Abstract
Objective(s)
Isoniazid (INH) is one of the main first line drugs used in treatment of tuberculosis and development of resistance against this compound can result in serious problems in treatment procedures. Resistance to INH is mediated mainly by mutation in KatG gene that is coded for the catalase enzyme. The proportional method for detection of INH-resistance is time consuming due to the slow growth rate of Mycobacterium tuberculosis. In this study, we used PCR-RFLP approach for screening of common mutations in KatG gene for detection of INH resistance, and compared the results to minimal inhibitory concentration (MIC) in M. tuberculosis isolates.
Materials and Methods
Fifty M. tuberculosis isolates were subjected to study of which, 25 strains were INH-resistant and 25 strains were INH-sensitive.
Results
Of 25 INH-resistant strains, the mutation was identified in 56% and 20% in the KatG315 and KatG463 loci, respectively. In 24% of INH-resistant strains, no mutation was observed in the studied loci. INH MIC was <0.2 μg/ml in all sensitive strains whereas among 25 INH -resistant isolates, INH MIC was higer than 0.2 μg/ml ranged from 0.2 to 3.2 μg/ml.
Conclusion
Our findings revealed that PCR-RFLP is capable to identify INH-resistance in more than 76% of INH- resistant M. tuberculosis strains, and could be used for rapid identification of INH resistance. High levels of INH MIC were observed in the strains which had mutation in the KatG gene in position 315.
Key Words: Isoniazid Resistance, Kat G, Mycobacterium tuberculosis, PCR, RFLP
Introduction
Although tuberculosis is regarded as a historical disease, in the recent years, the medical community has increasingly worried about the spread of drug resistant Mycobacterium tuberculosis strains. Isoniazid (INH) and rifampin are two first line drugs against tuberculosis and strains display resistance against these drugs are considered as multi drug Resistant (MDR) M. tuberculosis (1-3). The control program of tuberculosis has been affected seriously by the spread of MDR strains and so, rapid identification of resistant strains has a special impact on the treatment and control of dissemination of MDR strains in the communities (4,5). INH is a pro-drug that enters into the bacillus via passive diffusion, changes into an active form by enzyme catalase-peroxidase, and then the free radicals attack different targets in the microorganism. The previous observations have showed that tuberculosis bacillus lose their acid fastness property after exposure to INH (6-9).
Drug resistance in bacterial population takes place randomly by mutations. Resistance to INH is associated with a variety of mutations in several genes like KatG, inhA, oxyR-aphC, kasA and ndh (4, 8,10). The KatG gene encodes enzyme catalase-peroxidase and mutation in this gene decreases or blocks the enzyme activity. Mutation in the katG gene is the main mechanism of INH-resistance in most strains (11).
There are various methods for detection of INH-resistant M. tuberculosis strains including conventional and molecular methods. The conventional methods based on culture and proportional assay of the bacterial sensitivity are time consuming and need several weeks for bacterial growth. In the recent years, rapid molecular techniques such as PCR-RFLP (polymerase chain reaction-restriction fragment length polymorphism) have been proposed for detection of resistance to INH. This method reduces the time of diagnosis to few hours (1, 3, 4,11). Since the frequency and type of mutations in the KatG gene are varied in different geographic regions, this study aimed to determine the prevalence of mutations in the KatG gene and INH minimal inhibition concentration (MIC) in M. tuberculosis strains in Northwest of Iran.
Materials and Methods
The bacteria included in this study were 50 isolates of M. tuberculosis which were recovered from pulmonary tuberculosis patients. Out of 50 strains, 25 were susceptible and 25 were resistant to INH. Bacterial culture was accomplished in Lowenstein-Jensen (LJ) medium and the isolates were identified by standard microbiological methods such as Ziehl-Neelson staining, morphology of colony, pigment and niacin production, nitrate and catalase tests. For susceptibility testing the proportional method was employed (12-14). The MICs of INH (0.2, 0.4, 0.8, 1.6 and 3.2 μg/ml) was determined on LJ medium for INH- resistant strains. For all experiments, M. tuberculosis HRV37 was used as standard.
DNA Extraction
For bacterial DNA extraction, the grown colonies of M. tuberculosis on LJ medium was resuspended in 300 µl TE buffer (Tris 10 mM, pH 8; EDTA 1 mM) and inactivated for 40 minutes at 80 °C. Then the DNA of isolates was extracted by SDS and proteinase-K method (4,15).
PCR-RFLP
The coding region of KatG gene was amplified by primers KatG 904: 5′-AGCTCGTATGGC ACCGGAAC3′ and KatG 1523: 5′-TTGA CCTCCCACCCGACTTG3′ as described previously (16). The PCR reactions was prepared in a 25 µl volume included 10 pM of primers (1 µl of each forward and reverse primers), 2 mM MgCl2 (1.5 µl), 0.2 mM dNTPs (0.5 µl) and 2 unit (0.25 µl) of Taq DNA polymerase (Fermentas). The PCR program was initial denaturation at 94 °C for 4 minutes followed by 35 cycles of denaturation at 94 °C for 1 min, annealing at 63 °C for 1min and extension at 72 °C for 1 min with a final extension at 72 °C for 5 min. In order to characterize the mutations in the KatG gene, the PCR products were purified with PCR product purification columns () and digested by Mspl restriction enzyme (Fermentas). Finally, the reaction mixture was electrophoresed on 1% agarose gel and visualized on UV light after staining with ethidium bromide (16,17).
Results
Totally, 50 M. tuberculosis strains were isolated from pulmonary tuberculosis patients among which 28 (56%) were males and 22 (44%) were females. The age range of patients was 23 to 63 years and the median age was 42.92 years. Out of 50 M. tuberculosis strains, 25 strains were resistant and 25 strains were found to be sensitive to INH by proportional method. We studied the INH MIC among 25 resistant isolates and we also aimed to determine the probability of relationship between MIC ranges and type of mutations in the KatG gene. According to the protocol of proportional method, strains with MIC 0.2 μg/ml and higher was considered as INH resistant. The results indicated that among 25 INH-resistant strains, the MICs were 0.4 μg/ml in one (4%) isolate, 0.8 μg/ml in one (4%) isolate, 1.6 μg/ml in 3 (12%) isolates and 3.2 μg/ml in 4 (16 %) isolates. In the remaining 16 (64%) resistant isolates, the MICs were 0.2 μg/ml. The MICs of M. tuberculosis strain HRV37 (standard strain) and all INH-sensitive isolates, were less than 0.2 μg/ml.
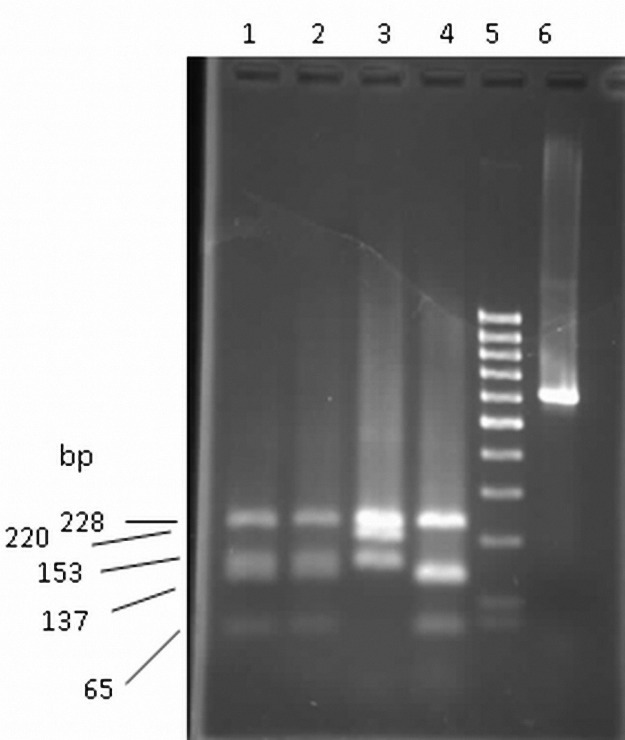
PCR amplification of KatG gene was positive in all isolates and resulted in a 620 bp product in agarose gel electrophoresis. After Msp1 digestion of KatG amplicon, four distinct RFLP patterns were observed (16) (Table and Figure 1).
Table1.
Predicted fragment sizes of Msp1 digest of KatG amplicone.
| KatG mutation | DNA fragments (bp) | |||||
|---|---|---|---|---|---|---|
| Wild type | 65 | 137 | 153 | 228 | ||
| at codon 315 (S→T) | 65 | 132 | 137 | 228 | ||
| at codon 463 (R→L) | 153 | 220 | 228 | |||
| at codons 315 and 463 | 132 | 220 | 228 | |||
Figure 1.
PCR RFLP pattern of INH-sensitive and INH-resistant M.tuberclosis isolates. Lanes 1 and 2, INH sensitive wild type; lane 3, R-463-L mutant; lane 4, S-315-T mutant isolates and lane 6, PCR amplified KatG gene before restriction digestion. Lane 5 is related a 100 bp DNA ladder.
Our findings showed that 25 INH-sensitive M. tuberculosis strains had no mutation in the KatG gene. Among 25 INH-resistant isolates, 14 strains (56%) showed mutation in the KatG315 and 5 strains (20%) showed mutation in the KatG 463 loci. Six resistant isolates (24%) had no mutation in the studied loci. Mutation in both 315 and 463 codons were not found in any isolates. M. tuberculosis strain HRV37 susceptible to all anti-tuberculosis drugs was used for quality control. This strain was negative for mutation in the KatG gene in PCR-RFLP. For confirmation of RFLP results, the PCR products from 10 stains were submitted for sequencing (MWG, ). The sequencing results were in agreement with PCR-RFLP results for both INH-resistant and INH-sensitive strains (Table 2).
Table 2.
DNA fragments sizes of PCR products after digestion with Mspl.
| Mutation | No. of strains | Fragments (bp) |
Observed phenotype | |||||
|---|---|---|---|---|---|---|---|---|
| 65 | 132 | 137 | 153 | 220 | 228 | |||
| No mutation | 31 (6 INH resistant, and 25 INH sensitive isolates) | + | + | + | + | Wild type | ||
| At codon 315 | 14 | + | + | + | + | Type 1 | ||
| At codon 463 | 5 | + | + | + | Type 2 | |||
Discussion
The spread of INH and rifampin resistant M. tuberculosis strains, which are known as MDR strains, have caused a major health problem in global community (18). Rapid detection of MDR strains would help efficient treatment of patients and prevents widespread distribution of these isolates (1-5). This study aimed to survey the use of PCR-RFLP in comparison with proportional method for rapid detection of INH resistant M. tuberculosis strains.
The resistance to INH was screened by proportional method in LJ medium and then INH MIC was determined in INH-resistant isolates. Analysis of mutation in two KatG gene loci was carried out by PCR- RFLP. The results indicated that PCR-RFLP was able to detect INH- resistance in 76% of 25 resistant strains. Mutation was identified at codon 315 in 56% of strains whereas codon 463 contained mutation in 20% of resistant strains.
Twenty five INH- sensitive M. tuberculosis strains as well as standard strain (M. tuberculosis H37RV) showed no mutation in the studied codons. These findings are consistent with some reports about the rate of mutation in the KatG gene in other parts of . Zaker Bostanabad et al (19) reported that 61% of INH-resistant M. tuberculosis isolates in the east region of contained mutation in the KatG gene. In another study carried out on the strains of Isfahan and Tehran, the mutation rate was 78% for Isfahan and 61% for Tehran (20). In other countries, the results varied in different part of the world. For instance, in Turkey, Cavusoglu et al (21) reported the mutation rate of 73% and in another study taken place in east of Turkey; the rate of mutation in the KatG was reported as 63% (22). Among countries in the southern boundary of Iran, the percentage of mutation in the KatG gene was reported 65% in Kuwait, 64% in Dubai, 35% in Beirut and 47% in Egypt (23-26). In the other countries, the mutations in the KatG have been reported as 98% in Russia, 84% in Lithonia, 71% in Vietnam, 65% in Australia, 60% in South Africa, 60% in China, 60% in Philippines, 59% in Spain, 46% in Switzerland, and 55% in India (1, 3, 21, 25,26).
In the present study, 20% of INH- resistant strains had mutation in the KatG codon 463 and no simultaneous mutation was observed in either codons 315 and 463. Zhang et al (27) reported mutation at codon 463 in 40% of INH-resistant M. tuberculosis strains. In 24% of our INH-resistant strains (6 strains) no mutation was identified in the KatG gene in the study loci. In a study in India, in 27% of 120 INH-resistant strains, no mutation was detected in the KatG gene (4). These findings show that mutations in other codons of KatG gene or mutations in other genes such as inhA, oxyR-aphC, kasA and ndh might be involved in INH-resistance in these isolates (3, 4, 8, 19, 23,25).
Analysis of INH MIC among 25 INH-resistant strains demonstrated that the MIC was 0.2 μg/ml in 16 strains, 0.4 μg/ml in one strain, 1.6 μg/ml in 3 strains, and 3.2 μg/ml in 4 strains. The results also indicated that the MIC of most strains with mutation at codon 315 was >2 μg/ml. These findings are consistent with reports on correlation of INH MIC and type of mutation in KatG gene (28-31). It has been reported that the level of INH MIC is correlated to the type and extent of changes in the KatG gene. Hass et al, (28) reported INH MIC>50 μg/ml in the strains which have lost their KatG totally on their chromosome whereas, in 83% of INH- resistant strains with mutation at codon 315, the INH MIC have been >2 μg/ml. Our findings in accordance with previous results showed that minor changes in the KatG gene were associated with decreased catalase activity and low INH MIC (28).
Conclusion
The result of this study revealed that mutation at codons 315 and 463 of KatG gene is responsible for INH resistance in 76% of M. tuberculosis strains in northwestern of . The result also indicated that PCR-RFLP method can be used for rapid diagnosis of NIH-resistant tuberculosis in most cases.
Acknowledgment
This work was supported by Tuberculosis and Lung Research Centre, Tabriz University of Medical Sciences, Tabriz, Iran
References
- 1.Simon S, Listiawan I. Drug resistance in Mycobacterium tuberculosis: a molecular perspective. J Indonesian Med Assoc. 2003;4:26–35. [Google Scholar]
- 2.Abbadi SH, Sameaa GA, Morlock G, Cooksey RC. Molecular identification of mutations associated with anti-tuberculosis drug resistance among strains of Mycobacterium tuberculosis. Int J Infect Dis. 2009;13:673–678. doi: 10.1016/j.ijid.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Abe C, Kobayashi I, Mitarai S, Wada M, Kawabe T, Takashima T, et al. Biological and molecular characteristics of Mycobacterium tuberculosis clinical isolates with low-level resistance to Isoniazid in Japan. J Clin Microbiol. 2008;46:2263–2268. doi: 10.1128/JCM.00561-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathuria JP, Nath G, Samaria JK, Anupurba S. Molecular characterization of INH-resistant Mycobacterium tuberculosis isolates by PCR-RFLP and multiplex-PCR in North India. Infect Genet Evol. 2009;9:1352–1355. doi: 10.1016/j.meegid.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Ghebremichael S, Petersson R, Koivula T, Pennhag A, Romanus V, Berggren I, et al. Molecular epidemiology of drug resistant tuberculosis in Sweden. Microbes Infect. 2008;10:699–705. doi: 10.1016/j.micinf.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Timmins GS, Deretic V. Mechanisms of action of isoniazid. Mol microbial. 2006;65:1220–1227. doi: 10.1111/j.1365-2958.2006.05467.x. [DOI] [PubMed] [Google Scholar]
- 7.Ramaswamy SV, Reich R, Dou SJ, Jasperse L, Pan X, Wanger A, et al. Single nucleotide polymorphisms in genes associated with isoniazid resistance in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2003;47:1241–12450. doi: 10.1128/AAC.47.4.1241-1250.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hristea A, Otelea D, Paraschiv S, Macri A, Baicus C, Moldovan O, et al. Detection of Mycobacterium tuberculosis resistance mutations to rifampin and isoniazid by real-time PCR. Indian J Med Microbiol. 2010;28:211–216. doi: 10.4103/0255-0857.66474. [DOI] [PubMed] [Google Scholar]
- 9.Narvskaya O, Otten T, Limeschenco E, Sapozhnikova N, Graschenkova O, Steklova L, et al. Nosocomial outbreak of multidrug-resistant tuberculosis caused by a strain of Mycobacterium tuberculosis W-Beijing family in St. Petersburg, Russia. Eur J Clin Microbiol Infect Dis. 2002;21:596–602. doi: 10.1007/s10096-002-0775-4. [DOI] [PubMed] [Google Scholar]
- 10.Kim SY, Park YJ, Kim WI, Lee SH, Chang CL, Kang SJ, et al. Molecular analysis of isoniazid resistance in Mycobacterium tuberculosis isolates recovered from South Korea. Diagn Microbiol Infect Dis. 2003;47:497–502. doi: 10.1016/s0732-8893(03)00132-9. [DOI] [PubMed] [Google Scholar]
- 11.Guo H, Seet Q, Denkin S, Parsons L, Zhang Y. Molecular characterization of isoniazid-resistant isolates of Mycobacterium tuberculosis from the USA. J Medical Microbiol. 2006;55:1527–1531. doi: 10.1099/jmm.0.46718-0. [DOI] [PubMed] [Google Scholar]
- 12.Goodwin A. Mycobacterium tuberculosis and other Nontuberculosis mycobacteria. In: Mahon CR, Lehman DC, Manuselis G, editors. Textbook of Diagnostic Microbiology. 3rd ed. New York: Saunders Elsevier; 2007. pp. 673–716. [Google Scholar]
- 13.Marttila HJ, Soini H, Huovinen P, Viljanen MK. katG mutations in isoniazid-resistant Mycobacterium tuberculosis isolates recovered from Finnish patients. Antimicrob Agents Chemother. 1996;40:2187–2189. doi: 10.1128/aac.40.9.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poojary A, Nataraj G, Kanade S, Metha P, Baveja S. Rapid antibiotic susceptibility testing of Mycobacterium tuberculosis: it's utility in resource poor settings. Indian J Med Microbiol. 2006;24:268–272. doi: 10.4103/0255-0857.29385. [DOI] [PubMed] [Google Scholar]
- 15.Murray PR, Rosenthal KS, Pfalle MA. Medical Microbilogy. 5th ed. USA: Elsevier Mosby; 2005. pp. 297–310. [Google Scholar]
- 16.Leung ET, Kam KM, Chiu A, Ho PL, Seto WH, Yuen KY, et al. Detection of KatG Ser315Thr substitution in respiratory specimens from patients with isoniasid-resistant Mycobacterium tuberculosis using PCR-RFLP. J Med Microbiol. 2003;52:999–1003. doi: 10.1099/jmm.0.05223-0. [DOI] [PubMed] [Google Scholar]
- 17.Marttila HJ, Soini H, Huovinen P, Viljanen MK. KatG mutations in isoniazid-resistant Mycobacterium tuberculosis isolates recovered from Finnish patients. Antimicrob Agents Chemother. 1996;40:2187–2189. doi: 10.1128/aac.40.9.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, Ziazarifi AH, et al. Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in iran. Chest. 2009;136:420. doi: 10.1378/chest.08-2427. [DOI] [PubMed] [Google Scholar]
- 19.Titov LP, Bahremand R. Frequency and molecular characterization of isoniazid resistance in the KatG region of MDR isolates from tuberculosis patients in southern endemic border of Iran. Infect Genet Evol. 2008;8:15–29. doi: 10.1016/j.meegid.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Mohajeri P, Tavakoli A, Moghim S. Detection of mutation at codon 315 KatG gene as a gene marker associated with isoniazid resistance, in Mycobacterium tuberculosis strains isolated from patients in Isfahan and Tehran by PCR-RFLP method. J Zanjan Unive Med Sci Health Services. 2009;17:29–40. [Google Scholar]
- 21.Cavusoglu C, Turhan A, Akinci P, Soyler I. Evaluation of the Genotype MTBDR assay for rapid detection of rifampin and isoniazid resistance in Mycobacterium tuberculosis isolates. J Clin Microbiol. 2006;44:2338–2342. doi: 10.1128/JCM.00425-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aktas E, Durmaz R, Yang D, Yang Z. Molecular characterization of isoniazid and rifampin resistance of Mycobacterium tuberculosis clinical isolates from Malatya, Turkey. Microb Drug Resist. 2005;11:94–99. doi: 10.1089/mdr.2005.11.94. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad S, Mokaddas E. Contribution of AGC to ACC and other mutations at codon 315 of the katG gene in isoniazid-resistant Mycobacterium tuberculosis isolates from the Middle East. Int J Antimicrob Agents. 2004;23:473–479. doi: 10.1016/j.ijantimicag.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Ahmad S, Fares E, Araj GF, Chaugh TD, Mustafa AS. Prevalence of S315T mutation within the KatG gene in isoniazid-resistant clinical Mycobacterium tuberculosis isolates from Dubai and Beirut. Int J Tuberc Lung Dis. 2002;6:920–926. [PubMed] [Google Scholar]
- 25.Valvatne H, Syre H, Kross M, Phyu S, Grewal M. Isoniazid and rifampicin resistance-associated mutations in Mycobacterium tuberculosis isolates from Yangon, Myanmar: implications for rapid molecular testing. J Antimicrob Chemother. 2009;64:694. doi: 10.1093/jac/dkp292. [DOI] [PubMed] [Google Scholar]
- 26.Musser JM. Antimicrobial agent resistance in mycobacteria: molecular genetic insights. Clin Microbiol Rev. 1995;8:496–514. doi: 10.1128/cmr.8.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang M, Yue J, Yang Y, Zhang H, Lei J, Jin R, Zhang X, et al. Detection of mutation associated with Isoniazid resistance in Mycobacterium tuberculosis isolates from China. J Clin Microbiol. 2005;43:5477–82. doi: 10.1128/JCM.43.11.5477-5482.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haas WH, Schilke K, Brand J, Amthor B, Weyer K, Fourie PB, et al. Molecular analysis of KatG gene mutations in strains of Mycobacterium tuberculosis complex from Africa. J Antimicrob Chemother. 1997;41:1601–1603. doi: 10.1128/aac.41.7.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Telenti A, Honoreacute N, Bernasconi C, March J, Ortega A, Heym B, et al. Genotypic assessment of isoniazid and rifampin resistance in Mycobacterium tuberculosis: a blind study at reference laboratory level. J Clin Microbiol. 1997;35:719–23. doi: 10.1128/jcm.35.3.719-723.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuijper E, Rinder H, Borgdorff MW. Mutations at amino acid position 315 of the KatG gene are associated with high-level resistance to isoniazid, other drug resistance, and successful transmission of Mycobacterium tuberculosis in the Netherlands. J Infect Dis. 2000;182:1788–1790. doi: 10.1086/317598. [DOI] [PubMed] [Google Scholar]