Abstract
Objective
The purpose of the present study was to evaluate the role of 68-gallium-1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-1-Nal3-octreotide (68Ga-DOTA-NOC) positron emission tomography CT (PET-CT) in carotid body chemodectomas (CBCs).
Methods
: 5 patients with known CBCs (conventional imaging and angiography) were evaluated retrospectively (3 males, 2 females; mean age 36.6 years). All underwent PET-CT after injection of 148 MBq (4 mCi) of 68Ga-DOTA-NOC.
Results
: At baseline there were four bilateral CBCs and one unilateral CBC with an additional glomus tympanicum and bilateral glomus jugulare tumour in these five patients. All these lesions showed intense uptake on 68Ga-DOTA-NOC PET-CT. Apart from these known lesions, additional tumours were detected in three patients; glomus jugulare in one, aortic body tumour and multiple abdominal paragangliomas in another and unsuspected vertebral metastasis in the last. Overall it led to a change in management in 3 of the 5 patients (60%).
Conclusion
: 68Ga-DOTA-NOC PET-CT is a promising non-invasive imaging modality in the detection and characterisation of CBCs.
Chemodectomas are rare tumours of the chemoreceptor system. Carotid body chemodectoma (CBC) is the most common variety, arising at the carotid bifurcation and accounting for >50% of head and neck paragangliomas [1]. These are slow-growing neoplasms which can cause pressure changes in surrounding structures, including the hypoglossal and vagus nerves and the sympathetic chain. Common symptoms include hoarseness, cough and dysphagia. The tumours are very vascular, and approximately 5% may become malignant [2]. Bilateral CBCs are known to have a high familial incidence [3]. The preferred method of treatment is surgery, but this can become challenging at times because of the highly vascular nature of the tumour, which is often densely adherent to the carotid bifurcation.
Ultrasound, CT or MRI have been used for imaging CBCs. Colour-flow duplex sonography can show a hypervascular mass nestled in the carotid bifurcation, which differentiates it from a relatively non-vascular mass, and is now the most widely utilised non-invasive method [4]. Arteriography was once the diagnostic tool of choice for demonstrating a hypervascular mass arising in the crotch of the carotid bifurcation. It is still essential for identifying large tumours that may be easily embolised as a preparatory step for surgical excision [5]. CT along with CT angiography (CTA) can demonstrate head and neck vessels, tumour angiogenesis and the tumour's relationship with the surrounding blood vessels [6].
Apart from the various anatomical imaging modalities, certain functional imaging techniques have also been utilised for the diagnosis and localisation of such lesions, including 111-indium-pentetreotide and meta-iodo-benzyl-guanidine (MIBG) labelled with 123I/131I [7]. 18-fluorodeoxyglucose positron emission tomography (18FDG PET) represents another tool in the investigation of these neoplasms, but its sensitivity is reported to be low in slowly growing tumours with low metabolic activity like the paragangliomas [8]. 68-Gallium-1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-1-Nal3-octreotide (68Ga-DOTA-NOC) is a PET tracer for somatostatin receptor scintigraphy (SRS) and has been evaluated in a wide variety of neuroendocrine tumours [9]. However, there is no published literature evaluating its role in CBCs. In the present study we share our experience of imaging CBCs with this radiotracer.
Methods and materials
Patients
This is a retrospective review of data from 5 patients (3 males, 2 females; mean age 36.6 years) with known CBCs who underwent 68Ga-DOTA-NOC PET-CT at our institute between January 2007 and August 2010. Results of conventional imaging (CT and CTA) were available for all patients, and data analysis was carried out after approval from the institutional ethics committee.
68Ga-DOTA-NOC synthesis
68Ga-DOTA-NOC was synthesised as described in the literature [10] and as briefly summarised here. 30–50 mCi 68Ge/68Ga generator was eluted using 0.1 M hydrochloric acid (HCl). The eluent was loaded onto a cation exchange cartridge to pre-concentrate and pre-purify it (using 80% acetone/0.15 M HCl). Purified 68Ga (half-life, 68.3 min; β+ 88%; Eβ+ max, 1.9 MeV) was directly eluted with 97.7% acetone/0.05 M HCl into the reaction vial containing 30–50 µg of DOTA-D-Phe(1)-Tyr(3)-octreotide (DOTANOC). Synthesis was carried out at approximately 126 °C for 10–15 min. This was followed by the removal of a labelled peptide from an unlabelled peptide using a reverse phase C-18 column and 400 µl of ethanol. This was further diluted with normal saline and passed through a 0.22 µm filter to sterilise it in preparation for injection.
68Ga-DOTA-NOC PET-CT acquisition
The studies were carried out with a dedicated PET-CT scanner (BiographTM 2, Siemens, Erlangen, Germany). A dose of 148 MBq (4 mCi) of 68Ga-DOTA-NOC was injected intravenously. After a 30–45 min uptake period the patients were taken for PET-CT. Intravenous contrast (70–100 ml) was used for one patient (Ultravist® 370; Bayer Schering Pharma, Berlin, Germany). The image was acquired using a matrix of 512×512 pixels and pixel size of 1 mm. After CT, three-dimensional (3D) PET acquisition was done from skull to mid thighs. PET data were acquired using matrix of 128×128 pixels with a slice thickness of 1.5 mm. CT-based attenuation correction of the emission images was employed. PET images were reconstructed by the iterative method ordered subset expectation maximisation (OSEM; two iterations and eight subsets). After completion of PET acquisition, the reconstructed attenuation-corrected PET images, CT images and fused images of matching pairs of PET and CT images were reviewed.
Image analysis
Images were evaluated by two nuclear medicine physicians with expertise in evaluating 68Ga-DOTA-NOC PET-CT studies. Scans were examined for any non-physiological focal areas of increased tracer uptake and all such foci were anatomically correlated on the CT and fused PET-CT images. Standardised uptake values and size were calculated for all the lesions. Histopathology and/or conventional imaging served as the reference standard against which results of 68Ga-DOTA-NOC PET-CT were verified.
Results
Details of patient findings are summarised in Table 1. Four patients had known bilateral CBCs, while one patient had a unilateral CBC (Figures 1–5). A left glomus tympanicum and bilateral glomus jugulare tumours were also present in these patients (Table 1). 68Ga-DOTA-NOC PET-CT turned out to be positive in all the five patients with intense tracer uptake noted in the CBCs and other lesions, resulting in 100% sensitivity for these tumours. Also, there was the discovery of additional lesions in three of the five patients, previously unknown on conventional imaging studies. In patient 3 there was a focus of intense tracer uptake in the right jugular canal suggestive of a glomus jugulare tumour with equivocal conventional imaging results (Figure 3). This was later confirmed on MRI on follow-up imaging at 8 months while a contrast-enhanced PET-CT showed intense enhancement in both the CBC and glomus jugulare. In patient 4, who had bilateral carotid body masses and a left glomus tympanicum, additional tumours were discovered in the mediastinum (aortic body tumour) and in the abdomen (multiple sympathetic chain paragangliomas) (Figure 4). Finally, in patient 5 there were multiple vertebral metastases in the dorsal and lumbar vertebrae which were previously not known (Figure 5). For all lesions, CT and PET-CT were concordant in two (Figures 4 and 5) and were discordant in three of the five patients.
Table 1. Patients' characteristics and findings of 68-gallium-1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-1-Nal3-octreotide (68Ga-DOTA-NOC) positron emission tomography (PET)-CT.
| Patient number | Age (years) | Sex | Clinical presentation | 68Ga-DOTA-NOC PET-CT | Carotid body chemodectoma | Size (cm) | SUVmax | Other lesions | Additional lesion by PET-CT |
| 1 | 40 | M | Left painless neck mass | Positive | Left | Lt 2.6×3.5 | Lt 15.5 | None | No |
| 2 | 28 | F | Bilateral painless neck mass | Positive | Bilateral | Rt 2.4×3.8 | Rt 14.4 | None | No |
| Lt 1.6×1.8 | Lt 23.8 | ||||||||
| 3 | 33 | M | Right painless neck mass | Positive | Bilateral | Rt 2.5×2.9 | Rt 6.5 | Right jugular foramen | Yes |
| Lt 1.5×1.6 | Lt 8.7 | [glomus tumour (1×1cm; SUVmax 1.4)] | |||||||
| 4 | 37 | F | Bilateral painless neck mass with tinnitus and left facial nerve palsy | Positive | Bilateral | Rt 2.1×1 | Rt 51 | Left glomus tympanicum (SUVmax 89.1) | Yes |
| Lt 4.87×4 | Lt 61 | Aortic body (SUVmax 72) paraganglionoma (SUVmax 27.3, 11) | |||||||
| 5 | 45 | M | Bilateral painless neck masses and tinnitus | Positive | Bilateral | Rt 3.2×4.1 | Rt 40 | Bilateral glomus jugulare tumour (Rt., SUVmax 68; Lt., SUVmax 30) | Yes |
| Lt 6.2×8.5 | Lt 36 | Vertebral metastasis at D5 and L2 (SUVmax 27 and 54) |
D5, fifth dorsal vertebra; F, female; L2, second lumbar vertebra; Lt, left; M, male; Rt, right; SUVmax, standardised uptake value maximum.
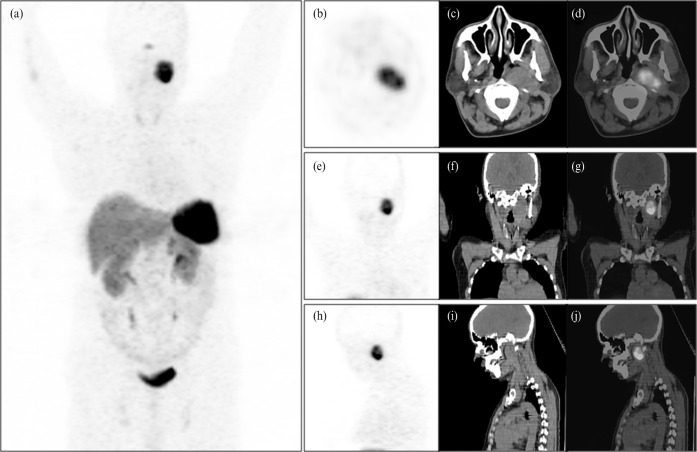
Figure 1.
68-Gallium-1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-1-Nal3-octreotide (68Ga-DOTA-NOC) positron emission tomography (PET) maximum intensity projection image (a) of a 40-year-old male patient showing an area of intensely increased radiotracer uptake in the left side of the neck apart from the normal distribution of the tracer in the pituitary gland, spleen, liver, kidneys, ureter and the urinary bladder. The transaxial (b), coronal (e) and sagittal (h) PET, CT (c, f, i) and PET-CT (d, g, j) images show the left-sided carotid body chemodectoma (2.6×3.5 cm) displaying intense tracer uptake (standardised uptake value maximum, 15.5).
Figure 5.
A whole body maximum intensity projection image (a) is shown on the extreme right, showing multiple areas of increased tracer uptake in the bilateral carotid body, bilateral glomus jugulare, central thoracic and abdominal region. The midline lesions in thorax and abdomen were the vertebral metastasis involving the fifth dorsal and second lumbar vertebra, respectively. Positron emission tomography (PET)-CT transaxial sections through the neck region showing the bilateral carotid body chemodectomas (b) and bilateral glomus jugulare (c) with intense tracer uptake CT (d) and PET-CT (e) images show sclerotic lesions involving the fifth dorsal vertebrae with intense tracer uptake.
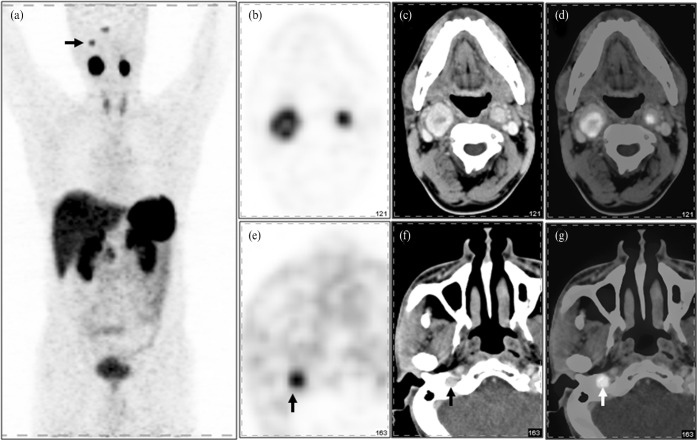
Figure 3.
Maximum intensity projection image (a) of a 33-year-old male shows abnormal areas of increased tracer uptake in the neck region bilaterally (right>left) and in the right side of the base of skull (arrow shows glomus jugulare). Grouped positron emission tomography (PET) (b), contrast-enhanced CT (c) and contrast-enhanced PET-CT (d) images show the presence of bilateral carotid body chemodectomas with intense tracer uptake [right standardised uptake value maximum (SUVmax), 6.5; left SUVmax, 8.7]. Also shown is increased tracer uptake (vertical arrow) in the region of the right jugulare foramen in PET (e), contrast-enhanced CT (f) and contrast-enhanced PET-CT (g) images, which was later confirmed to be a glomus jugulare tumour (SUVmax, 1.4).
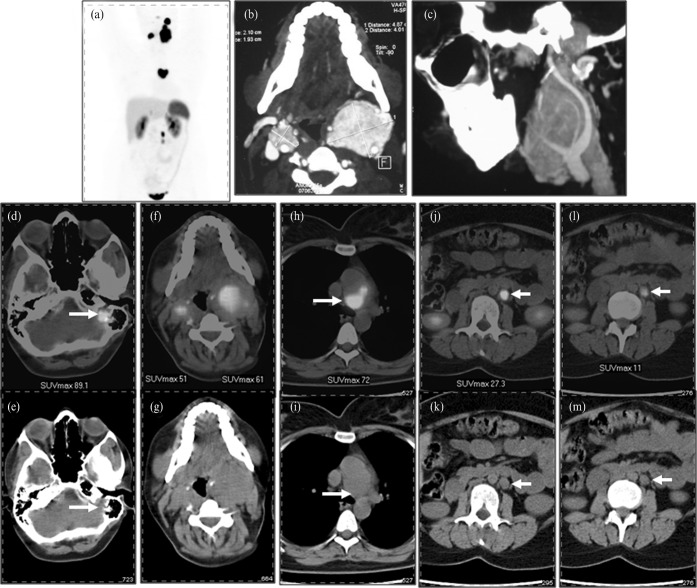
Figure 4.
Whole body maximum intensity projection image (a) of a 37-year-old female patient who presented with bilateral painless neck masses, tinnitus and left-sided facial nerve palsy. Multiple areas of intense tracer uptake in the head and neck region were seen on positron emission tomography CT. The two areas in the neck were diagnosed as bilateral carotid chemodectomas (f, g) while a smaller area of tracer activity above the left carotid tumour (arrow) was identified as glomus tympanicum (d, e). Also noted are a large area of intense tracer uptake in the central thoracic cavity (h) and two small areas of tracer uptake in the abdomen medial to the left kidney (j, l) (arrow). The former was confirmed as an aortic body tumour while the latter were paragangliomas. Corresponding CT images are shown in the lower row (i, k, m). A contrast-enhanced CT (b) of the neck was performed, which showed bilateral enhancing masses and confirmed the vascular origin of the masses, and a carotid angiogram (c) was also undertaken which revealed splaying of the carotids, a classic finding of such cases.
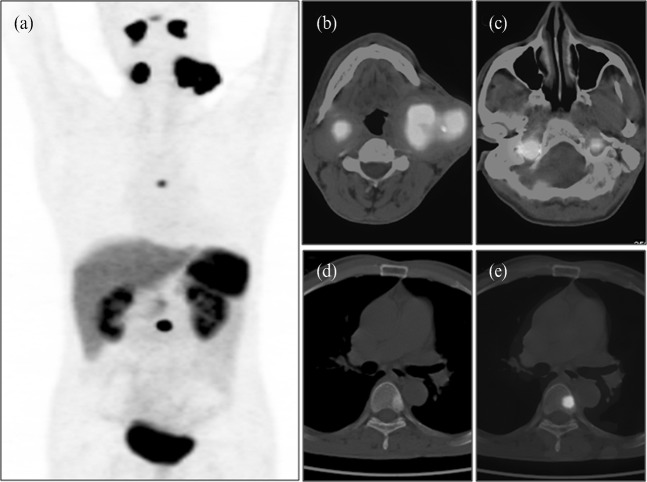
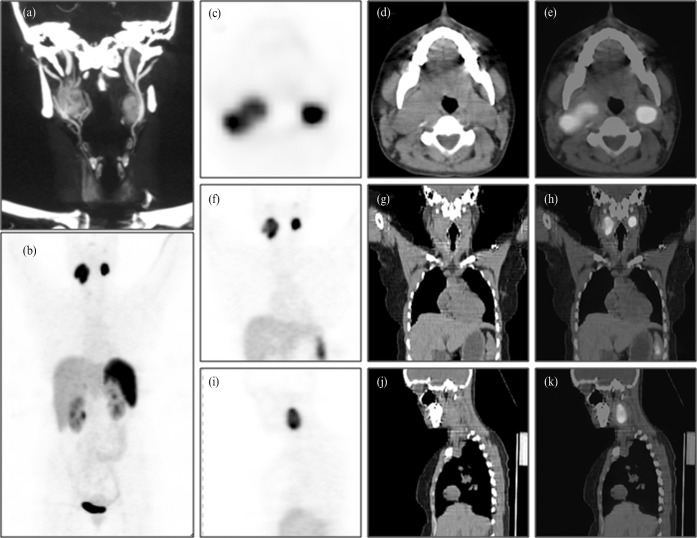
Figure 2.
Contrast-enhanced CT angicgram (a) of a 28-year-old female patient showing bilateral enhancing carotid masses. Maximum intensity projection image (b) shows intense tracer activity in both sides of the neck (right>left). Grouped positron emission tomography (PET) (c, f, i), CT (d, g, j) and PET-CT (e, h, k) images show bilateral enlarged neck masses (carotid body chemodectomas) at the level of the carotid bifurcation with increased tracer uptake [right standardised uptake value maximum (SUVmax), 14.4; left SUVmax, 23.8].
Discussion
Surgery remains the mainstay of treatment for these groups of tumours. However, two important questions need to be addressed before surgery: whether the tumour is benign or malignant and mapping the extent of the disease. Conventional imaging modalities like ultrasound, Doppler, CT and MRI play an important role in the diagnosis of CBCs and can detect lesions in the head and neck region and other sites with reasonably good sensitivity. However, they tend to miss small lesions at unexpected sites and distant metastasis in cases of malignant CBC. 111-Indium-pentetreotide (OctreoscanTM; Covidien, Dublin, Ireland), a single-photon emission CT (SPECT) agent for SRS, was considered the gold standard functional investigation for imaging paragangliomas, with an imaging sensitivity of 94% [7]. However, it is not without potential drawbacks. Smaller lesions can be missed because of the limited SPECT resolution; the high physiological uptake in the liver and spleen may mask their involvement; and results are generally available only after 48 h. Radiolabelled MIBG (123I/131I) is another useful functional imaging modality in the localisation of these tumours. However, its sensitivity and specificity is quite low since MIBG concentrates only in functioning paragangliomas.
68Ga-DOTA-NOC is a promising PET-based radiotracer for somatostatin receptor imaging [9]. In comparison with SPECT imaging, PET has a higher spatial resolution (3–6 mm vs 10–15 mm) that enables the detection of smaller lesions and also facilitates quantitative assessment of tracer uptake. In the present study all known CBCs and other lesions were demonstrated with PET-CT with the discovery of additional unsuspected lesions as well. However, the size of the tumours was fairly large (range 1–8.5 cm) in this series of patients. In patient 3, a right glomus jugulare was identified which was previously unsuspected because of the absence of local symptoms. Early detection, as in this case, provides the opportunity to treat with a curative intent as these tumours are known to enlarge and cause significant local symptoms and debility. In patient 4, apart from the bilateral CBCs and glomus tympanicum, other sites of abnormal tracer activity were also found in the mediastinum (aortic body tumour) and multiple sites in the abdomen (abdominal paragangliomas), significantly altering the patient management. Patient 5 had known large bilateral CBCs and glomus jugulare, which showed intense tracer uptake on PET-CT. Additional lesions were detected in the form of multiple vertebral metastasis (dorsal and lumbar), thereby changing the stage and the management strategy from a curative to palliative intent. It must also be stressed that, in addition to the detection and localisation of such tumours, 68Ga-DOTA-NOC PET-CT provides the opportunity to demonstrate the in vivo expression of somatostatin receptors, which can be exploited for treatment with peptide-based radioreceptor therapy.
This study is not without limitations. Only five patients with CBCs were available to be analysed. This number is too small to make any generalised statement. However, given the rarity of these tumours, it will be difficult to enrol a larger patient population at a single centre. Secondly, contrast-enhanced PET-CT was not done in all patients, which can be a one-stop shop for such patients. The retrospective nature of the present study might have also influenced the interpretation of PET-CT findings.
Conclusion
Our results demonstrate that 68Ga-DOTA-NOC PET-CT is a promising non-invasive imaging modality in the detection and characterisation of CBCs. Unexpected discovery of additional previously unknown lesions has a bearing on the management of patients, as they radically change the strategy from a more local to a generalised approach.
References
- 1.Pellitteri PK, Rinaldo A, Myssiorek D, Gary Jackson C, Bradley PJ, Devaney KO, et al. Paragangliomas of the head and neck. Oral Oncol 2004;40:563–75 [DOI] [PubMed] [Google Scholar]
- 2.Pacheco-Ojeda L. Malignant carotid body tumors: report of three cases. Ann Otol Rhinol Laryngol 2001;110:36–40 [DOI] [PubMed] [Google Scholar]
- 3.Rush BF., Jr Familial bilateral carotid body tumors. Ann Surg 1963;157:633–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barry R, Pienaar A, Pienaar C, Browning NG, Nel CJ. Duplex Doppler investigation of suspected vascular lesions at the carotid bifurcation. Ann Vasc Surg 1993;7:140–4 [DOI] [PubMed] [Google Scholar]
- 5.Litle VR, Reilly LM, Ramos TK. Preoperative embolization of carotid body tumors: When is it appropriate? Ann Vasc Surg 1996;10:464–8 [DOI] [PubMed] [Google Scholar]
- 6.Deng Y, Wang XM, Wu LB, Sun C, Duan YH, Cheng ZP, et al. Significance of the preoperative guidance of dual-source CT in carotid body tumor. Chin Med J (Engl) 2010;123:2816–19 [PubMed] [Google Scholar]
- 7.Kwekkeboom DJ, van Urk H, Pauw BK, Lamberts SW, Kooij PP, Hoogma RP, et al. Octreotide scintigraphy for the detection of paragangliomas. J Nucl Med 1993;34:873–8 [PubMed] [Google Scholar]
- 8.Brink I, Hoegerle S, Klisch J, Bley TA. Imaging of pheochromocytoma and paraganglioma. Fam Cancer 2005;4:61–8 [DOI] [PubMed] [Google Scholar]
- 9.Prasad V, Ambrosini V, Hommann M, Hoersch D, Fanti S, Baum RP. Detection of unknown primary neuroendocrine tumours (CUP-NET) using (68)Ga-DOTA-NOC receptor PET/CT. Eur J Nucl Med Mol Imaging 2010;37:67–77 [DOI] [PubMed] [Google Scholar]
- 10.Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, et al. Processing of generator-produced 68Ga for medical application. J Nucl Med 2007;48:1741–8 [DOI] [PubMed] [Google Scholar]