Abstract
Self-esteem and self-efficacy are theorized to serve as mediators of the relationship between religious involvement and health outcomes. Studies confirming these relationships have produced mixed evidence. This study examined whether self-esteem and self-efficacy mediate the relationship between religious involvement (beliefs, behaviors) and a set of modifiable health behaviors in a national probability sample of African Americans. African Americans, in general, are relatively high in religious involvement and have higher than average rates of chronic disease. Participants were interviewed by telephone, and a Religion-Health Mediational Model was tested using structural equation modeling. Results suggest that self-esteem and self-efficacy at least in part mediate the relationship between religious beliefs (e.g., relationship with God) and greater fruit and vegetable consumption, and lower alcohol consumption. Religious behaviors (e.g., service attendance) were found to have direct, unmediated effects on health behaviors. Findings have implications for church-based health promotion in African American communities such as education or support groups.
Keywords: Religion, Self-esteem, Self-efficacy, African Americans, Health behaviors
Literature reviews on the relationship between religion and health have widely suggested evidence for a generally, though not always, positive role of religious involvement in health outcomes (Koenig, et al., 2001; Levin, 2001). These reviews conclude that religious involvement is associated with a number of health-related outcomes, such as mental health, depressive symptoms, mortality, and cancer coping. Research in this area has moved from accumulation of additional evidence for this association, to trying to explain why it exists. Focus on the mechanisms, or mediators, of the association has been discussed in several studies, including the present Religion and Health in African Americans, or “RHIAA” study.
Religious involvement is conceptualized as “an organized system of [religious] beliefs, practices, rituals, and symbols”, while spirituality involves “one’s transcendent relationship to some form of higher power” (Thoresen, 1998; p. 415). The current study focuses on religious involvement, as opposed to the broader construct of spirituality. Some segments of the population tend to be more religiously involved than others, including African Americans (Levin, et al., 1994; Taylor, et al., 1996). Fifty-five percent (55%) of African Americans report that they attend religious services at least once a week or almost every week, compared to 41% of non-Hispanic Whites (Gallup, 2010). In the African American community, the church has historically served functions beyond worship services, providing a hub for a variety of services and support (Lincoln & Mamiya, 1990). Resources provided by the church to both members and nonmembers include health programs (often called health ministries) that provide health education on a variety of topics, and counseling/support for those coping with issues such as substance abuse or HIV/AIDS (Belgrave & Allison, 2010). Further, African Americans’ religious and spiritual beliefs are an important part of coping strategies in response to stressful events, including health problems, and the absence of such beliefs are related to maladaptive coping, such as alcohol use (Belgrave, 1998; Potts, 1996; Wilson & Miles, 2001).
The study of religious involvement and health in this group is particularly important because African Americans are disproportionately impacted by health problems (Pleis & Lethbridge-Çejku, 2007), termed health disparities/inequities. The neonatal mortality rate for African Americans is 9.2 per 1,000 compared to 3.8 for Whites (National Center for Health Statistics 2007). Life expectancy for African American males at birth is 69.5 years compared to White males at birth of 75.7 years. Life expectancy for African American females at birth is 76.3 years compared to 80.8 years for White females (Arias, 2004). African Americans have hypertension rates higher than other groups and lower rates of hypertension control (Centers for Disease Control and Prevention, 2011). African Americans are 1.4–2.2 times more likely to have diabetes than are Whites (Agency for Healthcare Research and Quality, 2001). Cancer disparities are also apparent in deaths per 100,000 for colorectal cancer (African American = 24.8, White = 16.9), prostate cancer (African American = 53.3, White = 22.6), and breast cancer (African American = 32.8, White = 23.4). Herein also lies the applied value of the current research, to identify the mechanisms/mediators between religious involvement and health outcomes. If such mediators can be identified, they can be capitalized upon in faith-based health promotion efforts aimed at health disparities reduction.
Theoretical foundations
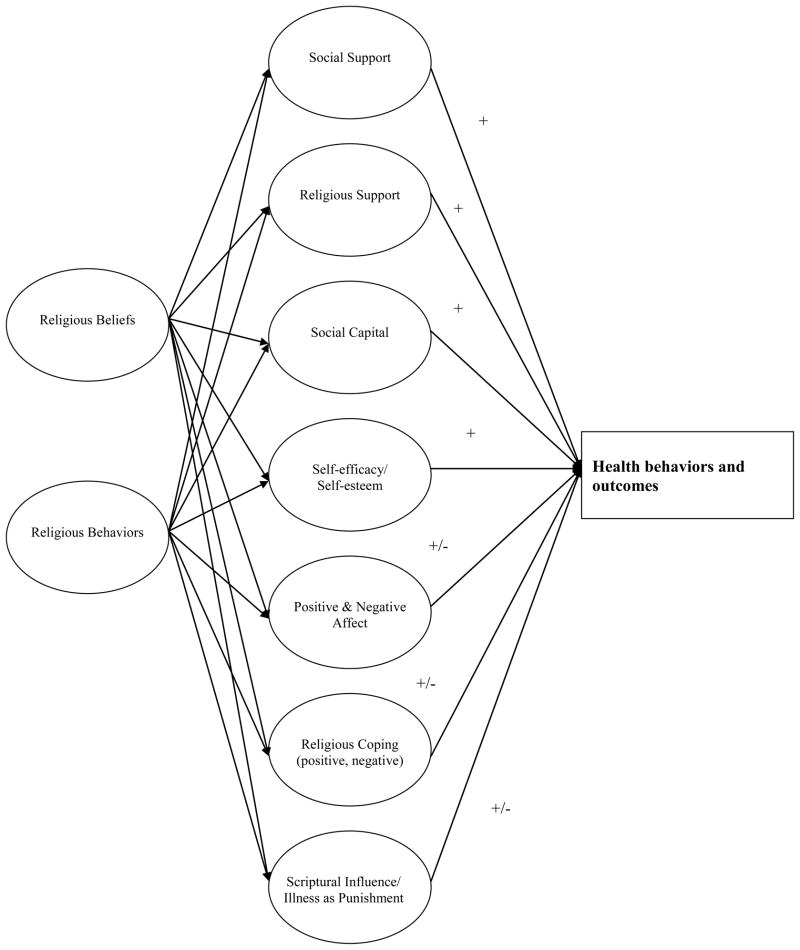
A number of explanatory models of the religion-health connection have been previously proposed in the religion and health literature. The present study utilizes a Religion-Health Mediational Model (see Figure 1), based on a systematic review of the literature on religion/spirituality and health (both physical and mental), and a program of previous qualitative research (Holt, et al., 2005; Holt & McClure, 2006; Schulz, et al., 2008; Holt, et al., 2009a; Holt, et al., 2009b). The Religion-Health Mediational Model involves a set of factors widely recognized to be possible mediators of the religion-health connection. To date, the model has been used to examine the role of mediators including religious coping (Holt, Clark, Debnam, & Roth, 2012), religious support (Holt, Wang, Clark, Williams, & Schulz, 2012), and social capital (Holt, Clark, Wang, Williams, & Schulz, 2012). In summary, religious beliefs were associated with greater vegetable consumption, in part due to the role of positive and negative religious coping (Holt, Clark, Debnam, & Roth, 2012). Negative religious coping appeared to play a role in the relationship between religious beliefs and increased alcohol consumption. Emotional religious support played a mediating role between religious behaviors and better emotional functioning and lower depressive symptoms (Holt, Wang, Clark, Williams, & Schulz, 2012). Finally, social capital in the form of interconnectedness mediated the relationship between religious behaviors and fewer depressive symptoms (Holt, Clark, Wang, Williams, & Schulz, 2012).
Figure 1.
Religion-Health Mediational Model
Previous theoretical models of the religion-health connection propose that, among other factors, religious involvement may impact health-related outcomes through the experience of positive self-perceptions, primarily self-esteem and self-efficacy. Self-esteem is defined as a positive or negative evaluation of a person’s value of one’s self (Rosenberg, 1965). Self-efficacy is defined as a person’s beliefs in their “capabilities to mobilize the motivation, cognitive resources, and courses of action needed to meet given situational demands” (Wood & Bandura, 1989, p. 408).
Religious involvement is said to promote health behaviors by increasing one’s self-esteem and self-efficacy (Ellison & Levin, 1998). These positive self-perceptions were proposed to impact health “beliefs, behaviors, and attitudes, and thus influence patterns of health care use” (p. 706). The review article concluded that while some have documented negative effects of religiosity involving beliefs about sin, there were generally modest, positive associations between religious involvement and self-esteem and self-efficacy. In terms of why religious involvement may result in these positive self-perceptions, several ideas were proposed (Ellison & Levin, 1998). People may strengthen self-perceptions through prayer, other religious practices, and a relationship with a higher power (Pollner, 1989; Ellison, 1994). Those who have such a relationship may experience unconditional love and a sense of divine guidance (Poloma & Gallup, 1991). Being involved in a faith community can provide social support that may bolster positive self-perceptions (Krause, 1995; Ellison, 1993), or affirm one’s values and way of life (Ellison, 1993).
A review by George and colleagues (2002) indicated that self-efficacy and self-esteem were promising mechanisms as psychological resources that religious involvement provides. They reviewed three cross-sectional studies and one longitudinal study that tested for mediation, and concluded that evidence was mixed and additional research was “badly needed” (p. 195). In a study specific to African Americans, it is proposed that religious involvement fosters self-esteem through social support and positive reflected appraisals of fellow congregation members, or how people believe that others in their faith community view them (Ellison, 1993). Findings from national data supported these ideas. In a recent review, it was concluded that research on the mechanisms is in the early stages (Ellison, et al., 2010). However, psychological resources such as self-esteem were included as a promising mechanism, whereby church members gain status and roles, and engage in skill building. Devotional activities were also proposed to build self-esteem and empowerment.
The current analysis must also consider why self-esteem and self-efficacy would be proposed to play a role in health behaviors. In addition to the theoretical frameworks presented above, we can look to theories of health behavior change. For example, the Health Belief Model (Rosenstock, Strecher, & Becker, 1988) and Social Cognitive Theory (Bandura, 1986) contain self-efficacy as one of their central constructs.
Mixed evidence
The evidence for self-esteem and self-efficacy as mediators of the religion-health connection has been mixed. In a prospective study of African American adults, Ellison and Flannelly (2009) found that the degree of guidance from religion in daily life acted as a protective factor for depressive symptoms even after controlling for socio-demographic variables and self-esteem. A nationwide cross-sectional study of older African American adults provided evidence for partial mediation for self-worth (Krause, 1992). Findings suggested that religious involvement protects against physical health and mortality by increasing feelings of self-worth, even after controlling for emotional support.
In contrast, self-esteem failed to mediate the relationship between service attendance and depressive symptoms in a sample of older Dutch citizens with various religious denominations (Braam, et al., 1998). Study results found that only among Roman Catholics did self-esteem mediate the relationship between church membership and depressive symptoms; this relationship did not persist among Calvinist study participants. Furthermore, in a Detroit sample, self-esteem was not found to mediate well-being or psychological distress (Ellison, et al., 2001). Data from this sample showed that the main effects of religious involvement on the mental health outcomes could not be explained by self-esteem. To date, no conclusive evidence can be drawn for the mediating effects of these psychosocial resources in the religion-health connection.
Research on the religion-health connection has focused on a variety of outcomes, both related to physical and mental/emotional health. While much previous research focuses on mental/emotional health outcomes such as depressive symptoms, well-being, and anxiety the present study was conducted in the context of physical health and health disparities impacting African Americans. As discussed above, African Americans suffer a disproportionate burden of chronic disease, which is impacted in part by lifestyle behaviors such as diet, physical activity, and alcohol consumption.
The current study focuses on health behaviors for several reasons. First, they are highly relevant to African Americans. Second, they are risk/prevention factors for a variety of chronic diseases (e.g., heart disease, diabetes, cancer). Thus, what is learned from the proposed study will be broadly applicable. Third, they are modifiable and have been the target of intervention efforts, including many community-and faith-based interventions.
The present study
Previous research suggests that although positive self-perceptions have been proposed as a religion-health mediator, there has been little empirical research testing their mediational role in the context of health-related outcomes. The few studies have suggested mixed and inconsistent findings, and have focused mainly on emotional health outcomes as opposed to those related to physical health. Therefore, examination of positive self-perceptions as a potential mediator of the religion-health connection warrants further investigation, with an adequate sample, and validated instruments.
African Americans have both higher levels of disease burden than other US emographic subgroups and they tend to have higher religious involvement. The RHIAA study, comprised of a national probability sample of African Americans, was designed for the purpose of empirically examining mediators of the religion-health connection. The purpose of the present study was to test the Religion-Health Mediational Model, specifically focusing on the mediator of positive self-perceptions (self-esteem and self-efficacy). The analysis will determine whether these constructs play a mediating role in a set of modifiable health risk and prevention behaviors in a national sample of African Americans. While the model includes more mediators than tested in the present study, testing of such a comprehensive theory is not feasible in a single statistical model. Therefore, the current study will focus on the positive self-perceptions aspect of the model, as part of a broader theory-testing initiative involving the systematic investigation of religion-health mediators conducted in the overall RHIAA study.
Method
Telephone survey methods
A professional sampling firm (Gensys) generated a call list of households from all 50 United States using probability-based methods. The firm obtained phone numbers from publicly available data such as motor vehicle records. Professional interviewers dialed telephone numbers from this call list. The interviewers identified an adult who lived at the household, and then introduced the project. If the contact expressed interest, a brief eligibility screener was administered to determine whether they were African American and age 21 or older. Interested and eligible contacts were read an informed consent script and provided verbal assent. Eligible individuals were self-identified African Americans, age 21 and older, who had not had a diagnosis of cancer. Cancer history was an exclusion criterion due to the collection of screening data for another part of the RHIAA initiative. Participants were mailed a $25 gift card upon completion of the 45-minute interview.
Measures
Religious involvement
An established Religiosity Scale previously validated with African Americans was used to assess private religious participation and beliefs [hereafter termed “beliefs”] (e.g., “I have a personal relationship with God”; “I feel the presence of God in my life.”; I pray often.”) and public religious participation and behaviors [hereafter termed “behaviors”] (e.g., church service attendance, involvement in other church activities like Bible study, choir rehearsal, other committee or ministry meetings; reading religious materials; watching religious television programs; Lukwago, et al., 2001). Based on previous work (Roth, et al., 2012; Holt, et al., 2012; Holt, Oster, et al., 2011; Holt, Wang, et al., 2011), four items were considered measures of beliefs, and 5 items assessed behaviors. Seven of the items used a 5-point Likert-type response format, and two monthly service attendance items used a 3-point response format (0; 1–3; 4+ times per month). Internal reliability of the beliefs (α=.89) and behaviors (α=.73) items were reasonable to high in the present sample.
Positive self-perceptions
Self-efficacy was assessed using the New General Self-Efficacy Scale eight-item scale (e.g., “I will be able to achieve most of the goals that I have set for myself.”) that has high internal reliability (α=.85–.88; α=.86 in the present sample) and test-retest reliability (r=.62–.66) (Chen, et al., 2001). Participants responded to items using a 5-point response format (strongly disagree…strongly agree).
Self-esteem was assessed using the Rosenberg Self-Esteem Scale (Rosenberg, 1965). The instrument contains 10 items (e.g., “I feel that I have a number of good qualities.”), has reasonable internal reliability (α=.77; α=.85 in the present sample) and 2-week test-retest reliability (r=.85) (Silber & Tippett, 1965). Participants responded to items using a 4-point response format (strongly disagree…strongly agree).
Health behaviors
Alcohol use was assessed using items from the Behavioral Risk Factor Surveillance System (BRFSS). This is an established interview, administered nationally, that has been tested and is appropriate for the study population. It has demonstrated adequate test-retest reliability over a 21-day period in a sample of African Americans (Stein, et al., 1993). Items assessed alcohol use in the past 30 days (no = 0, yes = 1), for those who reported some alcohol use, the largest number of drinks on any one occasion in past 30 days and number of binge drinking days in past 30 days. The cutoff for binge drinking was 4 or more drinks for women, and 5 or more drinks for men.
To assess fruit and vegetable consumption, an adaptation of National Cancer Institute’s Five-A-Day Survey was used (Block, et al., 1986). This instrument was validated with the study population (Kreuter, et al., 2005). It consists of 7 items that assess fruit consumption and 5 that assess vegetable consumption (e.g., “In a typical week, about how many times do you have…a piece of fresh fruit, like an apple, orange, banana, or pear.”). Fifteen different fruits and 18 vegetables are assessed specifically within these items, and “other fruit” and “other vegetable” items are included as well. The response scale varies from 0 to 8 or more servings per week. Consumption is assessed by asking participants to think about a typical week, and servings per day can be computed by summing all items and dividing by 7. The test-retest reliability over a two-week period (intraclass correlation coefficient) for the both the fruit (r = .52, p < .001) and the vegetable (r = .60, p < .001) portions were adequate.
Demographics
A standard demographic module assessed participant characteristics including sex, age, relationship status, educational attainment, work status, self-rated health status, and household income before taxes.
Statistical methods
All analyses reported in this paper were conducted using maximum likelihood estimation methods as performed by Mplus (version 6.1; Muthén & Muthén, 2010). A modification of the traditional two-step approach (Anderson & Gerbing, 1988) was used such that confirmatory factor analysis models were first run that specified the observed items to be indicators of underlying latent constructs and structural models were then run that tested the significance of the mediated and unmediated effects of religious involvement on the health behavior outcomes. In the confirmatory factor analysis measurement models, fit statistics were evaluated and correlated measurement residuals were then added between select indicators within factors as suggested by modification indices in order to obtain measurement models for each construct with adequate fit. The root mean square error of approximation (RMSEA) was the primary fit criterion used, and an RMSEA of 0.05 or less was considered indicative of excellent fit.
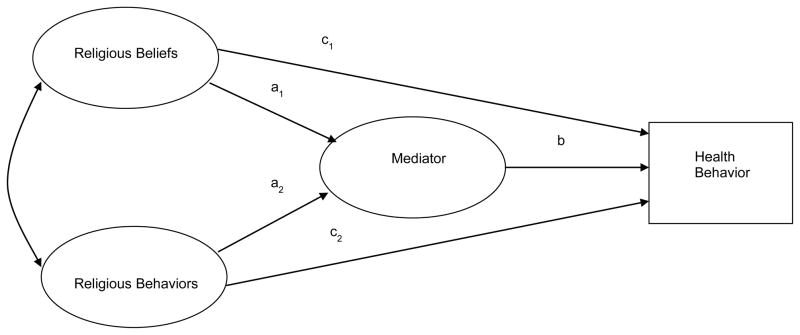
The general outline of the structural models is illustrated in Figure 2. Two mediators (self-esteem and self-efficacy) were examined individually in combination with 5 different outcome variables (fruit servings per day, vegetable servings per day, any alcohol use, largest number of drinks, number of binge drinking days) for a total of 10 different structural models. The analyses for the largest number of drinks and number of binge drinking days were run on the subset of participants who reported some alcohol use. In all models, four exogenous covariates – age, gender, education, and self-rated health status – were included as predictors of the religious involvement factors, mediating factor, and health behavior outcome variable. The standardized estimates from these models relevant to the mediated and unmediated (direct) effects were tested for statistical significance. These standardized estimates also constituted effect size measures that were compared across mediators and outcome measures to aid in the interpretation and integration of the findings across analyses.
Figure 2.
Structural model
Results
A total of 12,418 individuals were contacted for participation, and 2,370 agreed to participate. The overall response rate is calculated as accepted/[accepted + non-interviewed], or 19%. Of those contacted who did not participate (N=10,048), 8,240 refused prior to a determination of eligibility, 1,658 were not eligible [81 were under age twenty-one, 444 refused to provide an age for screening purposes, 878 were not African American, 224 reported a history of cancer, and 5 refused to respond to the question about cancer history]. Twenty six were incapable of participating in the interview. Only 150 were determined to be eligible but then refused to participate, making for an upper bound response rate of 94% (2,370/2,520). This study was approved by the University of Alabama at Birmingham and University of Maryland Institutional Review Boards. A description of the sample is provided in Table 1.
Table 1.
Participant demographic characteristics
| Characteristic | Categories | N=2,370 |
|---|---|---|
| Age, mean (SD) | 53.63 (14.82) | |
| Relationship status | Never married | 13.3% |
| Single | 17.2% | |
| Married or living w/partner | 36.9% | |
| Separated or Divorced | 18.8% | |
| Widowed | 13.8% | |
| Education | Grades 1–8 | 2.7% |
| Grades 9–11 | 9.4% | |
| Grade 12 or GED* | 32.8% | |
| 1–3 yrs college | 29.3% | |
| 4+ yrs college | 25.7% | |
| Work status | Full-time | 38.3% |
| Part-time | 11.8% | |
| Not currently | 12.6% | |
| Retired | 26.2% | |
| Receiving disability | 11.2% | |
| Income | < $5,000 | 8.7% |
| $5,000–$10,000 | 12.4% | |
| $10,000–$20,000 | 14.8% | |
| $20,000–$30,000 | 13.4% | |
| $30,000–$40,000 | 11.6% | |
| $40,000–$50,000 | 9.3% | |
| $50,000–$60,000 | 8.3% | |
| >$60,000 | 21.4% |
Note. Numbers may not sum to 2,370 or 100% due to missing data.
GED = General Equivalency Diploma
Those who refused to participate were asked to complete a brief non-responder survey (N=317 agreed to do so). Non-responders were in general older (M=60.82, SD=16.60, vs. M=53.63, SD=14.82, respectively), more likely to be men (48.3% men vs. 31.1% women), less likely to have attended four or more years of college (16.1% vs. 26%, respectively), less likely to have attended religious services in the past year (65.0% vs. 83.6%, respectively), and less likely to attend religious services four or more times per month (36.0% vs. 50.6%, respectively), than responders.
Measurement models
The results of the two-factor measurement model (beliefs and behaviors) for religious involvement items have already been published for this sample (Roth et al., 2012). After allowing for two correlated residuals – one between the first two items that both load on the religious beliefs factor and both reflect the concept of closeness with God, and one for two consecutive items that both load on the religious behaviors factor and both reflect attendance at religious services – excellent fit was observed for the religious involvement measurement model (χ2 = 138.57, df = 24, RMSEA = .045; Roth et al., 2012).
For the analyses in this paper, this religious involvement measurement model was expanded by adding items and factors for self-efficacy and for self-esteem in separate models. For self-efficacy, when all 8 items for this mediator loaded on a single latent factor in addition to the religious beliefs and behavior factors, excellent fit was observed for this three-factor model (χ2 = 700.66, df = 114, RMSEA = .047) and no correlated residuals were added for the items loading on the self-efficacy factor. For the self-esteem model, when all 10 items loaded on a single latent factor in addition to the two religious involvement factors, the overall measurement model provided reasonably good fit to the observed item data (χ2 = 1833.38, df = 147, RMSEA = .070). However, modification indices suggested the addition of three correlated residuals between adjacent items (1 and 2, 6 and 7, and 9 and 10), and when this modified model was estimated, the resulting measurement model met our threshold for excellent fit (χ2 = 979.87, df = 144, RMSEA = .049). These error covariances were considered appropriate because the items involved fell consecutively on the survey and were similarly worded, potentially causing their errors to be correlated.
Structural models
The effects of the two religious involvement factors on the two mediating latent variables and the 5 health behavior outcome variables are summarized in Table 2. Standardized estimates are reported both before and after taking into account four demographic covariates (age, gender, education, self-rated health) and the other religious involvement factor. Religious beliefs had stronger effects than religious behaviors on the self-efficacy and self-esteem mediating variables, whereas this pattern was reversed when examining the effects of the religious involvement factors on the health behavior outcomes. Table 3 summarizes the findings of the structural equation models that were conducted to test the mediation hypotheses. The standardized path estimates in Table 3 for the a, b, and c paths correspond directly to those effects illustrated in Figure 2 for each mediator and each health behavior analyzed separately. Table 3 also reports the overall RMSEA from each model after including the outcome variable and the four exogenous covariates. Since the a1 and a2 paths represent the effects of the religious beliefs and religious behaviors, respectively, on the mediator, these estimates are consistent and change very little from one health behavior outcome to another within a certain mediator variable.
Table 2.
Adjusted and unadjusted effects
| Mediator/Outcome | Religious Beliefs | Religious Behaviors | ||||
|---|---|---|---|---|---|---|
| Unadjusted | CV Adjusted | CV-Rel Adjusted | Unadjusted | CV Adjusted | CV-Rel Adjusted | |
| Self-efficacy (latent factor) | .210*** | .203*** | .183*** | .120*** | .159*** | .030 |
| Self-esteem (latent factor) | .238*** | .236*** | .241*** | .129*** | .162*** | −.007 |
| Fruit Servings | .055* | .036 | −.114** | .188*** | .148*** | .228*** |
| Vegetable Servings | .041 | .021 | −.060 | .126*** | .080** | .122** |
| Alcohol Use (Y/N) | −.097*** | −.067* | .058 | −.220*** | −.149** | −.190*** |
| Largest Number of Drinks | −.047 | −.037 | .075 | −.125** | −.118** | −.170** |
| Binge Drinking Days | −.106** | −.065 | .015 | −.179*** | −.111** | −.122* |
p < .05
p < .01
p < .001
Note. The CV adjusted effects are adjusted for age, gender, education, and self-rated health. The CV-Rel adjusted effects are those adjusted for age, gender, education, self-rated health, and the other religious involvement latent factor.
Table 3.
Summary of structural models
| Mediator | Health Behavior | b | Religious Beliefs | Religious Behaviors | RMSEA | ||||
|---|---|---|---|---|---|---|---|---|---|
| a1 | Direct (c1) | Indirect | a2 | Direct (c2) | Indirect | ||||
| Self- efficacy | Fruit servings | .077** | .182*** | −.128*** | .014** | .031 | .224*** | .002 | .043 |
| Vegetable servings | .093*** | .183*** | −.075* | .017** | .031 | .117** | .003 | .043 | |
| Alcohol Use (Y/N) | .066** | .183*** | .045 | .012* | .030 | −.191*** | .002 | .044 | |
| Largest Number of Drinks | .025 | .183*** | .012 | .005 | .031 | −.121* | .001 | .043 | |
| Binge Drinking Days | −.009 | .183*** | .077 | −.002 | .031 | −.167** | −.000 | .043 | |
| Self- esteem | Fruit Servings | .108*** | .237*** | −.140*** | .026*** | −.008 | .228*** | −.001 | .046 |
| Vegetable Servings | .097*** | .237*** | −.082* | .023** | −.008 | .121** | −.001 | .046 | |
| Alcohol Use (Y/N) | .044 | .237*** | .047 | .010 | −.008 | −.188*** | −.000 | .047 | |
| Largest Number of Drinks | −.111** | .237*** | .045 | −.026* | −.008 | −.123* | .001 | .046 | |
| Binge Drinking Days | −.097* | .237** | .098 | −.023* | −.008 | −.170** | .001 | .046 | |
RMSEA = root mean square error of approximation
For religious behaviors, the unmediated or direct effects are statistically significant for all five health behavior outcomes. Both before and after adjusting for the effects of religious beliefs, more religious behaviors were associated with more fruit and vegetable intake and less alcohol use. The religious behaviors factor was not significantly associated with either mediator after adjusting for the effects of religious beliefs, as evidence by the non-significant a2 paths in Table 3.
A more complicated pattern was observed for religious beliefs. After adjusting for the effects of religious behaviors, more religious beliefs had significant effects on both mediators (a1 paths). In addition, for both fruit and vegetable servings and both mediators, both the direct and the mediated effects of religious behaviors were statistically significant and in opposite directions. The direct effects were negative, meaning that after adjusting for religious behaviors and the mediator, higher religious beliefs was associated with lower fruit and vegetable intake, but the indirect effects through the self-efficacy and self-esteem mediators are positive and partially mitigate these negative direct effects. These patterns are indicative of inconsistent mediation, a type of suppressor effect (MacKinnon, et al., 2000; MacKinnon, et al., 2007), caused by the high correlation between religious beliefs and behaviors.
Discussion
The present study is one of the few to examine the mediating role of self-esteem and self-efficacy in the relationship between religious involvement and health behaviors among the health disparities-impacted population of African Americans. The study employed a multidimensional measure of religious involvement and was part of a comprehensive theory-testing initiative that was informed by previous literature and qualitative research with the priority population. Findings are discussed beginning with the “a” paths, then the direct “c” paths, and the mediation or “b” paths, as outlined in Figure 2.
Individuals high in religious beliefs were likely to have both high self-efficacy and self-esteem (Ellison & Levin, 1998; George, et al., 2002). This was not the case for religious behaviors, which included participation in services and activities. It appears that having a personal relationship with God/higher power and prayer are associated with increased self-esteem and self-efficacy in this population. This is somewhat different than the mechanism as originally proposed, in which individuals may bolster self-esteem through worship service and church activities (Ellison, 1993; Ellison, et al., 2010).
The direct paths suggest that people who were religiously involved in terms of behaviors were likely to have greater fruit and vegetable consumption, and less likely to use alcohol. It is possible that involvement in a religious community may be protective against alcohol consumption due to religious sanctions (Musick, et al., 2000; Strawbridge, et al., 2001). Previous research has agreed that religious involvement is associated with higher fruit and vegetable consumption (Holt, et al., 2005).
For religious beliefs, when examining the unadjusted paths in Table 2, findings suggest that those who have a close personal relationship with God/higher power and pray often were also likely to have greater fruit and vegetable consumption, and less likely to use alcohol. These findings agree with those for religious behaviors, suggesting that both dimensions of religious involvement carry salutary relationships with these health behaviors. Again, these findings had to be interpreted carefully due to the aforementioned suppressor effect. In fact due to the high correlations between religious beliefs and behaviors, the relationships at first glance appeared to be opposite in direction, but when examined in the unadjusted models without the influence of this correlation, the nature of the relationship was revealed.
Finally, with regard to mediation, it appears that self-efficacy at least in part accounts for the association between religious beliefs and greater fruit and vegetable consumption, as well as lower alcohol use. For the self-esteem mediation, findings were similar, in that self-esteem at least in part accounted for the association between religious beliefs and greater fruit and vegetable consumption, and lower alcohol use, particularly heavy drinking. This means that individuals who have a have a close personal relationship with God/higher power and pray often engage in these healthier behaviors in part because this relationship provides them with greater self-efficacy and self-esteem. This finding is consistent with previous research (Ellison & Levin; 1998; George, et al., 2002). Interestingly, neither self-efficacy nor self-esteem played a mediational role for the relationship between religious behaviors and any of the health behavior outcomes. As previously noted, religious behaviors were not associated with the mediators.
Strengths and limitations
There are several notable strengths of the present study. First, the RHIAA dataset was designed to test a theoretical model of the religion-health connection utilizing validated measures of the relevant constructs, rather than relying on secondary data analysis. Second, the study focuses on African Americans, a population disproportionately impacted by chronic disease and understudied in this area (Ellison, et al., 2010). Third, the analysis employed sophisticated modeling techniques to examine complex relationships among the study constructs.
However, the study findings must be interpreted in the context of several limitations. First, the telephone survey methods are subject to bias, particularly response bias. The nature of this bias is estimated and reported with the non-respondent survey findings. Second, the current analysis focused on positive self-perceptions including self-esteem and self-efficacy. As outlined in the literature review, there are additional factors (e.g., social norms, social support) that undoubtedly play a role in accounting for the religion-health connection. Due to the complexity of the relationships being examined, statistical models can easily become difficult to interpret as constructs are added. For this reason, the current analysis was focused on a clear understanding of fewer mediators, rather than a more inclusive but unintelligible model. Third, the study used general rather than specific measures of self-esteem and self-efficacy. Perhaps were health-specific self-esteem and self-efficacy measures administered, a more robust association would have been detected. In addition, the measure of religious beliefs reflected personal beliefs in having a relationship with a higher power and personal activities such as private prayer. It was not designed to measure specific religious beliefs per se. Fourth, because these data were cross sectional, implications about causality cannot be drawn. It may be that individuals who engage in healthy behaviors derive increased self-esteem and self-efficacy, and these relationships cannot be determined from the current data. Longitudinal data are required to answer this question, an initiative on which the RHIAA team is currently embarking.
Implications and future research
These findings indicate that religious beliefs, specifically involving a close personal relationship with a higher power, have positive relationships with dietary behaviors involving fruit/vegetable intake and lower alcohol consumption, and this may be in part due to higher levels of self-esteem and self-efficacy. This has implications for health promotion interventions, particularly community- or faith-based initiatives targeted for African Americans. Individuals who develop church- or faith-based educational or health promotion interventions can use these findings to improve the effectiveness of their programs. For example, an intervention to increase fruit and vegetable consumption may aim to strengthen dietary self-efficacy as part of the theoretical foundation of the content. Additionally, faith-based programs aimed at controlling alcohol abuse (e.g. Celebrate Recovery) or providing support groups may want to give special consideration to building self-esteem and self-efficacy as part of their program. These examples can be but one tool in the efforts to reduce the health disparities that continue to impact the African American community.
Acknowledgments
This work was supported by a grant from the National Cancer Institute, (#1 R01 CA105202) and was approved by the University of Maryland Institutional Review Board (#08-0328).
The team would like to acknowledge the work of Opinion America, who conducted participant recruitment and data collection activities for the present study.
References
- Agency for Healthcare Research and Quality. AHRQ Publication No 02-P007. Agency for Healthcare Research and Quality; Rockville, MD: 2001. Nov, [Accessed October 20 2012]. Diabetes Disparities Among Racial and Ethnic Minorities. [Online]. http://www.ahrq.gov/research/diabdisp.htm. [Google Scholar]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103:411–423. [Google Scholar]
- Arias E. National vital statistics reports. 14. Vol. 52. National Center for Health Statistics; 2004. United States life tables, 2001. [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, N.J: Prentice-Hall; 1986. [Google Scholar]
- Belgrave FZ. Psychosocial aspects of chronic illness and disability among African Americans. Westport, CT US: Auburn House/Greenwood Publishing Group; 1998. [Google Scholar]
- Belgrave FZ, Allison KW. African American Psychology: from Africa to America. 2. Thousand Oaks California: 2010. Introduction to African American Psychology. [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner LA. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Braam AW, Beekman ATF, Knipscheer CPM, Deeg DJH, van den Eeden P, van Tilburg W. Religious denomination and depression in older Dutch citizens: Patterns and models. Journal of Aging and Health. 1998;9:483–503. doi: 10.1177/089826439801000405. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed October 20, 2012];Fact sheet: Health disparities in hypertension and hypertension control. 2011 [Online]. http://www.cdc.gov/minorityhealth/reports/CHDIR11/FactSheets/Hypertension.pdf.
- Chen G, Gully SM, Eden D. Validation of a new general self-efficacy scale. Organizational Research Methods. 2001;4:62–83. [Google Scholar]
- Ellison CG. Religious involvement and self-perception among black Americans. Social Forces. 1993;71:1027–1055. [Google Scholar]
- Ellison CG. Religion, the life stress paradigm, and the study of depression. In: Levin JS, editor. Religion in aging and health: Theoretical foundations and methodological frontiers. Thousand Oaks, CA: Sage; 1994. pp. 78–121. [Google Scholar]
- Ellison CG, Boardman JD, Williams DR, Jackson JS. Religious involvement, stress, and mental health: Findings from the 1995 Detroit Area Study. Social Forces. 2001;80:215–249. [Google Scholar]
- Ellison CG, Flannelly KJ. Religious involvement and risk of major depression in a prospective nationwide study of African American adults. The Journal of Nervous and Mental Disease. 2009;197:568–573. doi: 10.1097/NMD.0b013e3181b08f45. [DOI] [PubMed] [Google Scholar]
- Ellison CG, Hummer RA, Burdette AM, Benjamins MR. Race, religious involvement, and health: The case of African Americans. In: Ellison CG, Hummer RA, editors. Religion, Families, and Health: Population-based Research in the United States. Rutgers University Press; New Brunswick, NJ: 2010. pp. 321–348. [Google Scholar]
- Ellison CG, Levin JS. The religion-health connection: Evidence, theory, and future directions. Health Education & Behavior. 1998;25:700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- Gallup Inc. [Accessed October 18 2012];Americans’ church attendance inches up in 2010. [online] 2010 Available: http://www.gallup.com/poll/141044/americans-church-attendance-inches-2010.aspx.
- George LK, Ellison CG, Larson DB. Explaining the relationships between religious involvement and health. Psychological Inquiry. 2002;13:190–200. [Google Scholar]
- Holt CL, Caplan L, Schulz E, Blake V, Southward P, Buckner A, Lawrence H. Role of religion in cancer coping among African Americans: A qualitative examination. Journal of Psychosocial Oncology. 2009a;27:248–273. doi: 10.1080/07347330902776028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Clark EM, Debnam KJ, Roth DL. Religious involvement and health behaviors in a national sample of African Americans: The role of religious coping. 2012. Manuscript submitted for publication. [Google Scholar]
- Holt CL, Clark EM, Wang MQ, Williams BR, Schulz E. The religion- health connection among African Americans: What is the role of social capital? 2012. Manuscript submitted for publication. [Google Scholar]
- Holt CL, Haire-Joshu DL, Lukwago SN, Lewellyn LA, Kreuter MW. The role of religiosity in dietary beliefs and behaviors among urban African American women. Cancer Control, Cancer Culture and Literacy Supplement. 2005;12:84–90. doi: 10.1177/1073274805012004S12. [DOI] [PubMed] [Google Scholar]
- Holt CL, Lewellyn LA, Rathweg MJ. Exploring religion-health mechanisms among African American parishioners. Journal of Health Psychology. 2005;10:511–527. doi: 10.1177/1359105305053416. [DOI] [PubMed] [Google Scholar]
- Holt CL, McClure S. Perceptions of the religion-health connection among African American church members. Qualitative Health Research. 2006;16:268–281. doi: 10.1177/1049732305275634. [DOI] [PubMed] [Google Scholar]
- Holt CL, Oster RA, Clay KS, Urmie J, Fouad M. Religiosity and physical and emotional functioning among African American and White colorectal and lung cancer patients. Journal of Psychosocial Oncology. 2011;29:372–393. [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Schulz E, Williams B, Clark EM, Wang MQ, Southward PL. Assessment of religious and spiritual capital in African American communities. Journal of Religion and Health. 2012 doi: 10.1007/s10943-012-9635-4. Article first published online: 19 JUL 2012. [DOI] [PubMed] [Google Scholar]
- Holt CL, Schulz E, Wynn TA. Perceptions of the religion-health connection among African Americans in the Southeastern United States: Sex, age, and urban/rural differences. Health Education and Behavior. 2009b;36:62–80. doi: 10.1177/1090198107303314. [DOI] [PubMed] [Google Scholar]
- Holt CL, Wang MQ, Caplan L, Schulz E, Blake V, Southward VL. Role of religious involvement and spirituality in functioning among African Americans with cancer: Testing a mediational model. Journal of Behavioral Medicine. 2011;34:437–448. doi: 10.1007/s10865-010-9310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Wang MQ, Clark EM, Williams B, Schulz E. Religious involvement and physical and emotional functioning among African Americans: The mediating role of religious support. Psychology and Health. 2012 doi: 10.1080/08870446.2012.717624. Article first published online: 06 AUG, 2012. [DOI] [PubMed] [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. New York: Oxford University Press; 2001. [Google Scholar]
- Krause N. Stress, religiosity, and psychological well-being among older Blacks. Journal of Aging and Health. 1992;4:412–439. [Google Scholar]
- Krause N. Religiosity and self-esteem among older adults. Journal of Gerontology: Psychological Sciences. 1995;50:P236–P246. doi: 10.1093/geronb/50b.5.p236. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Skinner CS, Holt CL, Clark EM, Haire-Joshu D, Fu QJ, Steger-May K, Booker AC, Bucholtz DC. Cultural tailoring for mammography and fruit and vegetable consumption among low-income African American women in urban public health centers. Preventive Medicine. 2005;41:53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Levin JS. God, faith, and health: Exploring the spirituality-healing connection. Hoboken: John Wiley & Sons; 2001. [Google Scholar]
- Levin JS, Taylor RJ, Chatters LM. Race and gender differences in religiosity among older adults: Findings from four national surveys. Journal of Gerontology. 1994;49:S137–S145. doi: 10.1093/geronj/49.3.s137. [DOI] [PubMed] [Google Scholar]
- Lincoln CE, Mamiya LH. The black church in the African American experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- Lukwago SL, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family and Community Health. 2001;24:63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musick MA, Traphagan JW, Koenig HG, Larson DB. Spirituality in physical health and aging. Journal of Adult Development. 2000;7:73–86. [Google Scholar]
- Muthén LK, Muthén BO. Mplus software version 6.0. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Pleis JR, Lethbridge-Çejku M. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. National Center for Health Statistics. Vital Health Statistics. 2007;10(235) [PubMed] [Google Scholar]
- Pollner M. Divine relations, social, relations, and well-being. Journal of Health and Social Behavior. 1989;30:92–104. [PubMed] [Google Scholar]
- Poloma MM, Gallup G. Varieties of prayer: A survey report. Philadelphia: Trinity Press International; 1991. [Google Scholar]
- Potts RG. Spirituality and the experience of cancer in an African-American community: Implications for psychosocial oncology. Journal of Psychosocial Oncology. 1996;14:1–19. doi: 10.1300/J077v14n01_01. [DOI] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social Learning Theory and the Health Belief Model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Roth DL, Mwase I, Holt CL, Clark EM, Lukwago S, Kreuter MW. Religious involvement measurement model in a national sample of African Americans. Journal of Religion and Health. 2012;51:567–578. doi: 10.1007/s10943-011-9475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz E, Holt CL, Caplan L, Blake V, Southward P, Buckner A, Lawrence H. Role of spirituality in cancer coping among African Americans: A qualitative examination. Journal of Cancer Survivorship. 2008;2:104–115. doi: 10.1007/s11764-008-0050-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silber E, Tippett JS. Self-esteem: Clinical assessment and measurement validation. Psychological Reports. 1965;16:1017–1071. [Google Scholar]
- Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine. 2001;23:68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- Stein AD, Lederman RI, Shea S. The Behavioral Risk Factor Surveillance System questionnaire: its reliability in a statewide sample. American Journal of Public Health. 1993;83:1768–1772. doi: 10.2105/ajph.83.12.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Jayakody R, Levin JS. Black and white differences in religious participation: A multisample comparison. Journal for the Scientific Study of Religion. 1996;35:403–410. [Google Scholar]
- Thoresen CE. Spirituality, health, and science: The coming revival? In: Roth-Roemer S, Kurpius SR, editors. The emerging role of counseling psychology in health care. New York: W. W. Norton; 1998. pp. 409–431. [Google Scholar]
- Wilson SM, Miles MS. Spirituality in African-American mothers coping with a seriously ill infant. Journal of the Society of Pediatric Nurses. 2001;6:116–122. doi: 10.1111/j.1744-6155.2001.tb00133.x. [DOI] [PubMed] [Google Scholar]
- Wood R, Bandura A. Impact of conceptions of ability on self-regulatory mechanisms and complex decision making. Journal of Personality and Social Psychology. 1989;56:407–415. doi: 10.1037//0022-3514.56.3.407. [DOI] [PubMed] [Google Scholar]