Abstract
This article updates trends from five national U.S. surveys to determine whether the prevalence of activity limitations among the older population continued to decline in the first decade of the twenty-first century. Findings across studies suggest that personal care and domestic activity limitations may have continued to decline for those ages 85 and older from 2000 to 2008, but generally were flat since 2000 for those ages 65–84. Modest increases were observed for the 55- to 64-year-old group approaching late life, although prevalence remained low for this age group. Inclusion of the institutional population is important for assessing trends among those ages 85 and older in particular.
Keywords: Aging, Disability, Functioning, Trends, Harmonization
Introduction
Over the past 50 years, life expectancy has increased in the United States to nearly 78 years of age (Xu et al. 2010). Although the increase has recently slowed, a fundamental focus of the literature on the demography of aging continues to be whether such increases have been accompanied by an expansion or a contraction in the number of years of life spent with disability (Crimmins 2004; Martin et al. 2010b).
Late-life activity limitations are of particular interest because the economic costs of dependency and underlying medical conditions at older ages are large and projected to grow rapidly in the coming decades (Johnson and Wiener 2006). In addition, maintaining the well-being of older individuals experiencing declines in functioning and their families is a fundamental societal concern. Hence, tracking the proportion of older adults and of those nearing late life who need assistance with daily tasks has become an important and policy-relevant exercise.
Dozens of studies have documented and verified substantial declines in the prevalence of late-life activity limitations in the United States from the mid-1980s through the late 1990s, including an earlier collaborative study (Freedman et al. 2004), which this research updates and extends. Indeed, these declines have been viewed as one of the most significant advances in the health and well-being of Americans in the past quarter-century (Schoeni et al. 2008). In this research note, we present findings for the period 2000–2008.
Data and Methods
Data Sets
We analyzed five national data sets covering the older U.S. population (parenthetical Ns refer to the 65-and-older community population in 2008 except where noted): (1) the biennial 2000–2008 Health and Retirement Study (HRS; N = 10,573), (2) the 2000–2008 Medicare Current Beneficiary Survey (MCBS; N = 12,597 including institutional population), (3) the 2000–2008 National Health Interview Survey (NHIS; N = 8,478), (4) the 1999/2000 to 2007/2008 National Health and Nutrition Examination Survey (NHANES; N = 1,556 in 2007/2008), and (5) the 1999 and 2004 National Long Term Care Survey (NLTCS; N = 16,080 in 2004 including institutional population). Of the five studies, only the NLTCS and MCBS allow analysis of trends across both community and institutional populations. See Online Resource 1 for additional study details.
Measures
We first constructed broad measures of limitations in activities of daily living (ADLs) and instrumental activities of daily living (IADLs), using all available activities. For HRS, MCBS, and NHANES, the broadest definition was “difficulty with IADLs or ADLs,” with the latter two studies asking respondents to focus on difficulty without help or special equipment. For HRS, IADL responses of “yes” (has difficulty), “can't do,” and “don't do because of a health or memory problem,” and ADL responses of “yes,” “can't do,” and “don't do” were considered limitations. For MCBS, for both ADLs and IADLs, individuals responding “yes” or “doesn't do for a health reason” were considered limited, as were residents of long-term care facilities. For NHANES, responses of “some difficulty,” “much difficulty,” or “unable to do” were treated as limitation. For NHIS, we used a measure of needing help with IADLs or ADLs. Finally, for NLTCS, we used the summary measure of ADL or IADL limitation or institutional residence provided with the public-use data: ADL limitation was defined as inability, use of assistive devices, having active or standby help, or need for help in the prior week and IADL limitation as inability to perform an activity because of disability or a health problem. In addition, all institutional residents were considered to have limitations.
We also constructed common definitions across surveys. For IADLs, we created two measures: difficulty with activities and inability to perform activities (“can't do” or “doesn't do” for health-related reasons). For both measures, we identified four IADL activities that were common across three studies (HRS, MCBS, and NLTCS): preparing meals, shopping, managing money, and making phone calls. For ADLs, we also created two measures: difficulty performing ADLs and receiving (or needing) help. For difficulty with activities, we compared HRS, MCBS, and NHANES estimates. Both HRS and MCBS identify difficulty with any of six activities (bathing, dressing, eating, transferring, toileting, or walking). We also included NHANES in the comparison, although it excludes questions on toileting and bathing. For help, we focused on any of the six activities using HRS, MCBS, and NLTCS, which measure receipt of help, and using NHIS, which measures need for help.
Analyses
To test for trends, we estimated a series of linear probability models for each survey using pooled samples over all years included. For each model, we regressed a dependent variable valued 1 for the outcome of interest (e.g., any of four IADLs) and 0 otherwise on a trend variable valued 0 for the base year and valued in subsequent years according to the interval between survey waves (e.g., 1, 2, 3 for the annual MCBS and NHIS; 2, 4, 6 for the biennial HRS). We chose this modeling strategy over logistic regression because the coefficient estimate for the trend variable is readily interpreted as the average annual percentage point change over the study period. In all cases, standard errors were adjusted for complex sample design.
We estimated separate models for the full period (2000–2008) and for the first and latter half of the period (2000–2004, 2004–2008). For the two surveys for which we did not have point estimates for 2000, we used 1999 (NLTCS) or a combination of 1999 and 2000 (NHANES). We also ran age-specific models with 10-year groupings. Because NHANES began top-coding age in the later period, only selected estimates are presented for that survey. We also examined trends for the 55–64 age group using the HRS and NHIS, and we examined the sensitivity of trend estimates to inclusion of the institutional population in the MCBS and NLTCS.
Results
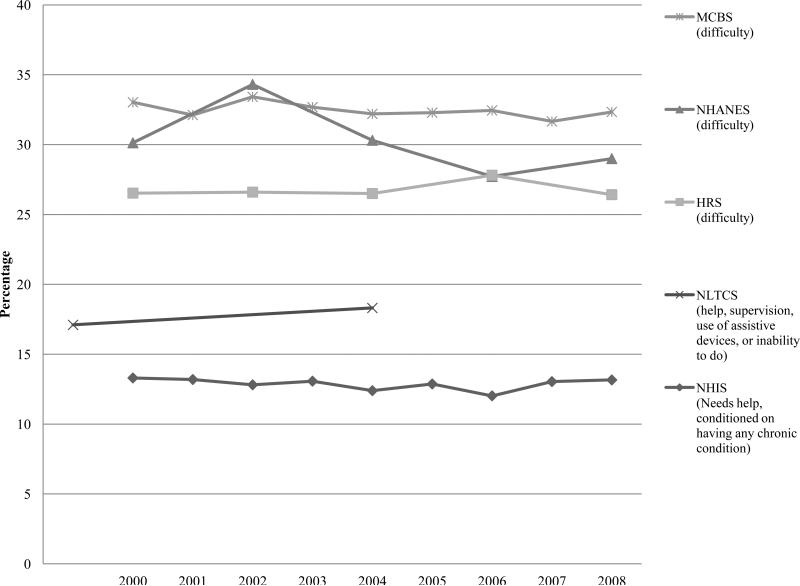
The five surveys produce a wide range of estimates but no evidence of continued downward trends in ADL or IADL limitations taken together for the 65-and-older population as a whole. The three surveys measuring difficulty produce consistently higher prevalence than the measures of getting or needing help (Fig. 1), as would be expected. No survey shows a significant trend from 2000 to 2008. Only the NLTCS estimates (defined as using assistive devices, having active or standby help, or needing help) show a statistically significant difference between the observations in 1999 and 2004, which suggests a slight increase in the prevalence of activity limitations among the community-based older population.
Fig. 1.
Prevalence of any ADL or IADL limitation, 2000–2008: Community-based population ages 65 and older
Adding the institutional population to estimates for the MCBS and NLTCS in Fig. 1 would increase the prevalence of activity limitations in each year by roughly 3 percentage points, but the overall trend would remain nonsignificant for the MCBS and would become nonsignificant for the NLTCS (not shown). In both surveys, the size of the institutional population declined significantly (about 0.1 percentage points per year) during the study period.
IADL Limitations
Based on the common definitions of IADL limitations, results for the community-residing population are mixed (Table 1). For the 65-and-older population, both the MCBS and the HRS indicate a flat trend in difficulty with IADL activities, but the MCBS shows declines in the percentage reporting inability to perform one or more of these activities (–0.14 percentage points per year; p < .01). Focusing on the age-specific results, the MCBS shows sizable declines for the 85-and-older population of 0.77 and 0.54 percentage points for difficulty and inability, respectively, and a 0.1 percentage point decline per year in inability (p <. 05) for those ages 65–74. Although the HRS estimates show no significant decline for any age group from 2000 to 2008, they indicate large significant declines for the 85-and-older group for both difficulty and inability in the 2004–2008 period, balanced by increases in the 2000–2004 period.
Table 1.
Prevalence of any IADL limitation, 2000–2008: Community-based population ages 65 and oldera
| Difficulty With IADLs |
Unable to Perform IADLs |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of Community Population |
Average Annual % Point Changeb |
% of Community Population |
Average Annual % Point Changeb |
|||||||||
| Survey | 2000 | 2004 | 2008 | 2000–2008 | 2000–2004 | 2004–2008 | 2000 | 2004 | 2008 | 2000–2008 | 2000–2004 | 2004–2008 |
| All Age 65+ | ||||||||||||
| HRS | 16.0 | 17.0 | 15.8 | 0.01 | 0.25 | –0.30* | 6.6 | 7.3 | 6.6 | 0.02 | 0.19 | –0.18 |
| MCBS | 19.5 | 18.4 | 18.1 | –0.12 | –0.25 | 0.03 | 6.4 | 6.2 | 5.4 | –0.14** | –0.10 | –0.12 |
| NLTCS | — | — | — | — | — | — | 8.7 | 9.3 | — | — | 0.10 | — |
| Ages 65–74 | ||||||||||||
| HRS | 10.0 | 10.0 | 9.7 | –0.03 | 0.02 | –0.08 | 3.2 | 3.1 | 2.8 | –0.07 | –0.03 | –0.06 |
| MCBS | 11.8 | 11.3 | 11.4 | –0.07 | –0.11 | 0.06 | 3.1 | 3.0 | 2.6 | –0.10* | –0.06 | –0.08 |
| NLTCS | — | — | — | — | — | — | 4.1 | 4.4 | — | — | 0.06 | — |
| Ages 75–84 | ||||||||||||
| HRS | 18.7 | 19.1 | 18.1 | 0.01 | 0.12 | –0.24 | 7.8 | 8.3 | 7.6 | 0.02 | 0.12 | –0.17 |
| MCBS | 22.3 | 20.3 | 19.8 | –0.16 | –0.42 | 0.00 | 6.9 | 6.4 | 5.5 | –0.15 | –0.18 | –0.13 |
| NLTCS | — | — | — | — | — | — | 10.4 | 10.6 | — | — | 0.04 | — |
| Ages 85+ | ||||||||||||
| HRS | 39.7 | 43.6 | 37.9 | –0.30 | 0.99 | –1.41** | 21.1 | 25.1 | 21.6 | 0.02 | 1.00* | –0.91* |
| MCBS | 46.4 | 41.9 | 40.0 | –0.77** | –1.06* | –0.31 | 19.8 | 19.0 | 16.5 | –0.54** | –0.39 | –0.42 |
| NLTCS | — | — | — | — | — | — | 29.8 | 30.3 | — | — | 0.11 | — |
2000 estimates are from 1999 for NLTCS and are the average of 1999 and 2000 for NHANES. 2004 estimates for NHANES are the average of 2003–2004, and 2008 estimates are the average of 2007–2008. The four IADL activities included are preparing meals, shopping, managing money, and using the telephone.
Uses all intervening waves, estimated from linear probability (ordinary least squares; OLS) models with year coded as a continuous measure, starting with baseline = 0. Estimates for the full period may fall outside those observed for the first and latter halves because of nonmonotonic changes between intervening years within each half.
p < .05
p < .01
ADL Limitations
Turning to the common definitions of ADLs (Table 2), no significant changes are observed from 1999/2000 to 2008 for the full community population age 65 or older across the five surveys, regardless of whether limitation is defined as difficulty or getting/needing help. Only one survey, the HRS, suggests a decline between 2000 and 2004: the percentage having difficulty changes by –0.31 percentage points per year. In the age-specific analyses, we see largely flat results with only a few exceptions: the HRS shows a decline in difficulty for ages 65–74 for 2000–2004, and the MCBS indicates statistically significant declines in ADL difficulty and help among the 85-and-older population (–0.49 and –0.41 percentage points per year, respectively) for 2000–2008.
Table 2.
Prevalence of any ADL limitation, 2000-2008: Community-based population ages 65 and oldera
| Difficulty With ADLs |
Help With ADLs |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of Community Population |
Average Annual % Point Changeb |
% of Community Population |
Average Annual % Point Changeb |
|||||||||
| Survey | 2000 | 2004 | 2008 | 2000–2008 | 2000–2004 | 2004–2008 | 2000 | 2004 | 2008 | 2000–2008 | 2000–2004 | 2004–2008 |
| All Age 65+ | ||||||||||||
| HRS | 20.7 | 19.5 | 20.4 | 0.01 | –0.31** | 0.21 | 8.5 | 8.4 | 8.4 | 0.00 | –0.02 | –0.02 |
| MCBS | 27.7 | 27.1 | 27.3 | –0.10 | –0.06 | –0.05 | 8.3 | 8.5 | 7.9 | –0.04 | 0.06 | –0.15 |
| NHANES | 23.6 | 25.5 | 24.2 | –0.20 | 0.50 | –0.30 | — | — | — | — | — | — |
| NHISc | — | — | — | — | — | — | 5.5 | 5.4 | 5.6 | 0.02 | –0.02 | 0.10 |
| NLTCS | — | — | — | — | — | — | 6.2 | 6.4 | — | — | 0.03 | — |
| Ages 65–74 | ||||||||||||
| HRS | 15.3 | 13.6 | 14.4 | –0.06 | –0.42** | 0.19 | 5.4 | 5.0 | 4.9 | –0.05 | –0.09 | –0.03 |
| MCBS | 20.5 | 19.6 | 20.1 | –0.13 | –0.08 | –0.08 | 4.7 | 5.1 | 4.8 | –0.02 | 0.15 | –0.10 |
| NHANES | 18.5 | 20.9 | 20.4 | –0.10 | 0.60 | –0.10 | — | — | — | — | — | — |
| NHIS3 | — | — | — | — | — | — | 3.0 | 2.7 | 2.8 | 0.00 | –0.10 | 0.02 |
| NLTCS | — | — | — | — | — | — | 3.2 | 3.2 | — | — | –0.01 | — |
| Ages 75–84 | ||||||||||||
| HRS | 23.4 | 21.6 | 22.9 | 0.01 | –0.45 | 0.33 | 9.5 | 9.2 | 9.4 | 0.02 | –0.09 | 0.07 |
| MCBS | 30.8 | 30.4 | 30.4 | –0.08 | –0.04 | –0.01 | 9.1 | 9.0 | 8.3 | –0.04 | –0.05 | –0.13 |
| NHANESd | 24.8 | 27.6 | 28.4 | 0.20 | 0.70 | 0.04 | — | — | — | — | — | — |
| NHISc | — | — | — | — | — | -- | 6.1 | 6.1 | 6.0 | –0.03 | –0.06 | 0.05 |
| NLTCS | — | — | — | — | — | -- | 7.3 | 7.4 | — | — | 0.02 | — |
| Ages 85+ | ||||||||||||
| HRS | 41.3 | 41.2 | 41.5 | –0.05 | –0.05 | 0.07 | 21.5 | 22.2 | 21.3 | –0.15 | 0.16 | –0.21 |
| MCBS | 51.4 | 48.3 | 47.7 | –0.49* | –0.79 | –0.13 | 22.4 | 21.2 | 18.6 | –0.41* | –0.42 | –0.58 |
| NHANESd | 50.0 | 42.7 | 49.1 | –0.60 | –2.00 | 3.20 | — | — | — | — | — | — |
| NHISc | — | — | — | — | — | -- | 18.0 | 16.1 | 17.3 | –0.08 | –0.06 | 0.47 |
| NLTCS | — | — | — | — | — | -- | 19.7 | 19.7 | — | — | –0.01 | — |
2000 estimates are from 1999 for NLTCS and are the average of 1999 and 2000 for NHANES. 2004 estimates for NHANES are the average of 2003–2004, and 2008 estimates are the average of 2007–2008. The six ADL activities included are bathing, dressing, eating, transferring, walking, and toileting; for NHANES, bathing and toileting are omitted.
Uses all intervening waves, estimated from linear probability models with year coded as a continuous measure, starting with baseline = 0. Estimates for the full period may falloutside those observed for the first and latter halves because of nonmonotonic changes between intervening years within each half.
Needs help, conditioned on having any chronic condition.
Because NHANES top coded age at 80 beginning in 2007, trends for this age group are through 2005/2006.
p < .05
p < .01
Adding the institutional population strengthens the declines in ADL limitations for the 85-and-older population (Table 3). For the MCBS, for instance, we find stronger declines from 2000 to 2008 in getting help with ADLs when the institutional population is included (–0.71 percentage points per year; p < .01) than when it is not (–0.41 per year; p < 0.05). Similarly, for the period up to 2004, both the MCBS and NTLCS show significant declines in getting help with ADLs for the 85-and-older population: –0.90 percentage points per year for MCBS (p < .01) and –0.60 per year for NLTCS (p < .05). For all other age groups, conclusions about trends are not changed by inclusion of the institutional population.
Table 3.
Prevalence of an ADL limitation, 2000–2008: Community-based and institutional population ages 65 and oldera
| Help With ADLs: Community and Institutional Population |
||||||
|---|---|---|---|---|---|---|
| % of Population | Average Annual % Point Changeb | |||||
| Survey | 2000 | 2004 | 2008 | 2000–2008 | 2000–2004 | 2004–2008 |
| All Age 65+ | ||||||
| MCBS | 12.0 | 11.9 | 11.0 | –0.10 | –0.04 | –0.23 |
| NLTCS | 10.4 | 10.0 | — | — | –0.09 | — |
| Ages 65–74 | ||||||
| MCBS | 5.6 | 5.9 | 5.7 | –0.02 | 0.12 | –0.10 |
| NLTCS | 4.4 | 4.1 | — | — | –0.05 | — |
| Ages 75–84 | ||||||
| MCBS | 12.5 | 12.3 | 11.2 | –0.11 | –0.10 | –0.23 |
| NLTCS | 11.3 | 10.9 | — | — | –0.07 | — |
| Ages 85+ | ||||||
| MCBS | 34.9 | 31.6 | 28.2 | –0.71** | –0.90** | –0.81* |
| NLTCS | 35.8 | 32.7 | — | — | –0.61* | — |
2000 estimates are from 1999 for NLTCS. The six ADL activities included are bathing, dressing, eating, transferring, walking, and toileting.
Uses all intervening waves, estimated from linear probability (OLS) models with year coded as a continuous measure, starting with baseline = 0. Estimates for the full period may fall outside those observed for the first and latter halves because of nonmonotonic changes between intervening years within each half.
p < .05
p < .01
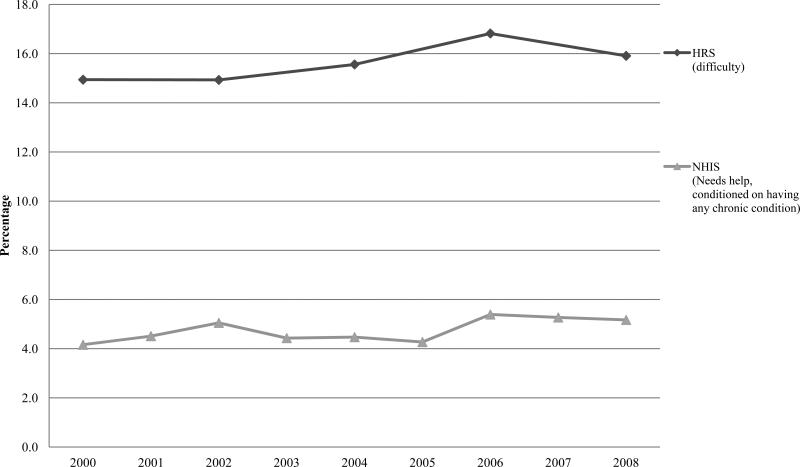
Activity Limitations in Middle Age
For the community-residing cohort approaching late life, limitations in IADLs or ADLs appear to be increasing (Fig. 2). Although the rates of activity limitations for those ages 55–64 are relatively low, both surveys show modest increases over the past decade for this age group. The NHIS indicates a significant increase of about 0.1 percentage point per year in needing help. The HRS indicates an increase of about 0.2 percentage points per year.
Fig. 2.
Prevalence of any ADL or IADL limitation, 2000–2008: Community-based population ages 55–64
Discussion
Several new findings have emerged from this analysis of U.S. activity limitation trends during the first decade of the twenty-first century. Overall, the percentage of the older population with one or more activity limitations has been flat since 2000. Yet, for the oldest-old who have the highest rates of activity limitations, we found evidence of continuing declines in both IADL and ADL limitations and of contractions in the size of the institutional population. At the same time, adults poised to enter late life over the next decade appear to have rates of activity limitations that, albeit low relative to the older age groups, are about 1 percentage point higher than the same age group born 10 years earlier.
Our analysis is limited in that it does not provide insight into why the declines of the 1980s and 1990s have paused, and this is a worthy area for further investigation. We demonstrated that the flattening is concentrated in the 65–74 and 75–84 age groups, sandwiched between increases among the 55–64 age group and decreases among those ages 85 and older. We also were unable to investigate whether declines among the oldest-old reflect improvements in the capacity to carry out activities, shifts in how activities are carried out, or the environments in which the oldest-old are living. More detailed measures of disability and functioning are needed to allow a fuller examination of such issues (Freedman et al. 2011).
Finally, the finding that activity limitations have increased over the last decade among those nearing late life is not new (e.g., Martin et al. 2010a; Seeman et al. 2010). However, our study underscores the difficulty of discerning the implication of this uptick for future trends at older ages in light of the steep increase in activity limitations with age. We agree with Martin and colleagues (2010a) that although disconcerting and worthy of careful monitoring, more research is needed to understand the implications of disability in midlife for later-life population prevalence.
Supplementary Material
Acknowledgments
This research was funded by a grant from the National Institute on Aging (P30-AG012846, PI: Bound) through the TRENDS Disability Research Network. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the funding agency or the authors’ employers.
Footnotes
An earlier version of this article was presented at the annual meeting of the Population Association of America, March 29– April 2, 2011, Washington DC.
Contributor Information
Vicki A. Freedman, Institute for Social Research, University of Michigan, 426 Thompson Street, Ann Arbor, MI 48106 vfreedma@umich.edu.
Brenda C. Spillman, Urban Institute
Patti M. Andreski, University of Michigan
Jennifer C. Cornman, University of Southern California.
Eileen M. Crimmins, University of Southern California
Ellen Kramarow, National Center for Health Statistics.
James Lubitz, RAND.
Linda G. Martin, RAND
Sharon S. Merkin, University of California Los Angeles
Robert F. Schoeni, University of Michigan
Teresa E. Seeman, University of California Los Angeles
Timothy A. Waidmann, Urban Institute
References
- Crimmins EM. Trends in the health of the elderly. Annual Review of Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins E, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Waldmann T. Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography. 2004;41:417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Kasper J, Cornman J, Agree E, Bandeen-Roche K, Mor V, Wolf D. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. Journals of Gerontology A: Biological Sciences and Medical Sciences. 2011 doi: 10.1093/gerona/glr087. doi: 10.1093/gerona/glr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R, Wiener J. Profile of frail older Americans and their caregivers (The Retirement Project, Occasional Paper Number 8) The Urban Institute; Washington, DC: 2006. Retrieved from http://www.urban.org/UploadedPDF/311284_older_americans.pdf. [Google Scholar]
- Martin LG, Freedman VA, Schoeni RF, Andreski PM. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Affairs. 2010a;29:725–731. doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Schoeni RF, Andreski PM. Trends in health of older adults in the United States: Past, present and future. Demography. 2010b;47(Suppl.):S17–S40. doi: 10.1353/dem.2010.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Quarterly. 2008;86:47–89. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988–1994 and 1999–2004. American Journal of Public Health. 2010;100:100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. National Vital Statistics Reports. 19. Vol. 58. National Center for Health Statistics; Hyattsville, MD: 2010. Deaths: Final data for 2007. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.