Abstract
This study explored pathways through which hurricane-related stressors affected the psychological functioning of elementary school aged children who survived Hurricane Katrina. Participants included 184 mothers from the New Orleans area who completed assessments one year pre-disaster (Time 1), and one and three years post-disaster (Time 2 and Time 3, respectively). Mothers rated their children’s behavior problems at Time 3 only (n = 251 children; 53.0% male; Mean age: 10.19 years, SD = 1.68 years). A path analytic model indicated that hurricane-related stressors were associated with increased maternal psychological distress and school mobility in the first post-disaster year, which were associated with higher child internalizing and externalizing symptoms three years post-disaster. Mediation analysis indicated that hurricane-related stressors were associated with child symptoms indirectly, through their impact on maternal psychological distress. Findings underscore the importance of interventions that boost maternal and child mental health and support children through post-disaster school transitions.
Keywords: natural disasters, elementary school students, low-income families, maternal psychological distress, child behavior problems
Predicting Low-Income Mothers’ Reports of their Children’s Mental Health Three Years after Hurricane Katrina
Children who were exposed to Hurricane Katrina faced a range of stressors, including the loss of loved ones and threats to their physical safety (Madrid & Grant, 2008; Osofsky, Osofsky, & Harris, 2007). In the years since the disaster, many have faced ongoing stressors associated with caregiver mental health problems, residential instability, and multiple school transitions (Osofsky et al., 2007; Pane, McCaffrey, Tharp-Taylor, Asmus, & Stokes, 2006; Spell et al., 2008). Not surprisingly, a growing body of research has documented the adverse mental health consequences of Hurricane Katrina on children (e.g., Abramson, Park, Stehling-Ariza, & Redlener, 2010; Scheeringa & Zeanah, 2008). The purpose of this study was to investigate the longer-term impact of hurricane exposure on low-income mothers’ reports of their elementary school aged children’s psychological functioning. We explored both the direct effects of hurricane exposure on child functioning, as well as the indirect effects of maternal psychological distress and disruptions in schooling.
Impact of Hurricane Katrina on Children’s Psychological Functioning
Children exposed to Hurricane Katrina and other natural disasters are at increased risk for short and long-term psychological distress, including symptoms of depression, post-traumatic stress (PTS), separation anxiety, and oppositionality (e.g., Abramson et al., 2010; La Greca, Silverman, Lai, & Jaccard, 2010; Scheeringa & Zeanah, 2008). According to several studies (e.g., McLaughlin et al., 2010; Weems et al., 2010), elevated levels of child psychological distress (e.g., symptoms of PTS and emotional disturbance) have persisted in the years following Hurricane Katrina. For example, in a study of school-aged children (n = 283) in which households that had been displaced or affected greatly by Hurricane Katrina were randomly selected from FEMA and census databases, Abramson and colleagues (2010) found that 37.5% had been given a mental health diagnosis since the hurricane (per parent reports), and that 30.0% were still suffering from the diagnosed condition four years after the hurricane. Another study (n = 576) that used a probability sample of residents of the areas affected by Hurricane Katrina (recruited by either random-digit-dialing or through a random selection of families applying for assistance from the American Red Cross) documented higher rates of parent-reported child psychosocial problems (e.g., conduct problems, peer relation problems) and associated parent-reported functional impairment as measured by the Strengths and Difficulties Questionnaire (SDQ) 18–27 months (15.1%) and 36–39 months (11.5%) post-Katrina (McLaughlin et al., 2010), which was notably higher than the pre-Katrina estimates of elevated SDQ status (4.2%).
It is important to note, however, that children’s reactions to the difficult circumstances caused by Hurricane Katrina have varied widely. Although many have exhibited symptoms of distress, others have remained remarkably unscathed (e.g., La Greca et al., 2010; McLaughlin et al., 2010). Research on post-disaster functioning has revealed a dose-response relationship, in which psychological symptoms vary in proportion to disaster exposure (e.g., La Greca et al., 2010; Scheeringa & Zeanah, 2008). Disaster exposure has relevance to children’s psychological functioning during and in the immediate aftermath of the hurricane as well as in the longer-term disaster recovery process (Abramson et al., 2010; Bonanno, Brewin, Kaniasty, & La Greca, 2010; La Greca et al., 2010; McLaughlin et al., 2010). With regard to the immediate impact, increased exposure to the disaster (e.g., being in locations hardest hit by the storm, being stranded in shelters) increased the likelihood of experiencing threatening and potentially traumatic events, thereby leading to increased risk of psychological distress. The association between disaster exposure and children’s post-disaster psychological functioning is more complex as it is likely mediated by a range of factors (Bonanno et al., 2010). Considering children’s ecological contexts and the multiple spheres of influence on their functioning, including child, family, school and community contexts (Bronfenbrenner, 1977), provides a useful framework for understanding the mechanisms by which disasters impact children’s long-term functioning (Weems & Overstreet, 2008).
Family context
Children’s post-disaster functioning occurs within the context of the family system, particularly parent-child relationships. Thus, children’s experiences of disasters and their aftermath are affected by their parents’ mental health (Scheeringa & Zeanah, 2008) and the consistency and warmth of care parents are able to provide both during and after a disaster. For example, in a convenience sample of preschool aged children and their caregivers (n = 70) who were living in the New Orleans metropolitan area at the time of Hurricane Katrina, Scheeringa and Zeanah (2008) found that timing of caregiver symptom onset moderated the strength of association between caregiver and child symptoms. Specifically, stronger correlations were observed between children’s and caregivers’ posttraumatic stress disorder symptoms among caregivers with new (i.e., post-Katrina) symptoms as compared to caregivers with pre-existing or no symptoms, although all symptomatology was assessed post-Katrina. Hurricane-related stressors can lead to increases in parents’ distress which, in turn, can decrease their parenting efficacy and capacity to cope with the demands of parenting, thereby negatively influencing child psychological functioning (Abramson et al., 2010; Scaramella, Sohr-Preston, Callahan, & Mirabile, 2008). For example, using a sample that combined two separate groups of pre-and post-Katrina low-income mothers and their 2-year-old children (n = 102) recruited from Head Start centers, Scaramella and colleagues (2008) found that financial strain and neighborhood violence were associated with higher levels of maternal depressed mood, which was associated with lower levels of parenting efficacy and subsequent increased levels of child internalizing and externalizing problems.
Thus, particularly in the context of the challenges presented by natural disasters, difficulties experienced by the parent can negatively affect child psychological functioning (Proctor et al., 2007; Scaramella et al., 2008). Proctor and colleagues (2007) gathered observational parent-child play data prior to the Northridge earthquake and parent-reported symptoms of parental stress and child distress 8 months after the earthquake within a sample of two-parent families (n = 117) with children (ages 4 to 5 years). The effect of the earthquake’s impact on child distress was mediated (fully for boys and partially for girls) by parental stress. In addition to parental stress, maternal depression is associated with reduced parenting sensitivity, warmth, disciplinary consistency, efficacy, and responsiveness (Field, 2010; Scaramella, et al., 2008; Weinberg, Olson, Beeghly, &Tronick, 2006) and heightened risk for child emotional and behavioral problems (e.g., Van der Molen, Hipwell, Vermeiren, & Loeber, 2011). Although parent psychological functioning has been examined in relation to child functioning following disasters (e.g., Proctor et al., 2007; Scheeringa & Zeanah, 2008), we know of no studies that have included parent psychological functioning assessed pre-disaster, which is necessary to control for parents’ pre-existing psychological vulnerabilities and reduce bias introduced by retrospective reporting.
School context
Children’s post-disaster psychological functioning may also be impacted by disruptions associated with hurricane exposure, such as moves and changes in schools. In the aftermath of Hurricane Katrina, many families were forced to relocate in response to the devastation of residences and local economies (Gault, Hartmann, Jones-DeWeever, Werschkul, & Williams, 2005; Groen & Polivka, 2009). Consequently, approximately 196,000 school-aged children (kindergarten through grade 12) were displaced from Louisiana following Hurricane Katrina (Pane, et al., 2006). Residential mobility can be extremely disruptive to both children and their parents, as it often entails the loss of family and friendship networks, additional financial burdens, and the adjustment to new social, educational, and occupational demands. Indeed, residential instability is associated with decreased social support, increased stress, and increased symptoms of psychological distress (e.g., Magdol, 2002; Magdol & Bessel, 2003).
Although residential mobility often prompts changes in schools, even those children who remained in New Orleans faced school disruptions, or school mobility, as the hurricane seriously damaged or destroyed educational facilities and led to numerous school closures (Liu, Fellowes, & Mabanta, 2006; Pane, et al., 2006). For example, approximately one year after Hurricane Katrina made landfall, less than one third of the New Orleans metropolitan area public schools were in operation (Liu et al., 2006). School-related disruptions rendered by hurricane exposure can have negative effects on children’s psychosocial functioning. Indeed, changes in school enrollment outside of those required by the school system (i.e., outside of normative transitions from elementary school to middle school) increase children’s risk for academic problems (Gruman, Harachi, Abbott, Catalano, & Fleming, 2008; Mantzicopoulos & Knutson, 2000) and psychosocial problems (Gilman, Kawachi, Fitzmaurice, & Buka, 2003; Hoglund & Leadbeater, 2004), even when controlling for other factors commonly associated with mobility (e.g., poverty, family structure).
School disruptions are often associated with a loss of peer, teacher, and mental health support. School resources, including relationships with classmates, teachers and other staff members, can serve as a comforting source of support and stability for children following disaster (Pina et al., 2008; Prinstein, La Greca, Vernberg, & Silverman, 1996). Children who lack that support due to changes in schooling may be more vulnerable to post-disaster psychological and behavioral problems than children with stable schooling. In the aftermath of Hurricane Katrina, mental health providers working in Louisiana school-based health centers that received a greater number of displaced students reported larger increases in psychosocial problems and mental health needs than providers working in schools that received lower numbers of displaced students (Madrid et al., 2008). Additionally, given that schools serve as a vital provider of services, (Farmer, Burns, Phillips, Angold, & Costello, 2003; Yeh et al., 2002), school changes likely meant disruptions in the receipt of mental health care.
Moreover, school disruptions may be a marker of a broader constellation of cumulative stressors. That is, as children transition in and out of different schools and communities, their vulnerability to psychological symptoms rises sharply (e.g., Sameroff, Bartko, Baldwin, & Seifer, 1998). Disruptions and losses associated with Hurricane Katrina occurred over a protracted period, meaning that their impact might not be detected in assessments of children’s short-term post-disaster psychological functioning. Rather, it might be necessary to take a longer-term perspective to detect to the effects of post-disaster disruption on children’s mental health.
Present Study
The purpose of this study was to investigate the impact of hurricane exposure on the psychological functioning of children who survived Hurricane Katrina. We took an ecological systems approach to understanding how the hurricane could impact children’s functioning, focusing on maternal mental health and school mobility in a low-income sample of primarily African American mothers. We sought to clarify the mechanisms by which disasters can negatively impact children’s long-term psychological functioning by examining the impact of maternal psychological health and school disruptions. We hypothesized that hurricane-related stress exposure would affect children’s internalizing and externalizing symptoms three years after the storm both directly and indirectly, through its influence on (a) maternal psychological distress and (b) school mobility (defined as the number of schools the child had attended in the school year following the hurricane).
The current dataset, which spans one year pre-disaster to three years post-disaster, permitted a stronger test of causal pathways than previous studies, most of which have been fully cross-sectional and have examined a shorter period of post-disaster data. Because data were not collected on children’s functioning until the three-year post-disaster assessment, the child outcomes component of the present study is cross-sectional. Nonetheless, the larger longitudinal design focused on maternal well-being afforded the opportunity to include pre-and post-Katrina data on maternal functioning across three time points, which enabled us to control for maternal pre-disaster functioning and to explore how changes in maternal distress from pre- to post-disaster related to mother-reported child functioning three years following Hurricane Katrina. Moreover, previous research has found that higher pre-disaster psychological distress is predictive of both higher post-disaster distress (Weems et al., 2007) and greater disaster exposure (Green et al., 2012), and we were able to take this pre-existing vulnerability into account.
Although the majority of studies on children’s post-disaster functioning have not included pre-disaster data, there are a few notable exceptions. For example, using a longitudinal sample of school-aged children, Weems and colleagues (2007) found that children’s pre-Katrina negative affect predicted disaster-related PTS symptoms and generalized anxiety disorder symptoms (pre-disaster n = 173; post-disaster n = 53; retention rate: 30.1%). La Greca and colleagues (La Greca, Silverman, & Wasserstein, 1998) used a prospective longitudinal sample and child-, teacher-, and peer-reported data, and found that child pre-disaster psychosocial and academic functioning were associated with child PTS symptoms 3 months after Hurricane Andrew and that child pre-disaster anxiety predicted PTS symptoms 7 months post-disaster (baseline n = 138; 3-month n = 92; 7-month n = 74; overall retention rate: 53.6%). These studies have highlighted the importance of pre-disaster symptoms in predicting children’s post-disaster psychological functioning, but have not focused on the role of contextual factors, including the influence of maternal distress and school-related disruptions.
The current study adds to the extant body of literature on children’s adaptation post-disasters through its focus on a multiply at-risk population and its relatively high retention rate. The sample of low-income, young, African American single mothers were especially vulnerable to the impact of Hurricane Katrina (e.g., Brewin, Andrews, & Valentine, 2007). Indeed, the racial, class, and gender disparities that were present before Hurricane Katrina in the New Orleans area rendered lower-income, African American families particularly vulnerable to the impact of the storm (Jones-DeWeever & Hartmann, 2006; Rhodes et al., 2010, Ruscher, 2006). Young, single mothers were at increased risk of clinically elevated psychological symptoms following Hurricane Katrina (e.g., Kessler et al., 2008; Rhodes et al., 2010) and they were exposed to child-related stressors during the storm, such as parent-child separations, which further exacerbated their risk for psychological distress (Lowe, Chan, & Rhodes, 2011). Furthermore, and consistent with research on the multiple co-occurring risk factors associated with living in poverty (Yoshikawa, Aber, & Beardslee, 2012), families headed by low-income, African American single women have faced a number of additional stressors since the storm, including financial barriers (e.g., Galea, Tracy, Norris, & Coffey, 2008; Jones-deWeever, 2008) and concerns about lack of occupational opportunities, crime, and safety (Kaiser Family Foundation, 2010). These interrelated stressors may further increase mothers’ risk for psychological distress and place children in these families at heightened risk for adjustment disorders and mental health problems (Biglan, Flay, Embry, & Sandler, 2012; Yoshikawa et al., 2012). Given the dearth of previous Katrina research focused on large samples of young, single, African American mothers and the increased vulnerabilities of the children in this group, our sample addresses a gap in the existing literature and an important area of study.
Method
Procedure
Institutional Review Boards from MDRC and the Principal Investigators’ universities (Harvard University, Princeton University, and University of Massachusetts Boston) approved the study. Participants were initially part of a larger study examining whether performance-based scholarships to attend community college affected the academic achievement, health, and well being of low-income parents (Richburg-Hayes et al., 2009). To be eligible for the study, students had to be between the ages of 18 and 34, have at least one dependent child under 19 years of age, have a household income under 200 percent of the federal poverty level, and have a high school diploma or equivalent. Beginning in 2004, students were recruited through a general marketing and outreach campaign, which included flyers, newspaper and radio announcements, and oral presentations in mandatory orientation and testing sessions for incoming freshman. The larger study had multiple sites throughout the United States, including three community colleges in the New Orleans area, from which participants were recruited in 2004–2005. At baseline (i.e., upon enrollment in the study and prior to random assignment) participants provided primarily demographic information (e.g., age, race, number of children).
By the time Hurricanes Katrina and Rita made landfall, on August 29, 2005 and September 24, 2005, respectively, 492 participants had been enrolled in the program long enough to complete a 12-month, pre-disaster follow-up survey (Time 1). Trained interviewers conducted the survey via phone, which included a measure of psychological distress. Given the impact of Hurricane Katrina on the New Orleans area, and on the three community colleges the participants had attended, the New Orleans sample was dropped from the larger scholarship study. However, the investigators mobilized efforts to follow the New Orleans participants as an investigation of how the hurricane affected their psychosocial functioning and physical health.
After Hurricanes Katrina and Rita, between May 2006 and March 2007, extensive efforts were made to locate participants. The researchers first made use of contact information, including addresses, phone numbers, and email addresses for each participant and another person who would likely know of their whereabouts, collected at Time 1. Additional contact information was obtained from participants’ community colleges and person locator databases. Through these efforts, 402 of the 492 participants from Time 1 (81.7%) were successfully located and surveyed. Trained interviewers administered the post-disaster survey (Time 2), which included the same questions as the 12-month follow-up survey, as well as a module of hurricane experiences. Approximately three years after the hurricanes, between April 2009 and March 2010, trained researchers administered an additional follow-up survey over the phone (Time 3). The Time 3 survey included the same measures as the previous surveys. In addition, participants reported the ages of each of their children, completed a measure of psychological functioning for each of their children between the ages of 4 and 17 years, and answered questions assessing the impact of the hurricanes on each of their children’s schooling. Of the 402 participants who completed the Time 2 survey, 345 (85.8%; 70.1% of the Time 1 sample) also completed the Time 3 survey. A small number of male participants (n = 14) was dropped due to our focus on the impact of maternal mental health on child functioning. Participants were compensated for their time with gift cards at each time point ($20 at Time 1, $50 at Times 2 and 3).
Participants
The current study included mothers of children who had been in elementary school at the time of Hurricane Katrina. Of the 331 mothers who completed the study, 185 (55.9%; 37.6% of the Time 1 sample) fit this criterion. An additional mother was dropped from the study, since her one school-aged child, a 13-year old daughter, had missed an entire year of school in the aftermath of the hurricane. The final sample consisted of 184 mothers of school-aged children, ages 8- to 13-years at Time 3 (5- to 10-years at the time Hurricane Katrina hit). All of the mothers were community college students at baseline and were living in areas affected by Hurricane Katrina at the time of the hurricane. Over half (53.8%) were living in areas affected by Hurricane Rita when it made landfall less than a month later. On average, mothers provided data on 1.36 school-aged children (SD = 0.67); 132 (71.17%) had one school-aged child, 41 (22.3%) two school-aged children, and 11 (5.9%) three or more school-aged children. The total number of children in the sample about whom information was obtained was 251. Demographic data for the 184 mothers and the 251 children are listed in Table 1. In light of previous findings indicating that child sex and age are related to post-disaster psychological functioning (e.g., La Greca et al., 2010; Lonigan et al., 1994; Vernberg, La Greca, Silverman, & Prinstein, 1996; Weems et al., 2010), we included these as covariates in our analysis.
Table 1.
Demographic data on for mothers (N = 184) and children (N = 251)
| M / % | SD / n | N | |
|---|---|---|---|
| Mothers | |||
| Age at baseline | 26.10 | 3.44 | 184 |
| Race / Ethnicity | 178 | ||
| non-Hispanic Black | 86.5% | 154 | |
| non-Hispanic White | 7.9% | 14 | |
| Hispanic | 2.8% | 5 | |
| Other race/ethnicity | 2.8% | 5 | |
| Number of school-aged children | 1.36 | .67 | 184 |
| Time 1 Psychological distress | 5.55 | 4.41 | 184 |
| Time 2 Psychological distress | 6.37 | 5.15 | 184 |
| Hurricane-related stressors | 3.80 | 3.19 | 182 |
| Children | |||
| Age | 10.19 | 1.68 | 251 |
| Gender | 251 | ||
| Female | 47.0% | 118 | |
| Male | 53.0% | 133 | |
| Number of schools attended | 2.08 | .98 | 241 |
| Internalizing subscale | 3.06 | 3.81 | 245 |
| Externalizing subscale | 7.64 | 8.32 | 245 |
Measures
Hurricane-related stressors
Sixteen questions assessed stressors experienced during the hurricanes and the week that followed. The questions were drawn from a larger survey of the demographic and health characteristics, evacuation and hurricane experiences, and future plans of Hurricane Katrina evacuees. The Washington Post, the Kaiser Family Foundation, and the Harvard School of Public Health jointly designed the scale (Brodie, Weltzien, Altman, Blendon, & Benson, 2006). Participants indicated whether they had experienced the following as a result of the hurricanes: 1) lacked enough fresh water to drink, 2) lacked enough food to eat, 3) felt their life was in danger, 4) lacked necessary medicine, 5) lacked necessary medical care, 6) had a family member who lacked necessary medical care, 7) lacked knowledge of safety of children, and 8) lacked knowledge of safety of other family members. These questions were asked for both Hurricane Katrina and Hurricane Rita, yielding 16 items in total. A composite score with the count of affirmative responses to these items was created (KR-20 = .84).
Maternal psychological distress
The K6 scale, a six-item screening measure of nonspecific psychological distress (Kessler et al., 2003), was used to assess the mothers’ psychological distress at each time point. This scale has been shown to have good psychometric properties; for example, two independent validation studies have shown the K6 to have an area under the receiver operator characteristic curve between 0.86 and 0.89 in predicting DSM-IV mood disorders that meet the severity criteria for the Substance Abuse and Mental Health Services Administration’s definition of serious mental illness (Furukawa, Kessler, Slade, & Andrews, 2003; Kessler et al., 2002; Kessler et al., 2003). In addition, the K6 has been used in previous research on the psychological functioning of Hurricane Katrina survivors (e.g., Galea et al., 2007). Participants rated items (e.g., “During the past 30 days, about how often did you feel so depressed that nothing could cheer you up?”) on a 5-point Likert-type scale ranging from 0 (none of the time) to 4 (all the time). Reliability of the K6 scale in this study was Cronbach’s alpha of .70 at Time 1, .80 at Time 2, and .80 at Time 3.
School mobility
At Time 3, mothers indicated how many schools each of their children attended in the school year following the hurricane. Eighty children (33.2%) attended one school; 83 (34.4%), two schools; 60 (24.9%), three schools; and 18 (7.5%), four or more schools.
Child behavioral problems
The Behavioral Problems Index (BPI; Peterson & Zill, 1986) was used to assess children’s psychological functioning at Time 3. Consisting of 32 items, the BPI was developed for children ages 4 to 17, and was used in the National Survey of Children, the National Health Interview Survey, and the National Longitudinal Survey of Youth (Zill, 1990). It includes several items from the widely used Child Behavior Checklist (Achenbach & Edelbrock, 1986), and has been shown to have acceptable reliability and internal consistency (Chase-Lansdale, Mott, Brooks-Gunn, & Phillips, 1991; Peterson & Zill, 1986). Previous research has found the BPI to discriminate between youth who have and have not received clinical treatment (Zill, 1990), and between youth from high- and low-conflict marriages (Peterson & Zill, 1986). The BPI includes subscales of internalizing (10 items, e.g., “worries too much”) and externalizing (20 items, e.g., “is impulsive, or acts without thinking”) behaviors. Mothers rated the extent to which their children exhibited each behavior on a three-point scale from 1 (not at all true) to 3 (often true). Mothers completed the BPI for each of their children between the ages of 4 and 17 years. Cronbach’s alpha reliabilities for the internalizing and externalizing subscales were .85 and .91, respectively.
Results
Preliminary Analysis
Descriptive statistics
Prior to path analysis, Pearson correlations were computed with the disaggregated dataset for a preliminary exploration of relationships between the variables (Table 2). Consistent with our hypotheses, the number of hurricane-related stressors was significantly and positively correlated with Time 2 maternal psychological distress and schools attended, which in turn were significantly and positively correlated with child internalizing and externalizing symptoms (all p < .05). A paired-samples t-test found that mothers’ psychological distress increased from Time 1 to Time 2, t(183) = 2.04, p = .04.
Table 2.
Correlation Matrix for all Variables Included in the Study with the Disaggregated Dataset (N = 251)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Time 1 maternal psychological distress | -- | |||||||
| 2. Hurricane-related stressors | .12a | -- | ||||||
| 3. Time 2 maternal psychological distress | .34*** | .23*** | -- | |||||
| 4. Number of schools attended | .04 | .19** | .11a | -- | ||||
| 5. Child age | −.02 | .04 | .05 | .08 | -- | |||
| 6. Child sex (female = 1) | −.02 | −.06 | −.05 | −.10 | < −.01 | -- | ||
| 7. Time 3 child internalizing symptoms | .07 | .13* | .26*** | .20** | −.15* | −.11a | -- | |
| 8. Time 3 child externalizing symptoms | .14* | .15* | .27*** | .27*** | .06 | −.25*** | .78*** | -- |
Note.
p < .05,
p < .01,
p < .001.
Missing data
All the variables in the study had less than 5% missing data. In subsequent analysis, missing data was handled using the full-information maximum likelihood (FIML) approach in Mplus 6.0.
Path Analytic Models
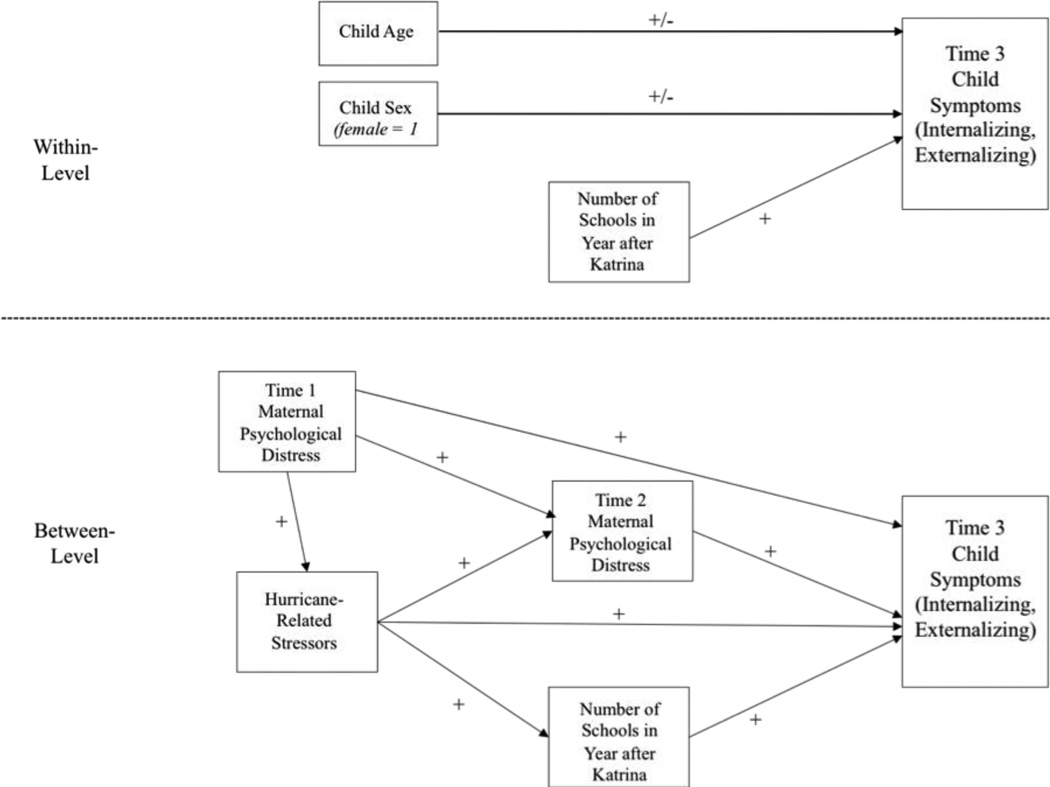
Because the children in the study were nested in families, with an average of 1.36 children per family (SD = 0.67), we conducted a multilevel path analytic model in MPlus 6.0. Time 1 and Time 2 maternal psychological distress and hurricane-related stressors were entered at the family level only, whereas child age, sex, and number of schools attended were allowed to vary both within and between families. The hypothesized multi-level models are illustrated in Figure 1. Within families, it was expected that more schools attended would predict greater Time 3 child internalizing and externalizing symptoms, whereas no a priori hypotheses were made about the relationships between child age, sex, and symptoms. Between families, it was hypothesized that more hurricane-related stressors would predict greater Time 2 maternal psychological distress and number of schools, which in turn would predict greater Time 3 child internalizing and externalizing symptoms. Additionally, higher Time 1 maternal psychological distress was hypothesized to predict a greater number of hurricane-related stressors and higher Time 2 maternal psychological distress, and more hurricane-related stressors were hypothesized to predict more Time 3 child internalizing and externalizing symptoms. Number of schools was included at both levels because of its high intraclass correlation (ICC = .94), indicating that, although there was some variation in number of schools attended within families, the majority of variation was between families. Therefore, we were able to investigate the impact of number of schools on child symptoms between families, while still accounting its impact at the withinfamily level. Following the recommendations of Hu and Bentler (1998), we set the cutoff of acceptable model fit at < .08 for RMSEA and > .95 for CFI.
Figure 1.
Hypothesized Path Analytic Model
Note. A plus sign indicates a hypothesized positive relationship; a negative sign indicates a hypothesized negative relationships; a plus/minus sign indicates no priori prediction for direction.
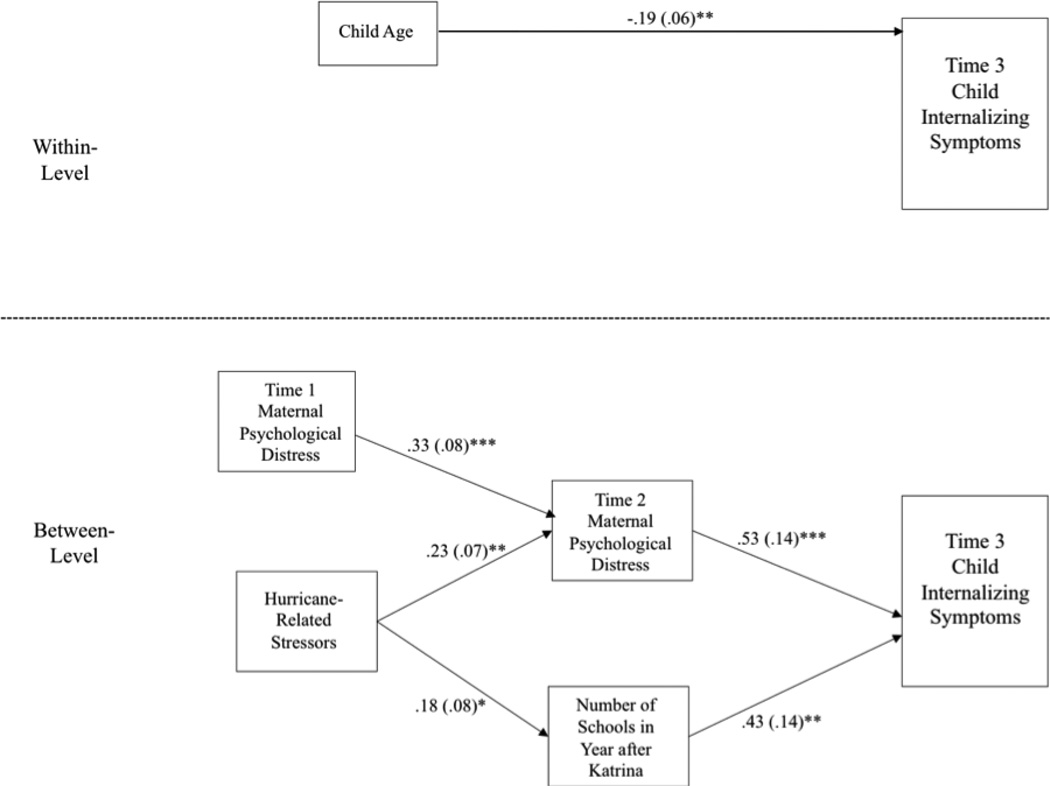
The hypothesized two-level path analytic model for internalizing symptoms had good fit, χ2 (16) = 15.20, p > .05, RMSEA < .001, CFI > .99. Two non-significant paths were trimmed at the within-family level, (the paths from sex and number of schools to Time 3 child internalizing symptoms), and three non-significant paths were trimmed at the between-family level, (the paths from hurricane-related stressors and Time 1 maternal psychological distress to Time 3 child internalizing symptoms and the path from Time 1 maternal psychological distress to hurricane-related stressors). The resulting trimmed model also had good fit, χ2(11) = 11.48, p > .05, RMSEA = .01, CFI = .99. A comparison of the hypothesized and trimmed models using the Satorra-Bentler scaled chi-square difference test for multilevel models (Santorra & Bentler, 2001) revealed no significant difference in model fit, (χ2(5) = 2.17, p > .01). Therefore, the more parsimonious, or trimmed model, was used for interpretation and is illustrated in Figure 2. As shown, greater hurricane-related stressors were significantly predictive of greater number of schools in the year after Hurricane Katrina, as well as greater Time 2 maternal psychological distress. More schools attended and higher Time 2 maternal psychological distress were significantly predictive of greater Time 3 child internalizing symptoms.
Figure 2.
Results of Trimmed Path Analytic Model Predicting Time 3 Internalizing Symptoms
Note. Numbers represent standardized path coefficients. Standard errors are in parentheses. * p < .05, ** p < .01, *** p < .001.
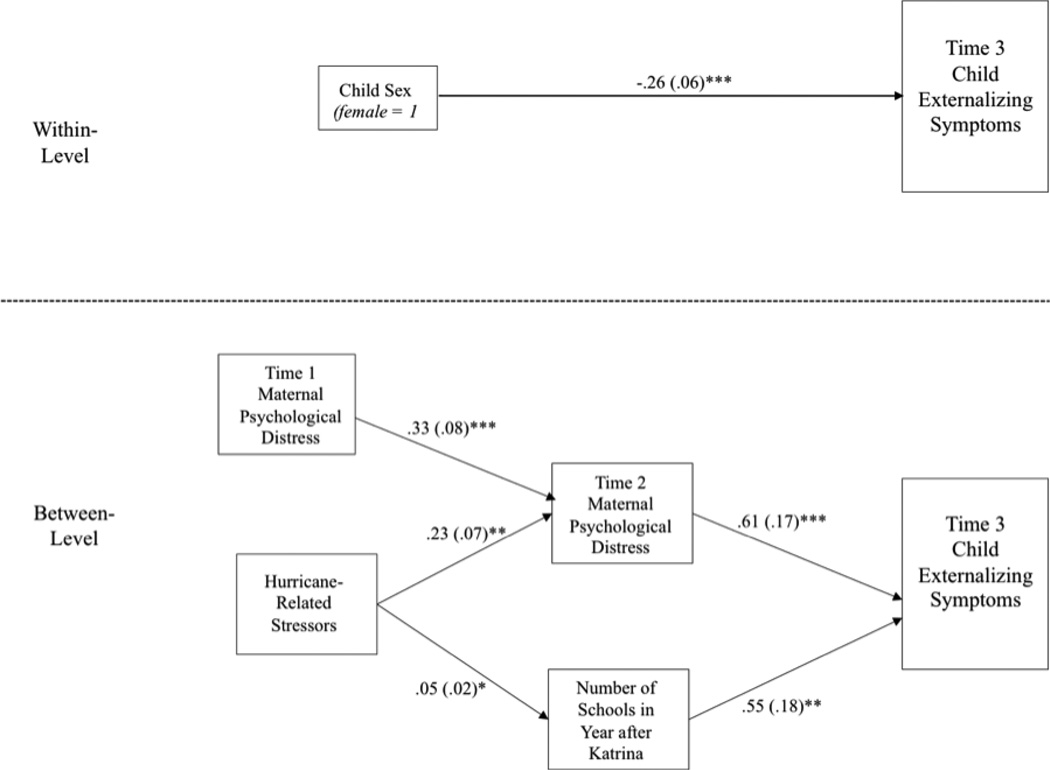
The same analytic procedure was repeated for child externalizing symptoms. Again, the hypothesized model had good fit with the data, χ2(16) = 16.23, p > .05, RMSEA = .01, CFI > .99. Two non-significant paths were trimmed from the within-family level (the paths from age and number of schools to Time 3 child externalizing symptoms), as were three non-significant paths at the between-family level (the paths from hurricane-related stressors and Time 1 maternal distress to Time 3 child externalizing symptoms, and the path from Time 1 maternal distress to hurricane-related stressors). The trimmed model had good fit with the data, χ2(11) = 9.04, p > .05, RMSEA < .001, CFI > .99 (Figure 3). Comparison of the two models using Satorra-Bentler scaled chi-square difference test found that the trimmed model significantly improved fit, χ2(5) = 11.43, p < .05. As with child internalizing symptoms, the paths from hurricane-related stressors to number of schools attended and Time 2 maternal psychological distress were positive and significant. The paths from number of schools and Time 2 maternal psychological distress to Time 3 child externalizing symptoms were also positive and significant.
Figure 3.
Results of Trimmed Path Analytic Model Predicting Time 3 Externalizing Symptoms
Note. Numbers represent standardized path coefficients. Standard errors are in parentheses. * p < .05, ** p < .01, *** p < .001
Mediation Analysis
To further test the indirect effects of hurricane-related stressors on child internalizing and externalizing symptoms, we used a mediation procedure for multilevel models outlined by Preacher, Zyphur, and Zhang (2010). Indirect effects through schools attended and Time 2 maternal psychological distress were specified and added to the trimmed models. Each indirect effect was computed as the product of the paths from hurricane-related stressors (the independent variable) to the mediator (number of schools attended or Time 2 maternal psychological distress) and from the mediator to Time 3 child internalizing or externalizing symptoms (the dependent variable).
Results from the mediation analysis are listed in Table 3. For both child internalizing and externalizing symptoms, the indirect effect from hurricane-related stress through Time 2 maternal psychological distress was significant, whereas the indirect effect through number of schools attended was not.
Table 3.
Results of Mediation Analysis Predicting Time 3 Internalizing and Externalizing Symptoms
| 95% Confidence Interval | ||||||
|---|---|---|---|---|---|---|
| Estimate | S.E. | Z | p | Lower | Upper | |
| Time 3 Child Internalizing Symptoms | ||||||
| Time 2 maternal psychological distress | .07* | .03 | 2.49 | .01 | .02 | .11 |
| Number of schools attended | .04 | .03 | 1.59 | .11 | < −.01 | .09 |
| Time 3 Child Externalizing Symptoms | ||||||
| Time 2 maternal psychological distress | .15* | .06 | 2.69 | .01 | .06 | .24 |
| Number of schools attended | .11a | .06 | 1.71 | .09 | <.01 | .21 |
Note.
p< .10,
p< .05.
Discussion
The purpose of this study was to explore the impact of Hurricane Katrina on the psychological functioning of elementary school aged children (5–10 years old) of low-income mothers who were exposed to the storm, 53.8% of whom were also exposed to Hurricane Rita. Mothers, who were initially part of a community college intervention study, provided data on their own psychological functioning both prior to and a year after the hurricanes, their exposure to hurricane-related stressors, and their children’s internalizing and externalizing symptoms three years after the storm. Through path analysis, we found support for a model wherein a greater number of hurricane-related stressors was associated with significantly higher maternal psychological distress, as well as a significantly greater number of schools children attended in the year following Hurricane Katrina. Higher maternal psychological distress and number of schools attended, in turn, were associated with significantly higher mother-reported child internalizing and externalizing symptoms three years after the storm.
To test for mediation, we added indirect effects to the path analytic model and found that hurricane-related stressors had a significant indirect effect on mother-reported child internalizing and externalizing symptoms through post-disaster maternal psychological distress, whereas indirect effects through number of schools were non-significant. Maternal psychological distress at approximately one year post-disaster was a mediator of the relationship between hurricane-related stressors and mother-reported child symptoms, controlling for pre-disaster maternal distress. It is likely that mothers’ increased psychological distress put a strain on their ability to effectively support their children through the challenges following the hurricane(s), disrupting mother-child relationships. Alternatively, children might have been attuned and reactive to their mothers’ increased distress. These interpretations, which could be further explored in future studies, are consistent with the results of previous research, which have documented the effects of natural disasters on family processes (e.g., Abramson et al., 2010).
Inclusion of pre-disaster data on maternal distress provided insight into how changes in maternal distress from pre- to post-disaster relate to mother-reported child functioning. We found that maternal distress significantly increased from pre- to post-disaster. The results further suggest that exposure to a greater number of hurricane-related stressors was associated with increases in pre- to post-disaster distress, and that such increases were associated with greater mother-reported child symptoms three years after Hurricane Katrina. Additional waves of data would have enabled us to use hierarchical linear modeling and other statistical techniques to demonstrate with greater precision how changes in maternal distress in the aftermath of disasters relate to child functioning (Green, et al., 2012).
Because the data in our study spanned one year pre-disaster to three years post-disaster, we are able to make stronger claims about causal pathways from maternal distress to child functioning than fully cross-sectional studies, which comprise the majority of disaster studies (Norris et al., 2002). Moreover, because we controlled for pre-disaster maternal psychological distress, we could account for mothers’ pre-existing psychological vulnerabilities, which might have contributed to children’s symptoms. Previous research has shown that parents’ symptoms can affect assessments of their children’s functioning.(e.g., Briggs-Gowan, Carter, & Schwab-Stone, 1996). Because we were able to control for pre-disaster mental health, we could provide insight into changes in maternal mental health in the aftermath of the storm and the impact of changes in maternal functioning on children’s internalizing and externalizing behaviors. Additionally, because maternal psychological distress was measured one year post-disaster, whereas child symptoms were assessed three years post-disaster, the potential impact of concurrent maternal symptoms on assessments of children’s mental health was reduced and the long-term consequences of maternal distress was highlighted.
Degree of exposure to hurricane-related stressors had a direct effect on the number of schools attended, which, in turn, was associated with mother-reported child symptoms. The indirect effect of hurricane-related stressors on mother-reported symptoms was not significant, however, suggesting that number of schools did not mediate the relationship between hurricane-related stressors and child symptoms. This phenomenon, in which direct effects are established but indirect (meditational) effects are not, has been referred to as direct-only non-mediation (Zhao, Lynch, & Chen, 2010). The findings could indicate that variance in child symptoms explained by number of schools attended was independent from that explained by hurricanerelated stressors. For example, frequent school transitions are associated with psychosocial stressors that are quite distinct from exposure to concrete stressors during a natural disaster and might therefore have differential effects on child development. Disrupted friendships and teacher relationships, adjustment to new academic settings and standards, and the potential for peer rejection and neglect can heighten the risk of symptoms of psychological distress (Gruman, et al., 2008; Prinstein et al., 1996), particularly given the protective role of social support in the aftermath of disasters (Kaniasty & Norris, 2009; Pina et al., 2008). Moreover, school changes could represent residential instability in the aftermath of the hurricane, which corresponds to other risk factors and stressors, such as financial strain and the disruption of social support networks (Gasper, DeLuca, & Estacion, 2010; Scanlon & Devine, 2001). Given the lack of research on children’s school experiences in the aftermath of disasters, future research focusing on this topic would be a major contribution to the disaster literature.
Implications
The results of this study have implications for research, policy, and practice. With regard to research, as mentioned above, future investigators should delve further into the pathways through which disaster-related stressors impact children’s functioning, including through parenting and attachment styles, and peer and teacher relationships. In doing so, researchers could also explore potential moderators of the effect, for example gender and age, which have been found to influence children’s post-disaster psychological responses (e.g., Shannon, Lonigan, Finch, & Taylor, 1994; Weems et al., 2007). Alternative means of data collection, including observations of parent-child relationships and child- and teacher-reported assessments of children’s mental health, would further add to our understanding of children’s post-disaster functioning. Qualitative analysis of mothers’ and children’s experiences would likewise shed light on how mothers understand family processes, residential changes, and children’s academic experiences, and their effects on child development in the aftermath of disasters. Additionally, longitudinal data on children’s post-disaster psychological responses would permit further exploration of reciprocal relationships between post-disaster maternal and child psychological functioning over time.
With regard to practice and policy, the results suggest the importance of practices that bolster schools and families’ readiness for disasters. This might include additional means for reaching out to parents and tracking students in the aftermath of disasters, both to ensure that students are connected with new schools and to foster communication amongst students, parents, teachers, counselors, and other school personnel during transitions. Students who maintain some connection to their former school might feel supported even as they enter a new school and community. To improve tracking efforts, schools could require families to update their contact information more frequently and provide more emergency contacts, including those who are out of state. Policymakers could encourage the use of a national student database to ensure that students are located and tracked post-disaster. Even prior to disasters, schools could include a disaster plan in their parent orientation and attempt to forge connections with schools in communities that might attract a large number of evacuees post-disaster. To the extent possible, post-disaster policies should prioritize and facilitate temporary locations for damaged schools, and planning for their reconstruction. Policies that promote the long-term stability of low-income families, who are particularly likely to face a large number co-occurring stressors, in the aftermath of disasters would also protect against frequent school transitions and psychological distress (Yoshikawa et al., 2012).
The results suggest that children who change schools frequently in the aftermath of disasters would be appropriate targets for mental health services. Routine screening of new students for mental health problems would help identify children in need, and identified children could receive counseling services during the school day. Schools represent an ideal setting for screening and the provision of psychological services for children in the aftermath of disasters, given that they are a common point of entry and provider of services for children with mental health needs (Farmer et al., 2003), and that they can serve as “nurturing environments,” helping to foster prosocial behaviors and prevent mental health problems (Biglan et al., 2012).
Empirically supported interventions for children in the aftermath of disasters, such as cognitive behavioral and trauma-focused therapies, would protect against elevated symptoms (Jaycox et al., 2010; La Greca & Silverman, 2009; Salloum & Overstreet, 2008). Interventions could help children build skills to cope with emergent symptoms. For example, a study by Weems and colleagues (2009) found that a group behavioral intervention for test anxiety, consisting of relaxation and graded exposure, not only reduced test anxiety and improved academic performance of ninth graders in New Orleans, but also was associated with decreased posttraumatic stress. Interventions that boost children’s regulatory skills (e.g., attention and inhibitory control) and reduce the use of negative coping strategies could also protect against post-disaster psychological symptoms (Terranova, Boxer, & Morris, 2009a).
Further research has indicated bidirectional relationships between psychological symptoms and peer relational problems, including bullying behaviors and peer victimization experiences (Terranova et al., 2009a; Terranova, Boxer, & Morris, 2009b). Therefore, interventions aiming to reduce children’s post-disaster psychological symptoms could improve peer relationships. Psychosocial interventions that help new students build relationships with classmates and teachers and fill academic gaps would also facilitate children’s adjustment to new schools and protect against psychological symptoms (Gruman, et al., 2008; Jason et al., 1993). School-based interventions could be either facilitated by mental health professionals, or developed in tandem with teachers and integrated into the standard curriculum (Margolin, Ramos, & Guran, 2010).
Given the strong associations between maternal distress and mother-reported child outcomes, in screening and treating children, school counselors should be encouraged to include parents in interventions and/or facilitate referrals to community providers. More generally, the results suggest that mental health services for low-income mothers in the aftermath of disasters could offset the impact of these disasters on the psychological functioning of children. In addition to reaching low-income mothers through children’s schools, practitioners could connect with mothers through religious communities, housing developments, social service agencies, and community health centers to provide support and advocacy. Empirically-supported, culturally competent, and developmentally appropriate mental health services would help to reduce maternal psychological distress, enabling mothers to more effectively care for their children in the post-disaster period (Costa, Weems, & Pina, 2009; Hobfoll et al., 2007). Clinicians should take into account structural barriers that often prevent low-income mothers from receiving services, including lack of insurance, childcare, and transportation (Miranda & Green, 1999). Attitudinal barriers (e.g., concerns about being medicated and the fit of psychotherapy with religious beliefs and practices) also can reduce low-income women’s willingness to access mental health services, calling for the need for outreach and psychoeducation groups (Miranda & Green, 1999).
Limitations
Despite its potential to inform research, policy, and practice, this study has several limitations. Although we benefitted from data on maternal psychological distress collected prior to the storm, we did not have access to pre-disaster data on children’s functioning. We were therefore unable to account for children’s pre-disaster mental health, which has been found to influence post-disaster responses (e.g., Weems et al., 2007). Child functioning was not assessed in the first post-disaster assessment, rendering it impossible to document children’s symptomatology in the more immediate aftermath of the storm and its relation to hurricane-related stressors, maternal psychological distress, and school disruptions, and there was a two year time span between the two post-disaster assessments. We were also unable to explore reciprocal relationships between child and maternal psychological functioning, and it was likely that mothers were influenced by the specific nature of their children’s distress. As noted earlier, we did not have data from children directly and, although not collected concurrently, mothers’ psychological symptoms could have affected their reports of child functioning (Briggs-Gowan, et al., 1996). Future studies would benefit from the use of independent observers to rate children’s behavior and distress as well as the quality of parent-child relationships in the aftermath of disasters. Information about other family members, including fathers, siblings, and grandparents, and their relationships with children would also be useful in understanding children’s post-disaster functioning.
Additionally, our maternal mental health measure was of non-specific psychological distress, and we were therefore unable to explore the influence of specific disorders that are elevated in the aftermath of disaster (e.g., posttraumatic stress disorder, major depression) on children. Mothers also provided data on hurricane-related stressors, and it is possible that children might not have faced the same stressors (e.g., if mothers and children were separated) or perceived them in the same way. Likewise, our hurricane-related stressors measure did not include other experiences that could potentially affect children, such as bereavement, property loss, and home damage (e.g., Goenjian et al., 2001; Russoniello et al., 2002). Our single-item measure of school mobility, number of schools in the aftermath of disaster, did not allow for in-depth exploration of children’s post-disaster academic experiences and their impact on functioning. For example, we were unable to ascertain whether children returned to their pre-disaster schools at any point, which could shape their experiences. We also did not include other stressors that children might have endured in their post-disaster environments, including family conflicts and negative interactions with neighborhood peers. Because participants were initially part of a community college intervention study, the results might not generalize to all low-income families that endured Hurricane Katrina.
Despite these limitations, the results of this study shed new light on the processes by which exposure to stressors such as Hurricane Katrina has longer-term effects on child functioning. Although maternal stress certainly had some direct effects on children, it is important that the effects on maternal functioning over a longer period of time also appeared to undermine family processes that nurture child psychological development. Disruptions in schooling rendered by the hurricane could also have long-term effects, even as children settle into new schools and communities. Further research on the processes by which exposure to hurricanes and other disasters affects children’s functioning can assist in the development of policies and interventions to offset long-term psychological effects.
Highlights.
-
-
Mothers were surveyed one year prior to Hurricane Katrina, and one and three years after.
-
-
A model linking hurricane-related stressors to child behavior problems was tested.
-
-
Hurricane-related stressors predicted increases in maternal psychological distress.
-
-
Stressors were associated with increased school mobility post-disaster.
-
-
School mobility and increased maternal distress predicted child behavior problems.
Acknowledgments
The study was funded by NIH grant R01HD046162, and the National Science Foundation, the MacArthur Foundation, and the Center for Economic Policy Studies at Princeton University. We thank Thomas Brock, MDRC, Christina Paxson, Elizabeth Fussell, and Mary Waters.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramson DM, Park YS, Stehling-Ariza T, Redlener I. Children as bellwethers of recovery: Dysfunctional systems and the effects of parents, households, and neighborhoods on serious emotional disturbance in children after Hurricane Katrina. Disaster Medicine and Public Health Preparedness. 2010;4(S1):S17–S27. doi: 10.1001/dmp.2010.7. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. Behavior problems and competences reported by parents of normal and disturbed children aged four through sixteen. Monographs of the Society for Research in Child Development. 1981;46:1–82. [PubMed] [Google Scholar]
- Biglan A, Flay BR, Embry DD, Sandler IN. The critical role of nurturing environments for promoting human well-being. American Psychologist. 2012;67(4):257–271. doi: 10.1037/a0026796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting & Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Schwab-Stone M. Discrepancies among mother, child, and teacher reports: examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology. 1996;24:749–765. doi: 10.1007/BF01664738. [DOI] [PubMed] [Google Scholar]
- Brodie M, Weltzien E, Altman D, Blendon RJ, Benson JM. Experiences of Hurricane Katrina evacuees in Houston Shelters: Implications for future planning. American Journal of Public Health. 2006;96:1402–1408. doi: 10.2105/AJPH.2005.084475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Chase-Lansdale PL, Mott FL, Brooks-Gunn J, Phillips DA. Children of the National Longitudinal Survey of Youth: A unique research opportunity. Developmental Psychology. 1991;27:918–931. [Google Scholar]
- Costa NM, Weems CF, Pina AA. Hurricane Katrina and youth anxiety: The role of perceived attachment beliefs and parenting behaviors. Journal of Anxiety Disorders. 2009;23:935–941. doi: 10.1016/j.janxdis.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54:60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behavior and Development. 2010;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian. Psychological Medicine. 2003;33:357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, Kessler RC. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry. 2007;64:1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Tracy M, Norris F, Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress. 2008;21:357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Gasper J, DeLuca S, Estacion A. Coming and going: Explaining the effects of residential and school mobility on adolescent delinquency. Social Science Research. 2010;39:459–476. [Google Scholar]
- Gault B, Hartmann H, Jones-DeWeever A, Weschkul M, Williams E. The women of New Orleans and the Gulf Coast: Multiple disadvantages and key assets for recovery. Part I. Poverty, race, gender and class. Washington, DC: Institute for Women’s Policy Research; 2005. Briefing Paper #D464. [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka L. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychological Medicine. 2003;33:1341–1355. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, Alvarez ML, Goenjian HA, Pynoos RS. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after Hurricane Mitch. American Journal of Psychiatry. 2001;158:788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- Green G, Lowe SR, Rhodes JE. Understanding the impact of natural disasters: A three-wave study of low-income mothers who survived Hurricane Katrina. Journal of Traumatic Stress. 2012;25:1–8. [Google Scholar]
- Groen JA, Polivka A. Going home after Hurricane Katrina: Determinants of return migration and changes in affected areas. Washington, DC: U.S. Bureau of Labor Statistics; 2009. Working Paper 428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruman DH, Hartman TW, Abbott RD, Catalano RF, Fleming CB. Longitudinal effects of student mobility on three dimensions of elementary school engagement. Child Development. 2008;79:1833–1852. doi: 10.1111/j.1467-8624.2008.01229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll SE, Watson P, Bell CC, Bryan RA, Brymer MJ, Friedman MJ, Ursano RJ. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry. 2007;70:283–315. doi: 10.1521/psyc.2007.70.4.283. [DOI] [PubMed] [Google Scholar]
- Hoglund WL, Leadbeater BJ. The effects of family, school, and classroom ecologies on changes in children's social competence and emotional and behavioral problems in first grade. Developmental Psychology. 2004;40(4):533–544. doi: 10.1037/0012-1649.40.4.533. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Intergovernmental Panel on Climate Change [IPCC] Summary for policymakers. In: Solomon S, Qin D, Manning M, Chen Z, Marquis M, Averyt KB, Tignor M, Miller HL, editors. Climate change 2007: The physical science basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2007. Retrieved from http://www.ipcc-wg2.org/ [Google Scholar]
- Jason LA, Weine AM, Johnson JH, Danner KE, Kuraski KS, Warren-Sohlberg L. The School Transitions Project: A comprehensive preventive intervention. Journal of Emotional and Behavioral Disorders. 1993;1:65–70. [Google Scholar]
- Jaycox LH, Cohen JA, Mannarino AP, Walker DW, Langley AL, Gegenheimer KL, Schonlau M. Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused therapies. Journal of Traumatic Stress. 2010;23:223–231. doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones-DeWeever A. Women in the wake of the storm: Examining the post-Katrina realities of the women of New Orleans and the Gulf Coast. Washington, DC: Institute for Women’s Policy Research; 2008. [Google Scholar]
- Jones-DeWeever AA, Hartman H. Abandoned before the storms: The glaring disaster of gender, race, and class disparities in the gulf. In: Hartman C, Squires GD, editors. There is No Such Thing as a Natural Disaster: Race, Class, & Hurricane Katrina. New York, NY: Routledge; 2006. pp. 85–101. [Google Scholar]
- Kaiser Family Foundation. New Orleans five years after the storm. Menlo Park, CA: Author; 2010. [Google Scholar]
- Kaniasty K, Norris FH. Distinctions that matter: Received social support, perceived social support, and social embeddedness afterdisasters. In: Neria Y, Galea S, Norris F, editors. Mental health consequences of disasters. New York, NY: Cambridge University Press; 2009. pp. 175–201. [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, Zaslavsky AM. Short screening scales to monitor population prevalances and trends in nonspecific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Groerer JC, Hiripi E, Zaslavsky AM. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Molecular Psychiatry. 2008;13:374–384. doi: 10.1038/sj.mp.4002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK. Treatment and prevention of posttraumatic stress reactions in children and adolescents exposed to disasters and terrorism: What is the evidence? Child Development Perspectives. 2009;3:4–10. [Google Scholar]
- La Greca AM, Silverman WK, Lai B, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children's persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Child Psychology. 2010;78(6):794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Wasserstein SB. Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting and Clinical Child Psychology. 1998;66(6):883–892. doi: 10.1037//0022-006x.66.6.883. [DOI] [PubMed] [Google Scholar]
- Liu A, Fellowes M, Mabanta M. Special edition of the Katrina Index: A one-year review of key indicators of recovery in post-storm New Orleans. Washington, DC: The Brookings Institution Metropolitan Policy Program; 2006. [Google Scholar]
- Lonigan CJ, Shannon MP, Taylor CM, Finch AJ, Sallee FR. Risk factors for the development of post-traumatic symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:94–106. doi: 10.1097/00004583-199401000-00013. [DOI] [PubMed] [Google Scholar]
- Lowe SR, Chan CS, Rhodes JE. The impact of child-related stressors on the psychological functioning of lower-income mothers after Hurricane Katrina. Journal of Family Issues. 2011 doi: 10.1177/0192513X11412492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madrid PA, Grant R. Meeting mental health needs following a natural disaster: Lessons from Hurricane Katrina. Professional Psychology: Research and Practice. 2008;39:86–92. [Google Scholar]
- Madrid PA, Garfield R, Jaberi P, Daly M, Richard G, Grant R. Mental health services in Louisiana school-based health centers post-Hurricanes Katrina and Rita. Professional Psychology: Research and Practice. 2008;39:45–51. [Google Scholar]
- Magdol L. Is moving gendered?. The effects of residential mobility on the psychological well-being of men and women. Sex Roles. 2002;47:553–561. [Google Scholar]
- Magdol L, Bessel DR. Social capital, social currency, and portable assets: The impact of residential mobility on exchanges of social support. Personal Relationships. 2003;10:149–169. [Google Scholar]
- Mantzicopoulos P, Knutson DJ. Head Start children: School mobility and achievement in the early grades. Journal of Educational Research. 2000;93:305–311. [Google Scholar]
- Margolin G, Ramos MC, Guran EL. Earthquakes and children: The role of psychologists with families and communities. Professional Psychology: Research and Practice. 2010;41:1–9. doi: 10.1037/a0018103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott BM, Palmer LJ. Post-disaster emotional distress, depression and event-related variables: Findings across child and adolescent developmental stages. Australian and New Zealand Journal of Psychiatry. 2002;36:754–761. doi: 10.1046/j.1440-1614.2002.01090.x. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Fairbank JA, Gruber MJ, Jones RT, Osofsky JO, Pfefferbaum B, Sampson NA, Kessler RC. Trends in serious emotional disturbance among youths exposed to Hurricane Katrina. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:990–1000. doi: 10.1016/j.jaac.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Green BL. The need for mental health services research focusing on poor young women. Journal of Mental Health Policy and Economics. 1999;2:73–80. doi: 10.1002/(sici)1099-176x(199906)2:2<73::aid-mhp40>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Norris F, Friedman M, Watson P, Byrne C, Diaz E, Kaniasty K. 60,000 disaster victims speak. Part I: An empirical review of the empirical literature 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Osofsy JD, Osofsky HJ, Harris WW. Katrina’s children: Social policy considerations for children in disasters. Social Policy Report. 2007;21:3–18. Retrieved from http://www.srcd.org. [Google Scholar]
- Pane JF, McCaffrey DF, Tharp-Taylor S, Asmus GJ, Stokes BR. Technical Report TR430. Santa Monica CA: RAND Corporation; 2006. Student displacement in Louisiana after the Hurricanes of 2005: Experiences of public schools and their students. [Google Scholar]
- Peterson JL, Zill N. Marital disruption, parent-child relationships, and behavior problems in children. Journal of Marriage and the Family. 1986;48:295–307. [Google Scholar]
- Pina AA, Villalta IK, Ortiz CD, Gottschall AC, Costa NM, Weems CF. Social support, discrimination, and coping as predictors of posttraumatic stress reactions in youth survivors of Hurricane Katrina. Journal of Clinical and Adolescent Psychiatry. 2008;37:564–574. doi: 10.1080/15374410802148228. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A general SEM framework for assessing multilevel mediation. Psychological Methods. 2010;15:209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, LaGreca AM, Vernberg EM, Silverman WK. Children's coping assistance: How parents, teachers, and friends help children cope after a natural disaster. Journal of Clinical Child Psychology. 1996;25:463–475. [Google Scholar]
- Proctor LJ, Fauchier A, Oliver PH, Ramos MC, Rios MA, Margolin G. Family context and young children’s responses to earthquake. Journal of Child Psychology and Psychiatry. 2007;48:941–949. doi: 10.1111/j.1469-7610.2007.01771.x. [DOI] [PubMed] [Google Scholar]
- Rhodes JE, Chan CS, Paxson C, Rouse CE, Waters M, Fussell E. The impact of Hurricane Katrina on the mental and physical health of low-income parents in New Orleans. American Journal of Orthopsychiatry. 2010;80:237–247. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richburg-Hayes L, Brock T, LeBlanc A, Paxson C, Rouse CE, Barrow L. Rewarding persistence: Effects of a performance-based scholarship program for low-income parents. New York, NY: MDRC; 2009. [Google Scholar]
- Ruscher JB. Stranded by Katrina: Past and present. Analyses of Social Issues and Public Policy. 2006;6:33–38. [Google Scholar]
- Russoniello CV, Skalko TK, O'Brien K, McGee SA, Bingham-Alexander D, Beatley J. Child posttraumatic stress disorder and efforts to cope after Hurricane Floyd. Behavioral Medicine. 2002;28:61–71. doi: 10.1080/08964280209596399. [DOI] [PubMed] [Google Scholar]
- Salloum A, Overstreet S. Evaluation of individual and group grief trauma interventions for children post disaster. Journal of Clinical Child and Adolescent Psychiatry. 2008;37:495–507. doi: 10.1080/15374410802148194. [DOI] [PubMed] [Google Scholar]
- Santorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlon E, Devine K. Residential mobility and youth well-being: Research, policy, and practice issues. Journal of Sociology and Social Welfare. 2001;28:119–138. Retrieved from http://www.wmich.edu/hhs/newsletters_journals/jssw/index.htm. [Google Scholar]
- Scaramella LV, Sohr-Preston SL, Callahan KL, Mirabile SP. A test of the family stress model on toddler-aged children’s adjustment among Hurricane Katrina impacted and nonimpacted low-income families. Journal of Clinical Child and Adolescent Psychology. 2008;37:530–541. doi: 10.1080/15374410802148202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH. Reconsideration of harm's way: onsets and comorbidity patterns of disorders in preschool children and their caregivers following Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:508–518. doi: 10.1080/15374410802148178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon MP, Lonigan CJ, Finch AJ, Taylor CM. Epidemiology of post-traumatic symptoms and symptom profiles. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:80–94. doi: 10.1097/00004583-199401000-00012. [DOI] [PubMed] [Google Scholar]
- Spell AW, Kelley ML, Wang J, Self-Brown S, Davidson KL, Pellegrin A, Baumeister A. The moderating effects of maternal psychopathology on children’s adjustment post-Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:553–563. doi: 10.1080/15374410802148210. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidel LS. Using multivariate statistics. 5th ed. Boston, MA: Pearson Education; 2007. [Google Scholar]
- Terranova AM, Boxer P, Morris AS. Factors influencing the course of posttraumatic stress following a natural disaster: Children’s reactions to Hurricane Katrina. Journal of Applied Developmental Psychology. 2009a;30:344–355. [Google Scholar]
- Terranova AM, Boxer P, Morris AS. Changes in children’s peer interactions following a natural disaster: How predisaster bullying and victimization rates changed following Hurricane Katrina. Psychology in the Schools. 2009b;46:333–347. [Google Scholar]
- Van der Molen E, Hipwell AE, Vermeiren R, Loeber R. Maternal characteristics predicting young girls' disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2011;40(2):179–190. doi: 10.1080/15374416.2011.546042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernberg EM, La Greca AM, Silverman WK, Prinstein MJ. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew. Journal of Abnormal Psychology. 1996;105:237–248. doi: 10.1037//0021-843x.105.2.237. [DOI] [PubMed] [Google Scholar]
- Weems CF, Pina AA, Costa NM, Watts SE, Taylor LK, Cannon MF. Predisaster trait anxiety and negative affect predict posttraumatic stress in youths after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2007;75:154–159. doi: 10.1037/0022-006X.75.1.154. [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Cannon MF, Marino R, Romano DM, Scott BG, Perry AM, Triplett V. Posttraumatic stress, context, and the lingering effects of the Hurricane Katrina disaster among ethnic minority youth. Journal of Abnormal Child Psychology. 2010;38:49–56. doi: 10.1007/s10802-009-9352-y. [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Costa NM, Marks AB, Romano DM, Verrett SL, Brown DM. Effect of a school-based test anxiety intervention in ethnic minority youth exposed to Hurricane Katrina. Journal of Applied Developmental Psychology. 2009;30:218–226. [Google Scholar]
- Weinberg MK, Olson KL, Beeghly M, Tronick EZ. Making up is hard to do, especially for mothers with high levels of depressive symptoms and their infant sons. Journal of Child Psychology and Psychiatry. 2006;47(7):670–683. doi: 10.1111/j.1469-7610.2005.01545.x. [DOI] [PubMed] [Google Scholar]
- Weems CF, Overstreet S. Child and adolescent mental health research in the context of Hurricane Katrina: an ecological needs-based perspective and introduction to the special section. Journal of Clinical Child and Adolescent Psychology. 2008;37(3):487–494. doi: 10.1080/15374410802148251. [DOI] [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hurlburt M, Hough R, Hazen A, Culver S, Landsverk J. Referral sources, diagnoses, and service types of youth in public outpatient mental health care: a focus on ethnic minorities. Journal of Behavioral Health Services Research. 2002;29(1):45–60. doi: 10.1007/BF02287831. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, Aber JL, Beardslee WR. The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. American Psychologist. 2012;67(4):272–284. doi: 10.1037/a0028015. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Jr, Chen Q. Reconsidering Barron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37:197–206. [Google Scholar]
- Zill N. Behavior problem index based on parent report. Washington, DC: Child Trends; 1990. [Google Scholar]