Abstract
Introduction
There is limited pediatric information on the complex relationships among the dose of tenofovir disoproxil fumarate (TDF), plasma concentrations of tenofovir (TFV), and intracellular TFV-diphosphate (TFV-DP) concentrations. Our objectives were to describe TFV-DP pharmacokinetics in children and adolescents and investigate the effect of age on TFV and TFV-DP concentrations.
Methods
TFV-DP pharmacokinetics were determined in 47 children and adolescents. TFV and TFV-DP were quantified with validated LC/MS/MS methods. Data were pooled with other studies in HIV-infected adults (N=55). Nonlinear mixed effects modeling was used to develop the population model and explore the influence of covariates on TFV. A two-compartment model, partitioned for slow and fast absorbers by age, with weight allometrically scaled for children and adolescents best described TFV pharmacokinetics. An indirect stimulation of response model best described TFV-DP formation.
Results
Apparent oral TFV clearance (CL/F) was significantly faster in patients <25 versus ≥25 years. The most significant covariate on CL/F and central distribution volume was creatinine clearance. The TFV plasma concentration producing 50% of maximal TFV-DP concentrations (EC50) was almost 2-fold lower in patients <25 versus ≥25 years. The estimated intracellular TFV-DP half-life for these groups was 70 and 87 hours, respectively.
Conclusions
These data demonstrate children and adolescents receiving standard TDF dosing of 300 mg once daily achieve higher intracellular TFV-DP concentrations than adults, despite lower plasma TFV concentrations. This age-related difference appears to arise from an increased sensitivity to formation of TFV-DP.
Keywords: age difference, antiretroviral therapy, NRTI, tenofovir, tenofovir diphosphate
Tenofovir disoproxil fumarate (TDF), anucleotide analogue and prodrug of tenofovir (TFV), is widely used in combination with other antiretrovirals for treatment of human immunodeficiency virus type 1 (HIV-1) infection. Intracellular phosphorylation of TFV to TFV-diphosphate (TFV-DP) is necessary for inhibition of viral reverse transcriptase. Our previous work has elucidateda relationship between plasma concentrations of TFV and formation of intracellular TFV-DP in adults [1]. We showed TFV-DP formation could be described as a function of plasma TFV concentrations with an indirect, stimulation of response, maximum effect (Emax) model. The estimated elimination half-life of TFV-DP was 87 hours, consistent with in vitro data.
Pediatric pharmacokinetic data for TFV in plasma are limited; information on intracellular concentrations of TFV-DP in children even more so. International Maternal Pediatric and Adolescent AIDS Clinical Trial Group (IMPAACT) study P1058 evaluated the steady-state pharmacokinetics of TFV and TFV-DP in HIV-infected pediatric patients on stable antiretroviral therapy; plasma TFV data have been previously published [2]. The objective of the present work was to describe the pharmacokinetics of intracellular TFV-DP in these HIV-infected pediatric patients and investigate age related differences.
Methods
Study design, subjects, and bioanalytical methods
P1058 determined the steady-state pharmacokinetics of TFV and TFV-DP when TDF was given in combination with nucleoside (NRTI) or non-nucleoside reverse transcriptase inhibitors (NNRTI) with or without protease inhibitors (PIs) to 47 children and adolescents [2]. These data were pooled with those from two other studies in adolescents and adults. The first study, conducted by the Adolescent Trials Network (ATN) for HIV/AIDS Interventions (Protocol ATN056) characterized TFV and ritonavir-boosted atazanavir pharmacokinetics [3]. The second was a single-center two-group study (known as 1427) of TFV pharmacokinetics and renal clearance in persons taking lopinavir/ritonavir versus those not receiving a PI [4]. In all studies, the TDF dose was 300 mg once daily, administered following a meal. Steady state TFV plasma concentrations were measured at six or eight different sampling times based on the study (one sample before TDF administration and five or seven at specified times throughout the 24 hour dosing interval) from 102 patients (61 male/41 female). Among the 102 patients, 88 had measurements of intracellular TFV-DP concentrations at 2 or 3 different sampling times, either pre-dose, 1, 4, 5, and/or 24 hours post dose. The complete study methods and primary results of these two studies have been published [2–4]. The institutional review boards at each site recruiting subjects approved the studies, and all subjects provided written informed consent. For all studies, plasma TFV and intracellular TFV-DP concentrations in peripheral blood mononuclear cells (PBMCs) were quantified by validated liquid chromatography/tandem mass spectrometry (LC/MS/MS) procedures, as previously described, in the same laboratory [5–7].
Population pharmacokinetic modeling
Pharmacokinetic modeling was accomplished using a nonlinear mixed effects approach. A first-order conditional estimation method with interaction (FOCEI; NONMEM® Version 7.2 and PDx-Pop Version 5, ICON Development Solutions, Hanover, MD) [8]. Xpose [9] and R (http://www.r-project.org/) were used for goodness-of-fit assessment and model evaluation.
The model building process has been discussed in detail previously [1]. In this study, however, following development of a base two-compartment model for plasma TFV, further model development was undertaken with the population subdivided by age (<25 years of age hereafter referred to as children and young persons, where young persons are an age group between 10–24 years as defined by WHO [10], and adults ≥25 years of age). Weight was scaled to 70 kg body weight for children and young persons using the allometric 0.75 or 1 power model for clearance/inter-compartmental clearance (CL/Q) or volume terms (V), respectively, and the absorption rate constant for plasma TFV was partitioned for slow and fast absorbers (Tmax either <2 or >2 hrs, respectively). An exponential and proportion error model for inter- and intra-patient variability, respectively, was utilized to describe plasma TFV pharmacokinetics. The variance component and consequently covariates for Q/F were not estimated. Following identification of this modified base model, the influence of demographic covariates (sex, weight, and race), estimated creatinine clearance (CrCL), method of Cockcroft and Gault [11] for patients >18 years and Schwartz equation [12] for patients <18 years, and tanner stage (only P1058) [13] on TFV pharmacokinetics were evaluated. Selection criteria for significant parameter-covariate relationships were similar to previously published approaches [1].
Plasma and intracellular concentrations were modeled sequentially. The plasma concentration producing 50% (EC50) of the maximum TFV-DP concentrations (Emax) and intracellular elimination rate constant (kout) of TFV-DP were partitioned by age (<25 or ≥25 years) in the indirect stimulation of TFV-DP formation model. The zero-order constant for production of the response (kin) was estimated but not partitioned. The kout for the adult population was fixed to the previously estimated value [1] and Emax was fixed to the maximum value of measured intracellular concentrations (1200 fmol/106 cells). Inter individual variability using an exponential error model was described only for EC50 and a proportional error was used to describe residual variability. Apart from partitioning by age, a full covariate analysis was not performed for the intracellular model due to data limitations. Model evaluations were performed utilizing the bootstrap method by simulating one thousand data-sets and visual predictive check (VPC) by simulating 500 datasets.
Results
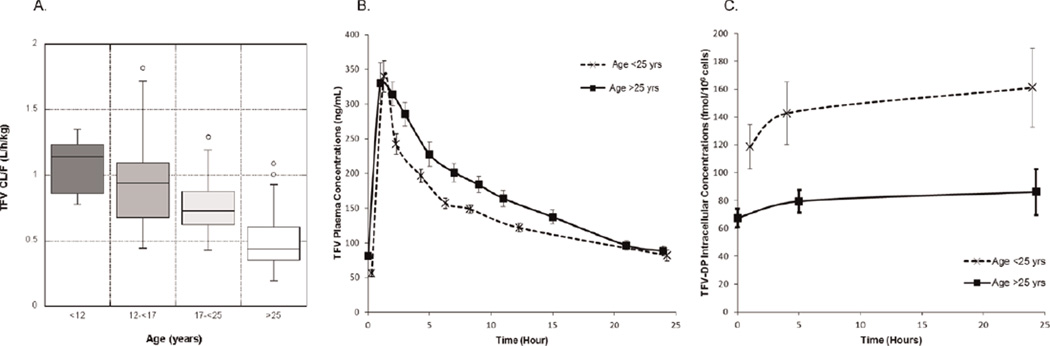
The patient demographics and analysis results are presented in Table 1. TFV plasma CL/F by age groups and mean plasma TFV and intracellular TFV-DP concentrations for <versus ≥25 years of age are presented in Fig. 1.
Table 1.
Patient Characteristics and Pharmacokinetic Parameters.
| <25 years of Age Children and Young Persons (N = 72) |
≥25 years of Age Adults (N = 30) |
|
|---|---|---|
| Patient Characteristics (Median and Range) | ||
| Gender (Male/Female) | 39/33 | 22/8 |
| Age (years) | 16 (8.6–25) | 39.5 (25–60) |
| Body weight (kg) | 58.1 (32.6–131.6) | 78 (38.7–121.4) |
| CrCL (mL/min)a | 144.1 (65.7–267.6) | 95.1 (43.2–154.9) |
| Pharmacokinetic Parameters (Parameter Estimates (95% CI)) | ||
| TFV CL/F (L/h) | 57.6 (52.8–62.4) | 42.3 (38.3–46.3) |
| TFV Vc/F (L) | 392 (287–497) | 367 (289–445) |
| TFV Vp/F (L) | 654 (522–786) | 414 (352–476) |
| TFV AUCτ (mg*hr/mL)d | 2.99 (1.23–6.35) | 3.79 (1.58–6.27) |
| TFV-DP C24 (fmol/106 cells)b,d | 95.89 (4.31–1143.4) | 60.59 (10.59–414.62) |
| EC50 (ng/mL)b,c | 100.5 (13.8–299) | 192 (3–884) |
| TFV-DP T1/2 (hours)b | 70 | 87 (Fixed) |
For patients under 18 years, Schwartz formula was used to estimate CrCL.
N = 56 (<25 years) and N = 32 (>25 years).
Bootstrap estimates.
Median and Range.
Fig. 1. Box plot of plasma TFV CL/F versus age group (1a); mean (and standard error of the mean) plasma TFV concentrations in subjects <25 years of age and ≥25 years of age (1b); and intracellular TFV-DP concentrations (1c) in subjects <25 years of age and ≥25 years of age.
Plasma TFV CL/F normalized by weight was highest in those <12 years followed by 12 to <17 years, 17 to <25 years and then lowest for >25 years. Overall, plasma TFV concentrations were lower in study participants <25 years of age (estimated CL/F of 57.6 L/hr) than in adults (estimated CL/F 42.3 L/hr). The median intracellular TFV-DP concentrations were higher in subjects <25 years of age compared with adults: TFV-DP C24 was 96 fmol/106 cells versus 61 fmol/106 cells.
The 47 patients (25 male and 22 female; 8.6 to 17 years; mean CrCL, 154.5 ml/min) from the P1058 population had plasma TFV concentrations ranging from 16.4 to 920.1 ng/mL; intracellular TFV-DP concentrations in 37 of these patients ranged from 4.3 to 1143.4 fmol/106 cells. The 55 patients in the ATN and 1427 populations had TFV plasma concentrations ranging from 12.5 to 643 ng/mL and intracellular concentrations in 51 of these patients ranged from 10.6 to 414 fmol/106 cells. The final population model for plasma TFV found an approximately 36% faster apparent oral clearance (CL/F) for children and young persons when compared with adults. Typical CL/F was 57.6 L/hr in children and young persons compared with 42.3 L/hr for adults with a 31.2% inter-individual variability on both populations. CrCL was the most significant covariate on CL/F and apparent volume of the central compartment (Vc/F). The EC50 was 100 ng/mL for the children and young person cohort compared with 192 ng/mL for adults. The intracellular elimination half-life of TFV-DP for children and young persons was estimated at 70 hours versus the previously estimated half-life of 87 hours in adults.
Discussion
These data suggest an influence of age on TFV and TFV-DP pharmacokinetics. These results validate previous findings of age related differences in TFV pharmacokinetics between older and younger adults and extend them to a younger population of children and adolescents [3,14–16]. In this analysis, interestingly, the lower plasma TFV concentrations in children and young persons did not result in decreased intracellular TFV-DP concentrations. TFV-DP concentrations were almost 50% higher in children and young persons compared with adults.
The population PK model satisfactorily described TFV plasma and TFV-DP intracellular concentrations. We noticed some patients achieved plasma Cmax faster than others, perhaps due to the type of food taken. As expected, results showed TFV CL/F was dependent upon renal function with CrCL having a significant influence on TFV CL/F and Vc/F. The most likely explanation for the faster CL/F of TFV in children and young persons is their relatively increased kidney size compared with body size and/or increased kidney function. Overall, the estimates for CL/F and Vc/F and the variability associated with these parameters compare well with literature values for both adult [17,18] and adolescent populations [16].
Others have previously suggested children and adolescents have a lower systemic exposure to TFV compared with adults [14– 16]. An unanticipated finding in this study was higher intracellular TFV-DP concentrations in children and young persons despite their lower parent drug systemic exposure. Intuitively, a decreased intracellular exposure would be expected as a consequence of lower plasma TFV exposure. This is not the first inverse relationship found for a nucleoside, however; increased intracellular zidovudine monophosphate concentrations were associated with lower plasma zidovudine [19]. The pharmacokinetic modeling results suggest the higher intracellular TFV-DP concentrations arise from children and young persons being more susceptible to formation of TFV-DP from a given level of exposure to TFV, as seen by a lower EC50, instead of slower intracellular elimination.
There are limitations to the strength of these observations. The primary is the need to fix the intracellular parameters Emax and adult kout, because of data limitations. However, we did perform a sensitivity analysis with various scenarios of fixing parameter estimates versus estimating parameters. Different estimates for Emax were tested by either fixing to different literature estimates ranging from 400 to 2000 fmol/106 cells or by estimating Emax. Similarly, adult kout values were fixed to literature ranging values from 20 to 100 hours or estimating, but none of these resulted in successful model convergence or minimization. The VPC evaluation of the final model supported a reliable description of the TFV and TFV-DP data.
Antiretroviral therapy in children and adolescents requires knowledge of age-related pharmacokinetic characteristics, and dosing strategies to account for developmental associated changes in these characteristics. The paradigm of antiretroviral dosing in children and adolescents, especially with TDF and other NRTIs, has been based on the assumption that achieving a plasma exposure similar to an adult would result in a similar intracellular exposure. Evidence to prove this assumption is lacking. The present data provide evidence to the contrary. These observations, which need confirmation, potentially have clinically relevant dosing implications for NRTIs in children. A similar plasma exposure that achieves increased intracellular concentrations may have excellent efficacy but could result in increased rates of adverse reactions, such as mitochondrial [20] or renal toxicity [21]. Conversely, a similar plasma exposure that results in lower intracellular concentrations may increase the risk of virologic failure. Either of these scenarios provides motivation for an increased emphasis on achieving intracellular drug exposure in children and adolescents that is similar to adults as a determinant of NRTI dosing strategies. TDF has recently been approved by the FDA for use in children 2 years and older. No signals are apparent that children and adolescents have different or a different incidence of TDF-related adverse events. The limited experience with long-term therapy and higher intracellular exposure in children warrant careful monitoring to be certain this remains the case.
In conclusion, our data suggest that compared with adults, children and young persons who receive the usual TDF dose of 300 mg once daily, have lower plasma TFV concentrations but increased intracellular TFV-DP concentrations. Further examination of this age related difference in plasma and intracellular pharmacokinetics offers the potential to understand the mechanism(s) responsible and may facilitate more informed investigations of the clinical and intracellular pharmacology of TFV.
Acknowledgements
Support was provided by P01 AI074340 (to CVF) from the National Institute of Allergy and Infectious Diseases (NIAID), and the International Maternal Pediatric Adolescent AIDS Clinical Trial (IMPAACT) Group, which is supported by NIAID (U01 AI068632), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institute of Mental Health (NIMH). We are grateful to the individuals who participated in this study, and the investigators and staff for their valuable contributions.
Footnotes
Author Contributions: G.B and C.V.F developed the objective for this study and performed all data analyses. J.R.K. was chair of the IMPAACT P1058 protocol. G.B., J.R.K., E.P.A., and C.V.F. all contributed to the interpretation of the results and to the preparation of the manuscript.
Conflicts of interest
None declared
References
- 1.Baheti G, et al. Plasma and intracellular population pharmacokinetic analysis of tenofovir in HIV-1-infected patients. Antimicrobial agents and chemotherapy. 2011;55:5294–5299. doi: 10.1128/AAC.05317-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King JR, et al. Steady-state pharmacokinetics of tenofovir-based regimens in HIV-infected pediatric patients. Antimicrobial agents and chemotherapy. 2011;55:4290–4294. doi: 10.1128/AAC.01334-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kiser JJ, et al. Pharmacokinetics of antiretroviral regimens containing tenofovir disoproxil fumarate and atazanavir-ritonavir in adolescents and young adults with human immunodeficiency virus infection. Antimicrob Agents Chemother. 2008;52:631–637. doi: 10.1128/AAC.00761-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kiser JJ, et al. The effect of lopinavir/ritonavir on the renal clearance of tenofovir in HIV-infected patients. Clin Pharmacol Ther. 2008;83:265–272. doi: 10.1038/sj.clpt.6100269. [DOI] [PubMed] [Google Scholar]
- 5.Delahunty T, Bushman L, Fletcher CV. Sensitive assay for determining plasma tenofovir concentrations by LC/MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci. 2006;830:6–12. doi: 10.1016/j.jchromb.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Delahunty T, et al. The simultaneous assay of tenofovir and emtricitabine in plasma using LC/MS/MS and isotopically labeled internal standards. J Chromatogr B Analyt Technol Biomed Life Sci. 2009;877:1907–1914. doi: 10.1016/j.jchromb.2009.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King T, et al. Liquid chromatography-tandem mass spectrometric determination of tenofovir-diphosphate in human peripheral blood mononuclear cells. J Chromatogr B Analyt Technol Biomed Life Sci. 2006;843:147–156. doi: 10.1016/j.jchromb.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 8.Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM User’s Guides (1989–2009) Ellicott City, MD, USA: Icon Development Solutions; 2009. [Google Scholar]
- 9.Jonsson EN, Karlsson MO. Xpose–an S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Computer methods and programs in biomedicine. 1999;58:51–64. doi: 10.1016/s0169-2607(98)00067-4. [DOI] [PubMed] [Google Scholar]
- 10.Sawyer SM, et al. Adolescence: a foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 11.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz GJ, et al. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 1976;58:259–263. [PubMed] [Google Scholar]
- 13.Schneider MB. In: Physical examination. 2nd Ed ed. Comprehensive Adolescent Health Care. F.M. Friedman SB, Schoenberg SK, Alderman EM, editors. St. Louis, MO: Mosby-Year Book, Inc.; 1998. pp. 69–80. [Google Scholar]
- 14.Hazra R, et al. Single-dose and steady-state pharmacokinetics of tenofovir disoproxil fumarate in human immunodeficiency virus-infected children. Antimicrob Agents Chemother. 2004;48:124–129. doi: 10.1128/AAC.48.1.124-129.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirt D, et al. Plasma and intracellular tenofovir pharmacokinetics in the neonate (ANRS 12109 trial, step 2) Antimicrobial agents and chemotherapy. 2011;55:2961–2967. doi: 10.1128/AAC.01377-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bouazza N, et al. Population pharmacokinetics of tenofovir in HIV-1-infected pediatric patients. Journal of acquired immune deficiency syndromes. 2011;58:283–288. doi: 10.1097/QAI.0b013e3182302ea8. [DOI] [PubMed] [Google Scholar]
- 17.Gagnieu MC, et al. Population pharmacokinetics of tenofovir in AIDS patients. Journal of Clinical Pharmacology. 2008;48:1282–1288. doi: 10.1177/0091270008322908. [DOI] [PubMed] [Google Scholar]
- 18.Jullien V, et al. Population pharmacokinetics of tenofovir in human immunodeficiency virus-infected patients taking highly active antiretroviral therapy. Antimicrob Agents Chemother. 2005;49:3361–3366. doi: 10.1128/AAC.49.8.3361-3366.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodman JH, et al. A systemic and cellular model for zidovudine plasma concentrations and intracellular phosphorylation in patients. The Journal of infectious diseases. 1996;174:490–499. doi: 10.1093/infdis/174.3.490. [DOI] [PubMed] [Google Scholar]
- 20.Kohler JJ, et al. Tenofovir renal toxicity targets mitochondria of renal proximal tubules. Laboratory investigation a journal of technical methods and pathology. 2009;89:513–519. doi: 10.1038/labinvest.2009.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodriguez-Novoa S, et al. Impairment in kidney tubular function in patients receiving tenofovir is associated with higher tenofovir plasma concentrations. AIDS. 2010;24:1064–1066. doi: 10.1097/QAD.0b013e32833202e2. [DOI] [PubMed] [Google Scholar]