 Australia,15 35 the UK,20 26 30 34 Ireland,29 France,27 36 Finland,31 Germany,33 Spain37 and Japan.28 In view of growing concerns about a shortage of generalists, many studies have focused on the decision to seek a career in primary care,2 4–6 18 25 family medicine,14 32 general practice,15 20 33 35 internal medicine,22 24 paediatrics30 and general surgery.9 13 16 19 23 29 34
An extensive list of factors influencing specialty choice has been considered, including: financial remuneration,1–6 8–15 17 19 24 35 lifestyle and work hours,1 2 4–16 19 21–24 29 33 35–37 prestige among colleagues or the general public,1–5 9 10 13–15 19 25 37 mentors and other role models,1 5 7 15 16 18 19 21 23 31 34 36 the length of the residency training programme,1 3 5 12 13 15 16 32 the clinical clerkship experience in medical school,1 5 13 15 16 19 21 22 25 30 direct patient interaction and continuity of care,2–4 9 10 13 24 27 32 33 35 debt upon graduation,5 6 8 13 15 16 22 25 research and teaching opportunities,2 5 10 14 15 35 potential for career advancement,13 15 29 31 influence of parents, relatives and peers,4 5 15 32 malpractice litigation risk,8 9 15 opportunity to perform procedures or work with new technology,2 5 15 21 23 intellectual challenge7 9 and hospital versus ambulatory orientation.2 23 Gender differences in the importance of these factors have also been studied.8 19–21 27–29
In 2011, we conducted a cross-sectional survey of Spanish medical students in their final year before electing a specialty training programme. In view of the severe, ongoing economic crisis that began in late 2008, we studied whether the likelihood of obtaining employment had assumed a key role in determining specialty preference.
Spain's healthcare system and the financial crisis
The Spanish healthcare system is dominated by the public sector. In 2009, total healthcare expenditures constituted 9.5% of gross domestic product (GDP), of which only 2.5% was privately financed. The vast majority of physicians are employees of the public sector, where salaries are fixed by separate negotiations between unions of healthcare workers and the governments of each of Spain's 17 autonomous communities. Physicians in many specialties have opportunities to earn additional income in the private sector, either by treating paying patients in their own private practices or by performing consults on inpatients while on call at private hospitals. However, there is essentially no such demand for specialists in Family and Community Medicine (FCM), who work almost exclusively as full-time employees of health centres.
Medical specialisation in Spain is governed by a system widely known as MIR, which stands for Médico Interno Residente, literally ‘resident medical intern’.38 39 On an annual basis, the central government's Ministry of Health authorises postgraduate training programmes in 47 different specialties, imposing limits on the number of positions (plazas) in each programme. Each medical school graduate (candidato) seeking a training position is ranked on the basis of his academic transcript and his score on the annual nationwide MIR examination. In a sequential process, the top-ranked applicant first chooses from all available training programmes, after which each successively ranked candidate is permitted to choose from the remaining available training slots. In the 2011 MIR cycle, for example, the Ministry of Health authorised 6881 positions in 560 training centres throughout the country.40 A total of 6873 applicants accepted training positions through the sequential selection process.
Unemployment among graduates of Spanish medical schools was a relatively rare phenomenon until the financial crisis erupted in late 2008. With real GDP in decline, the nationwide unemployment exceeding 10% and heading towards 20% and interest rates on Spanish sovereign debt approaching record highs, the federal and regional governments began to engage in increasingly severe budgetary cutbacks. The healthcare sector was not immune from these budgetary cuts. While established physicians with seniority had essentially lifetime government jobs, many younger graduates were compelled to accept contingent employment contracts. Still others could not find work at all. By February 2010, the number of out-of-work physicians nationwide had for the first time crossed the psychological threshold of 1000.41 In the spring of 2011, when the survey described in this report was in the field, there were prominent headlines about personnel cuts in the health budgets of many autonomous communities, notably Catalonia.42 By April 2012, with increasing austerity measures, the number of unemployed physicians had broken the 2000 barrier.43
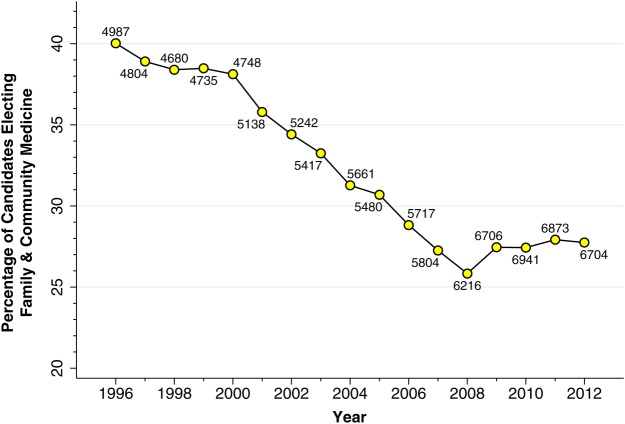
There is presumptive evidence that the financial crisis has had a significant effect on the career choices of recent medical school graduates. As figure 1 indicates, the percentage of candidates participating in the annual MIR selection process who elected a training position in FCM underwent an abrupt reversal after 2008. For the past 3 years (2010–2012), the number of candidates electing FCM has been limited by the number of available training positions, whereas during 2006–2009, some training positions in FCM remained unfilled.
Figure 1.
Percentage of candidates participating in the Annual Internship-Residency (MIR) Selection Process who elected training position in Family and Community Medicine, 1996–2012. Adjacent to each point is the total number of candidates participating in the MIR selection process in the corresponding year. Source: Compiled from annual data provided by the Ministerio de Sanidad y Política Social, Subdirección General de Ordenación Profesional, Spain. MIR, Médico Interno Residente.
Subjects and methods
Cross-sectional survey
In April 2011, with the assistance of professors, deans and student associations, we invited all students in their final year in each of the 27 medical schools of Spain to participate in a survey of career preferences. Students were not contacted individually. Instead, posters advertising the survey and directing students to the survey website were posted on every medical school campus. Participants were eligible to win a lottery prize. Participation in the survey was voluntary, and anonymity was assured. With the exception of students at the University of Las Palmas de Gran Canaria, who took the electronic survey as a classroom-based pilot, all respondents completed the survey online.
Survey questionnaire
The electronic survey questionnaire contained three blocks: (1) personal data (age, sex, nationality, residential postal code, university, anticipated date of graduation and how many parents or grandparents were physicians); (2) questions eliciting preferences among the 47 specialties in Spain's MIR system of postgraduate training and (3) questions eliciting perceptions and expectations concerning these specialties.
In the second block, in particular, each student was first asked to designate his preferred specialty, that is, which specialty he would choose in the annual MIR selection process if he faced no restrictions as a result of his academic performance or his score on the nationwide examination. Each student was then asked to designate his favorite specialty, that is, which specialty he enjoyed the most, without regard to remuneration or working conditions (Sin tener en cuenta los aspectos económicos, condiciones laborales, etc., ¿cuál es la especialidad que más te gusta?).
In the third block, each student was presented with seven questions concerning each specialty within a limited menu of six specialties. The menu included the preferred specialty he had just chosen in the second block, the specialty of FCM, and four other specialties chosen at random from four balanced subsets. Each subset contained medical, surgical and diagnostic specialties, with one specialty in each quartile of the global ranking of specialties observed in the MIR 2010 selection cycle.38
The seven questions, whose translated text appears in table 1, addressed the following attributes of each specialty: (1) the probability of obtaining employment; (2) lifestyle and work hours; (3) recognition by patients; (4) prestige among colleagues; (5) opportunity for professional development; (6) annual remuneration for a physician with 10–15 years experience and (7) the proportion of the physician's compensation from private practice. Four of the attributes (2, 3, 4 and 5) were measured on a 10-point scale, while two (1 and 7) were gauged on a percentage scale from 0 to 100. The remaining attribute (6) was measured in thousands of euros. We chose these seven attributes based upon our review of the literature and our discussions with experts knowledgeable about Spanish healthcare institutions. Inclusion of the first attribute, in particular, was motivated by our hypothesis that the ongoing economic crisis and widely publicised budgetary cuts in the health sector had influenced students’ perceptions about the likelihood of employment.
Table 1.
Seven survey questions on attributes of medical specialties*
| Attribute and survey text | FCM Mean SD |
All others Mean SD |
|---|---|---|
| 1. Probability of obtaining employment. ‘How would you rate the probability of obtaining work in the next three years, whether in the public or private sector, for an individual who became certified in this specialty today? (0 to 100 percent)’ | 83.98 19.89 |
64.78 23.92 |
| 2. Lifestyle and work hours. ‘Work hours, working conditions, and the ability to reconcile work with family life. (0 to 10, 0=very bad, 10=very good)’ | 7.78 2.09 |
6.78 2.25 |
| 3. Recognition by patients. ‘Recognition of professional work on the part of patients. (0 to 10)’ | 5.92 2.60 |
6.34 2.73 |
| 4. Prestige among colleagues. ‘Prestige and recognition among colleagues as well as social recognition. (0 to 10)’ | 3.92 2.28 |
6.30 2.52 |
| 5. Opportunity for professional development. ‘Possibility of promotion or future professional development within the specialty (new fields, new techniques, scientific advances). (0 to 10)’ | 5.11 2.30 |
7.20 2.15 |
| 6. Annual remuneration with 10–15 years’ experience. ‘Estimate the current average annual gross remuneration (public and private combined) of a specialist with 10–15 years of experience. (Thousands of euros)’† | 60.00 0.16 |
86.56 31.96 |
| 7. Proportion of compensation from private practice. ‘What percentage of this remuneration (including public and private) do you believe comes from private practice? (0 to 100 percent)’† | 0.00 0.00 |
39.32 23.40 |
*The introductory text was, ‘In this section, you'll define your profile of some medical specialties, including the one that you've just chosen as your first choice as well as others chosen at random. Think about your perceptions and expectations concerning each specialty.’
†The preamble to the two questions on attributes 6 and 7 was: ‘The following questions are about compensation. To facilitate your responses, recall that the average annual gross income of a full-time specialist in Family & Community Medicine with 10–15 years of experience is currently about 60 000 euros.’
FCM, Family and Community Medicine.
Statistical methods
We employed the mixed multinomial logit model44 to assess the influence of each of the seven attributes on students’ choice of preferred specialty. The mixed multinomial logit model differs from the standard multinomial logit model in that the coefficients of each predictor variable may vary randomly in the population. In the context of discrete choice modelling, the mixed multinomial logit model captures the potential heterogeneity of individual preferences. For example, in the case of attribute 2, the mixed model admits the possibility that some students prefer a specialty with reduced work hours and a comfortable lifestyle, while others prefer a specialty with long work hours and little leisure time.
In our application of the mixed multinomial logit model, the observations corresponded to the six specialties within the menus evaluated by each of the student respondents. For each student, the dependent variable was a binary indicator equal to 1 for the preferred specialty and 0 for the remaining five specialties in the student's menu. The independent variables were each student's valuations of the seven attributes. In addition, we included interaction terms between each of the seven attributes and each personal characteristic in order to test whether the coefficients of the attributes differed by sex, age, university, expected graduation date or the presence of physicians in the family. We also tested interactions between each attribute and a binary variable indicating concordance between the student's preferred and favourite specialty.
Adhering to the mixed logit specification, we further assumed that the coefficients of each attribute were normally distributed in the population with an unknown mean and SD. To assess whether there was significant heterogeneity in the coefficients of each attribute, apart from those differences attributable to the foregoing observed personal characteristics, we tested the null hypothesis that the estimated SD of each coefficient's population distribution was equal to zero. We employed the χ2 test based on the log likelihood ratio to assess the overall model goodness of fit.
To estimate our mixed multinomial logit model, we relied on the mixlogit routine in the Stata V.11 statistical software.45 Each raw coefficient outputted by this routine corresponds to the effect of a unit change in each attribute on the logarithm of the odds of preferring a specialty. Each raw coefficient can also be interpreted as the contribution of a unit change in each attribute to the ‘utility’ of the specialty. In the tabulated results below, we report the exponentiated values of the raw coefficients, that is, the effect of a unit change on the odds of specialty preference. However, we used the raw coefficients to assess the quantitative trade-offs between attributes. For example, to estimate the percentage increase in the proportion of the physician's compensation from private practice (attribute 7) that would yield the same utility as a 1% increase in the probability of obtaining employment (attribute 1), we computed the ratio of the raw coefficient of attribute 1 to the raw coefficient of attribute 7.
Finally, to assess the external validity of our mixed multinomial logit model, we compared its predictions of specialty choice with the global ranking of specialties observed among the same nationwide cohort of medical graduates in the 2012 MIR selection process. We chose the 2012 MIR cycle for comparison because the students responding to our April 2011 survey subsequently graduated from medical school in June 2011, then studied for and took the MIR examination in January 2012, and then made their specialty selections during March of that year. Specifically, for each specialty within each student's menu, we computed the predicted probability that the student would prefer that specialty. For each specialty, we then compared its median predicted probability, as derived from our model, with its median ranking among all candidates who elected a specialty in the 2012 MIR cycle.
Results
Survey response
Out of a total population of 3874 registered sixth-year medical students nationwide, we received 978 responses (or 25%). These responses included students from each of Spain's 27 medical schools. While the response rate varied among medical schools, there were no significant differences in the gender or age composition of the respondents and the entire nationwide population (survey respondents: 71% women, mean age 24.1 years; nationwide population of sixth-year students: 71% women, mean age 24.7 years).
Descriptive statistics
Among the 978 medical students responding to the survey, 892 (91.2%) designated a preferred specialty, of whom 836 (93.7%) also designated a favourite specialty. For each of the seven questions, table 1 shows the corresponding sample means and SDs of students’ responses for FCM and for all remaining specialties combined. For all seven attributes, the differences in the mean ratings between FCM and other specialties combined were statistically significant (p<0.001).
Predictors of specialty preference
Table 2 gives the principal results of our regression analyses. Model 1 represents the standard multinomial logit regression, in which all attribute coefficients are fixed, while models 2 through 4 represent mixed multinomial logit regressions. In model 2, in particular, the coefficient of attribute 2 (lifestyle and work hours) is permitted to vary within the population. In model 3, interaction terms with attribute 6 (annual remuneration with 10–15 years’ experience) are included as explanatory variables. In model 4, attribute 6 and its interactions are removed altogether. We omit the results of other models where we found insignificant interactions between each attribute and sex, age, university, expected graduation date, the presence of physicians in the family, as well as a binary variable indicating concordance between the student's preferred and favourite specialty.
Table 2.
Mixed multinomial logit regression results*
| Explanatory variable | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| 1. Probability of obtaining employment† | 1.324 (1.263 to 1.388) | 1.346 (1.278 to 1.418) | 1.339 (1.271 to 1.412) | 1.337 (1.272 to 1.405) |
| 2. Lifestyle and work hours | 0.905 (0.867 to 0.944) | 0.901 (0.852 to 0.952) | 0.891 (0.843 to 0.943) | 0.907 (0.860 to 0.957) |
| Population SD | 0.288 (0.161 to 0.415) | 0.282 (0.155 to 0.409) | 0.301 (0.182 to 0.419) | |
| 3. Recognition by patients | 1.105 (1.055 to 1.157) | 1.118 (1.064 to 1.176) | 1.116 (1.061 to 1.173) | 1.098 (1.047 to 1.151) |
| 4. Prestige among colleagues | 1.082 (1.024 to 1.143) | 1.096 (1.033 to 1.163) | 1.110 (1.046 to 1.179) | 1.062 (1.005 to 1.121) |
| 5. Opportunity for professional development | 1.326 (1.254 to 1.403) | 1.347 (1.267 to 1.432) | 1.347 (1.265 to 1.433) | 1.303 (1.229 to 1.381) |
| 6. Annual remuneration with 10–15 years’ experience‡ | 0.821 (0.782 to 0.863) | 0.812 (0.770 to 0.856) | 1.062 (0.701 to 1.610) | |
| Interaction: female gender | 0.884 (0.817 to 0.957) | |||
| Interaction: concordance with favourite specialty§ | 0.885 (0.815 to 0.962) | |||
| Interaction: age (years) | 0.995 (0.978 to 1.012) | |||
| 7. Proportion of compensation from private practice† | 1.195 (1.139 to 1.255) | 1.210 (1.148 to 1.276) | 1.218 (1.154 to 1.285) | 1.071 (1.028 to 1.116) |
| Number of respondents¶ | 836 | 836 | 818 | 887 |
| Number of observations** | 4839 | 4839 | 4738 | 5184 |
*The coefficients represent the effect of a unit change in the independent variable on the odds of preferring a specialty. Numbers in brackets below each coefficient are 95% CI.
†Attribute values normalised to range from 0 to 10, so that each unit corresponds to 10%.
‡Attribute values normalised so that each unit corresponds to €10 000.
§Binary variable equal to 1 when the student's preferred specialty is also his favourite specialty.
¶Number of students with data on all explanatory variables in the model.
**Number of specialty choices with data on all explanatory variables in the model.
In all model specifications in table 2, attribute 1 (the probability of obtaining employment) significantly influenced specialty preference. In model 4, for example, each 10% increment in the probability of obtaining employment increased the odds of preferring a specialty by 33.7% (95% CI 27.2% to 40.5%). The magnitude of the effect was comparable to that of attribute 5 (professional development, including the possibility of promotion). Attributes 3 (recognition by patients) and 4 (prestige among colleagues) had smaller but significantly positive influences on specialty choice. For both attributes, a 1-point increment on a 10-point scale increased the odds of preferring a specialty by approximately 10–11%. The findings of model 4 were not significantly altered when we included an interaction term for students at the University of Las Palmas de Gran Canaria, who took the electronic survey as a classroom-based pilot (results not shown).
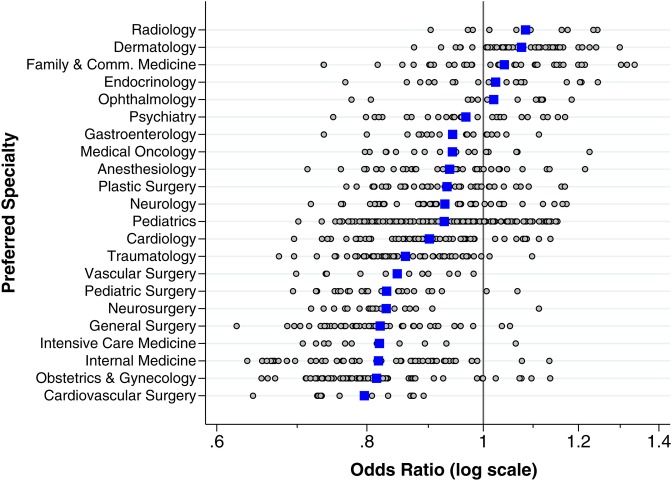
Heterogeneity of preferences for lifestyle and work hours
Although attribute 2 (lifestyle and work hours) appeared to have a significant negative influence on specialty choice, our mixed multinomial logit models 2–4 revealed considerable population heterogeneity in this effect. In model 4, for example, the population average effect was 0.907, with a 1-SD range from 0.606 to 1.208 (ie, 0.907±0.301). Equivalently, a 1-point increment on a 10-point scale reduced the odds of preferring a specialty on average by an estimated 9.3%. However, for 68% of the students (which corresponds to the 1-SD range for a normal distribution), the effect of a 1-point increment ranged from a 39.4% decrease to a 20.8% increase in the odds of preferring a specialty. Attribute 2 was the only explanatory variable to show significant population heterogeneity in our mixed multinomial logit regressions.
Figure 2 offers a visual representation of the population heterogeneity in the influence of lifestyle and work hours. Each open point in the figure represents one student. The points are arranged in rows corresponding to the student's preferred specialty. Among the 887 students included in model 4, a total of 231 (or 26%) had a positive predicted effect of lifestyle and work hours on specialty preference.
Figure 2.
Effect of a 1-point increment in Lifestyle and Work Hours rating on OR of preferring a specialty. We used the results of model 4 to compute the predicted effect for each individual student of a 1-point increment in attribute 2 (Lifestyle and Work Hours). Each open point in the figure represents one student. The points are arranged in rows corresponding to the student's preferred specialty. The horizontal axis gauges the predicted effect of a 1-point increment on a 10-point scale of favourable lifestyle and work hours. The solid blue squares represent the population mean effect for students in each preferred specialty. Not shown are preferred specialties with fewer than 10 respondents.
Figure 2 displays considerable heterogeneity between preferred specialties. For example, among the group of 53 students preferring dermatology, whose predicted effects are arrayed in the second row in figure 2, the average effect of a 1-point increment on a 10-point scale of favourable lifestyle and work hours was a 7.6% increase in the odds of preferring that specialty (corresponding to the solid blue square in the second row). Within this group, the predicted effect ranged from a 12.5% decrease to a 29.9% increase. For the 35 students preferring FCM, arrayed on the third row, the average effect of a 1-point increment along the scale of lifestyle and work hours was a 4.1% increase in the odds of specialty preference (corresponding to the solid blue square in the third row), with a predicted effect ranging from a 26.4% decrease to a 33.6% increase. By contrast, among the group of 73 students preferring obstetrics and gynaecology, whose predicted effects are arrayed in the next-to-last row of the figure, the average effect of a 1-point increment was an 18.5% decrease in the odds of preferring that specialty (the next-to-last solid blue square). Within this group, the predicted effect ranged from a 34.6% decrease to a 13.7% increase.
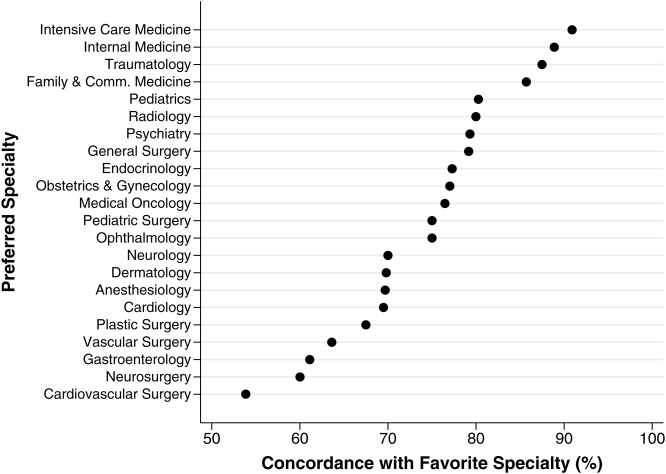
Concordance between preferred and favourite specialties
Among the 892 students who reported both a preferred and a favourite specialty, we observed a concordance between the two responses in 676 students (or 75.8%). Figure 3 shows the rate of concordance, classified by the preferred specialty. The rate of concordance ranged from a low of 53.8% among students who preferred Cardiovascular Surgery to 90.9% among those who preferred Intensive Care Medicine. The rate of concordance for FCM was 85.7%.
Figure 3.
Concordance of preference with favourite specialty. For each preferred specialty, the black points show the proportion of students who also designated that specialty as their favourite.
Opportunities for private sector remuneration
In models 1 and 2 in table 2, attribute 6 (annual remuneration with 10–15 years’ experience) had a significant negative influence on specialty preference, while attribute 7 (proportion of compensation from private practice) had a significant positive effect. To address the apparent inconsistency between the estimated effects of the two different attributes, we included interaction terms with attribute 6 in our specification of model 3. We found that the negative relation between annual remuneration and specialty preference remained statistically significant for female students and for those who reported a concordance of preferred and favourite specialty. There was no relationship between the effect of annual remuneration and a student's age.
Finally, in model 4, when we dropped attribute 6 altogether, the effect of attribute 7 remained significant and positive, but its magnitude was decreased. With annual remuneration included as an explanatory variable, each 10% increment in the proportion of compensation from private practice increased the odds of preferring a specialty by approximately 20–22%. With annual remuneration excluded, the effect of 10% increment in the proportion of compensation from private practice compensation increased the odds of specialty preference by only 7%.
Trade-off between job availability and opportunities for private sector remuneration
We focused specifically on the quantitative trade-off between job availability (attribute 1) and opportunities for private sector remuneration (attribute 7). Relying on the results of model 4, we found that the raw coefficients of attributes 1 and 7 were 0.290 (95% CI 0.241 to 0.340) and 0.069 (95% CI 0.028 to 0.110), respectively. The percentage increase in the proportion of the physician's compensation from private practice (attribute 7) that would yield the same utility as a 1% increase in the probability of obtaining employment (attribute 1) was therefore 0.290/0.069=4.2. Based on a linear approximation of the variance of the ratio of two random variables, we computed the 95% CI around this estimate as 1.7–6.8.
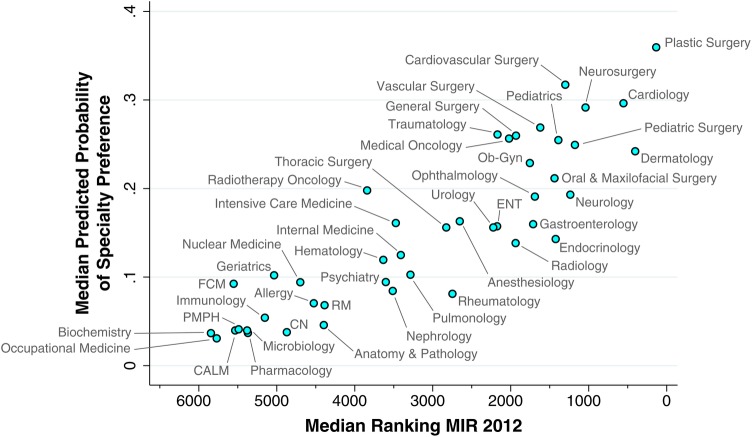
External validity: comparison with MIR 2012 global rankings
For all four models, the χ2 statistic based on the log likelihood ratio showed a significant goodness of fit (p<0.002). As a further check of internal validity, we found a close match between the observed and predicted probabilities of specialty choice when broken down by the decile of predicted probability.46
Figure 4 displays a check of external validity. For each specialty, the figure plots the median predicted probability of specialty preference against the median specialty ranking in the 2012 MIR cycle. The latter variable is plotted on a reverse scale since the most preferred specialties in the MIR selection process will have the lowest ranking numbers. Also plotted is the ordinary least squares regression line relating the two variables. The Spearman rank correlation between the two variables was −0.88 and highly significant (p<0.0001).
Figure 4.
Median predicted probability of specialty preference in relation to the median specialty ranking in the 2012 MIR selection process. CALM, Clinical Analysis & Laboratory Medicine; CN, Clinical Neurophysiology; ENT, Otorhinolaryngology; FCM, Family and Community Medicine. Ob-Gyn, Obstetrics and Gynaecology; PMPH, Preventive Medicine and Public Health; RM, Rehabilitation Medicine.
The strong correlation between the model predictions and the MIR rankings can be seen through a comparison of Cardiology at the upper right, Anaesthesiology near the centre and FCM near the bottom left. Thus, among the 6704 candidates nationwide who elected a specialty during the 2012 MIR selection process, the median ranking of those candidates choosing Cardiology was 555. (Only two specialties had a higher median ranking: Plastic Surgery at 136, and Dermatology at 404.) From a menu of six specialties offered to students participating in our survey, the median predicted probability of preferring Cardiology was 29.6%. For Anaesthesiology, by contrast, the median ranking in the 2012 MIR cycle was 2652, while the median predicted probability among survey respondents was 16.3%. For FCM, the median ranking in the 2012 MIR cycle was 5552, while the median predicted probability among survey respondents was 9.2%.
Discussion
In a cross-sectional survey of medical students in their final year before graduation, conducted in the midst of Spain's economic crisis, we found that job availability had a significant impact on specialty preference. Based on our model 4 specification, we found that each 10% increment in the probability of obtaining employment increased the odds of preferring a specialty by 33.7% (95% CI 27.2% to 40.5%). Moreover, we observed considerable variability in the effect of lifestyle and work hours on students’ specialty preferences. Among students who would elect Dermatology if there were no restrictions on specialty choice, the average effect of a 1-point increment on a 10-point scale of favourable lifestyle and work hours was a 7.6% increase in the odds of preferring that specialty. By contrast, among students preferring Obstetrics and Gynaecology, the average effect of a 1-point increment was an 18.5% decrease in the odds of preferring that specialty.
We also asked students to designate their favourite specialty, that is, the specialty that they enjoyed the most, independent of future remuneration or working conditions. The concordance between students’ preferred and favourite specialties varied considerably. Approximately 54% of students who preferred Cardiovascular Surgery also designated it as their favourite specialty. By contrast, approximately 86% of students who preferred FCM also designated it as their favourite specialty, while 91% of students who preferred Intensive Care Medicine also designated it as their favourite specialty.
Our survey included two attributes that reflected different aspects of physician compensation: the average remuneration of a physician with 10–15 years experience, and the proportion of compensation from private practice. We found that the former had an unexpectedly negative relation to specialty preference, particularly among female students and those whose favourite specialty matched their preferred specialty, while the latter had a significant positive relation to specialty preference (model 3). Eliminating the former from our regression analysis (model 4), we estimated the trade-off between job security and opportunities for private practice. An increase of approximately 4% in the proportion of the physician's compensation from private practice would yield the same utility as a 1% increase in the probability of obtaining employment.
Finally, as an external validity check, we found a high correlation between the specialty ranking predicted by our mixed multinomial logit model with the nationwide specialty ranking in the 2012 MIR selection process. In particular, the median probability that a student would select FCM out of a menu of six specialty choices was approximately 9%, while the median MIR ranking of this specialty was 5552 out of 6704 candidates.
Study limitations
Our study has a number of important limitations. To begin with, our survey sample of 978 respondents constituted only 25% of the entire nationwide population of 3874 registered students in their final year of medical school. While our sample covered all 27 of Spain's medical schools, and while we found no significant difference in gender or age composition between our sample and the entire nationwide population, the apparently low response rate raises the possibility that our conclusions cannot be generalised or are subject to non-response bias.
Open-ended online surveys generally yield much lower response rates than a direct personal invitation via postal mail accompanied by a paper questionnaire.47 In particular, surveys of specialty choice among students in a single medical school or clinical rotation have yielded high response rates ranging from 65% to 97%.4 5 7 9 13 28–30 34 37 By contrast, an Internet-based survey soliciting participation of students in 70 US medical schools received online responses from students in only 16 schools.16 An online survey covering students in all five medical schools in the federal state of Baden-Wuerttemberg in Germany yielded only 11% of eligible students.33 A recent online survey of students taking the 2011 National Grading Examination in France yielded a 24% response rate.36
Despite the low response rate, our Internet-based survey achieved wide coverage at low cost. It is at least arguable that the conclusions from our sample of 978 students from all 27 of Spain's medical schools are more generalisable than a hypothetical study of a 100% sample of 978 students from a single medical school. We do not have any evidence of significant non-response bias. Students at the University of Las Palmas de Gran Canaria, who took the survey as a classroom pilot and had a higher response rate, nonetheless placed the same valuation on job availability as those who took the survey online.
An additional limitation of our study is the lack of prior survey results for comparison. We surveyed students only once in April 2011. We have no data from a comparable cross-sectional survey carried out before the onset of Spain's economic crisis in late 2008. Our results are at least consistent with the finding from a 2009 survey in Ireland—carried out in the midst of the country's financial crisis—that medical students and junior doctors attached high importance to ‘future employment’ in specialty choice.29 A 2010 survey of all first-year through sixth-year medical students from a single Spanish medical school found that ‘quality of life’ and ‘professional prestige’ were important factors in specialty choice, but aspects of job security were not considered.37 Further confirmation of the lasting importance of job security in specialty choice will require repeat surveys once employment prospects for physicians have improved.
Nor do we report longitudinal follow-up data on the evolution of our respondents’ specialty preferences over time. There is evidence from longitudinal studies that students’ specialty preferences evolve during medical school.48 49 In a study of internal medicine residents in the USA, 62% changed the subspecialty career choice at least once during residency.50 In a longitudinal follow-up of UK medical graduates 10 years after graduation, approximately one-quarter were working in a specialty different from that chosen 3 years after graduation.26 It is notable, however, that 91.2% of students that we surveyed reported a preferred specialty, whereas in the UK, 28% of medical school graduates in the 1990s knew their preferred specialty 1 year after graduation.26 The high correlation between the specialty choice predicted by our model and specialty choices observed in the MIR 2012 cycle (figure 3) does not suggest a marked shift in preferences during the 1-year period after medical school graduation, during which prospective candidates study for the national examination and then participate in the sequential selection process.
The explanatory variables in our model (table 1) were derived from students’ perceptions and expectations, rather than objective data. It is entirely possible, for example, that students exaggerated the importance of job security (attribute 1). By April 2012, with Spain's overall unemployment rate hovering around 25%, the psychologically menacing figure of 2000 unemployed doctors51 still represented only 1% of the active physician workforce. While a few studies have correlated specialty preferences with objective data on remuneration, work hours, malpractice risk and debt upon graduation,8 12 we stress that students’ subjective perceptions and expectations are the principal determinants of specialty choice.
While a number of studies have focused on the ‘controllable lifestyle’ as an important determinant of specialty choice,1 2 4–16 19 21–24 35 our results shed new light on the heterogeneity of preferences for lifestyle and work hours. We find, in fact, that only 26% of respondents placed a positive value on reduced work hours, while 74% placed a positive value on working more (as shown by the distribution of points in figure 2). One possible explanation is that, in a healthcare system where public sector salaries are fixed by collective bargaining, taking on additional on-call assignments after regular working hours is viewed primarily as a means of increasing remuneration. In the EuroStat Labor Force Surveys, Spanish physicians reported working an average of 39 h/week,52 even though the collectively agreed-upon formal work week was 35 h.
Our failure to find a significant positive effect of annual remuneration (attribute 6) may reflect students’ inadequate knowledge of physicians’ salaries, a phenomenon that has also been observed in the USA53 It is possible that students’ estimates of remuneration were overly influenced by short-term concerns about job security, even though the underlying question was framed over a 10-year to 15-year horizon. Nationally representative data on the earnings of Spanish physicians have not been published. Students’ estimates of the annual remuneration of a non-FCM specialist were on average 44% greater than that of a practitioner of FCM (table 1), a value that falls within the range of specialist–general practitioner remuneration ratios of other OECD countries.54
In Canada, physicians’ fee-for-service payments correlate strongly with income,17 whereas in the UK, opportunities for non-National Health Service consultant work constitute an important determinant of variations in income.55 Our finding that attribute 7 was a significant predictor of specialty choice indicates that, in Spain's healthcare system where publicly financed salaries are the dominant form of physician compensation, opportunities for additional private sector employment are a more sensitive proxy for physician income. For this reason, we based our calculations of the trade-off between job security and remuneration on the results of model 4, which excludes attribute 6 entirely.
A few studies have employed a discrete choice experiment—rather than a cross-sectional survey—to assess the determinants of physicians’ choice of specialty,35 working conditions55 56 and urban versus rural practice.57 A discrete choice experiment has the advantage that each potential determinant of physician choice can be independently controlled and varied randomly. In principle, such a study design might have helped us distinguish more precisely between total remuneration (attribute 6) and opportunities for private sector employment (attribute 7). It might also have allowed us to assess more precisely the extent to which the ‘workaholics’ in our study, who preferred specialties with more working hours (attribute 2), would trade off higher income for reduced leisure time. One drawback of the discrete choice experimental design is that respondents choose between hypothetical choices constructed by the experimenter, whereas in our cross-sectional study, we directly observe the perceived attributes of the actual specialty options available to graduating medical students. While the results of discrete choice experiments can be used in simulations, our cross-sectional design thus facilitates external validation of our results (figure 4).
We asked students to report both their preferred and favourite specialties, a distinction we have not encountered in any other study. While Spanish medical students generally report a high level of concordance between the two (76%), we observed considerable variation by preferred specialty (figure 2). It is noteworthy that five of the highest ranked specialties in the 2011 MIR cycle (Cardiovascular Surgery, Neurosurgery, Plastic Surgery, Cardiology and Dermatology; see figure 4) had low levels of concordance. By contrast, the observed high levels of concordance for Internal Medicine and FCM suggest that students who prefer these specialties do so despite the low salaries, minimal opportunities for private sector remuneration or unfavourable working conditions. This conclusion is further supported by the observed negative effect of the interaction between concordance and remuneration in model 3 (table 2).
Policy implications
Increased remuneration, more favourable working conditions and enhanced prestige have routinely been proposed as incentives to lure medical students into primary care and family practice. In Spain, however, physician remuneration within the public sector is determined by decentralised collective bargaining between unions and local governments. Opportunities for practitioners of FCM to earn additional income in the private sector are scarce and even less under the control of the central government. Improvements in working conditions and enhancement of prestige are longer term solutions that will require reformulation of the nature of work of the primary care physician and the role of community health centres.38 39
Our findings, by contrast, suggest other shorter term policy levers that may take advantage of the high level of perceived job availability of FCM (table 1) and thus increase the flow of medical school graduates into the field. To the extent that the healthcare budgets of the country's 17 autonomous communities must continue to endure budgetary cuts, our results argue for sparing community health centres and the practitioners of FCM who work in them. As part of its crisis management, the Spanish central government has recently increased physicians’ legal work week from 35 to 37.5 h, a measure that has sparked more than a few protests.58 59 Ironically, this measure will cut mostly into the incomes of non-FCM specialists who earned additional income through after-hours private consultations and thus reduce the income disparity with FCM physicians.
As a separate policy instrument, the central government's Ministry of Health could cautiously expand the number of approved postgraduate training positions in FCM, which has recently become a limiting factor in the resurgence of this specialty since 2008 (figure 1). There is evidence that many residents already in training in FCM have chosen to retake the national MIR examination and re-enter the selection process as candidatos despite the requirement that they abandon their current training position.38 It is conceivable that too large an excess of unfilled training slots in FCM could aggravate this perverse incentive.
Conclusions
In the midst of an ongoing economic crisis, the likelihood of obtaining employment has assumed critical importance as a determinant of specialty preference among Spanish medical students. Public policies that take advantage of the enhanced perceived job availability of FCM may be an effective way to steer medical school graduates into this specialty.
Supplementary Material
Acknowledgments
We gratefully acknowledge the research assistance of Teresa Suárez de Sousa.
Footnotes
Contributors: All authors (JEH, BGL, VO and PB) contributed substantially to the conceptualisation and design of the survey. JEH, BGL and PB performed statistical analyses on the survey data. JEH and BGL wrote the initial drafts, while VO and PB made substantive changes to various drafts. All contributors approved the final version for publication.
Funding: The Spanish Ministry of Science and Innovation, through Grant ECO2010–21558 to BGL as the principal investigator, supported the development, execution and analysis of the survey described in this study.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The detailed results of all statistical analyses, including statistical code, are available from the corresponding author at jeffrey@mit.edu.
References
- 1.Schwartz RW, Haley JV, Williams C, et al. The controllable lifestyle factor and students’ attitudes about specialty selection. Acad Med 1990;65:207–10 [DOI] [PubMed] [Google Scholar]
- 2.Kassler WJ, Wartman SA, Silliman RA. Why medical students choose primary care careers. Acad Med 1991;66:41–3 [DOI] [PubMed] [Google Scholar]
- 3.Hurley JE. Physicians’ choices of specialty, location, and mode: a reexamination within an interdependent decision framework. J Hum Resour 1991;26:47–71 [Google Scholar]
- 4.Fincher RM, Lewis LA, Rogers LQ. Classification model that predicts medical students’ choices of primary care or non-primary care specialties. Acad Med 1992;67:324–7 [DOI] [PubMed] [Google Scholar]
- 5.Osborn EH. Factors influencing students’ choices of primary care or other specialties. Acad Med 1993;68:572–4 [DOI] [PubMed] [Google Scholar]
- 6.Rosenthal MP, Diamond JJ, Rabinowitz HK, et al. Influence of income, hours worked, and loan repayment on medical students’ decision to pursue a primary care career. JAMA 1994;271:914–17 [PubMed] [Google Scholar]
- 7.Burack JH, Irby DM, Carline JD, et al. A study of medical students’ specialty-choice pathways: trying on possible selves. Acad Med 1997;72:534–41 [DOI] [PubMed] [Google Scholar]
- 8.Thornton J. Physician choice of medical specialty: do economic incentives matter? Appl Econ 2000;32:1419–28 [Google Scholar]
- 9.Gelfand DV, Podnos YD, Wilson SE, et al. Choosing general surgery: insights into career choices of current medical students. Arch Surg 2002;137:941–5; discussion 45–7 [DOI] [PubMed] [Google Scholar]
- 10.Nicholson S. Physician specialty choice under uncertainty. J Labor Econ 2002;20:816–47 [Google Scholar]
- 11.Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA 2003;290:1173–8 [DOI] [PubMed] [Google Scholar]
- 12.Thornton J, Esposto F. How important are economic factors in choice of medical specialty? Health Econ 2003;12:67–73 [DOI] [PubMed] [Google Scholar]
- 13.Azizzadeh A, McCollum CH, Miller CC, et al. Factors influencing career choice among medical students interested in surgery. Curr Surg 2003;60:210–13 [DOI] [PubMed] [Google Scholar]
- 14.Wright B, Scott I, Woloschuk W, et al. Career choice of new medical students at three Canadian universities: family medicine versus specialty medicine. CMAJ 2004;170:1920–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris MG, Gavel PH, Young JR. Factors influencing the choice of specialty of Australian medical graduates. Med J Aust 2005;183:295–300 [DOI] [PubMed] [Google Scholar]
- 16.Cochran A, Melby S, Neumayer LA. An internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg 2005;189:742–6 [DOI] [PubMed] [Google Scholar]
- 17.Gagne R, Leger PT. Determinants of physicians’ decisions to specialize. Health Econ 2005;14:721–35 [DOI] [PubMed] [Google Scholar]
- 18.Kutob RM, Senf JH, Campos-Outcalt D. The diverse functions of role models across primary care specialties. Fam Med 2006;38:244–51 [PubMed] [Google Scholar]
- 19.Sanfey HA, Saalwachter-Schulman AR, Nyhof-Young JM, et al. Influences on medical student career choice: gender or generation? Arch Surg 2006;141:1086–94; discussion 94 [DOI] [PubMed] [Google Scholar]
- 20.Lambert TW, Goldacre MJ, Turner G. Career choices of United Kingdom medical graduates of 2002: questionnaire survey. Med Educ 2006;40:514–21 [DOI] [PubMed] [Google Scholar]
- 21.Horn L, Tzanetos K, Thorpe K, et al. Factors associated with the subspecialty choices of internal medicine residents in Canada. BMC Med Educ 2008;8:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA 2008;300:1154–64 [DOI] [PubMed] [Google Scholar]
- 23.Scott IM, Matejcek AN, Gowans MC, et al. Choosing a career in surgery: factors that influence Canadian medical students’ interest in pursuing a surgical career. Can J Surg 2008;51:371–7 [PMC free article] [PubMed] [Google Scholar]
- 24.West CP, Drefahl MM, Popkave C, et al. Internal medicine resident self-report of factors associated with career decisions. J Gen Intern Med 2009;24:946–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med 2010;85(Suppl 10):S81–8 [DOI] [PubMed] [Google Scholar]
- 26.Goldacre MJ, Laxton L, Lambert TW. Medical graduates’ early career choices of specialty and their eventual specialty destinations: UK prospective cohort studies. BMJ 2010;341:c3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lefevre JH, Roupret M, Kerneis S, et al. Career choices of medical students: a national survey of 1780 students. Med Educ 2010;44:603–12 [DOI] [PubMed] [Google Scholar]
- 28.Fukuda Y, Harada T. Gender differences in specialty preference and mismatch with real needs in Japanese medical students. BMC Med Educ 2010;10:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glynn RW, Kerin MJ. Factors influencing medical students and junior doctors in choosing a career in surgery. Surgeon 2010;8:187–91 [DOI] [PubMed] [Google Scholar]
- 30.Bindal T, Wall D, Goodyear HM. Medical students’ views on selecting paediatrics as a career choice. Eur J Pediatr 2011;170:1193–9 [DOI] [PubMed] [Google Scholar]
- 31.Heikkila T, Hyppola H, Kumpusalo E, et al. Choosing a medical specialty—study of Finnish doctors graduating in 1977–2006. Med Teach 2011;33:e440–5 [DOI] [PubMed] [Google Scholar]
- 32.Scott I, Gowans M, Wright B, et al. Determinants of choosing a career in family medicine. CMAJ 2011;183:E1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kiolbassa K, Miksch A, Hermann K, et al. Becoming a general practitioner—which factors have most impact on career choice of medical students? BMC Fam Pract 2011;12:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ravindra P, Fitzgerald JE. Defining surgical role models and their influence on career choice. World J Surg 2011;35:704–9 [DOI] [PubMed] [Google Scholar]
- 35.Sivey P, Scott A, Witt J, et al. Junior doctors’ preferences for specialty choice. J Health Econ 2012;31:813–23 [DOI] [PubMed] [Google Scholar]
- 36.Gaucher S, Thabut D. Medical specialty choice: what impact of teaching? Results of a survey of two medical schools. Presse Med 2012. doi: 10.1016/j.lpm.2012.09.009. http://www.ncbi.nlm.nih.gov/pubmed/23153523?dopt=Citation [DOI] [PubMed] [Google Scholar]
- 37.Mena G, Llupia A, Sequera VG, et al. Specialized health education: medical students’ preferences and perceptions. Med Clin (Barc) 2012. doi: 10.1016/j.medcli.2012.09.031. http://www.ncbi.nlm.nih.gov/pubmed/23199832?dopt=Citation [DOI] [PubMed] [Google Scholar]
- 38.Gonzalez Lopez-Valcarcel B, Perez P Barber, Rubio V Ortun. ¿Por qué los médicos huyen y rehúyen la Medicina de Familia? Datos y claves sobre el problema en busca de soluciones. In: Ortún V, ed. La refundación de la Atención Primaria. Madrid: Springer Healthcare, 2011 [Google Scholar]
- 39.González López-Valcárcel B, Barber Pérez P. Planificación y formación de profesionales sanitarios, con foco en la atención primaria. Informe SESPAS 2012. Gaceta Sanitaria 2012. Published Online: 27 January 2012 doi:10.1016/j.gaceta.2011.07.029 [DOI] [PubMed] [Google Scholar]
- 40.Ministerio de Sanidad y Política Social Orden SAS/2448/2010, de 15 de septiembre, por la que se aprueba la convocatoria de pruebas selectivas 2010 para el acceso en el año 2011, a plazas de formación sanitaria especializada para Médicos. Boletín Oficial del Estado 2010;230(Sec. II.B.):80254–449 [Google Scholar]
- 41.Servicio Público de Empleo Estatal (SEPE) Información mensual de mercado de trabajo de titulados universitarios. Madrid: Gobierno de España, Ministerio de Trabajo e Información: 2010. http://www.sepe.es/contenido/observatorio/titulaciones/2010_02/titulados/ciencias_de_la_salud/ESTUDIO_TITULADOS_FI_4.pdf [Google Scholar]
- 42.Balsells F, Visa L. El recorte en sanidad alcanza las urgencias del hospital de l'Esperança: Salud decidirá antes del 22 de abril los recortes en personal, camas y servicios. El País 2011 http://elpais.com/diario/2011/04/01/catalunya/1301620038_850215.html [Google Scholar]
- 43.Servicio Público de Empleo Estatal (SEPE) Información mensual de mercado de trabajo de titulados universitarios. Madrid: Gobierno de España, Ministerio de Trabajo e Información, 2012 [Google Scholar]
- 44.Train K. Discrete choice methods with simulation, 2nd edn New York: Cambridge University Press, 2009 [Google Scholar]
- 45.Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ 2008;27:1078–94 [DOI] [PubMed] [Google Scholar]
- 46.Hosmer DW, Hosmer T, Le Cessie S, et al. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 1997;16:965–80 [DOI] [PubMed] [Google Scholar]
- 47.Kongsved SM, Basnov M, Holm-Christensen K, et al. Response rate and completeness of questionnaires: a randomized study of Internet versus paper-and-pencil versions. J Med Internet Res 2007;9:e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Compton MT, Frank E, Elon L, et al. Changes in U.S. medical students’ specialty interests over the course of medical school. J Gen Intern Med 2008;23:1095–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kazerooni EA, Blane CE, Schlesinger AE, et al. Medical students’ attitudes toward radiology: comparison of matriculating and graduating students. Acad Radiol 1997;4:601–7 [DOI] [PubMed] [Google Scholar]
- 50.West CP, Popkave C, Schultz HJ, et al. Changes in career decisions of internal medicine residents during training. Ann Intern Med 2006;145:774–9 [DOI] [PubMed] [Google Scholar]
- 51.Leo J. España supera la barrera de los 2.000 médicos en paro. Redacción Médica 2012;. [Google Scholar]
- 52.Simoens S, Hurst J. The supply of physician services in OECD countries. Paris: OECD Directorate for Employment, Labour and Social Affairs, Health Working Papers No. 21, 2006 [Google Scholar]
- 53.Nicholson S. How much do medical students know about physician income? J Hum Resour 2005;40:100–14 [Google Scholar]
- 54.OECD 3. Health workforce: 3.4 remuneration of doctors (general practitioners and specialists). Health at a Glance 2011: OECD Indicators 2012:66–7 [Google Scholar]
- 55.Ubach C, Scott A, French F, et al. What do hospital consultants value about their jobs? A discrete choice experiment. BMJ 2003;326:1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scott A. Eliciting GPs’ preferences for pecuniary and non-pecuniary job characteristics. J Health Econ 2001;20:329–47 [DOI] [PubMed] [Google Scholar]
- 57.Gunther OH, Kurstein B, Riedel-Heller SG, et al. The role of monetary and nonmonetary incentives on the choice of practice establishment: a stated preference study of young physicians in Germany. Health Serv Res 2010;45:212–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sevillano EG. Los médicos denuncian que la jornada de 37,5 horas les ha restado nómina. El País 25 April 2012 [Google Scholar]
- 59.Blasco P. Los médicos denuncian que, además de ampliar su horario, pierden sueldo. El Mundo 23 April 2012 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.