Abstract
Background
Social cohesion, the self-reported trust and connectedness between neighbors, may affect health behaviors via psychosocial mechanisms.
Purpose
Relations between individual perceptions of social cohesion and smoking cessation were examined among 397 Black treatment-seeking smokers.
Methods
Continuation ratio logit models examined the relation of social cohesion and biochemically-verified continuous smoking abstinence through 6 months post-quit. Indirect effects were examined in single mediator models using a nonparametric bootstrapping procedure. All analyses controlled for sociodemographics, tobacco dependence, and treatment.
Results
The total effect of social cohesion on continuous abstinence was non-significant (β=.05, p=.10). However, social cohesion was associated with social support, positive affect negative affect, and stress, which, in turn, were each associated with abstinence in adjusted models (ps<.05).
Conclusions
Results suggest that social cohesion may facilitate smoking cessation among Black smokers through desirable effects on psychosocial mechanisms that can result from living in a community with strong interpersonal connections.
Keywords: social cohesion, neighborhood trust, smoking cessation, mediation
Introduction
Smoking is the leading cause of preventable death and disability in the United States and is causally implicated in several cardiovascular diseases and at least 15 different cancers (1). However, the negative health effects of smoking are not equally distributed across all societal groups. For example, despite the later initiation of smoking and the consumption of fewer cigarettes per day than Whites, Black smokers are at significantly greater risk for the development of several smoking-related diseases, and are more likely to die from these diseases, than Whites (2). Moreover, some research suggests that Black smokers may be less likely to successfully quit smoking as compared to White smokers (3, 4). Investigating the determinants of smoking cessation among Black smokers is important to increase understanding about how to best intervene to increase smoking cessation rates among this group, and ultimately, to eliminate smoking-related health disparities.
Recently, there has been an increased focus on enhancing our understanding of the social-contextual determinants of health-related behaviors, including smoking. One construct of interest in these studies has been social cohesion. Social cohesion refers to the self-reported trust and connectedness between neighbors, including perceptions of community belonging, shared community values, and the availability of aid from neighbors (5). Social cohesion is thought to provide a protective influence on health and have a positive effect on health-related behaviors via the rapid dissemination of health-related information, the promulgation of community norms for healthy behaviors, the collective power to advocate for health-promoting community changes, or through positive effects on psychosocial mechanisms that come from living in a community with strong interpersonal connections (6, 7). Cross-sectional, population-based research has previously examined the relationship between social cohesion and smoking behaviors. These studies indicate significant and inverse associations between social cohesion and the likelihood of being a smoker (6, 7), as well as the number of cigarettes smoked per day among smokers (8). However, to our knowledge, no previous research has examined how individual perceptions of social cohesion might be prospectively associated with smoking cessation during a specific quit attempt.
A greater understanding of the effects of social cohesion on smoking behaviors, including smoking cessation, can be gained from longitudinal research that is focused on the mechanisms underlying these relationships. Currently, no empirical studies directly inform this area of the literature. However, schematic models of the social-contextual determinants of health and health-related behaviors highlight the importance of psychosocial mechanisms (e.g., stress) in these relationships (9). Supporting such models are empirical studies citing inverse relations between social cohesion (both when conceptualized as an individual-level variable as well as when aggregated to the neighborhood level) and psychosocial mechanisms underlying health-related behaviors, including psychological distress (10), negative affect (7, 11, 12), and stress (13). Similarly, research supports positive associations between social cohesion and social support (13). These psychosocial variables, as well as others (e.g., positive affect) have been cited as key determinants of smoking relapse in prominent models of addiction [e.g., relapse prevention (14–16)], and have been empirically associated with smoking cessation in prior research (17–31). For example, elevated stress and negative affect are important precipitants of smoking relapse (25, 26). On the other hand, higher reported social support and greater positive affect seem to play a protective role against smoking relapse (20, 32). Thus, if there is an association between social cohesion and smoking cessation, theory and research support that these psychosocial variables may be particularly relevant factors to explore as potential mediators.
Previous studies have suggested that race/ethnicity might moderate relationships between social cohesion and health-related behaviors (7), but studies examining these relations often lack sufficient power to detect racial/ethnic interaction effects (7). Thus, barring adequate samples to test for such interactions, research in this area may be best conducted within racial/ethnic groups so as to mitigate the influence of potential confounders. Because of the aforementioned burden of tobacco-related disease and death among Blacks, and because a better understanding of the determinants of smoking cessation is needed to facilitate interventions for this underserved population, research on the relations of social cohesion and smoking cessation among Black smokers is particularly important. Moreover, the proposed psychosocial mediators are culturally relevant to Black smokers. For example, research suggests that Blacks may experience greater stress than Whites, at least partially due to experiences of racism and discrimination, and that Blacks may also be more likely to smoke in response to stress than Whites [for summary see (33)]. This may especially be the case for Black smokers of lower socioeconomic status (33). Likewise, Blacks may be more likely than Whites to report negative affect (34) [at least in early adulthood (35)], potentially as a result of enduring relatively more adversities, including those associated with living in economically deprived or dangerous neighborhoods where trust between neighbors may be low.
The purpose of this study was to address current gaps in the literature by examining whether individual perceptions of social cohesion were associated with smoking cessation during a specific quit attempt, and exploring potential psychosocial mechanisms that could account for an indirect effect. We examine these issues among a treatment-seeking sample of low income Black adult smokers who were enrolled in a larger clinical trial. We hypothesized that greater social cohesion would be associated with higher odds of abstinence during a specific quit attempt, and that these relations would be accounted for (at least partially) by the associations of greater social cohesion with greater social support, less negative affect, greater positive affect, and less stress.
Methods
Participants and Procedures
Data were collected as part of a randomized clinical trial designed to determine the efficacy of a smoking cessation intervention designed for Black smokers (36). Individuals were proactively recruited from Houston, Texas using newspaper advertisements. They were eligible to participate if they self-identified as Black, were between the ages of 21 and 65, smoked five or more cigarettes per day for ≥12 months, produced expired carbon monoxide levels of ≥8 parts per million, were willing to quit smoking within the next 2 weeks, possessed a functioning home telephone number, had a permanent home address, and were able to understand English at a 6th grade literacy level. Individuals were excluded if they reported regular use of tobacco products other than cigarettes, were using pharmacological smoking cessation treatments at the time of enrollment, reported medical contraindications to the nicotine patch (i.e., a history of heart attacks, angina, cardiac arrhythmia, or blood circulation problem), or were pregnant or lactating.
Participants were enrolled between 2005 and 2006, and data collection concluded in 2007. Following an eligibility phone screen, data were collected during 7 in-person study visits, not all of which were relevant to the current study: Pre-Quit Day -19 (i.e., 19 days before the quit date), Pre-Quit Day -12, Pre-Quit Day -5, Post-Quit Day 3 (i.e., 3 days following the quit date), Post-Quit Day 10, Post-Quit Day 31, and Post-Quit Month 6. See Figure 1. Participants were compensated $20 for each of the first 5 visits, and $40 for each of the last 2 visits to encourage attendance. All study procedures were approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center, and written informed consent was obtained from all participants. Participant recruitment and flow through the study are reported elsewhere (36, 37).
Figure 1.
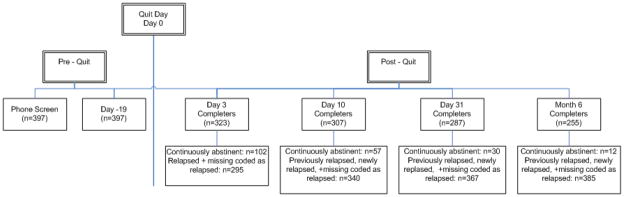
Timeline for the current study with detailed abstinence data.
Note: Continuous abstinence data at all Post-Quit study visits were used in analyses. Tobacco dependence variables were collected at the phone screen, sociodemographics and social cohesion were collected at Day -19, and psychosocial mediator data were collected at the Day 3 visit.
Participants were randomized to standard treatment or standard treatment plus computer delivered treatment following the Day -19 study visit. Standard treatment consisted of self-help materials, five cessation counseling sessions, and four weeks of nicotine replacement therapy (the patch). Participants in standard treatment plus computer delivered treatment also had access to six weeks of computer-based intervention via a palmtop computer. In addition, the computer delivered treatment included a personalized plan for quitting and culturally targeted motivational messages.
Variables of Interest and Manner of Collection
Participants viewed questionnaire items on a computer screen while listening to them on earphones and entered responses directly into the computer through the keyboard.
Sociodemographics
Sociodemographics were collected at Pre-Quit Day -19 and included age, gender, total annual household income, educational level, employment status, and partner status. Sociodemographics were included as covariates in analyses due to known associations with the variables of interest. Only income had substantial missingness (82 missing).
Tobacco Dependence
Tobacco dependence was assessed using the Heaviness of Smoking Index, which was calculated from information collected at the phone screen regarding the number of cigarettes smoked per day before the quit attempt and the time to the first cigarette of the day. (38) The Heaviness of Smoking Index was included as a covariate in analyses due to known associations with quitting behavior. (39)
Social Cohesion
Social Cohesion, collected at Pre-Quit Day -19, is a 5-item measure assessing participant’s beliefs about their neighbors’ willingness to help, trustworthiness, shared values, etc. (5). Participants are asked to indicate the degree to which they agree or disagree with each item on a 5-point scale ranging from strongly disagree to strongly agree. Responses are reversed coded where indicated, and summed to create a total score. Higher scores suggest greater social cohesion and trust. Social Cohesion has adequate reliability and validity as a measure of perceived trust and connectedness with neighbors [see (10, 40, 41)]. The coefficient alpha for Social Cohesion in this sample was 0.73.
Psychosocial Mediators
Four psychosocial variables, collected at Post-Quit Day 3, were examined as potential mediators of the relationship between social cohesion and smoking abstinence. General Social Support was measured by the total score on the 12-item version of the Interpersonal Support Evaluation List-12 (42, 43). Each item is rated on a 4-point scale and summed for a total score, with higher scores representing greater perceived support. The coefficient alpha for the Interpersonal Support Evaluation List-12 in this sample was 0.82. Positive and Negative Affect were measured with the 20-item Positive and Negative Affect Scale (44), forming Positive Affect and Negative Affect subscales. Each item is rated on a 5-point scale and responses are summed for a total score, with higher scores indicating greater positive and negative affect, respectively. The coefficient alphas for the Positive Affect and Negative Affect subscales were each 0.93. Stress was measured with the 4-item Perceived Stress Scale (45), which was designed to assess the degree to which respondents find their lives to be stressful. Each item is rated on a 5-point scale and responses are summed for a total score, with higher scores indicating greater perceived stress. The coefficient alpha for the Perceived Stress Scale in this sample was 0.77.
Smoking Abstinence
Continuous abstinence from smoking was defined as a self-report of no cigarettes smoked since the quit date (not even a puff) and an expired carbon monoxide level of <10 parts per million or a cotinine value of < 20 ng/ml. Smoking status was assessed at Post-Quit Day 3, Day 10, Day 31, and Month 6. Relapse at any of these data collections resulted in classification as relapsed from that point forward. Accounting for relapse in this manner, data were available to determine abstinence status for 84% of participants at Day 10, 84% of participants at Day 31, and 86.2% of participants at Month 6. Any missing data resulting from study visit no shows were handled by coding the participant as relapsed from that point forward.
Data Analysis
The total effect of social cohesion on abstinence from smoking through Post-Quit Month 6 was assessed in SAS version 9.1 (SAS Institute, Cary, NC) using continuation ratio logit models [PROC GENMOD; (46–48)]. Due to the minimal level of residential clustering in our database by Census block group (i.e., neighborhood proxy) and potential numerical instability in estimating certain within-block-group correlation structures, we treated all observations as independent in our analyses (49). Next, social support, positive affect, negative affect, and stress were examined as mediators of the relationship between social cohesion and continuous smoking abstinence in R version 2.11.2 (50) using a nonparametric bootstrapping procedure. This procedure generates an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect path with the use of 5,000 resamples with replacement from the dataset (51). Each potential mediator was assessed in a single mediator model. The proportion of the mediated effect was estimated using PME = ab/(c′+ab) (52). Finally, secondary analyses were conducted to determine whether results were resilient to the inclusion of the 82 participants with missing income. This was accomplished using an indicator variable for missing income data and re-running analyses. All analyses specified above controlled for sociodemographics, tobacco dependence, time, and treatment group.
Results
Of the 399 trial participants, 397 provided data on social cohesion and were available for inclusion in analyses. Participant characteristics are shown in Table 1. The sample was roughly evenly split by gender and was largely low income, with over three quarters reporting less than $30,000 in annual household income. In addition, more than three quarters of the sample were single, divorced, or widowed. On average, participants smoked 20.6 (±12.2) cigarettes per day prior to the quit attempt, and 59.7% of participants smoked their first cigarette within 5 minutes of waking. Figure 1 presents the study timeline with detailed abstinence data. Of the 397 participants, 26% were biochemically verified continuously abstinent through Post-Quit Day 3. Continuous abstinence rates decreased to 14% of participants through Post-Quit Day 10, 8% through Post-Quit Day 31, and 3% through Post-Quit Month 6. Univariate analyses indicated that participants who were older, employed, earning more than $10,000 in annual household income, and less dependent on tobacco were more likely to maintain continuous smoking abstinence through Post-Quit Month 6 relative to those who were younger, unemployed, earning less than $10,000 a year, and more dependent on tobacco (ps < .01). Similar results linking unemployment and low income to smoking relapse during a specific quit attempt have been reported previously (e.g., see 22), and the current results suggest that socioeconomic status remains an important factor even among very low income samples of Black smokers.
Table 1.
Participant Characteristics and Their Interrelations
| Participant Characteristics | Mean (SD)/Percentage | n | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age (years) | 42.4 (±9.7) | 397 | 1.00 | |||||||||||
| 2. Gender | −.05 | 1.00 | ||||||||||||
| Female | 50.9 | 202 | ||||||||||||
| Male (REF) | 49.1 | 195 | ||||||||||||
| 3. Total Annual Household Income | −.06 | 0.06 | 1.00 | |||||||||||
| < $10,000 (REF) | 48.3 | 152 | ||||||||||||
| $10,000 – $29,999 | 31.4 | 99 | ||||||||||||
| ≥ $30,000 | 20.3 | 64 | ||||||||||||
| 4. Educational Level | .08 | .14* | .33*** | 1.00 | ||||||||||
| < High School (REF) | 17.9 | 71 | ||||||||||||
| High School degree/Some College | 60.2 | 239 | ||||||||||||
| ≥ College degree | 21.9 | 87 | ||||||||||||
| 5. Employment Status | −.05 | .01 | .40*** | .27*** | 1.00 | |||||||||
| Employed | 39.3 | 153 | ||||||||||||
| Unemployed (REF) | 60.7 | 236 | ||||||||||||
| 6. Partner Status | .06 | .05 | .31*** | .06 | .05 | 1.00 | ||||||||
| Single/Widowed/Divorced (REF) | 78.3 | 306 | ||||||||||||
| Married/Living with Partner | 21.7 | 85 | ||||||||||||
| 7. Heaviness of Smoking Index | 3.5 (±1.4) | 392 | .04 | −.02 | −.09 | −.11* | −.07 | −.02 | 1.00 | |||||
| 8. Social Cohesion (range 5–25) | 15.8 (± 3.7) | 397 | .16** | −.06 | .26*** | .16** | .13* | .11* | .16** | 1.00 | ||||
| 9. Social Support (range 18–48) | 38.5 (±6.5) | 317 | −.10 | .02 | .28*** | .15** | .21*** | .05 | −.11 | .23*** | 1.00 | |||
| 10. Negative Affect (range 10–50) | 19.5 (±8.9) | 319 | −.07 | .08 | −.23*** | −.08 | −.16** | −.05 | .15** | −.27*** | −.46*** | 1.00 | ||
| 11. Positive Affect (range 15–50) | 35.8 (±8.8) | 319 | .01 | −.11 | .13* | .11* | .11 | −.05 | −.06 | .20*** | .43*** | −.47*** | 1.00 | |
| 12. Stress (range 0–15) | 5.4 (±3.3) | 318 | −.10 | .04 | −.20** | −.13* | −.14* | −.07 | .10 | −.27*** | −.51*** | .67*** | −.71*** | 1.00 |
Note:
p<.05;
p< .01;
p< .001. Interrelations between participant characteristics were evaluated using Pearson correlations for continuous-continuous variable associations, Point-biserial correlations for continuous-binary associations, Spearman correlations for continuous-categorical associations, Phi coefficients for binary-binary associations, and Contingency coefficients for categorical-categorical associations.
Social Support = Interpersonal Support Evaluation List-12; Negative Affect = Positive and Negative Affect Scale, Negative Affect subscale; Positive Affect = Positive and Negative Affect Scale, Positive Affect subscale; Stress = Perceived Stress Scale. REF= Reference group.
There was a positive association between social cohesion and the likelihood of continuous smoking abstinence in adjusted analyses, but the total effect did not reach the threshold for statistical significance [β = .05, SE = .03; χ2 (1) = 2.76; p=.10]. However, adjusted simple mediation analyses yielded significant indirect effects for social support, negative affect, positive affect, and stress in the relation between social cohesion and continuous smoking abstinence through Post-Quit Month 6 (ps < .05; Table 2). Specifically, social support and positive affect were positively associated with social cohesion and abstinence, whereas negative affect and stress were negatively associated with social cohesion and abstinence. This pattern of results was unchanged when missing income data were handled via an indicator variable (results available upon request).
Table 2.
Significance Testing of the Indirect Effect of Social Cohesion on Continuous Smoking Abstinence through Post-Quit Month 6 via Psychosocial Mediators
| Mediator | βapath | βbpath | Estimate of the Indirect Effect | BC 95% CI | PME | p | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | SD | Lower | Upper | |||||
| Social Support | 0.279 | 0.065 | 0.018 | 0.009 | 0.006 | 0.000 | 0.024 | 0.553 | <.05 |
| Negative Affect | −0.514 | −0.039 | 0.020 | 0.010 | 0.007 | 0.001 | 0.027 | 0.703 | <.05 |
| Positive Affect | 0.371 | 0.036 | 0.013 | 0.007 | 0.005 | 0.000 | 0.018 | 0.469 | <.05 |
| Stress | −0.166 | −0.123 | 0.021 | 0.010 | 0.006 | 0.002 | 0.026 | 0.753 | <.05 |
Note: Effects were tested in a series of single mediator models. βapath = Estimate of the effect between social cohesion and the mediator. βbpath = Estimate of the effect between the mediator and continuous smoking abstinence through Post-Quit Month 6. 1 = The unstandardized indirect effect estimates in the sample. 2 = The standardized indirect effect estimates in the sample. SD = The standard deviation of the standardized indirect effect. BC 95% CI = Bias corrected 95% confidence interval. PME = Proportion of the Mediated Effect. Social Support = Interpersonal Support Evaluation List-12; Negative Affect = Positive and Negative Affect Scale, Negative Affect subscale; Positive Affect = Positive and Negative Affect Scale, Positive Affect subscale; Stress = Perceived Stress Scale. All analyses were adjusted for age, gender, total annual household income, educational level, employment status, partner status, tobacco dependence, time, and treatment group.
Conclusions
This study was the first to examine the prospective relations of social cohesion and smoking cessation during a specific quit attempt, and to characterize psychosocial mechanisms that could account for that relationship, among Black adults. Although the total effect of social cohesion on continuous smoking abstinence was non-significant, the significant indirect effects through social support, affect, and stress are potentially important [cf. (53)]. Results indicated that social support and positive affect were positively associated with social cohesion and abstinence, whereas negative affect and stress were negatively associated with social cohesion and abstinence. It is possible that social cohesion, or the trust and connectedness one perceives with their neighbors, results in heightened perceptions of safety and security, which may positively affect psychosocial mechanisms, and ultimately facilitate smoking cessation. If so, interventions designed to increase community trust, and policies aimed at increasing the perceptions of social cohesiveness with neighbors may facilitate smoking cessation through effects on social support, affect and stress. Social cohesion may be built for example, through the organization of community events and through participation in group activities, which help to build community capacity and develop networks of support among neighbors. Literature supports that such interventions can affect community engagement among Black populations (54).
Results suggest potential benefits to the provision of smoking cessation interventions within communities, in a format that would allow neighbors to interact and support one another. For example, group-based cessation services might be provided in neighborhood community centers or within other important community gathering places like churches in order to facilitate community engagement. Previous research has supported the effectiveness of cessation interventions provided in such settings [e.g., churches; (55)], but additional research is needed to understand how such interventions might affect perceptions of social cohesion among smokers.
The psychosocial mediators examined in this study singularly accounted for between 47% and 75% of the mediated effect of social cohesion on smoking abstinence. Results complement the broader literature suggesting that stress and negative affect may be particularly relevant psychosocial mediators to explain health outcomes among Black adults (cf. 33–35), and add new knowledge regarding the particular mechanisms linking social cohesion to smoking cessation.
Contrary to our hypothesis, social cohesion was not significantly associated with a higher likelihood of continuous abstinence through six months following the quit date, over and above the effects of age, gender, partner status, socioeconomic status, and tobacco dependence. Prior studies have linked social cohesion to smoking prevalence (6, 7) and smoking rate (8), but the current results suggest relations do not extend to smoking cessation among Black treatment-seeking smokers. The low rate of continuous abstinence by Post-Quit Month 6 (3%) may have contributed to the non-significant relation with social cohesion in this sample; however, post-hoc analyses predicting short-term smoking abstinence (though Post-Quit Day 31) yielded virtually identical results (i.e., non-significant total effect but significant indirect effects). Similar findings were recently reported with regard to null associations of neighborhood collective efficacy (i.e., neighborhood-level social cohesion and social control) with smoking cessation (55). However, similar constructs (e.g., interpersonal trust, social participation) have been associated with smoking cessation in the literature (56). In general, mixed results in this emerging area suggest that additional research is needed to better understand how perceptions of social cohesion might be related to smoking cessation, and the potential implications of those relations for informing interventions to reduce smoking rates.
This study had several limitations. Most notably, although we hypothesized that individual perceptions of social cohesion influenced the proposed psychosocial mechanisms, an equally plausible explanation might be that the psychosocial variables influenced social cohesion. That is, there is a real possibility of same-source bias in our data that calls the legitimacy of the proposed meditational relationship into question. The longitudinal design of our study, while a strength, does not mitigate this possibility. Some previous studies have aggregated individual perceptions of social cohesion to the neighborhood level to help account for potential biases in self-reported data. Our data, however, were not ideal for aggregation because our participants were not randomly selected within neighborhoods, neighborhoods were not randomly sampled, and participants were unevenly distributed between neighborhoods. It is also worth noting that this study examined only four of a myriad of possible mediators of the relations between social cohesion and smoking abstinence. Other potential mediators (e.g., social norms, discrimination) should be examined in future research. Also, detailed health status information (e.g., presence of chronic health conditions, medication usage) was not collected in this study. Future studies should include these data given their potential relations with smoking behaviors and cessation.
Additional limitations include that participants were self-selected, treatment seeking Black smokers from a major metropolitan area in Texas. Self-selected, treatment seeking smokers may differ from smokers who attempt to quit without treatment in important ways, and the influence of social cohesion on cessation among the latter group remains unknown. Moreover, this study was focused on Black smokers, and results may not generalize to smokers of other race/ethnicities. Likewise, our findings may not generalize to smokers living in rural areas, or to other metropolitan areas, which may differ from the current study setting in important ways.
Finally, this study focused on continuous abstinence since the quit date. This is a conservative outcome that does not account for recovery from smoking lapses or a reduction in smoking rate over time. The relation of social cohesion with these factors has not been previously studied, but can be a focus of future research. In addition, rates of continuous smoking abstinence over time in this sample were quite low. This is a major limitation of our study, and likely reflective of the myriad challenges that low income Black smokers face in maintaining longer-term abstinence. Although smoking tends to be concentrated among those of lower socioeconomic status, it is important to note that the relations reported herein may not generalize to Black smokers of higher socioeconomic status who are attempting to quit.
Acknowledgments
Financial support: This research was supported by the National Cancer Institute (R01CA094826 and R25CA57730), the Centers for Disease Control and Prevention (K01DP001120), and the American Cancer Society (MRSGT-10-104-01-CPHPS), the National Institute for Minority Health and Health Disparities (P60MD003422) and the National Institutes of Health through MD Anderson’s Cancer Center Support Grant (CA016672). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
We would like to acknowledge the research staff at The University of Texas MD Anderson Cancer Center who assisted with implementation of the original project. We would also like to thank Ms. Lingyun Ji for her assistance with statistical analysis and for her recommendations on the handling of missing data. We also appreciate the contribution of Mr. Adolfo Cuevas regarding the cultural implications of our work.
Footnotes
Conflict of Interest Statement: Dr. Paul M. Cinciripini has served on the scientific advisory board of Pfizer Pharmaceuticals, has received grant support from Pfizer, and has conducted educational talks sponsored by Pfizer. All other authors declare no conflicts of interest.
References
- 1.ACS. Cancer facts and figures 2009. Altanta, GA: American Cancer Society; 2009. [Google Scholar]
- 2.Vidrine JI, Reitzel LR, Wetter DW. Smoking and health disparities. Current Cardiovascular Risk Reports. 2009;3:403–408. [Google Scholar]
- 3.Fu SS, Kodl MM, Joseph AM, et al. Racial/Ethnic disparities in the use of nicotine replacement therapy and quit ratios in lifetime smokers ages 25 to 44 years. Cancer Epidemiol Biomarkers Prev. 2008;17:1640–1647. doi: 10.1158/1055-9965.EPI-07-2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105(Suppl 1):75–83. doi: 10.1111/j.1360-0443.2010.03200.x. [DOI] [PubMed] [Google Scholar]
- 5.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 6.Patterson JM, Eberly LE, Ding Y, Hargreaves M. Associations of smoking prevalence with individual and area level social cohesion. Journal of Epidemiology and Community Health. 2004;58:692–697. doi: 10.1136/jech.2003.009167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Echeverria S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The Multi-ethnic Study of Atheroschlerosis. Health & Place. 2008;14:853–865. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Sapag JC, Poblete FC, Eicher C, et al. Tobacco smoking in urban neighborhoods: exploring social capital as a protective factor in Santiago, Chile. Nicotine Tob Res. 2010;12:927–936. doi: 10.1093/ntr/ntq117. [DOI] [PubMed] [Google Scholar]
- 9.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 10.Rios R, Aiken LS, Zautra AJ. Neighborhood Contexts and the Mediating Role of Neighborhood Social Cohesion on Health and Psychological Distress Among Hispanic and Non-Hispanic Residents. Ann Behav Med. 2011 doi: 10.1007/s12160-011-9306-9. [DOI] [PubMed] [Google Scholar]
- 11.Ahern J, Galea S. Collective Efficacy and Major Depression in Urban Neighborhoods. Am J Epidemiol. 2011 doi: 10.1093/aje/kwr030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mair C, Diez Roux A, Shen M, et al. Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the Multiethnic Study of Atherosclerosis. Ann Epidemiol. 2009;19:49–57. doi: 10.1016/j.annepidem.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young AF, Russell A, Powers JR. The sense of belonging to a neighborhood: Can it be measured and is it related to health and well-being in older women? Social Science & Medicine. 2004;59:2627–2637. doi: 10.1016/j.socscimed.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Marlatt G, Donovan D, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2. New York: Guilford Press; 2005. [Google Scholar]
- 15.Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am Psychol. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- 16.Niaura R. Cognitive social learning and related perspectives on drug craving. Addiction. 2000;95(Suppl 2):S155–163. doi: 10.1080/09652140050111726. [DOI] [PubMed] [Google Scholar]
- 17.Fang WL, Goldstein AO, Butzen AY, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. J Am Board Fam Pract. 2004;17:264–275. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- 18.Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: how important are household factors? Addiction. 2004;99:770–777. doi: 10.1111/j.1360-0443.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- 19.Lindstrom M, Isacsson SO, Elmstahl S. Impact of different aspects of social participation and social capital on smoking cessation among daily smokers: a longitudinal study. Tob Control. 2003;12:274–281. doi: 10.1136/tc.12.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mermelstein R, Cohen S, Lichtenstein E, Baer JS, Kamarck T. Social support and smoking cessation and maintenance. Journal of Consulting and Clinical Psychology. 1986;54:447–453. doi: 10.1037//0022-006x.54.4.447. [DOI] [PubMed] [Google Scholar]
- 21.Gulliver SB, Hughes JR, Solomon LJ, Dey AN. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90:767–772. doi: 10.1046/j.1360-0443.1995.9067673.x. [DOI] [PubMed] [Google Scholar]
- 22.Businelle MS, Kendzor DE, Reitzel LR, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychol. 2010;29:262–273. doi: 10.1037/a0019285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brandon TH. Negative affect as motivation to smoke. Current Directions in Psychological Science. 1994;3:33–37. [Google Scholar]
- 24.Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- 25.Shiffman S, Waters AJ. Negative affect and smoking lapses: a prospective analysis. J Consult Clin Psychol. 2004;72:192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- 26.Kenford SL, Smith SS, Wetter DW, et al. Predicting relapse back to smoking: contrasting affective and physical models of dependence. J Consult Clin Psychol. 2002;70:216–227. [PubMed] [Google Scholar]
- 27.Borland R. Slip-ups and relapse in attempts to quit smoking. Addict Behav. 1990;15:235–245. doi: 10.1016/0306-4603(90)90066-7. [DOI] [PubMed] [Google Scholar]
- 28.Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–185. [PubMed] [Google Scholar]
- 29.Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA. 1990;264:1546–1549. [PubMed] [Google Scholar]
- 30.Covey LS. Tobacco cessation among patients with depression. Prim Care. 1999;26:691–706. doi: 10.1016/s0095-4543(05)70124-x. [DOI] [PubMed] [Google Scholar]
- 31.Swan GE, Denk CE, Parker SD, et al. Risk factors for late relapse in male and female ex-smokers. Addict Behav. 1988;13:253–266. doi: 10.1016/0306-4603(88)90052-4. [DOI] [PubMed] [Google Scholar]
- 32.Reitzel LR, Mazas CA, Cofta-Woerpel L, et al. Subjective social status affects smoking abstinence during acute withdrawal through affective mediators. Addiction. 2010;105:928–936. doi: 10.1111/j.1360-0443.2009.02875.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernander AF, Patten CA, Schroeder DR, et al. Exploring the association of John Henry active coping and education on smoking behavior and nicotine dependence among Blacks in the USA. Soc Sci Med. 2005;60:491–500. doi: 10.1016/j.socscimed.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 34.George LK, Lynch SM. Race differences in depressive symptoms: a dynamic perspective on stress exposure and vulnerability. J Health Soc Behav. 2003;44:353–369. [PubMed] [Google Scholar]
- 35.Walsemann KM, Gee GC, Geronimus AT. Ethnic differences in trajectories of depressive symptoms: disadvantage in family background, high school experiences, and adult characteristics. J Health Soc Behav. 2009;50:82–98. doi: 10.1177/002214650905000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazas CA, Cofta-Woerpel L, Costello TJ, et al. A randomized clinical trial of a palmtop computer delivered treatment for smoking cessation among. African-American smokers. under review. [Google Scholar]
- 37.Kendzor DE, Cofta-Woerpel LM, Mazas CA, et al. Socioeconomic status, negative affect, and modifiable cancer risk factors in African-American smokers. Cancer Epidemiol Biomarkers Prev. 2008;17:2546–2554. doi: 10.1158/1055-9965.EPI-08-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 39.Borland R, Yong HH, O’Connor RJ, Hyland A, Thompson ME. The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine Tob Res. 2010;12(Suppl):S45–50. doi: 10.1093/ntr/ntq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lochner K, Kawachi I, Kennedy BP. Social capital: A guide to its measurement. Health & Place. 1999;5:259–270. doi: 10.1016/s1353-8292(99)00016-7. [DOI] [PubMed] [Google Scholar]
- 41.Echeverria SE, Diez-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81:682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brummett BH, Babyak MA, Siegler IC, et al. Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychol. 2006;25:220–225. doi: 10.1037/0278-6133.25.2.220. [DOI] [PubMed] [Google Scholar]
- 43.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Saranson IG, Saranson B, editors. Social Support: Theory, Research, and Applications. The Hague, Holland: Martines Niijhoff; 1985. [Google Scholar]
- 44.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 45.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 46.Agresti A. Categorical Data Analysis. 2. Hoboken, New Jersey: John Wiley & Sons, Inc; 2002. [Google Scholar]
- 47.Bender R, Benner A. Calculating Ordinal Regression Models in SAS and S-Plus. Biometrical Journal. 2000;42 [Google Scholar]
- 48.McGowan MJ. Ordinal Outcomes with the Continuation Ratio Model. Proceedings of the Northeast SAS Users Group Conference; 2000. [Google Scholar]
- 49.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- 50.Gentleman R, Ihaka R, Bates D, et al. The R Project for Statistical Computing. Retrieved Accessed on September 24, 2010 from http://www.r-project.org/index.html.
- 51.MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychol. 2008;27:S99–S100. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint effect in logistic and probit regression. Clin Trials. 2007;4:499–513. doi: 10.1177/1740774507083434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhou X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37 [Google Scholar]
- 54.Chung B, Jones L, Jones A, et al. Using community arts events to enhance collective efficacy and community engagement to address depression in an African American community. Am J Public Health. 2009;99:237–244. doi: 10.2105/AJPH.2008.141408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karasek D, Ahern J, Galea S. Social norms, collective efficacy, and smoking cessation in urban neighborhoods. Am J Public Health. 2012;102:343–351. doi: 10.2105/AJPH.2011.300364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Giordano GN, Lindstrom M. The impact of social capital on changes in smoking behaviour: a longitudinal cohort study. Eur J Public Health. 2011;21:347–354. doi: 10.1093/eurpub/ckq048. [DOI] [PubMed] [Google Scholar]


