Abstract
Objectives
To evaluate the effects of heart rate and heart rate variability on image quality, patient dose and diagnostic accuracy of 320-detector row CT.
Methods
94 patients were prospectively enrolled. Heart rate was defined as the mean value of different intervals elapsing between two consecutive R waves in an electrocardiogram (R–R intervals) and the heart rate variability was calculated as the standard deviation from the average heart rate. The image quality was evaluated by four grades, according to motion artefacts (“step artefacts” and “blurring artefacts”). The diagnostic accuracy was analysed in 43 patients who were scheduled for invasive coronary angiography (ICA). The coeffects of heart rate and heart rate variability on image quality, radiation dose and diagnostic accuracy were evaluated by multivariate regression.
Results
The mean image quality score was 1.2±0.5 and the mean effective dose was 14.8±9.8 mSv. The results showed that heart rate (74.0±11.2 beats per minute) was the single factor influencing image quality (p<0.001) and radiation dose (p<0.001), while heart rate variability (3.7±4.6) had no significant effect on them (p=0.16 and p=0.47, respectively). For 43 patients who underwent ICA, heart rate and heart rate variability showed no influence on the accuracy (p=0.17 and p=0.12, respectively). Overall sensitivity was 97.4% (37/38), specificity was 99.4% (351/353), positive predictive value was 94.9% (37/39) and negative predictive value was 99.7% (351/352).
Conclusion
320-detector row CT, with improved longitudinal coverage of detector, resolves step artefact and high patient dose caused by irregular heart rate. However, it is still recommended to control heart rate to a lower level to eliminate blurring artefact and radiation dose.
As the clinical application of 4-detector CT to scan the coronary arteries by a non-invasive procedure, CT coronary angiography has emerged as an attractive, diagnostic modality for detecting coronary artery disease. However, motion artefact by rapid movement throughout the cardiac cycle and blooming artefact caused by calcified plaque represent the major challenges for artefact-free coronary CT angiography. Generally, “step artefacts” and “blurring artefacts” are two kinds of motion artefact influencing the quality of coronary artery image. To improve image quality, CT scanners with higher spatial resolution, temporal resolution and wider detector array were developed.
The Discovery™ CT750 HD (GE Healthcare, Waukesha, WI) improves spatial resolution and decreased calcium blooming artefact significantly [1]. Dual-source CT (DSCT), with two X-ray sources and a temporal resolution of 83 ms, has improved blurring artefacts caused by high heart rate (HR) [2-4]. Nevertheless, as the coverage of the detectors is limited, step artefacts caused by heart rate variability (HRv) is still an inverse factor influencing the image quality [2,3]. Just as the improved temporal resolution should resolve the problem of high HR, the longitudinal coverage of the detector should be expanded further to resolve the influence of HRv [5-8]. 320-detector row dynamic volume CT (DVCT) can cover the whole heart within one heartbeat, which enables DVCT to have the potential to resolve the impact of HRv [9].
A previous study has shown that DVCT reliably provides high diagnostic accuracy without HR control [9]. The aim of our study was to evaluate the influence of degree of HR and HRv on image quality, radiation dose and diagnostic accuracy in patients undergoing DVCT.
Methods and materials
Study patients
Our study protocol and radiation dose information was approved by the local ethics committee. An informed consent that included information about the risk of radiation and iodine allergic reaction was obtained from all the patients [10].
Between May 2009 and September 2009, 112 patients suspected of coronary artery disease (CAD; n=93) or with recurrent angina in history of myocardial infarction (n=19) were enrolled in this study. Exclusion criteria were as follows: allergy to iodinated contrast agents (n=4), renal insufficiency (creatinine level >120 µmol l–1; n=2), pregnancy (n=2), haemodynamic instability (n=2), known abnormal origin and course of the coronary arteries (n=2) and previous history of coronary stented segments or coronary artery bypass graft (n=6). According to the exclusion criteria, the study included a total of 94 patients (29 women, 65 men; mean age, 65.6±10.3 years; age range, 39–91 years). Oral β-blockade (50 mg atenolol) was given to patients with HR >70 beats per minute (bpm; except 7 patients with contraindications). The mean body mass index (BMI; weight in kilograms divided by height in metres squared) was 23.9±3.5 kg m–2 (range, 16.7–31.5 kg m–2).
CT scanning protocol
All CT examinations were performed with a 320-detector row CT scanner (Aquilion ONE™; Toshiba, Nasu, Japan) without any complications. We administered 0.4 mg nitroglycerin 2 min before scanning in absence of contraindications (hypotension, current use of nitrate medications, migraine sensitive to nitrates). A breath-hold trial was performed by simulating scanning with a single 5-s breath-hold command to adjust scanner settings to individual patients [11]. The scanning range positioned from the level of the tracheal bifurcation to the diaphragm to cover the entire heart (scanning range coverage was 12–14 cm).
A 60-ml bolus of Iohexol (Omnipaque 350; Amersham Health, now GE Healthcare, Shanghai, China) was injected into an antecubital vein through an 18-gauge catheter at an injection rate of 5 ml s–1, followed by a 50-ml saline solution continuously. According to bolus-tracking technique (SUREStart, Toshiba), a threshold was set at 180 HU in the descending aorta. The scanning parameters were: collimation 320×0.5 mm, gantry rotation time of 350 ms, tube voltage and tube current of 100 kV and 350 mA for BMI <18 kg m–2, 100 kV and 400 mA for BMI from 19 to 24 kg m–2, 120 kV and 450 mA for BMI >24 kg m–2. A prospective electrocardiographic (ECG) gating was used in all cases. Data acquisition was performed using prospective ECG gating from 60 to 85% of the time elapsing between two consecutive R waves in an electrocardiogram (R–R interval) when the HR did not exceed 70 bpm, 40–85% in patients with HR between 70 and 80 bpm and 30–90% in patients with HR 80 bpm.
For HR <70 bpm at time of breath-hold trial, one-heartbeat scan acquisition mode was used. For HR between 70 and 80 bpm, two-heartbeat acquisition mode was used. For HR >80 bpm, three-heartbeat acquisition mode was necessary to improve temporal resolution. Using multisegment algorithm, the temporal resolution was able to reach 87.5–58.3 ms. If HRv changed 20% more than HR at time of breath-hold trial, the scanner would hold on scanning and the system would attempt to capture one normal beat until the maximum exposure time was reached.
Data analysis
Image reconstruction was performed using a section thickness of 0.5 mm and an increment of 0.25 mm. The field of view for the images was adjusted to exactly encompass the heart (180–240 mm). Images were first reconstructed at pre-set 75% of R–R interval. When the image quality was poor in patients with a stable HR, we determined which image from the automatically generated data stack at 75% of the R–R interval had the worst image quality. At this fixed level we then undertook further reconstructions at 2% steps through the available reconstruction window to determine the optimal reconstruction interval. For patients with an unstable HR, we used an absolute timing approach and reconstructed transverse images with a 10-ms step from peak R wave. In both cases, when the interval with least motion artefact was determined, the whole heart data were reconstructed.
All images were transferred to the workstation (Vitrea® II fX; VitalImages, Minnetonka, MN). Curve planar reconstruction and volume rendering were used to assess the image quality and coronary artery stenosis by two experts with 7 and 6 years of experience in cardiovascular radiology. Decisions were reached with a consensus. Coronary arteries were subdivided according to the 15-segment model proposed by the American Heart Association [12]. All segments with diameters <1.5 mm were excluded.
According to motion artefacts, quality score was measured by using the following four-point scale as follows [2]: 1, excellent (no motion artefacts and clear delineation of the segment); 2, good (minor artefacts and mild blurring of the segment); 3, adequate (moderate artefacts and moderate blurring without structure discontinuity); 4, non-evaluable (doubling or discontinuity in the course of the segment preventing evaluation or vessel structures not differentiable or severe artefacts). Stenoses were visually classified as significant (≥50% lumen diameter reduction) or non-significant (<50% lumen diameter reduction).
The ECG data were analysed by a third reviewer who was not involved in the image quality assessment. HR was defined as the mean HR of different R–R intervals during scanning; in patients scanned with multiple-heartbeat acquisition mode, the HRv during scanning was calculated as the standard deviation (SD) from the average HR during scanning, as previously shown [13].
Evaluation of radiation dose of CT coronary angiography
The dose–length product (DLP) displayed on the dose report on the CT scanner was recorded. An effective dose (E) was obtained using the equation:
| (1) |
which was calculated specifically for DVCT [14].
Invasive coronary angiography
For 43 patients who were scheduled for clinically indicated invasive coronary angiography (ICA), ICA was performed with the conventional Judkin technique. Four views of the left coronary artery and two views of the right coronary artery were analysed in consensus by two cardiologists with 11 years of experience. They were unaware of the CT results during the analysis. Coronary artery segments were defined according to the same guidelines mentioned above [12]. Lesions with a stenosis 50% or more in diameter were considered to be significant.
Statistical analysis
Statistical analysis was performed with SPSS® software (v. 16 for Windows; SPSS, Chicago, IL). A p-value of <0.05 indicated a statistically significant difference.
Quantitative variables were expressed as a mean ± standard deviation, and categorical variables as frequencies or percentages. The interobserver agreement for the determination of the image quality readout and assessment of significant coronary artery stenosis was calculated with kappa statistics.
In a subanalysis, patients were subdivided into three groups according to mean HR (Group A: HR <70 bpm; Group B: 70–79 bpm; Group C: HR ≥80 bpm). Bivariate data were tested by Pearson correlation. Multivariate regression analysis was performed to test for mutual effects of the mean HR and HRv on the mean image quality score and diagnostic accuracy. The diagnostic performance of DVCT for the detection of a significant stenosis was calculated using the following parameters for measurement: sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV).
Results
The average HR of 94 patients during scanning was 74.2±11.2 bpm (range, 54–114.3 bpm) and the average SD of HRv was 3.7±4.6 (range, 0–18.1). Among the 94 patients, there were 44 patients (14 women, 30 men; mean age, 63.6±10.5 years) with an HR >70 bpm and whose BMI was 24.4±3.8 kg m–2. There were 27 patients (6 women, 21 men; mean age, 68.2±9.3 years) with an HR of 70–80 bpm, whose BMI was 23.0 kg m–2±3.1. There were 23 patients (9 women, 14 men; mean age, 66.5±10.7 years) with an HR of >90 bpm, whose BMI was 23.9±3.0 kg m–2. Of the 94 patients, 1317 out of potentially 1410 segments were available for evaluation. 93 segments were non-accessible because of either variation in coronary anatomy or vessels possessing a diameter <1.5 mm at their origin. The image quality scores are shown in Table 1.
Table 1. Image quality of different coronary arteries.
| Characteristic | Total | RCA | LM/LAD | LCX |
| Number of segments | 1317 | 352 | 530 | 435 |
| Image quality score (mean±SD) | 1.17±0.47 | 1.19±0.54 | 1.15±0.44 | 1.18±0.45 |
| Percentage of segments with score | ||||
| 1 | 87.2 (1148/1317) | 88.1 (310/352) | 88.3 (468/530) | 85.1 (370/435) |
| 2 | 9.3 (122/1317) | 6.0 (21/352) | 9.1 (48/530) | 12.2 (53/435) |
| 3 | 3.3 (43/1317) | 5.4 (19/352) | 2.3 (12/530) | 2.8 (12/435) |
| 4 | 0.3 (4/1317) | 0.6 (2/352) | 0.4 (2/530) | 0 (0/435) |
LAD, left anterior descending artery; LCX, left circumflex artery; LM, left main artery; RCA, right coronary artery; SD, standard deviation.
Effect of heart rate and heart rate variability on image quality
The kappa value for image quality evaluation was excellent (κ=0.85). A significant correlation was found between mean HR and mean image quality (r=0.63, p<0.001) (Figure 1). Among the 47 patients with HR <70 bpm during the breath-hold trial, there were 43 patients scanned by one-heartbeat scan acquisition mode, 4 patients were scanned with 2- or 3-heartbeat scan acquisition as a premature beat happened. After eliminating the data of short R–R intervals, images were constructed using one R–R interval. Thus, there was no variability of HR for patients with HR <70 bpm during the breath-hold trial. For 47 patients with HR >70 bpm during the breath-hold trial, two or three R–R intervals were needed to improve temporal resolution. No significant correlation was found between HRv and the overall image quality (r=0.16, p=0.27; Figure 2).
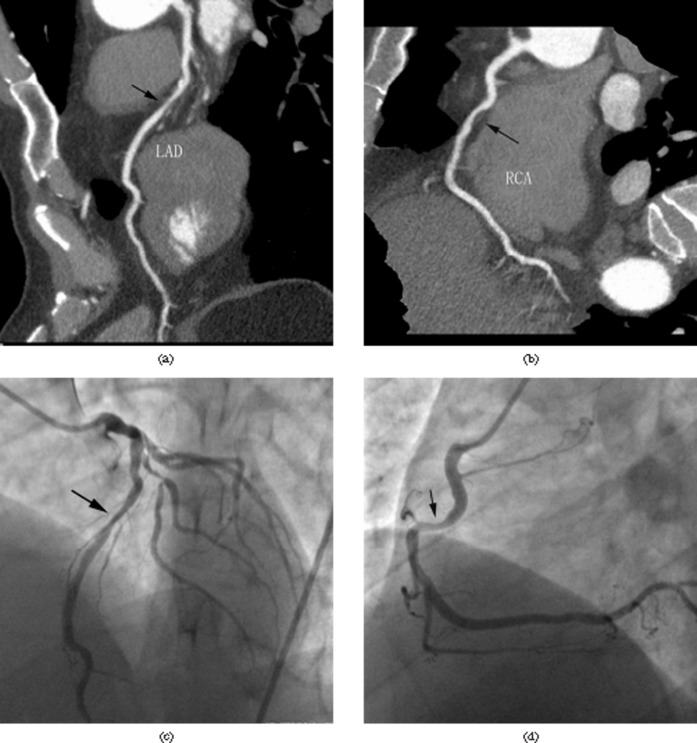
Figure 1.
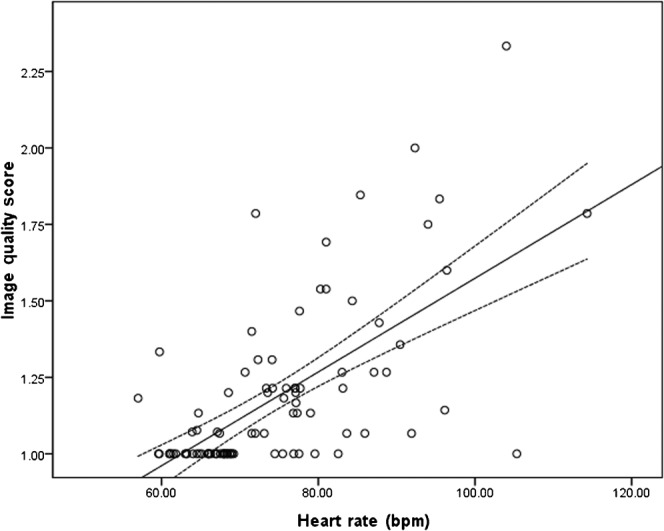
A linear regression plot of the image quality score (y-axis) against HR (x-axis). Dashed lines are 95% confidence interval limits.
Figure 2.
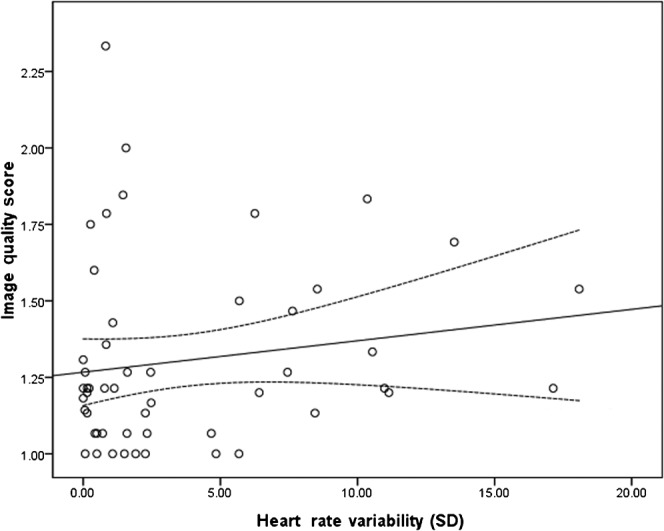
In total, there were 47 patients in which two or three R–R intervals (i.e. time elapsing between two consecutive R waves in an electrocardiogram) were needed to improve temporal resolution. No significant correlation was found between HRv (x-axis) and the overall image quality (y-axis). Dashed lines are 95% confidence limits. SD, standard deviation.
Multivariate regression analysis to consider the coeffect of mean HR and HRv on image quality showed that HR was the single factor of significant influence (p<0.001), while HRv had no significant effect on image quality (p=0.16).
Effects of heart rate and heart rate variability on radiation dose
The mean estimated effective dose was 14.8±9.8 mSv. In patients with an HR of <70 bpm, the mean radiation exposure of coronary CT angiography was 7.1±7.0 mSv. With higher HR, effective dose increased significantly (p<0.001; Table 2), while there was no significant influence of HRv regarding an effective dose (p=0.47).
Table 2. Radiation dose of different HR groups.
| Groups | Effective dose (mSv) | p-value |
| HR (bpm) | ||
| <70 | 7.1±7.0 | |
| 70–80 | 20.7±5.9 | <0.001a |
| ≥80 | 23.7±5.4 | <0.001a |
bpm, beats per minute; HR, heart rate.
aComparison with patients with HR <70 bpm, calculated by Dunnett's t-test.
Effect of mean heart rate and heart rate variability on diagnostic accuracy
The kappa value for coronary artery stenosis detection was 0.82. Significant coronary artery stenosis was presented in 38 segments of the 43 patients who underwent invasive coronary angiography. On the basis of a per-segment analysis, overall sensitivity was 97.4% (37/38), specificity was 99.4% (351/353), PPV was 94.9% (37/39) and NPV was 99.7% (351/352). According to multivariate logistic regression analysis, HR and HRv showed no influence on the accuracy of lesion detection (p=0.17 and 0.12, respectively; Figure 3).
Figure 3.
Images of a 63-year-old patient with an HR of 77.1 beats per min and an HRv of 17.1. Excellent and good images could be reconstructed. (a, b) Curve planar reconstruction showed stenosis in right coronary artery (RCA) and left anterior descending artery (LAD) (arrows). (c, d) Invasive coronary angiography confirmed the diagnosis.
Discussion
“Step artefacts” and “blurring artefacts”
Generally, the motion artefacts include step artefacts and blurring artefacts. For blurring artefacts, the degraded image quality is mainly caused by the low temporal resolution of the CT scanner. Because the image quality is affected by the rapid movement of the coronary artery, it is critical to expose at the cardiac phases with minimal motion. As the cardiac phases are shortened in higher HR, it is necessary to apply the multisegment algorithm to improve temporal resolution. However, when the interpolation between data derived from different heartbeats determines an image, there is the possibility that the images derived from different R–R intervals might be independent from the actual anatomical shape of the coronary segment. In this situation, the image quality is degraded by blurring artefacts.
For DSCT, with an improved temporal resolution of 83 ms, there is no need to use the multisegment algorithm. The blurring artefacts have been reduced greatly [2-4]. For DVCT, when HR was <70 bpm, the whole coronary artery can be imaged with one heartbeat. In patients with higher HRs, when higher temporal resolution is desired, multisegment reconstruction is necessary, and two or more heartbeats are needed to improve temporal resolution. When non-proportional shortening and prolongation of the cardiac phases happens, the ECG-gated image reconstruction technique at a fixed interval does not generate images at the same cardiac phases [15]. Thus, the blurring artefact cannot be avoided completely. Compared with image quality in HR <70 bpm, the degradation of image quality in higher HR is caused by the different reconstruction algorithms (multisegment algorithm vs single-segment algorithm).
For step artefacts, the image quality is mainly decreased by the limited longitudinal coverage of the detector. Applying 64-slice CT and DSCT, the entire heart must be imaged by subvolumes of the entire cardiac volume over multiple gantry rotations. When HRv happens, the HR along the z-axis are not stable. Using 64-slice CT, the correlation between image quality and HRv was 0.57–0.61. The image quality was degraded greatly by step artefacts. Applying DSCT, the image score increased from 2.0 to 2.4 and the accuracy decreased from 93% to 89% when HRv was greater than 15 bpm [16-18].
For DVCT, if HR was <70 bpm, the whole coronary artery can be imaged within one R–R interval; thus, HRv is 0. If HR was >70 bpm, the multisegment algorithm is required to improve temporal resolution. The degree of HRv, however, does not influence the image quality significantly. The main reason is the expanded longitudinal coverage of the detector. As the acquisition of the entire cardiac volume in a single gantry rotation allows the contrast bolus to be imaged at a single time point, there is no difference of R–R intervals along the z-axis. Thus, the step artefacts can be eliminated greatly. In addition, if HRv was >20%, the scanner will hold on and expose a similar R–R interval. HRv can be controlled within 20%. Therefore, the misalignment of images from the variation in R–R intervals is not statistically affected by the degree of HRv.
Patient dose
Baumüller et al's study of DSCT and 64-slice CT shows exposure doses of 10.9±1.1 mSv and 10.4±1.7 mSv, respectively [19]. Our study shows a higher dose (14.8±9.8 mSv). The redundant dose may be caused by the different conversion factor in dose estimation. In previous studies, the value of conversion factor k=0.017 mSv mGy−1 cm−1 was usually used [11,19]. However, this conversion factor is a chest conversion factor. Einstein et al suggest that the conversion factor should be 0.029 mSv mGy−1 cm−1 for DVCT [14].
Using DSCT, Weustink et al [20] revealed that the radiation dose increases significantly with HRv. As helical scanning mode is applied in their study, a low pitch is applied when HRv occurs. Thus, more overlapping exposures to the patient cause a higher radiation dose. In addition, as full X-ray exposure is initiated during two subsequent heartbeats to decrease step artefacts [21], the total exposure time increases significantly with HRv [20,22]. For DVCT, the whole heart is scanned by volume mode, which images the coronary artery with a pitch of 0. With full cardiac coverage, HRv does not cause more overlapping radiation exposure, which provides significant radiation dose savings for cardiac imaging. Furthermore, if a severe HRv is detected by DVCT, the scanner would hold on scanning of the short R–R intervals, which eliminates the influence of HRv further. Recently, step-and-shoot CT coronary angiography and DSCT using the spiral FLASH mode have gained interest as a means to reduce radiation exposure significantly. However, motion artefacts seem more severe. Therefore, it has more strict pre-conditions that HR should be low and regular [23-26].
As the temporal resolution of DVCT is low, the multisegment reconstruction is required in high HR. Therefore, more heartbeats are needed to complete image reconstruction. In addition, the exposure phase was also expanded in high HR. The exposure time and radiation dose increases significantly with HR. The multisegment reconstruction technology improves temporal resolution at the expense of significantly higher radiation dose. Thus, for DVCT, it is still suggested to control HR, if possible.
Diagnostic accuracy
With high HR and severe HRv enrolled in this study, the accuracy of DVCT is still high. We believe the main reason is the eliminated influence of HRv. In addition, as the image quality degradation caused by HR mainly presents in a shift from excellent to good, 97.3% segments are sufficient for image evaluation. Therefore, no effect of HR and HRv on diagnostic accuracy is found.
Several limitations should be declared. Firstly, as patients with HR <70 bpm have no variability of HR, the effect of HRv is only calculated in patients with HR >70 bpm. Thus, the comparison of patients between DVCT and other types of CT may be influenced by the different patients enrolled. Secondly, only some of the patients enrolled in this study underwent both DVCT and ICA. Thus, the analysis of diagnostic accuracy may be affected. Thirdly, image quality scoring might have been influenced by a subjectivity bias.
In conclusion, DVCT, with improved longitudinal of detector, resolves step artefact and high patient dose caused by HRv. As HR is still a main factor for higher radiation dose, it is still suggested to control HR to eliminate blurring artefact and radiation dose.
References
- 1.Pelberg RA, Mazur W, Clarke G, Szawaluk J. The what and why of cardiac CT angiography: data interpretation and clinical practice integration. Rev Cardiovasc Med 2009;10:152–63 [DOI] [PubMed] [Google Scholar]
- 2.Brodoefel H, Burgstahler C, Tsiflikas I, Reimann A, Schroeder S, Claussen CD, et al. Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology 2008;247:346–55 [DOI] [PubMed] [Google Scholar]
- 3.Matt D, Scheffel H, Leschka S, Flohr TG, Marincek B, Kaufmann PA, et al. Dual-source CT coronary angiography: image quality, mean heart rate, and heart rate variability. AJR Am J Roentgenol 2007;189:567–73 [DOI] [PubMed] [Google Scholar]
- 4.Weustink A, Neefjes L, Kyrzopoulos S, van Straten M, Neoh ER, Meijboom W, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology 2009;253:672–80 [DOI] [PubMed] [Google Scholar]
- 5.Kitagawa K, Lardo A, Lima J, George R. Prospective ECG-gated 320 row detector computed tomography: implications for CT angiography and perfusion imaging. Int J Cardiovasc Imaging 2009;25:201–8 [Google Scholar]
- 6.Bastarrika G, Lee Y, Huda W, Ruzsics B, Costello P, Schoepf U. CT of coronary artery disease. Radiology 2009;253:317–38 [DOI] [PubMed] [Google Scholar]
- 7.Choi SI, George RT, Schuleri KH, Chun EJ, Lima JA, Lardo AC. Recent developments in wide-detector cardiac computed tomography. Int J Cardiovasc Imaging 2009;25(suppl. 1):23–9 [DOI] [PubMed] [Google Scholar]
- 8.Klass O, Walker M, Siebach A, Stuber T, Feuerlein S, Juchems M, et al. Prospectively gated axial CT coronary angiography: comparison of image quality and effective radiation dose between 64- and 256-slice CT. Eur Radiol 2010;20:1124–31 [DOI] [PubMed] [Google Scholar]
- 9.Gang S, Min L, Li L, Guo-Ying L, Lin X, Qun J, et al. Evaluation of CT coronary artery angiography with 320-row detector CT in a high-risk population. Br J Radiol 2012; 85:562–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coats AJ. Ethical authorship and publishing. Int J Cardiol 2009;131:149–50 [DOI] [PubMed] [Google Scholar]
- 11.Dewey M, Zimmermann E, Deissenrieder F, Laule M, Dubel HP, Schlattmann P, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 2009;120:867–75 [DOI] [PubMed] [Google Scholar]
- 12.Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975;51:5–40 [DOI] [PubMed] [Google Scholar]
- 13.Leschka S, Wildermuth S, Boehm T, Desbiolles L, Husmann L, Plass A, et al. Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. Radiology 2006;241:378–85 [DOI] [PubMed] [Google Scholar]
- 14.Einstein AJ, Elliston CD, Arai AE, Chen MY, Mather R, Pearson GD, et al. Radiation dose from single-heartbeat coronary CT angiography performed with a 320-detector row volume scanner. Radiology 2010;254:698–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Husmann L, Leschka S, Desbiolles L, Schepis T, Gaemperli O, Seifert B, et al. Coronary artery motion and cardiac phases: dependency on heart rate—implications for CT image reconstruction. Radiology 2007;245:567–76 [DOI] [PubMed] [Google Scholar]
- 16.Yang L, Zhang Z, Fan Z, Xu C, Zhao L, Yu W, et al. 64-MDCT coronary angiography of patients with atrial fibrillation: influence of heart rate on image quality and efficacy in evaluation of coronary artery disease. AJR Am J Roentgenol 2009;193:795–801 [DOI] [PubMed] [Google Scholar]
- 17.Brodoefel H, Burgstahler C, Tsiflikas I, Reimann A, Schroeder S, Claussen C, et al. Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology 2008;247:346–55 [DOI] [PubMed] [Google Scholar]
- 18.Leschka S, Scheffel H, Husmann L, Gamperli O, Marincek B, Kaufmann PA, et al. Effect of decrease in heart rate variability on the diagnostic accuracy of 64-MDCT coronary angiography. AJR Am J Roentgenol 2008;190:1583–90 [DOI] [PubMed] [Google Scholar]
- 19.Baumüller S, Leschka S, Desbiolles L, Stolzmann P, Scheffel H, Seifert B, et al. Dual-source versus 64-section CT coronary angiography at lower heart rates: comparison of accuracy and radiation dose. Radiology 2009;253:56–64 [DOI] [PubMed] [Google Scholar]
- 20.Weustink AC, Neefjes LA, Kyrzopoulos S, van Straten M, Neoh ER, Meijboom WB, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology 2009;253:672–80 [DOI] [PubMed] [Google Scholar]
- 21.Cademartiri F, Mollet N, Runza G, Baks T, Midiri M, McFadden E, et al. Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ECG editing. AJR Am J Roentgenol 2006;186:634–8 [DOI] [PubMed] [Google Scholar]
- 22.Weustink A, Mollet N, Neefjes L, van Straten M, Neoh E, Kyrzopoulos S, et al. Preserved diagnostic performance of dual-source CT coronary angiography with reduced radiation exposure and cancer risk. Radiology 2009;252:53–60 [DOI] [PubMed] [Google Scholar]
- 23.Stolzmann P, Leschka S, Scheffel H, Krauss T, Desbiolles L, Plass A, et al. Dual-source CT in step-and-shoot mode: noninvasive coronary angiography with low radiation dose. Radiology 2008;249:71–80 [DOI] [PubMed] [Google Scholar]
- 24.Earls J, Berman E, Urban B, Curry C, Lane J, Jennings R, et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology 2008;246:742–53 [DOI] [PubMed] [Google Scholar]
- 25.Lell M, Marwan M, Schepis T, Pflederer T, Anders K, Flohr T, et al. Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol 2009;19:2576–83 [DOI] [PubMed] [Google Scholar]
- 26.Achenbach S, Marwan M, Schepis T, Pflederer T, Bruder H, Allmendinger T, et al. High-pitch spiral acquisition: a new scan mode for coronary CT angiography. J Cardiovasc Comput Tomogr 2009;3:117–21 [DOI] [PubMed] [Google Scholar]