Abstract
Objective
To compare hip fracture incidence in post-menopausal females who were differently stratified for the fracture risk according to bone mineral density and proximal femur geometry.
Methods
In a 5 year follow-up study, the hip fracture incidence in 729 post-menopausal females (45 of whom suffered from incident hip fracture) was assessed and compared. Forward logistic regression was used to select independent predictors of hip fracture risk, including age, age at menopause, height, weight, femoral neck bone mineral density (FNBMD), neck–shaft angle (NSA), hip axis length, femoral neck diameter and femoral shaft diameter as covariates. Fracture incidence was then calculated for the categories of young/old age, high/low FNBMD and wide/narrow NSA, which were obtained by dichotomising each hip fracture independent predictor at the value best separating females with and without a hip fracture.
Results
The hip fracture incidence of the whole cohort was significantly higher in females with a wide NSA (8.52%) than in those with a narrow NSA (3.51%). The combination of wide NSA and low FNBMD had the highest hip fracture incidence in the whole cohort (17.61%) and each age category. The combinations of narrow/wide NSA with low/high FNBMD, respectively, gave a significantly higher fracture incidence in older than in younger women, whereas women with a combined wide NSA and low FNBMD had no significantly different fracture incidence in young (14.60%) or old age (21.62%).
Conclusion
Our study showed that NSA is effective at predicting the hip fracture risk and that the detection in early post-menopause of a wide NSA together with a low FNBMD should identify females at high probability of incident hip fracture.
Hip fracture is the most clinically relevant osteoporotic fracture because it is expensive to treat and has severe consequences [1,2]. Bone mineral density (BMD) measurement at the hip is the strongest predictor of hip fracture [3]. Despite the statistically significant relationship between the femoral neck bone mineral density (FNBMD) and the risk of hip fracture [4], its ability to predict hip fragility fracture does not seem accurate enough for diagnostic purposes [5]. Therefore, hip fragility fracture predictors besides BMD are needed to identify people at risk for fracture prevention [6]. Among these predictors, proximal femur geometry (PFG) parameters have also been proposed, as bone shape adjusts the transmission of the impact forces through the bone, contributing, together with bone structure, to determine the effective stress within the bone [7]. This topic has been largely addressed by using dual energy X-ray absorptiometry (DXA) scans since Beck et al [8] showed the relationship between DXA bone mineral density and femoral neck strength, and Faulkner et al [9] described the association between the hip axis length (HAL) measured by DXA scans and the hip fracture risk. The PFG parameters that have been reported to predict effectively hip fracture independently of BMD are HAL and neck–shaft angle (NSA) [9-18].
The majority of these studies are nevertheless cross-sectional [10,12,13], and their results might not have such strong statistical evidence as those derived from longitudinal studies [9,17,18]. In addition, there are some discrepancies among authors about the best PFG parameter to predict the hip fracture risk [19-23]. The aims of this study were therefore to assess and compare in a longitudinal observation the ability of PFG parameters to separate post-menopausal females with hip fracture from those without fracture, and to assess how PFG parameters and BMD are associated with hip fracture incidence, and whether a combination of the two can identify subjects at higher risk of fracture.
Materials and methods
White Italian post-menopausal females who had undergone consecutive measurements of the FNBMD at our centre as outpatients for clinical reasons or to check and monitor post-menopausal BMD were enrolled for this prospective study. The females were followed up for 5 years. In the event of fracture, the time to fracture was recorded and those females were no longer followed up. Females were enrolled whether or not they were on medical treatment for osteoporosis.
Exclusion criteria were: Paget's bone disease, chronic kidney or lung disease, rheumatoid arthritis, long-term immobilisation, hyperparathyroidism, malignancies, chronic treatment with oral glucocorticoids and having undergone hip surgery. Previous fractures were not in the exclusion criteria except for femur fracture.
Data included in the study for each female at baseline observation were age, age at menopause, weight, height, FNBMD, NSA, HAL, femoral neck diameter (FND) and femoral shaft diameter (FSD). At the follow-up visit, females were questioned about the occurrence of hip fracture including both femoral neck and trochanter fracture. Only fractures due to falling while standing or walking were considered for the study. All fractures were verified by medical records and accepted for the study when radiographically confirmed. The BMD measure was taken at baseline using a pencil beam Norland XR-36® densitometer (Norland, Fort Atchinson, WI). The left hip was scanned in all subjects. For scan acquisition the patients' leg position was standardised by using the leg rotating fixture provided by the manufacturer. BMD was only measured at the femoral neck. The NSA measure was automatically generated by the device software. HAL was manually measured from the external side of the trochanter to the inner pelvic brim along the line of the femoral neck axis, which was automatically generated by the device software. FND was measured orthogonally to the hip axis at the narrow portion of the femoral neck. The FSD was measured 2 cm below the calcar, orthogonally to the femoral shaft axis. All measurements were taken using the dedicated options of the device software and were performed by a single operator (Figure 1). Using the Norland XR-36 densitometer, the measurement precision error of the PFG parameters and the FNBMD was validated and reported in previous papers by the present authors [10,24].
Figure 1.
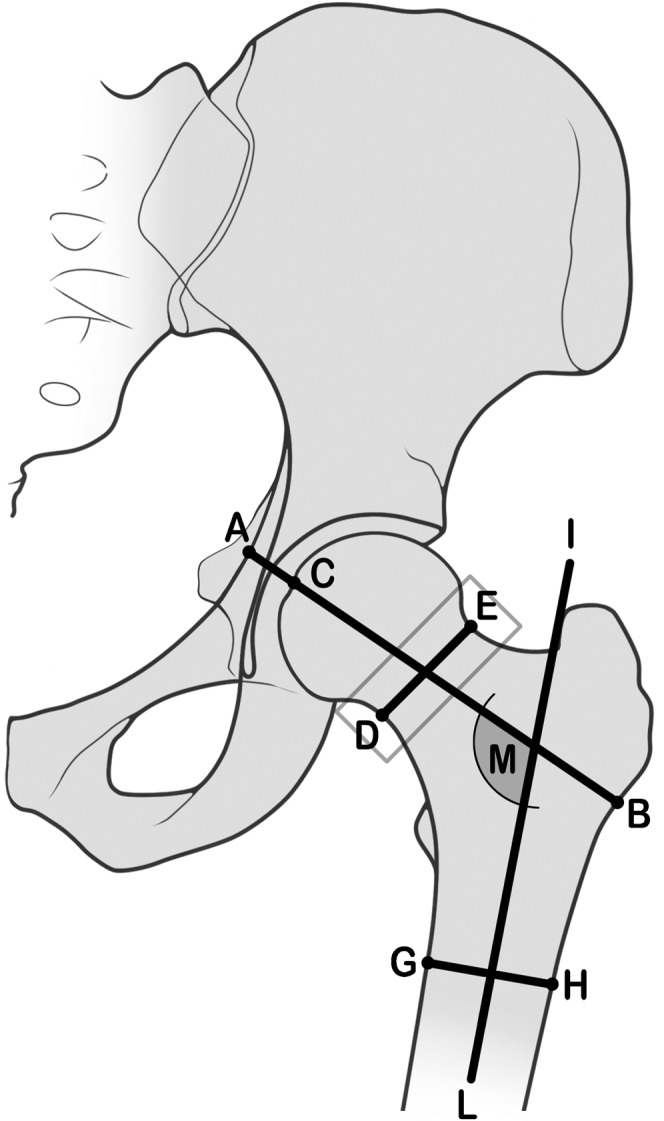
Measurements of geometric parameters from hip dual energy X-ray absorptiometry. AB, hip axis length from the external side of the trochanter to the inner pelvic brim. M, neck–shaft angle angle between the femoral neck and shaft axes (defined automatically by device software); DE, femoral neck diameter orthogonally to the hip axis at the narrow portion of the femoral neck; GH, femoral shaft diameter 2 cm below the calcar, orthogonally to the femoral shaft axis; IL, femoral shaft axis; CB, femoral neck axis (defined automatically by device software).
This study was approved by the local ethics committee.
Statistics
All continuous data were presented as mean and standard deviation of the mean; all categorical data were presented as frequency and incidence. The difference in the parameters between the age groups was tested by Student's unpaired t-test because the groups were normally distributed (Kolmogorov–Smirnov test) and homoscedastic (Levene test). Univariate logistic regression analysis was used to evaluate the influence of the studied predictors.
The significant predictors were dichotomised to be used for clinical purposes by the following method: sensitivity and specificity in separating fractured from not fractured women were calculated by receiver operating characteristic (ROC) curves for the whole range of values of each significant fracture predictor. The highest value of sensitivity plus specificity, when both were >50%, was then used to identify the fracture predictor value at which the cut-off was set to categorise the value range of the considered fracture predictor into two groups.
The multivariate logistic regression with Wald's forward method was used to select the predictors entering the best model for predicting hip fracture and to test their independence from each other. The covariates to obtain the best model were age, age at menopause, height and weight, FNBMD, NSA, HAL, FND and FSD. The forward logistic regression predicted probability (FPP) was also calculated from the multivariate best models. The areas under the ROC curves, having the fracture status as status variable and the tested predictors of the best logistic model as test variables, were calculated to assess the ability of the predictors to correctly classify subjects with and without hip fracture.
Specific fracture incidence rates per 1000 female-years and fracture incidence over the observational period were calculated for the whole population, and for the categories of fracture predictors in the best logistic model for fracture prediction: females older and younger than 65 years, those with low or high FNBMD (L-FNBMD or H-FNBMD), and those with wide or narrow NSA (W-NSA or N-NSA). Cut-off values (sensitivity and specificity) for the FNBMD were set at 0.638 g cm−2 (84.4 and 63.5%; corresponding to the T-score value of −2.59 for the female European population), at 123.97° for the NSA (71.1 and 55.0%) and at 65 years for age (71.1 and 66.7%).
Fisher's exact test was used to compare the incidence of hip fracture over the 5-year observation period between the groups of older/younger age, high/low FNBMD, wide/narrow NSA and those deriving from their combination.
Results
The present study analyses the data of 729 post-menopausal females aged 45–85 years, of whom 684 completed five years of follow-up and 45 were observed until the time of their hip fracture, making a total of 3512 female-years. Of these females, 469 were younger than 65 years (a total of 2310 female-years) and 260 were aged 65 years or older (a total of 1202 female-years). 45 female had their first hip fracture (21 on the left side and 24 on the right) during the observation period; 13 of these were younger than 65 and 32 were 65 or older. The estimated hip fracture incidence in the whole population was 12.8 per 1000 female-years female [95% confidence interval (CI) 9.1–16.5]. The number of females eligible for the study lost to follow-up was 249.
Compared with the age distribution of the females living in the district of Bologna (age 45–64=55.2%; age 65–85=43.8%) [25], in our cohort there were more females aged 45–64 (60.7%) and fewer females aged 65–85 years (39.4%). The biological data of the females studied are reported in Table 1 for the whole population, and for the two groups of younger females (younger than 65 years) and older females (65 years or older). Older age was associated with significantly lower FNBMD and height, narrower NSA, longer HAL, wider FND and FSD, and a significantly higher body mass index (BMI).
Table 1. Baseline characteristics of the post-menopausal females studied.
| Covariate | Whole population(n=729) | Age <65(n=469) | Age ≥65(n=260) | Unpaired t-test p-value(age <65 vs age ≥65) |
| Age (years) | 62.2±8.47 | 56.7±5.4 | 71.6±4.3 | 0.001 |
| Age at menopause (years) | 48.7±4.7 | 48.7±4.4 | 48.7±5.3 | 0.972 |
| Height (cm) | 159.6±6.2 | 160.1±6.2 | 158.8±6 | 0.006 |
| Weight (kg) | 62.3±9.9 | 62.0±10.1 | 62.8±9.7 | 0.274 |
| BMI (kg m−2) | 24.8±7.9 | 24.2±3.5 | 24.9±3.5 | 0.007 |
| FNBMD (g cm−2) | 0.676±0.102 | 0.701±0.100 | 0.632±0.091 | 0.001 |
| NSA (degrees) | 123.6±5.5 | 123.9±5.4 | 123.0±5.6 | 0.035 |
| HAL (cm) | 10.6±7.1 | 10.6±0.7 | 10.7±0.7 | 0.026 |
| FND (cm) | 3.3±0.2 | 3.2±0.2 | 3.3±0.2 | 0.001 |
| FSD (cm) | 3.3±0.2 | 3.3±0.2 | 3.4±0.2 | 0.001 |
BMI, body mass index; FNBMD, femoral neck bone mineral density; FND, femoral neck diameter; FSD, femoral shaft diameter; HAL, hip axis length; NSA, neck–shaft angle.
In the whole population, age, longer HAL, lower FNBMD and wider NSA, separately tested as covariates in the univariate logistic regression, were statistically significant risk factors for hip fracture, whereas height, weight, age at menopause, FND, FSD and BMI were not associated with fracture risk. In older females significant predictors for the hip fracture risk were age, FNBMD and NSA, whereas in younger women they were FNBMD, NSA, HAL, weight and BMI (Table 2).
Table 2. Odds ratio [OR; 95% confidence interval (CI)] of the hip fracture associated with each one of the considered fracture predictors separately tested as a covariate in the univariate logistic regression.
| Covariate | OR (95% CI) |
||
| Whole population | Age <65 years | Age ≥65 years | |
| Age | 1.158 (1.109–1.209)a | 1.091 (0.973–1.224) | 1.339 (1.209–1.482)a |
| Height | 0.989 (0.942–1.038) | 1.024 (0.937–1.119) | 0.991 (0–932–1.053) |
| Weight | 0.970 (0.938–1.003) | 0.932 (0.869–0.999)a | 0.937 (0.934–1.013) |
| BMI | 0.954 (0.910–1.000) | 0.892 (0.801–0.993)a | 0.962 (0.911–1.016) |
| Age at menopause | 1.013 (0.949–1.081) | 1.059 (0.917–1.224) | 1.000 (0.932–1.072) |
| FNBMD | 0.987 (0.983–0.991)a | 0.987 (0.980–0.993)a | 0.990 (0.985–0.995)a |
| NSA | 1.126 (1.064–1.191)a | 1.317 (1.150–1.509)a | 1.091 (1.022–1.165)a |
| HAL | 1.788 (1.199–2.665)a | 2.375 (1.210–4.660)a | 1.364 (0.826–2.225) |
| FND | 2.219 (0.638–7.718) | 1.808 (0.166–19.665) | 1.318 (0.287–6.048) |
| FSD | 2.699 (0.820–8.886) | 3.657 (0.420–31.815) | 0.937 (0.204–4.304) |
BMI, body mass index; FNBMD, femoral neck bone mineral density; FND, femoral neck diameter; FSD, femoral shaft diameter; HAL, hip axis length; NSA, neck–shaft angle.
ap<0.05.
The independent predictors of hip fracture, checked by the multivariate logistic regression model with Wald's forward method, were age [odds ratio (OR) 1.127, 95% CI 1.076–1.1182], NSA (OR 1.145, 95% CI 1.075–1.219) and FNBMD (OR 0.991, 95% CI 0.987–0.996).
The area under the ROC curve, with FPP as the test variable calculated from the best logistic model, was 0.884 (standard error 0.021).
Table 3 shows the 5-year fracture incidence and the specific fracture incidence rate per 1000 female-years for the selected categories of age, FNBMD, NSA and their possible combinations calculated in the whole population. Females with L-FNBMD, W-NSA or older age had a higher specific fracture incidence rate and significantly higher 5 year fracture incidence than females, respectively, with H-FNBMD, N-NSA or younger age.
Table 3. Fracture incidence rate per 1000 female-years and the incidence of fracture during 5 years of follow-up in the whole population according to the selected categories of FNBMD, NSA and age, and the possible combinations of FNBMD and NSA categories.
| Risk factors | Subjects exposed to the risk |
Hip fractures |
||
| n | n | 5 year incidence (%) | 1000 female-year incidence rate (95% CI) | |
| Age <65 years | 469 | 13 | 2.77 a | 5.5 (2.5–8.5) |
| Age ≥65 years | 260 | 32 | 12.31 a' | 26.1 (17.2–35.1) |
| H-FNBMD | 445 | 7 | 1.57 b | 3.2 (0.8–5.5) |
| L-FNBMD | 284 | 38 | 13.38 b' | 29.0 (19.9–38.1) |
| N-NSA | 342 | 12 | 3.51 c | 7.2 (3.1–11.2) |
| W-NSA | 387 | 33 | 8.52 c' | 16.7 (11.1–22.4) |
| N-NSA+H-FNBMD | 215 | 2 | 0.93 d | 1.9 (−0.7–4.4) |
| N-NSA+L-FNBMD | 127 | 10 | 7.87 e | 15.7 (6.1–25.4) |
| W-NSA+H-FNBMD | 230 | 5 | 2.17 f | 4.3 (0.5–8.2) |
| W-NSA+L-FNBMD | 159 | 28 | 17.61 g | 35.2 (22.4–48.0) |
CI, confidence interval; H-FNBMD, higher femoral neck bone mineral density; L-FNBMD, lower femoral neck bone mineral density; N-NSA, narrower neck–shaft angle; ns, not significant; W-NSA, wider neck–shaft angle.
Fisher's exact test for differences in % of incident hip fractures in 5 years: a vs a', p=0.001; b vs b', p=0.001; c vs c', p=0.008; d vs f, ns; e vs g, p=0.014; f vs g, p=0.001; d vs e, p=0.001; e vs f, p=0.014. BMD cut-off value=0.638 g cm–2, corresponding to the T-score value of −2.6; NSA cut-off value=123.97°; age cut-off value=65 years.
Females with W-NSA+L-FNBMD had the highest hip fracture incidence, which was significantly higher than that of females with N-NSA+L-FNBMD or W-NSA+H-FNBMD.
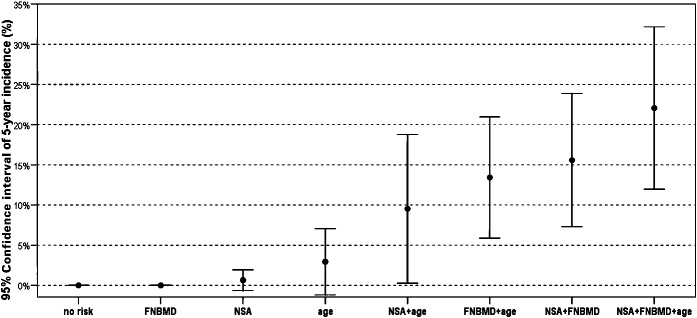
The specific fracture incidence rate per 1000 female-years and the within-5-year incidence of hip fracture for the possible combinations of the selected FNBMD and NSA categories are shown in Table 4, separately considering the younger and older age groups. In both age groups the 5 year fracture incidence of females with W-NSA+L-FMBMD was significantly higher than that of females of the same age group with the other possible combinations of FNBMD and N-NSA categories. Among females older than 65, those having N-NSA+L-FNBMD and W-NSA+H-FNBMD had a statistically significant higher 5 year hip fracture incidence than those with N-NSA+H-FNBMD. The combinations of N-NSA+L-FNBMD or W-NSA+L-FNBMD gave significantly higher 5 year hip fracture incidence in older females than in younger ones, whereas no statistically significant difference was found between age groups for females with W-NSA+L-FNBMD (Table 4; Figure 2).
Table 4. Specific fracture incidence rate per 1000 female-years and 5 year incidence of fracture in the younger and older female age groups according to the various combinations of the selected FNBMD and NSA categories.
| Risk factors | Subjects exposed to the risk |
Hip fracture |
||
| n | n | 5 year incidence (%) | 1000 female-year incidence rate (95% CI) | |
| N-NSA+H-FNBMD+age<65 years | 152 | 0 | 0 | 0 |
| N-NSA+L-FNBMD+age<65 years | 53 | 0 a | 0 | 0 |
| W-NSA+H-FNBMD+age<65 years | 181 | 1 a | 0.55 | 1.1 (1.1–3.9) |
| W-NSA+L-FNBMD+age<65 years | 83 | 12 b | 14.6 | 31.4 (13.9–48.9) |
| N-NSA+H-FNBMD+age≥65 years | 63 | 2 | 3.17 | 6.5 (−2.5–15.5) |
| N-NSA+L-FNBMD+age≥65 years | 74 | 10 c, d | 13.51 | 30.9 (12.0–49.7) |
| W-NSA+H-FNBMD+age≥65 years | 49 | 4 a, d | 8.16 | 17.2 (0.0–33.9) |
| W-NSA+L-FNBMD+age≥65 years | 74 | 16 b, e | 21.62 | 49.4 (25.7–73.0) |
CI, confidence interval; H-FNBMD, higher femoral neck bone mineral density; L-FNBMD, lower femoral neck bone mineral density; N-NSA, narrower neck–shaft angle; NS, not significant; W-NSA, wider neck–shaft angle.
Fisher's exact test for differences in % of incident hip fractures in 5 years: a=ns compared with the H-FNBMD+N-NSA of the same age group; b=p<0.001 compared with H-FNBMD+N-NSA of the same age group; c=p<0.033 compared with H-FNBMD+N-NSA of the same age group; d=p<0.005 compared with the corresponding FNBMD+NSA categories of age <65; e=ns compared with the corresponding FNBMD+NSA group of age <65.
Figure 2.
5 year incidence of hip fracture in post-menopausal females according to the various combinations of risk factors. H-FNBMD, higher femoral neck bone mineral density; L-FNBMD, lower femoral neck bone mineral density; N-NSA, narrow neck–shaft angle; W-NSA, wider neck–shaft angle. No risk=N-NSA+H-FNBMD+age <65 years. FNBMD=N-NSA+L-FNBMD+age <65 years. NSA= W-NSA+H-FNBMD+age <65 years. Age=N-NSA+H-FNBMD+age ≥65 years. NSA+age=W-NSA+H-FNBMD+age ≥65 years. FNBMD+age=N-NSA+L-FNBMD+age ≥65 years. NSA +FNBMD=W-NSA+L-FNBMD+age <65 years. NSA+FNBMD+age= W-NSA+L-FNBMD+age ≥65 years; CI, confidential interval.
Discussion
In this observational study we evaluated the association of PFG parameters with hip fracture relative risk and hip fracture incidence in post-menopausal females referred for DXA, over a 5 year period. The reason why we wanted to investigate this topic was to explore further the relationship between PFG parameters and the risk of hip fracture in a prospective study, the results of which would provide stronger statistical evidence than that of the cross-sectional studies generally used to investigate this topic. In addition, our intent was to evaluate the variations of the hip fracture incidence in groups of post-menopausal females having different degrees of fracture risk according to the presence/absence of low FNBMD and/or risk value of the proximal femur parameters.
We found that lower FNBMD, longer HAL and wider NSA, irrespective of other shared risk factors, were effective risk factors for hip fracture, whereas FND and FSD were not.
The association of NSA and HAL with hip fracture risk is not surprising, for biomechanical reasons. In fact, from a biomechanical point of view, the wider the NSA and the longer the HAL, the greater the force absorbed by the proximal femur when falling on the lateral side [26], because of a longer moment arm. Nevertheless, this explanation of the relationship between DXA-measured PFG parameters and hip fracture risk has some limitations. DXA-measured NSA and HAL, in fact, may be different from the true NSA and HAL because of the angle of femoral anteversion that can modify the real measure of the two PFG parameters in their frontal projection [27]. In addition, the hip moment arm at ground impact may not be the same as that estimated during DXA measurement, as the effective angulations of NSA on ground impact vary in relation to hip rotation when falling. Despite these limitations, the results of our study seem to indicate that wider NSA and longer HAL measured by DXA analysis represent unfavourable geometric conditions for hip resistance to stress upon ground impact when falling [15], in accordance with some cross-sectional [28] and prospective studies [17,18], and in disagreement with others [19-23].
Discrepancies among authors may reflect ethnic differences in the populations studied and/or biases of patient positioning during DXA scanning, which occurs more frequently in cross-sectional studies observing subjects after recent surgery. The magnification error of fan-beam equipment may also have played a role [29].
Our data also highlight that NSA is the only PFG parameter that predicts hip fracture independently of FNBMD. Although in the whole population its ability to distinguish females with hip fracture from those without is less than that of FNBMD, NSA is essential to improve the ability of the latter parameter to classify correctly females with and without hip fracture [30-33]. The hip fracture incidence in our population rose markedly with age in accordance with population-based studies [30,34], although the hip fracture incidence in our cohort was higher than that reported in those studies. This might be due to the fact that our study included only females referred for DXA, whose fracture risk is presumably higher than that of the general population [34-38].
The fracture incidence was lower in younger females than in older ones, or, considering the whole age range, in females with high BMD or narrow NSA rather than those with low BMD or wide NSA.
These results are not actually new, because the high FNBMD protective effect of hip fracture is well established, and also the inverse relationship of NSA width with the hip fracture risk has already been reported by most (although not all) studies [12,18].
When considering females with the combination of two different FNBMD and NSA categories, we found that the combination of L-FNBMD and W-NSA was associated with the highest percentage of incident hip fractures within an age group, which was significantly higher than that of the females with the remaining combinations of FNBMD and NSA categories. Interestingly, comparing younger with older females, only the hip fracture incidence associated with the combination of L-FNBMD+W-NSA was not significantly different between these two age groups, whereas it was significant considering H-FNBMD+W-NSA or L-FNBMD+N-NSA. The novel aspect of this study is the finding of no statistical difference in hip fracture incidence between post-menopausal osteoporotic females over 65 years old, with or without W-NSA, and those under 65 years old, but with W-NSA. It is of particular interest for clinical purposes because it shows that a subgroup of young post-menopausal females likely to have a high hip fracture incidence can be detected among those having low FNBMD simply by measuring the NSA.
If confirmed, this should lead to considering the measurement of NSA for hip fracture prevention in younger post-menopausal females without clinical risk factors for hip fracture who had a FNBMD measurement, which, although in contrast with the WHO fracture risk assessment (FRAX®) case finding strategy [39,40], is not precluded in females desiring treatment if their BMD is low [32]. These subjects should benefit from our finding, as the contemporary measurement of NSA should provide an opportunity to reassess their fracture probability and the relevant need for treatment. Conversely, in our study the measurement of NSA did not add information to the measurement of FNBMD to assess the hip fracture incidence in older females, probably because of the increased role of age-related factors in the elderly, although older females with L-FNBMD+W-NSA have the highest hip fracture incidence of all.
Our study has some limitations. Its design is not ideal for an observational study because of the small number of recruited subjects, particularly in terms of fractures. It is not population based, and its results, coming from a selected population not exactly reflecting the characteristics of the general population, prevented generalisability. It may have a selection bias because of the loss to follow-up, despite having tried to minimise this error by the recruitment of consecutively selected females. In addition, it lacks comparison with radiographic measurement of the PFG, and it also fails to assess possible fracture risk factors (such as tendency to fall, way of falling, bone quality etc.) that may interact with those studied.
Nevertheless, it shows that NSA is the best predictor of the hip fracture risk among the measured PFG parameters and the only one independent of age and BMD. Irrespective of age it does not predict hip fractures better than FNBMD, but it can improve hip fracture risk evaluation when used contemporarily. Finally, in early post-menopause a wide NSA could lead to identifying females with a higher probability of incident hip fracture among those with low FNBMD when contemporarily measured. Therefore, the measurement of NSA should be further considered in longitudinal studies to improve hip fracture prediction following menopause and to select among younger post-menopausal females those at a higher risk of incident hip fracture.
Acknowledgments
We wish to thank Mr Keith Smith for linguistic help and Mariapia Cumani for anatomical illustration.
References
- 1.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 1999;353:878–82 [DOI] [PubMed] [Google Scholar]
- 2.Haentjens P, Autier P, Barette M, Boonen S. The economic cost of hip fractures among elderly women: a one-year, prospective, observational cohort study with matched-pair analysis. J Bone Joint Surg Am 2001;83:493–500 [PubMed] [Google Scholar]
- 3.Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, et al. Bone density at various sites for prediction of hip fractures. Lancet 1993;341:72–5 [DOI] [PubMed] [Google Scholar]
- 4.Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner, et al. BMD at multiple sites and risk of fracture of multiple types: long-term results from the study of osteoporotic fractures. J Bone Miner Res 2003;18:1947–54 [DOI] [PubMed] [Google Scholar]
- 5.Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, et al. Assessment of fracture risk. Osteoporos Int 2005;16:581–9 [DOI] [PubMed] [Google Scholar]
- 6.De Laet C, Odén A, Johansson H, Johnell O, Jönsson B, Kanis JA. The impact of the use of multiple risk indicators for fracture on case-finding strategies: a mathematical approach. Osteoporos Int 2005;16:313–18 [DOI] [PubMed] [Google Scholar]
- 7.Gregory JS, Aspden RM. Femoral geometry as a risk factor for osteoporotic hip fracture in men and women. Med Eng Phys 2008;30:1275–86 [DOI] [PubMed] [Google Scholar]
- 8.Beck TJ, Ruff CB, Warden KE, Scott WW, Jr, Rao GU. Predicting femoral neck strength from bone mineral data: a structural approach. Invest Radiol 1990;25:6–18 [DOI] [PubMed] [Google Scholar]
- 9.Faulkner KG, Cummings SR, Black D, Palermo L, Glüer CC, Genant HK. Simple measurement of femoral geometry predicts hip fracture: the study of osteoporotic fractures. J Bone Miner Res 1993;8:1211–17 [DOI] [PubMed] [Google Scholar]
- 10.Gnudi S, Ripamonti C, Lisi L, Fini M, Giardino R, Giavaresi G. Proximal femur geometry to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. Osteoporos Int 2002;13:69–73 [DOI] [PubMed] [Google Scholar]
- 11.Gnudi S, Ripamonti C, Gualtieri G, Malavolta N. Geometry of proximal femur in the prediction of hip fracture in osteoporotic women. Br J Radiol 1999;72:729–33 [DOI] [PubMed] [Google Scholar]
- 12.Alonso CG, Curiel MD, Carranza FH, Cano RP, Peréz AD. Femoral bone mineral density, neck-shaft angle and mean femoral neck width as predictors of hip fracture in men and women. Osteoporos Int 2000;11:714–20 [PubMed] [Google Scholar]
- 13.Crabtree N, Lunt M, Holt G, Kröger H, Burger H, Grazio S, et al. Hip geometry, bone mineral distribution, and bone strength in European men and women: the EPOS study. Bone 2000;27:151–9 [DOI] [PubMed] [Google Scholar]
- 14.Frisoli A, Jr, Paula AP, Pinheiro M, Szejnfeld VL, Delmonte Piovezan R, Takata E, et al. Hip axis length as an independent risk factor for hip fracture independently of femural bone mineral density in Caucasian elderly Brazilian women. Bone 2005;37:871–5 [DOI] [PubMed] [Google Scholar]
- 15.Bergot C, Bousson V, Meunier A, Laval-Jeantet M, Laredo JD. Hip fracture risk and proximal femur geometry from DXA scans. Osteoporos Int 2002;13:542–50 [DOI] [PubMed] [Google Scholar]
- 16.Boonen S, Koutri R, Dequeker J, Aerssens J, Lowet G, Nijs J, et al. Measurement of femoral geometry in type I and type II osteoporosis: differences in hip axis length consistent with heterogeneity in the pathogenesis of osteoporotic fractures. J Bone Miner Res 1995;10:1908–12 [DOI] [PubMed] [Google Scholar]
- 17.Duboeuf F, Hans D, Schott AM, Kotzki PO, Favier F, Marcelli C, et al. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: the EPIDOS Study. J Bone Miner Res 1997;12:1895–902 [DOI] [PubMed] [Google Scholar]
- 18.Kaptoge S, Beck TJ, Reeve J, Stone KL, Hillier TA, Cauley JA, et al. Prediction of incident hip fracture risk by femur geometry variables measured by hip structural analysis in the study of osteoporotic fractures. J Bone Miner Res 2008;23:1892–904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Center JR, Nguyen TV, Pocock NA, Eisman JA. Volumetric bone density at the femoral neck as a common measure of hip fracture risk for men and women. J Clin Endocrinol Metab 2004;89:2776–82 [DOI] [PubMed] [Google Scholar]
- 20.El-Kaissi S, Pasco JA, Henry MJ, Panahi S, Nicholson JG, Nicholson GC, et al. Femoral neck geometry and hip fracture risk: the Geelong osteoporosis study. Osteoporos Int 2005;16:1299–303 [DOI] [PubMed] [Google Scholar]
- 21.Center JR, Nguyen TV, Pocock NA, Noakes KA, Kelly PJ, Eisman JA, et al. Femoral neck axis length, height loss and risk of hip fracture in males and females. Osteoporos Int 1998;8:75–81 [DOI] [PubMed] [Google Scholar]
- 22.Faulkner KG, Wacker WK, Barden HS, Simonelli C, Burke PK, Ragi S, et al. Femur strength index predicts hip fracture independent of bone density and hip axis length. Osteoporos Int 2006;17:593–9 [DOI] [PubMed] [Google Scholar]
- 23.Dretakis EK, Papakitsou E, Kontakis GM, Dretakis K, Psarakis S, Steriopoulos KA. Bone mineral density, body mass index, and hip axis length in postmenopausal Cretan women with cervical and trochanteric fractures. Calcif Tissue Int 1999;64:257–8 [DOI] [PubMed] [Google Scholar]
- 24.Gnudi S, Sitta E. Clinical risk factor evaluation to defer postmenopausal women from bone mineral density measurement. J Clin Densitom 2005;8:199–205 [DOI] [PubMed] [Google Scholar]
- 25.National InstituteforStatistic. Bologna −14 censimento popolazione 2001.Rome,IT:ISTAT,2006 Jan Available from: http://www3.istat.it/dati/catalogo/20071029_07gc_bologna.pdf. [Google Scholar]
- 26.Wang Q, Teo JW, Ghasem-Zadeh A, Seeman E. Women and men with hip fractures have a longer femoral neck moment arm and greater impact load in a sideways fall. Osteoporos Int 2009;20:1151–6 [DOI] [PubMed] [Google Scholar]
- 27.Wong JCH, Ong B. Evaluation of femur angle abduction/adduction and bone mineral density. J Clin Densitom 2005;8:472–5 [PubMed] [Google Scholar]
- 28.Pulkkinen P, Partanen J, Jalovaara P, Jämsä T. Combination of bone mineral density and upper femur geometry improves the prediction of hip fracture. Osteoporos Int 2004;15:274–80 [DOI] [PubMed] [Google Scholar]
- 29.Pocock NA, Noakes KA, Majerovic Y, Griffiths MR. Magnification error of femoral geometry using fan beam densitometers. Calcif Tissue Int 1997;60:8–10 [DOI] [PubMed] [Google Scholar]
- 30.Johnell O, Kanis A, Oden A, Johansson H, De Laet C, Delmas P, et al. A predictive value of BMD for hip and other fractures. J Bone Miner Res 2005;20:1185–94 [DOI] [PubMed] [Google Scholar]
- 31.Schott AM, Cormier C, Hand D, Favier F, Hausherr E, Dargent-Molina P, et al. How hip and whole body bone mineral density predict hip fracture in elderly women. The EPIDOS prospective study. Osteoporos Int 1998;8:247–54 [DOI] [PubMed] [Google Scholar]
- 32.Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster LY, Bourgstrom F, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 2008;19:399–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grisso JA, Kelsey JL, Strom DB, Chiu GY, Maislin G, O'Brien L, et al. , and the Northeast Hip fracture Study Group. Risk factors for fall as a cause of hip fracture in women. N Engl J Med 1991;324:1326–31 [DOI] [PubMed] [Google Scholar]
- 34.Siris ES, Brenneman SK, Barret-Connor E, Miller PD, Sajjan S, Berger ML, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int 2006;17:565–74 [DOI] [PubMed] [Google Scholar]
- 35.Hui SL, Slemenda CW, Johnston CC., Jr Age and bone mass as predictors of fracture in a prospective study. J Clin Invest 1988;81:1804–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chang KP, Center JR, Nguyen TV, Eisman JA. Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo osteoporosis epidemiology study. J Bone Miner Res 2004;19:532–6 [DOI] [PubMed] [Google Scholar]
- 37.Shott AM, Kassai Koupai B, Hans D, Dargent-Molina P, Ecochard R, Bauer DC, et al. Should age influence the choise of quantitative bone assessment technique in elderly women? The EPIDOS study. Osteoporos Int 2004;15:196–203 [DOI] [PubMed] [Google Scholar]
- 38.Piscitelli P, Gimigliano F, Gatto S, Marinelli A, Gimigliano A, Marinelli P, et al. Hip fractures in Italy: 2000–2005 extension study. Osteoporos Int 2010;21:1323–30 [DOI] [PubMed] [Google Scholar]
- 39.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 2008;19:385–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A. Case finding for the management of osteoporosis with FRAX: assessment and intervention thresholds for the UK. Osteoporos Int 2008;19:1395–408 Erratum in: Osteoporos Int 2009;20:499–502. [DOI] [PubMed] [Google Scholar]