Abstract
Summary
Guidance is provided in a European setting on the assessment and treatment of postmenopausal women at risk of fractures due to osteoporosis.
Introduction
The International Osteoporosis Foundation and European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis published guidance for the diagnosis and management of osteoporosis in 2008. This manuscript updates these in a European setting.
Methods
Systematic literature reviews.
Results
The following areas are reviewed: the role of bone mineral density measurement for the diagnosis of osteoporosis and assessment of fracture risk, general and pharmacological management of osteoporosis, monitoring of treatment, assessment of fracture risk, case finding strategies, investigation of patients and health economics of treatment.
Conclusions
A platform is provided on which specific guidelines can be developed for national use.
Keywords: Bone mineral density, Diagnosis of osteoporosis, Fracture risk assessment, FRAX, Health economics, Treatment of osteoporosis
Introduction
In 1997, the European Foundation for Osteoporosis and Bone Disease (subsequently the International Osteoporosis Foundation, IOF) published guidelines for the diagnosis and management of osteoporosis [1], subsequently updated in 2008 by the IOF and European Society for Clinical and Economic Evaluation of Osteoporosis and Osteoarthritis (ESCEO) [2]. Since then, there have been significant advances in the field of osteoporosis. These include the development of new techniques for measuring bone mineral, improved methods of assessing fracture risk and new treatments that have been shown to significantly reduce the risk of fractures at vulnerable sites. Against this background, the Scientific Advisory Board of the ESCEO, in collaboration with the IOF, has recognised a need to update the guidance which is detailed below. The high societal and personal costs of osteoporosis pose challenges to public health and physicians, particularly since most patients with osteoporosis remain untreated. Indeed, less than 20 % of patients with a fragility fracture receive therapy to reduce future fracture within the year following fracture [3–5]. The aim of this guidance is to stimulate a cohesive approach to the management of osteoporosis in Europe. The term guidance rather than guidelines is used, to avoid any prescriptive connotations since country- or region-specific guidelines are now widely available in many European countries and continue to evolve. Rather, the guidance can inform the development of new guidelines or the revision of existing guidelines. Whilst focussed on a European perspective and on postmenopausal women, the principles may be of some assistance in other regions of the world and in men.
Osteoporosis in Europe
Osteoporosis is defined as a systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [6]. Although the diagnosis of the disease relies on the quantitative assessment of bone mineral density, which is a major determinant of bone strength, the clinical significance of osteoporosis lies in the fractures that arise. In this respect, there are some analogies with other multifactorial chronic diseases. For example, hypertension is diagnosed on the basis of blood pressure whereas an important clinical consequence of hypertension is stroke. Because a variety of non-skeletal factors contribute to fracture risk [7–9], the diagnosis of osteoporosis by the use of bone mineral density (BMD) measurements is at the same time an assessment of a risk factor for the clinical outcome of fracture. For these reasons, there is a distinction to be made between the use of BMD for diagnosis and for risk assessment.
Common sites for osteoporotic fracture are the spine, hip, distal forearm and proximal humerus. The remaining lifetime probability in women, at menopause, of a fracture at any one of these sites exceeds that of breast cancer (approximately 12 %), and the likelihood of a fracture at any of these sites is 40 % or more in Western Europe [10] (Table 1), a figure close to the probability of coronary heart disease.
Table 1.
Remaining lifetime probability of a major fracture at the age of 50 and 80 years in men and women from Sweden [10] (with kind permission from Springer Science and Business Media)
| Site | At 50 years | At 80 years | ||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Forearm | 4.6 | 20.8 | 1.6 | 8.9 |
| Hip | 10.7 | 22.9 | 9.1 | 19.3 |
| Spine | 8.3 | 15.1 | 4.7 | 8.7 |
| Humerus | 4.1 | 12.9 | 2.5 | 7.7 |
| Any of these | 22.4 | 46.4 | 15.3 | 31.7 |
In the year 2000, there were estimated to be 620,000 new fractures at the hip, 574,000 at the forearm, 250,000 at the proximal humerus and 620,000 clinical spine fractures in men and women aged 50 years or more in Europe. These fractures accounted for 34.8 % of such fractures worldwide [11]. Osteoporotic fractures also occur at many other sites including the pelvis, ribs and distal femur and tibia. Collectively, all osteoporotic fractures account for 2.7 million fractures in men and women in Europe at a direct cost (2006) of €36 billion [12]. A more recent estimate (for 2010) calculated the direct costs at €29 billion in the five largest EU countries (France, Germany, Italy, Spain and UK) [13] and €38.7 billion in the 27 EU countries [14].
Osteoporotic fractures are a major cause of morbidity in the population. Hip fractures cause acute pain and loss of function, and nearly always lead to hospitalisation. Recovery is slow, and rehabilitation is often incomplete, with many patients permanently institutionalised in nursing homes. Vertebral fractures may cause acute pain and loss of function but may also occur without serious symptoms. Vertebral fractures often recur, however, and the consequent disability increases with the number of fractures. Distal radial fractures also lead to acute pain and loss of function, but functional recovery is usually good or excellent.
It is widely recognised that osteoporosis and the consequent fractures are associated with increased mortality, with the exception of forearm fractures [15]. In the case of hip fracture, most deaths occur in the first 3–6 months following the event, of which 20–30 % are causally related to the fracture event itself [16]. In Sweden, the number of deaths that are causally related to hip fracture account for more than 1 % of all deaths, somewhat higher than the deaths attributed to pancreatic cancer and somewhat lower than the deaths attributed to breast cancer [16]. In 2010, the number of deaths causally related to osteoporotic fractures was estimated at 43,000 in the European Union [14]. Approximately 50 % of fracture-related deaths in women were due to hip fractures, 28 % to clinical vertebral and 22 % to other fractures. In Europe, osteoporosis accounted for more disability and life years lost than rheumatoid arthritis, but less than osteoarthritis. With regard to neoplastic diseases, the burden of osteoporosis was greater than for all sites of cancer, with the exception of lung cancers [11].
Bone mineral measurements
The objectives of bone mineral measurements are to provide diagnostic criteria, prognostic information on the probability of future fractures and a baseline on which to monitor the natural history of the treated or untreated patient. BMD is the amount of bone mass per unit volume (volumetric density), or per unit area (areal density), and both can be measured in vivo by densitometric techniques.
A wide variety of techniques is available to assess bone mineral that are reviewed elsewhere [17–19]. The most widely used are based on X-ray absorptiometry of bone, particularly dual energy X-ray absorptiometry (DXA), since the absorption of X-rays is very sensitive to the calcium content of the tissue of which bone is the most important source. Other techniques include quantitative ultrasound (QUS), quantitative computed tomography (QCT) applied both to the appendicular skeleton and to the spine, peripheral DXA, digital X-ray radiogrammetry, radiographic absorptiometry, and other radiographic techniques. Other important determinants of bone strength for both cortical and trabecular bone include macro-and microarchitecture (e.g. cross-sectional moment of inertia, hip axis length, cortical thickness, trabecular bone score, Hurst parameters). X-ray-based technology is becoming available to estimate these components of bone strength which may have a future role in fracture risk assessment [20–23].
DXA is the most widely used bone densitometric technique. It is versatile in the sense that it can be used to assess bone mineral density/bone mineral content of the whole skeleton as well as specific sites, including those most vulnerable to fracture [17, 24, 25]. Areal density (in grams per square centimetre) rather than a true volumetric density (in grams per cubic centimetre) is measured since the scan is two dimensional. Areal BMD accounts for about two thirds of the variance of bone strength as determined in vitro on isolated bones, such as the vertebral body or proximal femur.
DXA can also be used to visualise lateral images of the spine from T4 to L4 to detect deformities of the vertebral bodies [26–30]. Vertebral fracture assessment (VFA) may improve fracture risk evaluation, since many patients with vertebral fracture may not have a BMD T-score classified as osteoporosis. This procedure involves less radiation and is less expensive than a conventional X-ray examination. Whereas whole body bone, fat and lean mass can also be measured using DXA, these measurements are useful for research; they do not assist in the routine diagnosis or assessment of osteoporosis.
The performance characteristics of many measurement techniques have been well documented [31, 32]. For the purpose of risk assessment and for diagnosis, a characteristic of major importance is the ability of a technique to predict fractures. This is traditionally expressed as the increase in the relative risk of fracture per standard deviation unit decrease in bone mineral measurement—termed the gradient of risk.
Limitations of BMD
There are a number of technical limitations in the general application of DXA for diagnosis which should be recognised [1, 33]. The presence of osteomalacia, a complication of poor nutrition in the elderly, will underestimate total bone matrix because of decreased mineralization of bone. Osteoarthrosis or osteoarthritis at the spine or hip are common in the elderly and contribute to the density measurement, but not necessarily to skeletal strength. Heterogeneity of density due to osteoarthrosis, previous fracture or scoliosis can often be detected on the scan and in some cases excluded from the analysis. Some of these problems can be overcome with adequately trained staff and rigorous quality control.
Diagnosis of osteoporosis
Bone mineral density is most often described as a T- or Z-score, both of which are units of standard deviation (SD). The T-score describes the number of SDs by which the BMD in an individual differs from the mean value expected in young healthy individuals. The operational definition of osteoporosis is based on the T-score for BMD [7, 34] assessed at the femoral neck and is defined as a value for BMD 2.5 SD or more below the young female adult mean (T-score less than or equal to −2.5 SD) [8, 35]. The Z-score describes the number of SDs by which the BMD in an individual differs from the mean value expected for age and sex. It is mostly used in children and adolescents.
The reference range recommended by the IOF, ISCD, WHO and NOF for calculating the T-score [8, 36] is the National Health and Nutrition Examination Survey (NHANES) III reference database for femoral neck measurements in Caucasian women aged 20–29 years [37]. Note that the diagnostic criteria for men use the same female reference range as that for women. This arises fortuitously because for any age and BMD at the femoral neck, the risk of hip fracture or a major osteoporotic fracture is the same in men and women [38–40]. However, the T-score cannot be used interchangeably with different techniques and at different sites, since the prevalence of osteoporosis and proportion of individuals allocated to any diagnostic category would vary (Table 2), as does the risk of fracture.
Table 2.
Estimates of T-scores and the prevalence of osteoporosis according to site and technique [36]
| Measurement site | Technique | T-score at 60 years | WHO classification | Prevalence of osteoporosis (%) |
|---|---|---|---|---|
| Spine | QCT | −2.5 | Osteoporosis | 50 |
| Spine | Lateral DXA | −2.2 | Low bone mass | 38 |
| Spine | DXA | −1.3 | Low bone mass | 14 |
| Forearm | DXA | −1. 4 | Low bone mass | 12 |
| Heel | Achilles | −1.5 | Low bone mass | 11 |
| Total hip | DXA | −0.9 | Normal | 6 |
| Heel | Sahara | −0.7 | Normal | 3 |
These considerations have led to the adoption of the femoral neck as the reference site [36], but do not preclude the use of other sites and technologies in clinical practice, though it should be recognised that the information derived from the T-score will differ from that provided by BMD at the femoral neck.
Measurement of multiple skeletal sites
A number of guidelines favour the concurrent use of BMD at the proximal femur and at the lumbar spine for patient assessment. Patients are defined as having osteoporosis on the basis of the lower of two T-scores [41, 42]. The prediction of fracture is, however, not improved overall by the use of multiple sites [43–45]. Selection of patients on the basis of a minimum value from two or more tests will, however, increase the number of patients selected. The same result can be achieved by less stringent criteria for the definition of osteoporosis, by defining osteoporosis, for example, as a T-score of ≤−2.0 SD rather than ≤−2.5 SD. Notwithstanding, the measurement of more than one site can aid in the assessment of individuals (discussed below).
Osteopenia
It is recommended that diagnostic criteria be reserved for osteoporosis and that osteopenia should not be considered a disease category. Rather, the description of osteopenia is solely intended for purposes of epidemiological description.
Prevalence of osteoporosis
Because the distribution of BMD in the young healthy population is normally distributed and bone loss occurs with advancing age, the prevalence of osteoporosis increases with age. The prevalence of osteoporosis in the largest countries in the EU (Germany, France, Italy, Spain and UK) using the WHO criteria is shown for women in Table 3 [13, 46]. Approximately 21 % of women aged 50–84 years are classified as having osteoporosis accounting for more than 12 million women in these countries.
Table 3.
Number (in thousands) of women with osteoporosis according to age in the EU5 using female-derived reference ranges at the femoral neck [13]
| Age group (years) | France | UK | Germany | Italy | Spain | EU5 |
|---|---|---|---|---|---|---|
| 50–54 | 135 | 127 | 192 | 128 | 95 | 695 |
| 55–59 | 200 | 175 | 265 | 180 | 126 | 974 |
| 60–64 | 286 | 276 | 328 | 276 | 175 | 1,385 |
| 65–69 | 271 | 308 | 489 | 335 | 215 | 1,672 |
| 70–74 | 364 | 365 | 718 | 464 | 270 | 2,236 |
| 75–79 | 484 | 411 | 672 | 546 | 368 | 2,543 |
| 80–84 | 526 | 417 | 686 | 558 | 357 | 2,612 |
| 50–84 | 2,266 | 2,079 | 3,350 | 2,487 | 1,606 | 12,117 |
These data assume that the distribution of femoral neck BMD is the same in these index countries. There may be small differences in the age- and sex-specific BMD in different European countries as well as within countries. If so, these differences in BMD are relatively small and insufficient to account for the observed differences in fracture rates (see below).
Risk factors for fracture
BMD
Assessment of BMD has provided a crucial determinant of fracture risk, and many guidelines have used BMD thresholds to determine whether treatments should be recommended. Intervention thresholds have ranged from T-scores of −3 SD to −1.5 SD depending on the clinical context, the country or health economic factors [1, 47–51]. The use of bone mass measurements for prognosis depends upon accuracy. Accuracy in this context is the ability of the measurement to predict fracture. In general, all densitometric techniques have high specificity but low sensitivity which varies with the cutoff chosen to designate high risk.
At the age of 50 years, for example, the proportion of women with osteoporosis who will fracture their hip, spine, forearm or proximal humerus in the next 10 years (i.e. positive predictive value) is approximately 45 %. Despite this, the overall detection rate for these fractures (sensitivity) is low, and 96 % of fractures at the spine, hip, forearm or proximal humerus will occur in women without osteoporosis [52]. The low sensitivity is one of the reasons why widespread population-based screening with BMD is not widely recommended in women at the time of the menopause [7].
Many cross-sectional and prospective population studies indicate that the risk for fracture increases by a factor of 1.5 to 3.0 for each standard deviation decrease in bone mineral density [31]. The ability of bone mineral density to predict fracture is comparable to the use of blood pressure to predict stroke and substantially better than serum cholesterol to predict myocardial infarction [7]. There are, however, significant differences in the performance of different techniques at different skeletal sites. In addition, the performance depends on the type of fracture that one wishes to predict [31, 53]. For example, BMD assessments by DXA to predict hip fracture are more predictive when measurements are made at the hip rather than at the spine or forearm (Table 4). For the prediction of hip fracture, the gradient of risk provided by hip BMD in a meta-analysis is 2.6 [31]. In other words, the fracture risk increases 2.6-fold for each SD decrease in hip BMD. Thus, an individual with a Z-score of −3 at the hip would have a 2.63 or greater than 15-fold higher risk than an individual of the same age with a Z-score of 0. Where the intention is to predict any osteoporotic fracture, the commonly used techniques are comparable: The risk of fracture increases approximately 1.5-fold for each standard deviation decrease in the measurement so that an individual with a measurement of 3 standard deviations below the average value for age would have a 1.53 or greater than 3-fold higher risk than an individual with an average BMD. Note that the risk of fracture in individuals with an average BMD is lower than the average fracture risk, since fracture risk is a convex function of BMD.
Table 4.
Age-adjusted increase in risk of fracture (with 95 % confidence interval) in women for every 1 SD decrease in bone mineral density (by absorptiometry) below the mean value for age (amended from [31], with permission from the BMJ Publishing Group)
| Site of measurement | Outcome | |||
|---|---|---|---|---|
| Forearm fracture | Hip fracture | Vertebral fracture | All fractures | |
| Distal radius | 1.7 (1.4–2.0) | 1.8 (1.4–2.2) | 1.7 (1.4–2.1) | 1.4 (1.3–1.6) |
| Femoral neck | 1.4 (1.4–1.6) | 2.6 (2.0–3.5) | 1.8 (1.1–2.7) | 1.6 (1.4–1.8) |
| Lumbar spine | 1.5 (1.3–1.8) | 1.6 (1.2–2.2) | 2.3 (1.9–2.8) | 1.5 (1.4–1.7) |
The performance characteristics of ultrasound are similar. Most studies suggest that measurements of broadband ultrasound attenuation or speed of sound at the heel are associated with a 1.5- to 2-fold increase in risk for each standard deviation decrease in the measured variable [32, 54]. Comparative studies indicate that these gradients of risk are very similar to those provided by peripheral assessment of bone mineral density at appendicular sites by absorptiometric techniques to predict any osteoporotic fracture [31]. However, the WHO criteria for the diagnosis of osteoporosis cannot be applied to ultrasound results.
Clinical risk factors
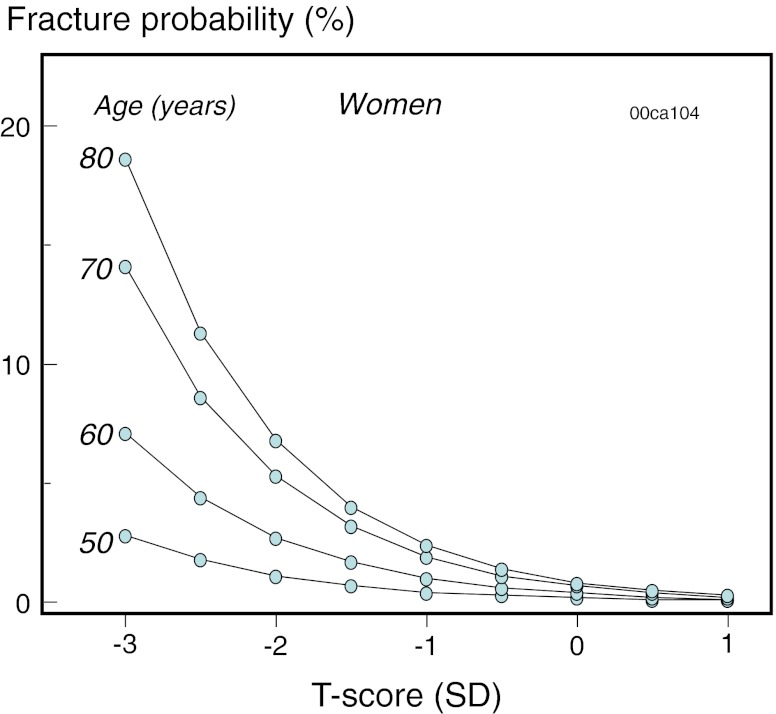
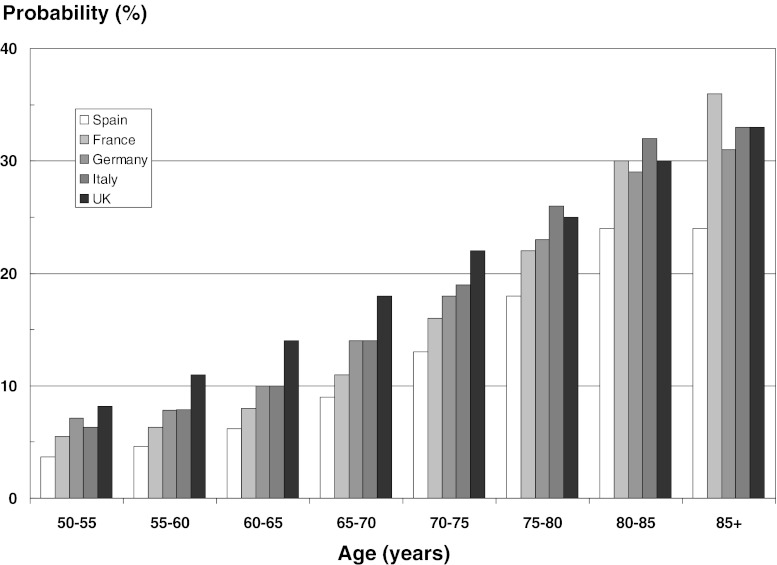
A large number of risk factors for fracture have been identified [55–57]. For the purposes of improving risk assessment, interest lies in those factors that contribute significantly to fracture risk over and above that provided by bone mineral density measurements or age [58]. A good example is age. The same T-score with the same technique at any one site has a different significance at different ages. For any BMD, fracture risk is much higher in the elderly than in the young [59]. This is because age contributes to risk independently of BMD. At the threshold for osteoporosis (T-score = −2.5 SD), the 10-year probability of hip fracture ranges 5-fold in women from Sweden depending on age (Fig. 1) [52]. Thus, the consideration of age and BMD together increases the range of risk that can be identified.
Fig. 1.
Ten-year probability of hip fracture in women from Sweden according to age and T-score for femoral neck BMD [52] with kind permission from Springer Science and Business Media
Over the past few years, a series of meta-analyses has been undertaken to identify additional clinical risk factors that could be used in case finding strategies, with or without the use of BMD. There are a number of factors to be considered in the selection of risk factors for case finding. Of particular importance, in the setting of primary care, is the ease with which they might be used. For a globally applicable tool, the chosen risk factors should also be valid in an international setting and their predictive value stable over time. A further and critical consideration is the reversibility of risk, i.e. is there evidence that the risk identified by a risk factor is amenable to therapeutic intervention (reversibility of risk—not reversible risk). Age is an example of an irreversible risk factor, but the risk of fracture identified by age has reversibility. The risk factors that are used for clinical assessment with FRAX are summarised in Table 5 [8, 38, 60–65]. Each of these risk factors has been shown to identify reversibility of risk [66].
Table 5.
Clinical risk factors used for the assessment of fracture probability ([8] with permission from the WHO Collaborating Centre, University of Sheffield, UK)
| Age |
| Sex |
| Low body mass index |
| Previous fragility fracture, particularly of the hip, wrist and spine, including morphometric vertebral fracture in adult life |
| Parental history of hip fracture |
| Glucocorticoid treatment (≥5 mg prednisolone daily or equivalent for 3 months or more) |
| Current smoking |
| Alcohol intake 3 or more units daily |
| Causes of secondary osteoporosis |
| •Rheumatoid arthritis |
| •Untreated hypogonadism in men and women, e.g. premature menopause, bilateral oophorectomy or orchidectomy, anorexia nervosa, chemotherapy for breast cancer, hypopituitarism, androgen deprivation therapy in men with prostate cancer |
| •Inflammatory bowel disease, e.g. Crohn's disease and ulcerative colitis. It should be noted that the risk is in part dependent on the use of glucocorticoids, but an independent risk remains after adjustment for glucocorticoid exposure. |
| •Prolonged immobility, e.g. spinal cord injury, Parkinson's disease, stroke, muscular dystrophy, ankylosing spondylitis |
| •Organ transplantation |
| •Type 1 and type 2 diabetes |
| •Thyroid disorders, e.g. untreated hyperthyroidism, thyroid hormone suppressive therapy |
| •Chronic obstructive pulmonary disease |
In the case of causes of secondary osteoporoses, the increase in fracture risk is presumed to be mediated by low BMD. The exceptions are glucocorticoid exposure and rheumatoid arthritis for which risks have been identified that are independent of BMD. A further candidate is type 2 diabetes mellitus since recent evidence suggests an important independent risk [67, 68].
It should be noted that falls risk is not included in Table 5, though it has been used in some risk engines [69, 70], since the risk of fracture that is identified may not be associated with reversibility of risk. For example, patients selected on the basis of risk factors for falling may respond less to agents that preserve bone mass than those selected on the basis of low BMD [71].
Biochemical assessment of fracture risk
Bone markers are increased after the menopause, and in several studies, the rate of bone loss varies according to the marker value [72]. Thus, a potential clinical application of biochemical indices of skeletal metabolism is in assessing fracture risk. Several prospective studies have shown that the serum levels and urinary excretion of markers of bone turnover correlate with subsequent risk of fractures in postmenopausal women [72, 73]. Thus, women that have marker values of bone turnover above the premenopausal range (25–40 % of postmenopausal women) have been shown in several—but not all—studies to have approximately a 2-fold increased risk of vertebral and non-vertebral fractures, including those at the hip, independently of age and of BMD. Currently, markers of bone turnover have not been validated sufficiently for fracture risk prediction, a topic that remains on the research agenda [74].
Assessment of fracture risk
Whereas BMD provides the cornerstone for the diagnosis of osteoporosis, the use of BMD alone is less than optimal as an intervention threshold for several reasons. Firstly, the fracture risk varies markedly in different countries, but the T-score varies only by a small amount. Secondly, the significance of any given T-score to fracture risk in women from any one country depends on age (see Fig. 1) and the presence of clinical risk factors. Intervention thresholds will also be determined in part by the cost and benefits of treatment. Whereas assessment guidelines have traditionally been based on BMD, the limitations above have stimulated the development of risk engines that integrate several risk factors for fracture. These include the Garvan fracture risk calculator [69], QFracture™ [70] and FRAX® [8, 75]. Of these, FRAX has been the most extensively used.
Introduction to FRAX
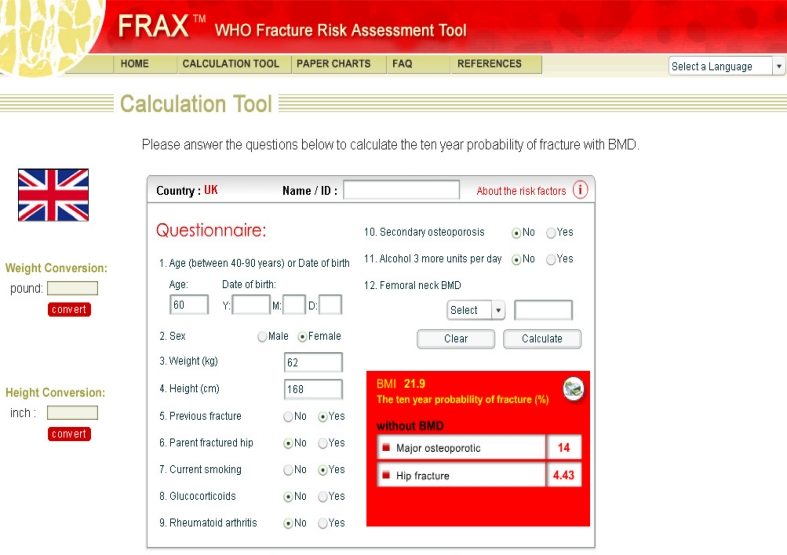
FRAX® is a computer-based algorithm (http://www.shef.ac.uk/FRAX) that calculates the 10-year probability of a major fracture (hip, clinical spine, humerus or wrist fracture) and the 10-year probability of hip fracture [8, 75, 76].
Fracture risk is calculated from age, body mass index and dichotomized risk factors comprising prior fragility fracture, parental history of hip fracture, current tobacco smoking, ever use of long-term oral glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis and alcohol consumption (Fig. 2). Femoral neck BMD can be optionally input to enhance fracture risk prediction [77]. Fracture probability is computed taking both the risk of fracture and the risk of death into account. The use of clinical risk factors in conjunction with BMD and age improves sensitivity of fracture prediction without adverse effects on specificity [77].
Fig. 2.
Screen page for input of data and format of results in the UK version of the FRAX® tool (UK model, version 3.5. http://www.shef.ac.uk/FRAX) [With permission of the World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School, UK]
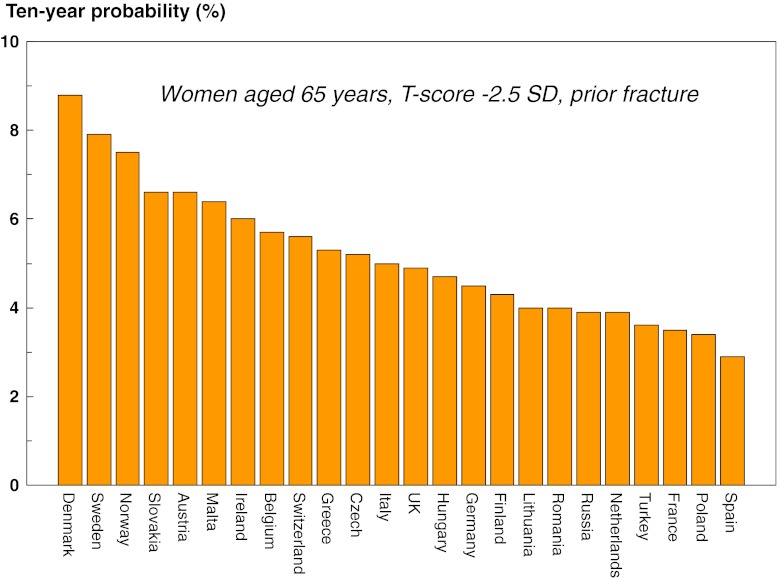
Fracture probability differs markedly in different regions of the world [78]. The heterogeneity in Europe is shown in Fig. 3. For this reason, FRAX is calibrated to those countries where the epidemiology of fracture and death is known (currently 45 countries).
Fig. 3.
Ten year probability (in percent) of a hip fracture in women from different European countries. BMI set to 24 kg/m2
Limitations of FRAX
The limitations of FRAX have been reviewed recently [79, 80]. The FRAX assessment takes no account of dose responses for several risk factors. For example, two prior fractures carry a much higher risk than a single prior fracture [79]. Dose responses are also evident for glucocorticoid exposure [81], cigarette smoking [82] and alcohol intake [62]. Since it is not possible to accommodate all such scenarios with the FRAX algorithm, these limitations should temper clinical judgement. Relatively simple arithmetic procedures have been formulated which, if validated, can be applied to conventional FRAX estimates of probabilities of hip fracture and a major fracture to adjust the probability assessment with knowledge of the dose of glucocorticoids (Table 6) [83]. For example, a woman aged 60 years from the UK taking glucocorticoids for rheumatoid arthritis (no other risk factors and BMI of 24 kg/m2) has a 10-year probability for a major fracture of 13 %. If she is on a higher than average dose of prednisolone (>7.5 mg daily), then the revised probability should be 15 % (13 × 1.15).
Table 6.
Average adjustment of 10-year probabilities of a hip fracture or a major osteoporotic fracture in postmenopausal women and older men according to dose of glucocorticoids (adapted from [83], with kind permission from Springer Science+Business Media B.V.)
| Dose | Prednisolone equivalent (mg/day) | Average adjustment over all ages |
|---|---|---|
| Hip fracture | ||
| Low | <2.5 | 0.65 |
| Medium | 2.5–7.5 | No adjustment |
| High | ≥7.5 | 1.20 |
| Major osteoporotic fracture | ||
| Low | <2.5 | 0.8 |
| Medium | 2.5–7.5 | No adjustment |
| High | ≥7.5 | 1.15 |
A further limitation is that the FRAX algorithm uses T-scores for femoral neck BMD. Whereas the performance characteristics of BMD at this site are as good as or better than other sites, the question arises whether T-scores from other sites and technologies can be used. Unfortunately, the T- and Z-scores vary according to the technology used and the site measured. Lumbar spine BMD is frequently measured by DXA and indeed is incorporated into several clinical guidelines [49–51, 84–86]. It is the site favoured for monitoring treatment, and there is thus much interest in the incorporation into FRAX of measurements at the lumbar spine. The same is true for peripheral measurements (and QUS) where there are no facilities for central DXA.
Although the measurement of two skeletal sites does not improve the general performance characteristics (sensitivity/specificity) of the BMD test in a given population [43], there are situations where there is a large discordance in the T-score at different skeletal sites in individuals for whom the use of this information will enhance the accuracy for the characterisation of risk, particularly if they lie close to an intervention threshold. The impact of spine/femoral neck T-score discordance has recently been explored in a large BMD-referral population from Manitoba, Canada. Fracture outcomes were available over a 10-year time frame. There was an approximately 10 % change in fracture risk for each unit of T-score discordance [87, 88]. On this basis, the authors propose that the clinician may ‘Increase/decrease FRAX estimate for a major fracture by one-tenth for each rounded T-score difference between the lumbar spine and femoral neck’.
Assessment of risk
At present, there is no universally accepted policy for population screening in Europe to identify patients with osteoporosis or those at high risk of fracture. With the increasing development of effective agents and price reductions, this view may change, particularly for elderly people. In the absence of such policies, patients are identified opportunistically using a case finding strategy on the finding of a previous fragility fracture or the presence of significant risk factors. The risk factors that are used for clinical assessment, summarised in Table 5, may be used, but in principle, any risk factor that alerts the physician to the possibility of osteoporosis is a candidate. Examples are height loss, thoracic kyphosis and the many other less well characterised causes of secondary osteoporosis.
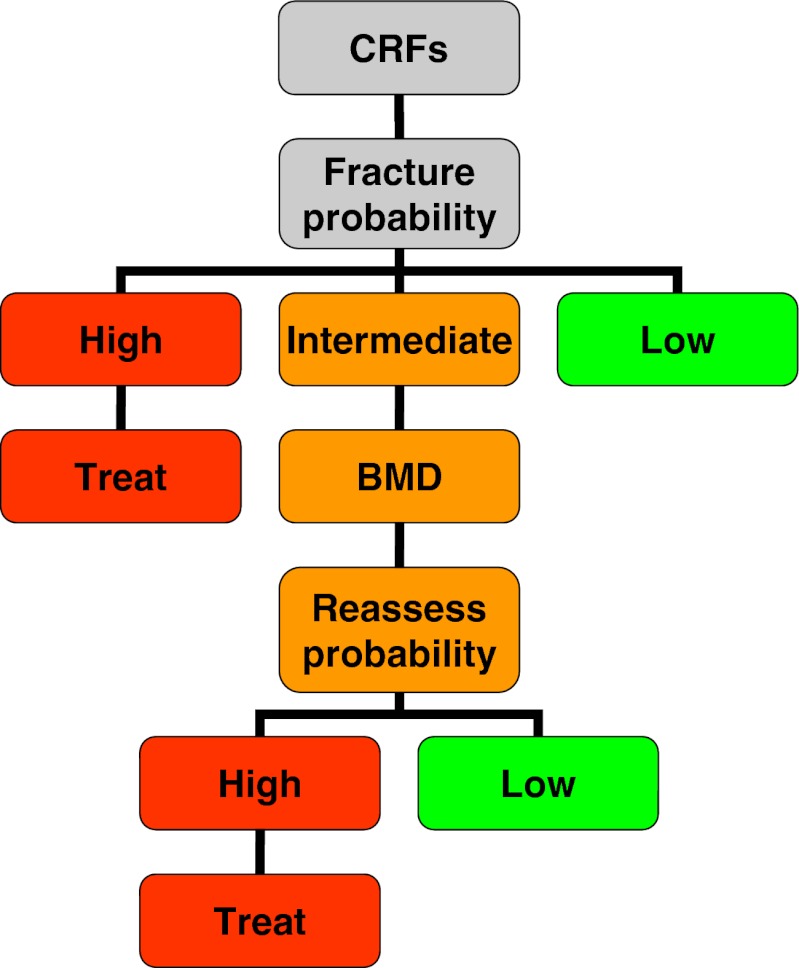
A general approach to risk assessment is shown in Fig. 4 [89]. The process begins with the assessment of fracture probability and the categorization of fracture risk on the basis of age, sex, BMI and the clinical risk factors. On this information alone, some patients at high risk may be considered for treatment without recourse to BMD testing. For example, many guidelines in Europe [1, 47, 89–98] recommend treatment in the absence of information on BMD in women with a previous fragility fracture (a prior vertebral or hip fracture in North America) [84, 99]. Many physicians would also perform a BMD test, but frequently, this is for reasons other than to decide on intervention, for example, as a baseline to monitor treatment. There will be other instances where the probability is so low that a decision not to treat can be made without BMD. Thus, not all individuals require a BMD test. The size of the intermediate category in Fig. 4 will vary in different countries. In countries that provide reimbursement for DXA, this will be a large category, whereas in a large number of countries with limited or no access to densitometry, the size of the intermediate group will necessarily be small. In other countries (e.g. the UK), where provision for BMD testing is sub-optimal [100], the intermediate category will lie between the two extremes.
Fig. 4.
Management algorithm for the assessment of individuals at risk of fracture [89] with kind permission from Springer Science and Business Media
Intervention thresholds
The use of FRAX in clinical practice demands a consideration of the fracture probability at which to intervene, both for treatment (an intervention threshold) and for BMD testing (assessment thresholds). Many approaches have been used to set intervention thresholds with FRAX [2, 84, 89, 99, 101–115]. The thresholds used have varied since they depend critically on local factors such as reimbursement issues, health economic assessment, willingness to pay for health care in osteoporosis and access to DXA. For this reason, it is not possible or desirable to recommend a unified intervention strategy. The strategy given below draws on that most commonly applied in Europe in the context of postmenopausal osteoporosis, but takes account that access to DXA varies markedly in different European countries [13, 100].
Since many guidelines recommend that women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test (other than to monitor treatment), a prior fracture can be considered to carry a sufficient risk that treatment can be recommended. For this reason, the intervention threshold in women without a prior fracture can be set at the age-specific fracture probability equivalent to women with a prior fragility fracture [89] and therefore rises with age from a 10-year probability of 8 to 33 % in the UK. In other words, the intervention threshold is set at the ‘fracture threshold’. This is the approach to intervention thresholds used in France, Switzerland and by the National Osteoporosis Guideline Group (NOGG) for the UK [101, 102, 116]. Incidentally, the same intervention threshold is applied to men, since the effectiveness and cost-effectiveness of intervention in men are broadly similar to that in women for equivalent risk [40, 117, 118]. The approach used has been well validated and the intervention strategy shown to be cost-effective [89, 119–124].
Using the same criteria, the intervention threshold will vary from country to country because the population risks (of fracture and death) vary [13, 78]. The fracture probability in women with a prior fracture in the five major EU countries is shown in Fig. 5. Probabilities are highest in the UK and lowest in Spain. The difference between countries is most evident at younger ages and becomes progressively less with advancing age.
Fig. 5.
The 10-year probability of a major osteoporotic fracture by age in women with a prior fracture and no other clinical risk factors in the five major EU countries as determined with FRAX (version 3.5). Body mass index was set to 24 kg/m2 without BMD
For the purposes of illustration in this guidance, an aggregate value is chosen. Thus, for the countries shown in Fig. 5, the mean probability of a major fracture in women with a prior fracture is 6.3 % between the ages of 50 and 55 years. The mean is weighted for population size in each age interval in each country. The probability rises with age (Table 7) and can be taken as an intervention threshold. Countries with much higher or lower probabilities may wish to develop intervention thresholds based on country-specific risks as has been proposed for the UK and Switzerland.
Table 7.
Intervention thresholds as set by FRAX-based 10-year probability (in percent) of a major osteoporotic fracture equivalent to women with a previous fracture (no other clinical risk factors, a body mass index of 24 kg/m2 and without BMD)
| Age range (years) | 10-year fracture probability (%) | ||
|---|---|---|---|
| Intervention threshold | Lower assessment threshold | Upper assessment threshold | |
| 40–44 | 5.2 | 2.3 | 6.2 |
| 45–49 | 5.4 | 2.4 | 6.5 |
| 50–54 | 6.3 | 2.9 | 7.6 |
| 55–59 | 7.6 | 3.6 | 9.1 |
| 60–64 | 9.9 | 4.9 | 11.9 |
| 65–69 | 13.4 | 6.9 | 16.1 |
| 70–74 | 17.6 | 9.7 | 21.5 |
| 75–79 | 23.0 | 13.7 | 27.6 |
| 80–84 | 29.1 | 18.7 | 34.9 |
| 85–89 | 31.8 | 20.9 | 38.2 |
| 90–94 | 31.7 | 20.8 | 38.0 |
| 95–99 | 32.2 | 21.1 | 38.6 |
| 100+ | 32.5 | 21.3 | 39.0 |
The lower assessment thresholds set by FRAX is based on the 10-year probability (in percent) of a major osteoporotic fracture equivalent to women without clinical risk factors (a body mass index of 24 kg/m2 and without BMD). The upper assessment threshold is set at 1.2 times the intervention threshold. Population weighted mean values for the five major EU countries
Assessment thresholds for BMD testing
The assessment strategy outlined in Fig. 4 requires the determination of assessment thresholds for making recommendations for the measurement of BMD. There are, in principle, two assessment thresholds [89]:
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold)
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold)
Most countries adopt a case finding strategy where individuals with clinical risk factors are identified for further assessment [8]. For this scenario, the lower assessment threshold can be set to exclude a requirement for BMD testing in women without clinical risk factors, as given in previous European guidelines [1, 2, 102, 111]. The probability equivalents are given in Table 7. In a few countries, population-based assessment with BMD is recommended (Germany and France in Europe). In such cases, there would be no lower assessment threshold
An upper threshold can be chosen to minimise the probability that a patient characterised to be at high risk on the basis of clinical risk factors alone would be reclassified to be at low risk with additional information on BMD [119]. In the UK, the upper assessment threshold was set at 1.2 times the intervention threshold [89]. The rationale is that reclassification of risk with the addition of a BMD test (from high risk to low risk and vice versa) is high when fracture probabilities estimated without BMD are close to the intervention threshold and the likelihood of reclassification decreases the further away the probability estimate is from the intervention threshold [119]. When patients have a fracture probability that is 20 % or more than the intervention threshold, almost no individuals will be reclassified (from high to low risk) when probabilities are recomputed with the addition of BMD to FRAX [119, 120, 123]. Thus, a quotient of 1.2 is applied to the intervention threshold, illustrated for the European example in Table 7. An attraction of the approach is that efficient use is made of BMD testing.
Application of probability thresholds
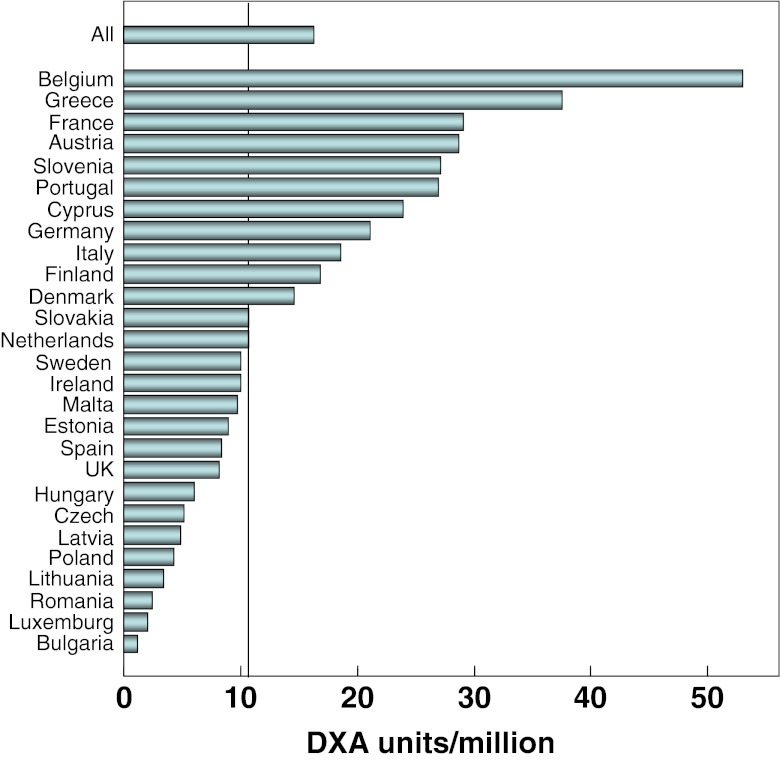
The application of these assessment thresholds depends critically on the availability (and reimbursement) of densitometry which varies from country to country. It has been estimated that the requirements to service osteoporosis amount to approximately 11 DXA units/million of the general population [100], though this estimate probably requires updating to take account of population demography. The availability of DXA falls above this estimate in a minority of European countries (Fig. 6). The large variation in resources for BMD testing demands the consideration of three assessment scenarios that depend on the access to central densitometry.
Fig. 6.
The density of central DXA equipment (units per million of the general population in the EU countries in 2010 [Kanis JA, data on file])
Unrestricted access to densitometry
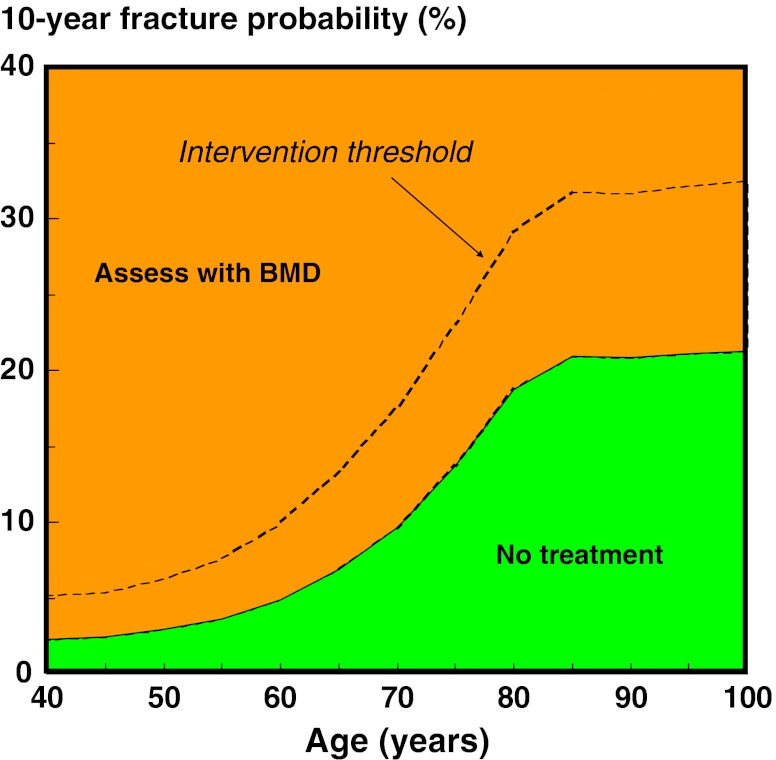
Where resources for BMD testing are adequate, BMD tests can be undertaken in women with any clinical risk factors as shown in Fig. 7. Treatment is recommended where fracture probability exceeds the intervention threshold. Note that the lower assessment threshold is set as equivalent to women without clinical risk factors (see above). In those countries where screening of women without risk factors is recommended, there would be no lower assessment threshold. An additional option is to recommend treatment in women with a prior fragility fracture without recourse to BMD (though BMD might be undertaken to monitor treatment).
Fig. 7.
Assessment of fracture risk in countries with high access to DXA. DXA is undertaken in women with a clinical risk factor. Assessment with DXA and/or treatment is not recommended where the FRAX probability is lower than the lower assessment threshold (green area). BMD is recommended in other women and treatment recommended where the fracture probability exceeds the intervention threshold (dotted line). The intervention threshold used is that derived from Table 7
The assessment algorithm is summarised in Box 1. BMD tests are recommended in all postmenopausal women with a clinical risk factor.
BOX 1 Assessment of fracture risk with FRAX with unlimited access to BMD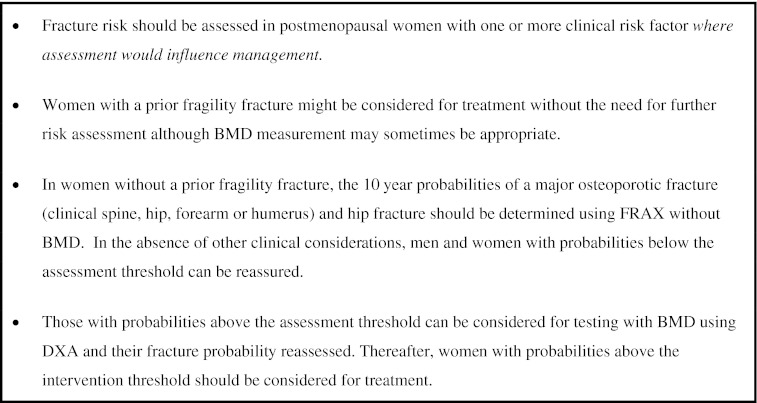
Limited access to densitometry
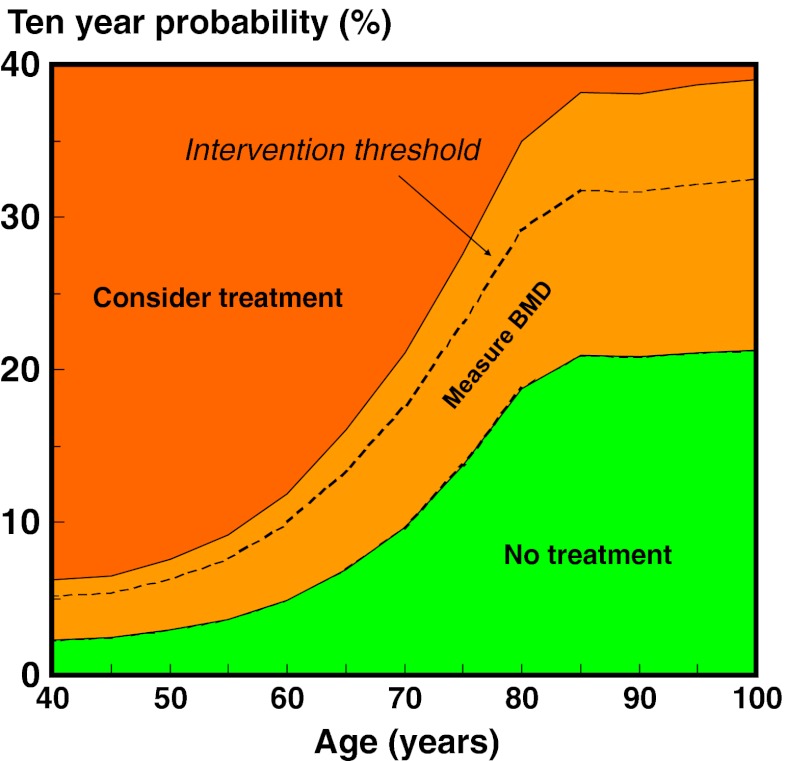
Several countries must take a parsimonious approach to the use of BMD, and this is reflected in the NOGG guidelines used in the UK. The guidance recommends that postmenopausal women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test. In women without a fragility fracture but with one or more other clinical risk factors (CRF), the intervention threshold set by NOGG is at the age-specific fracture probability equivalent to women with a prior fragility fracture and BMD testing is recommended in those in whom fracture probability lies between the upper and lower assessment threshold as described above [89]. This approach, adapted to the common EU thresholds shown in Table 7, is illustrated in Fig. 8.
Fig. 8.
Assessment guidelines based on the 10-year probability of a major fracture (in percent). The dotted line denotes the intervention threshold. Where assessment is made in the absence of BMD, a BMD test is recommended for individuals where the probability assessment lies in the orange region. The intervention threshold and BMD assessment thresholds used are those derived from Table 7
The assessment algorithm is summarised in Box 2.
BOX 2 Assessment of fracture risk with FRAX with limited access to BMD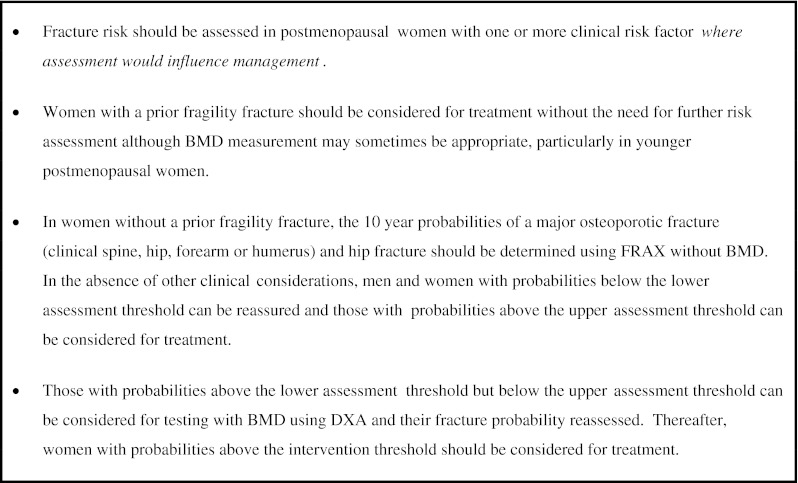
No access or patchy access to densitometry
In countries with very limited or no access to DXA, FRAX can be used without BMD. For the purpose of risk assessment, a characteristic of major importance is the ability of a technique to predict fractures, traditionally expressed as the increase in relative risk per SD unit decrease in risk score—termed the gradient of risk. The gradient of risk with FRAX is shown in Table 8 for the use of the clinical risk factors alone, femoral neck BMD and the combination [77].
Table 8.
Gradients of risk (the increase in fracture risk per SD change in risk score) with 95 % confidence intervals with the use of BMD at the femoral neck, clinical risk factors or the combination ([77] with kind permission from Springer Science+Business Media B.V.)
| Age (years) | Gradient of risk | ||
|---|---|---|---|
| BMD only | Clinical risk factors alone | Clinical risk factors + BMD | |
| (a) Hip fracture | |||
| 50 | 3.68 (2.61–5.19) | 2.05 (1.58–2.65) | 4.23 (3.12–5.73) |
| 60 | 3.07 (2.42–3.89) | 1.95 (1.63–2.33) | 3.51 (2.85–4.33) |
| 70 | 2.78 (2.39–3.23) | 1.84 (1.65–2.05) | 2.91 (2.56–3.31) |
| 80 | 2.28 (2.09–2.50) | 1.75 (1.62–1.90) | 2.42 (2.18–2.69) |
| 90 | 1.70 (1.50–1.93) | 1.66 (1.47–1.87) | 2.02 (1.71–2.38) |
| (b) Other osteoporotic fractures | |||
| 50 | 1.19 (1.05–1.34) | 1.41 (1.28–1.56) | 1.44 (1.30–1.59) |
| 60 | 1.28 (1.18–1.39) | 1.48 (1.39–1.58) | 1.52 (1.42–1.62) |
| 70 | 1.39 (1.30–1.48) | 1.55 (1.48–1.62) | 1.61 (1.54–1.68) |
| 80 | 1.54 (1.44–1.65) | 1.63 (1.54–1.72) | 1.71 (1.62–1.80) |
| 90 | 1.56 (1.40–1.75) | 1.72 (1.58–1.88) | 1.81 (1.67–1.97) |
The use of clinical risk factors alone provides a gradient of risk (GR) that lies between 1.4 and 2.1, depending upon age and the type of fracture predicted. These gradients are comparable to the use of BMD alone to predict fractures [31, 38]. For example, for the prediction of any osteoporotic fracture, the GR at the age of 70 years was 1.5 with femoral neck BMD [31]. With peripheral BMD, the gradient of risk is somewhat, though not significantly, lower (GR = 1.4/SD; 95 % CI = 1.3 − 1.5/SD). These data suggest that clinical risk factors alone are of value and can be used, therefore, in the many countries where DXA facilities are insufficient (Box 3). The rationale for the use of FRAX in the absence of access to BMD or limited access has been recently reviewed [66, 79]. Briefly, most of the risk factors incorporated within FRAX contribute to fracture risk independently of BMD but are not totally independent of BMD; thus, higher risk is associated with lower underlying BMD [119, 124].
BOX 3 Assessment of fracture risk with FRAX without BMD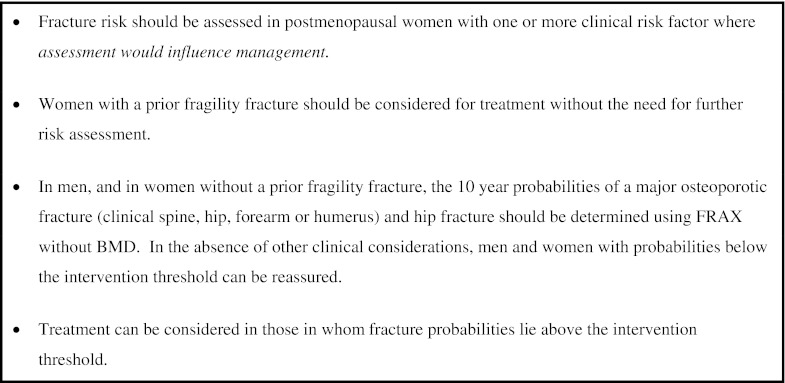
Alternative approaches to intervention thresholds
An alternative approach to intervention thresholds has been applied in Germany which uses a country-specific algorithm to estimate the 10-year incidence (not probability) of fracture [125]. A further important feature is that the output of the Dachverband Osteologie (DVO) model includes morphometric vertebral fractures, whereas the FRAX model considers clinically evident fractures. Rather than choosing a fracture threshold, a fixed threshold across all ages is used on the grounds that the use of the ‘fracture threshold’ is unfair age discrimination. The approach used is that patients are eligible for testing with BMD if the 10-year incidence of fracture is 20 % or greater. Patients are eligible for treatment where the T-score is −2.0 SD or less. Eligibility for testing is age and sex dependent. For example, a woman with a parental history of hip fracture is not eligible for assessment between the ages of 50 and 60 years, but becomes eligible for assessment from the age of 60 years. The corresponding age-dependent thresholds for men are 60–70 and >70 years, respectively.
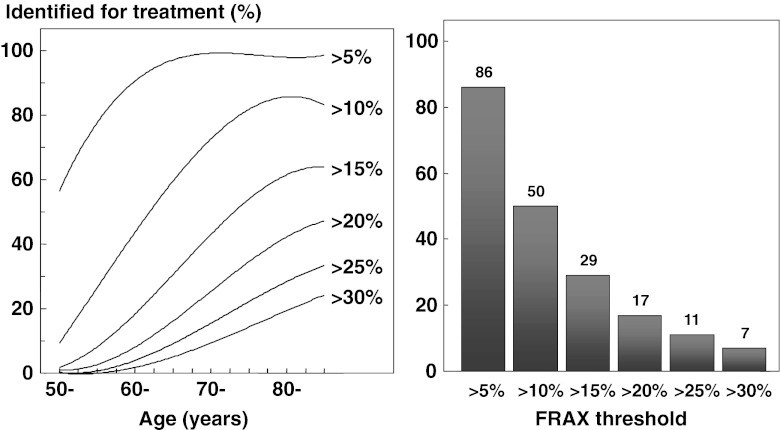
The impact of using a fixed intervention threshold is shown in Fig. 9 for postmenopausal women in the UK. At high thresholds, e.g. >20 % fracture probability, 17 % of postmenopausal women would be eligible for treatment. A problem that arises is that very few women under the age of 60 years would ever attain this threshold. On the other hand, if a less stringent threshold were chosen, say 10 %, then 10 % of women at the age of 50 years would exceed this threshold, the vast majority of women over the age of 65 would be eligible and the treatment threshold would be exceeded in 50 % of all postmenopausal women. Both scenarios could be justified on health economic criteria in the UK, but both are counterintuitive to clinical practice. In practice, this misdistribution is mitigated in the DVO guidelines in that patients with a prior hip fracture or two or more vertebral fractures are eligible for treatment without recourse to testing with BMD.
Fig. 9.
The impact of a fixed treatment threshold in postmenopausal women in the UK according to threshold values for the probability of a major fracture. The left-hand panel shows the proportion of the postmenopausal population exceeding the threshold shown at each age. The right-hand panel shows the proportion of the total postmenopausal population that exceeds a given threshold
An alternative approach has also been used in the USA. The National Osteoporosis Foundation recommends treatment for women who have had a prior spine or hip fracture and for women with a BMD at or below a T-score of −2.5 SD [99]. Treatment is not recommended in women with a T-score of >−1.0 SD. Thus, FRAX becomes relevant only in women with a T-score between −1 and −2.5 SD. Treatment is recommended in patients in whom the 10-year probability of a major fracture exceeds 20 % or when the 10-year probability of a hip fracture exceeds 3 %. The strategy differs from NOGG in that FRAX is always used with BMD. Indeed, a BMD test is a prerequisite. Additionally, a fixed intervention threshold is used at all ages, whereas the NOGG strategy uses an age-dependent threshold. The rationale for a fixed threshold is based on the fracture probability at which intervention becomes cost-effective in the USA and the 20% threshold is, therefore, not relevant for any other country.
Other assessment models
As well as the FRAX tool, other fracture risk calculators are available online which include the Garvan fracture risk calculator and QFracture™ [69, 70]. Their comparative features are summarised in Table 9. The QFracture™ tool is based on a UK prospective open cohort study of routinely collected data from 357 general practices on over 2 million men and women aged 30–85 years (www.qfracture.org). Like the FRAX tool, it takes into account history of smoking, alcohol, corticosteroid use, parental history (of hip fracture or osteoporosis) and several secondary causes of osteoporosis. Unlike FRAX, it also includes a history of falls (yes/no only over an unspecified time frame) and excludes previous fracture history and BMD. It has been internally validated (i.e. from a stratum of the same population) and also externally validated in the UK [126].
Table 9.
Comparative features of three fracture risk assessment algorithms
| Dubbo/Garvan | Qfracture | FRAX | |
|---|---|---|---|
| Externally validated | Yes (a few countries) | Yes (UK only) | Yes |
| Calibrated | No | Yes (UK only) | Yes |
| Applicability | Unknown | UK | 45 countries |
| Falls as an input variable | Yesa | Yes | No |
| BMD as an input variable | Yes | No | Yes |
| Prior fracture as an input variable | Yesa | No | Yes |
| Family history as an input variable | No | Yes | Yes |
| Output | Incidence | Incidence | Probability |
| Treatment responses assessed | No | No | Yes |
aAnd number of falls/prior fractures
The Garvan tool (www.garvan.org.au) is based on data from participants enrolled in the Australian Dubbo Osteoporosis epidemiology study of approximately 2,500 men and women age 60 years or more. It differs from FRAX by including a history of falls (categorised as 0, 1, 2 and >2 in the previous year) and the number of previous fragility fractures (categorised as 0, 1, 2 and >2), but does not include other FRAX variables. The output of the tool differs from FRAX in that it reports the risk of a larger number of fracture sites (additionally includes fractures of the distal femur, proximal tibia/fibula, distal tibia/fibula, patella, pelvis, ribs sternum, hands and feet excluding digits). As in the case of the QFracture, the Garvan tool captures fall risk.
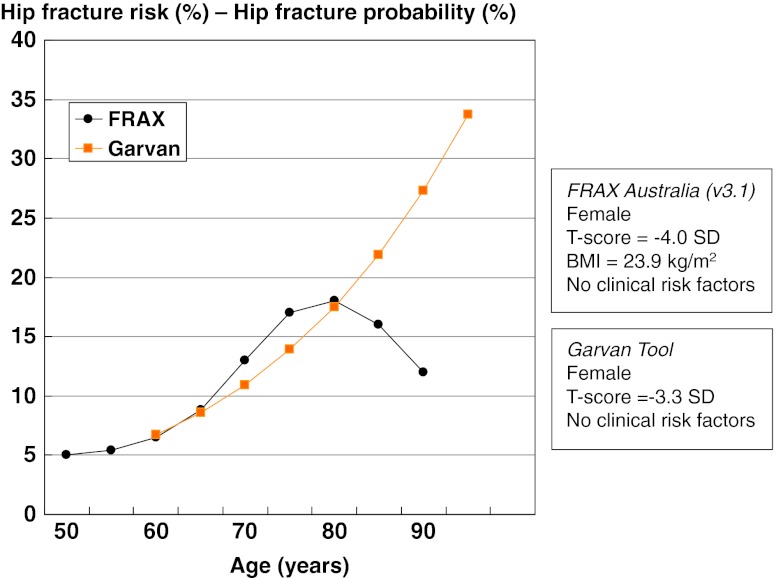
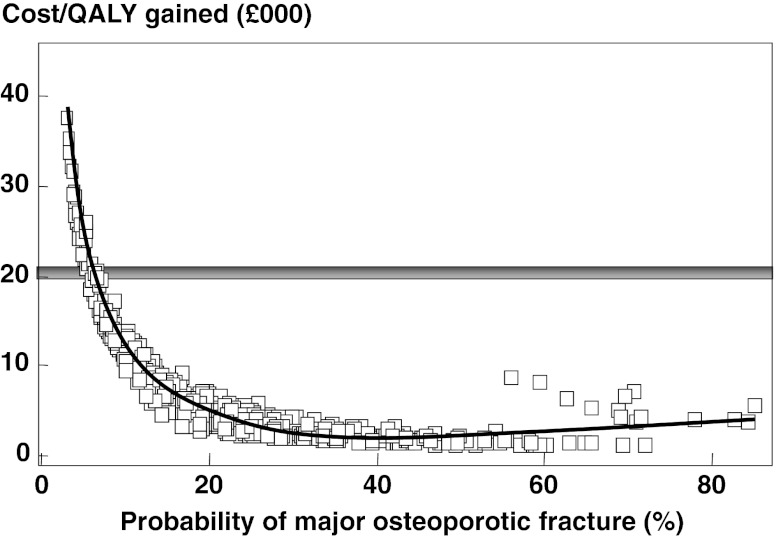
A fundamental difference between these risk models and FRAX is that the parameters of risk differ (incidence vs. probabilities) so that comparative data are not readily interpreted [127] (Fig. 10). In FRAX, fracture probability is computed taking both the risk of fracture and the risk of death into account. This is important because some of the risk factors affect the risk of death as well as the fracture risk. Examples include increasing age, sex, low BMI, low BMD, use of glucocorticoids and smoking.
Fig. 10.
The risk of hip fracture with age in a model that considers 10-year fracture risk alone (the Garvan tool) and FRAX which computes the probability of hip fracture from the fracture and death hazards (FRAX). The T-scores are set differently in the two models so that the risks are approximately equal at the age of 60 years. Data are computed from the respective websites [127]. With kind permission from Springer Science and Business Media
General management
Mobility and falls
Immobilisation is an important cause of bone loss. Immobilised patients may lose as much bone in a week when confined to bed than they would otherwise lose in a year. For this reason, immobility should, wherever possible, be avoided. The amount of weight-bearing exercise that is optimal for skeletal health in patients with osteoporosis is not known, but exercise forms an integral component of management [128–130]. Physiotherapy is an important component of rehabilitation after fracture. At all times, increased strength may prevent falls by improving confidence and coordination as well as maintaining bone mass by stimulating bone formation and by decreasing bone resorption, and by preserving muscle strength.
Such measures together can be coupled with a programme to reduce the likelihood of falls in those at high risk. Risk factors for falling are shown in Table 10 [131]. Modifiable factors such as correcting decreased visual acuity, reducing consumption of medication that alters alertness and balance and improving the home environment (slippery floors, obstacles, insufficient lighting, handrails) are important measures aimed at preventing falls [132, 133]. Although large trials have shown that it is possible to reduce falls [134, 135], randomised studies have not shown any significant decrease in fracture risk. Some randomised trials have shown that wearing hip protectors can markedly reduce hip fracture risk, particularly in the elderly living in nursing homes. A meta-analysis of well-conducted randomised controlled trials has, however, cast some doubt about the anti-fracture efficacy of this preventive measure [136–139].
Table 10.
Risk factors associated with falls (adapted from [131] with permission from Elsevier)
| 1. | Impaired mobility, disability |
| 2. | Impaired gait and balance |
| 3. | Neuromuscular or musculoskeletal disorders |
| 4. | Age |
| 5. | Impaired vision |
| 6. | Neurological, heart disorders |
| 7. | History of falls |
| 8. | Medication |
| 9. | Cognitive impairment |
Nutrition
At every stage of life, adequate dietary intakes of key bone nutrients such as calcium, vitamin D and protein contribute to bone health and reduce thereby the risk of osteoporosis and of fracture later in life [140]. Dietary sources of calcium are the preferred option, and calcium supplementation should only be targeted to those who do not get sufficient calcium from their diet and who are at high risk for osteoporosis. Calcium-rich foods such as dairy products contain additional nutrients that may also contribute to bone health [141].
The Recommended Nutrient Intakes (RNI) are at least 1,000 mg of calcium and 800 IU of vitamin D per day in men and women over the age of 50 years [142]. As calcium is mainly provided in dairies, calcium- and vitamin D-fortified dairy products (yoghurt, milk) providing at least 40 % of the RNI of calcium (400 mg) and 200 IU of vitamin D per portion are valuable options (e.g. yoghurt, such as Danone Densia/Danaos, or milk, such as Valio Plus Hyla) that are likely to improve long-term adherence.
There is a high prevalence of calcium, protein and vitamin D insufficiency in the elderly. Combined calcium and vitamin D supplements in a daily dose of 0.5–1.2 g and 400–800 IU, respectively, are generally recommended in patients receiving bone protective therapy, since most randomised controlled trial evidence for the efficacy of interventions is based on co-administration of the agent with calcium and vitamin D supplements [13]. Calcium and vitamin D supplements decrease secondary hyperparathyroidism and reduce the risk of proximal femur fracture, particularly in the elderly living in nursing homes. Intakes of at least 1,000 mg/day of calcium, 800 IU of vitamin D and of 1 g/kg body weight of protein can be recommended in the general management of patients with osteoporosis [140, 143].
Vitamin D supplements alone may reduce the risk of fracture and of falling provided the daily dose of vitamin D is greater than 700 IU [144]. In contrast, studies with large annual doses of vitamin D have reported an increased risk of hip fracture and, in one study, also of falls [145, 146]. Meta-analyses also indicate that vitamin D may have a small beneficial effect on cardiovascular risk and mortality [147, 148]. In contrast, a recent meta-analysis concluded that calcium supplements without co-administered vitamin D were associated with an increase in the risk of myocardial infarction by around 30 % [149]. Cardiovascular outcomes were not primary endpoints in any of the studies, and the association remains the subject of some controversy [150–156].
Whereas a gradual decline in caloric intake with age can be considered as an appropriate adjustment to the progressive reduction in energy expenditure, the parallel reduction in protein intake may be detrimental for maintaining the integrity and function of several organs or systems, including skeletal muscle and bone. Sufficient protein intakes are necessary to maintain the function of the musculoskeletal system, but they also decrease the complications that occur after an osteoporotic fracture. Correction of poor protein nutrition in patients with a recent hip fracture has been shown to improve the subsequent clinical course by significantly lowering the rate of complications, such as bedsores, severe anaemia, and intercurrent lung or renal infection. The duration of hospital stay of elderly patients with hip can thus be shortened [157].
Major pharmacological interventions
The most commonly used agents in Europe are raloxifene; the bisphosphonates alendronate, ibandronate, risedronate and zoledronic acid; agents derived from parathyroid hormone; denosumab and strontium ranelate. Until recently, hormone replacement treatment was also widely used. They have all been shown to reduce the risk of vertebral fracture. Some have also been shown to reduce the risk of non-vertebral fractures, and in some cases, agents have been shown specifically to decrease fracture risk at the hip (Table 11) [158, 159].
Table 11.
Anti-fracture efficacy of the most frequently used treatments for postmenopausal osteoporosis when given with calcium and vitamin D, as derived from randomised controlled trials (updated from [2])
| Effect on vertebral fracture risk | Effect on non-vertebral fracture risk | |||
|---|---|---|---|---|
| Osteoporosis | Established osteoporosisa | Osteoporosis | Established osteoporosisa | |
| Alendronate | + | + | NA | + (Including hip) |
| Risedronate | + | + | NA | + (Including hip) |
| Ibandronate | NA | + | NA | +b |
| Zoledronic acid | + | + | NA | +c |
| HRT | + | + | + | + (Including hip) |
| Raloxifene | + | + | NA | NA |
| Teriparatide and PTH | NA | + | NA | +d |
| Strontium ranelate | + | + | + (Including hipb) | + (Including hipb) |
| Denosumab | + | +c | + (Including hip) | +c |
NA no evidence available, + effective drug
aWomen with a prior vertebral fracture
bIn subsets of patients only (post hoc analysis)
cMixed group of patients with or without prevalent vertebral fractures
dShown for teriparatide only
Selective oestrogen-receptor modulators
Selective oestrogen-receptor modulators (SERMs) are nonsteroidal agents that bind to the oestrogen receptor and act as oestrogen agonists or antagonists, depending on the target tissue. The concept of SERMs was triggered by the observation that tamoxifen, which is an oestrogen antagonist in breast tissue, is a partial agonist on bone, reducing the rate of bone loss in postmenopausal women. Raloxifene is the only SERM widely available for the prevention and treatment of postmenopausal osteoporosis. Raloxifene prevents bone loss [160] and reduces the risk of vertebral fractures by 30–50 % in postmenopausal women with low bone mass and with osteoporosis with or without prior vertebral fractures as shown in the Multiple Outcomes of Raloxifene Evaluation (MORE) trial [161]. There was no significant reduction of non-vertebral fractures. In women with severe vertebral fractures at baseline (i.e. at highest risk of subsequent fractures), a post hoc analysis showed a significant reduction of non-vertebral fractures [160].
In the MORE study and its placebo controlled 4-year follow-up, the only severe (but rare) adverse event was an increase of deep venous thromboembolism. Hot flushes and lower limb cramps are commonly reported. There was a significant and sustained decrease of the risk of invasive breast cancer (by about 60 %) [162] that has been subsequently confirmed in two other large cohorts, including the STAR study that showed similar breast cancer incidences with raloxifene and tamoxifen in high-risk populations [163]. The RUTH study, performed in postmenopausal women at high risk of cardiovascular disease [164], showed that raloxifene had no effect on cardiovascular death and on the incidence of coronary heart disease and stroke [165]. The efficacy of raloxifene has been shown in women with osteopenia [166] and is not dependent on the level of fracture risk assessed by FRAX [167]. In summary, the overall risk benefit ratio of raloxifene is favourable, and the drug is approved widely for the prevention and treatment of postmenopausal osteoporosis.
Bazedoxifene is a selective oestrogen receptor modulator that has been approved in Europe but is only available in Spain and Germany. In phase 3 clinical trials, bazedoxifene was shown to significantly reduce the risk of new vertebral fracture, with favourable effects on bone mineral density, bone turnover markers and the lipid profile [168, 169]. In a subgroup of women at increased risk of fracture, bazedoxifene significantly decreased non-vertebral fracture risk. In contrast to raloxifene, the efficacy of bazedoxifene is dependent on the level of fracture risk assessed by FRAX [170]. In common with raloxifene, venous thromboembolic events, primarily deep vein thromboses, leg cramps and hot flushes were more frequently reported in the active treatment groups compared with the placebo group [171].
Bisphosphonates
Bisphosphonates are stable analogues of pyrophosphate characterised by a P–C–P bond. A variety of bisphosphonates has been synthesized, the potency of which depends on the length and structure of the side chain. Bisphosphonates have a strong affinity for bone apatite, both in vitro and in vivo, which is the basis for their clinical use. They are potent inhibitors of bone resorption and produce their effect by reducing the recruitment and activity of osteoclasts and increasing their apoptosis. The potency and chemical affinity to bone of bisphosphonates determines their effect to inhibit bone resorption and varies greatly from compound to compound. Potency differences can range 10,000-fold in vitro, so that the doses used clinically also vary. The mechanism of action on osteoclasts includes inhibition of the proton vacuolar adenosine triphosphatase (ATPase) and alteration of the cytoskeleton and the ruffled border. Aminobisphosphonates also inhibit the farnesyl pyrophosphate synthase step in the mevalonate pathway, thereby modifying the isoprenylation of guanosine triphosphate binding proteins.
Oral bioavailability of bisphosphonates is low, around 1 % of the dose ingested, and is impaired by food, calcium, iron, coffee, tea and orange juice. Bisphosphonates are quickly cleared from plasma, about 50 % being deposited in bone and the remainder excreted in urine. Their half-life in bone is very prolonged [172].
Alendronate 70 mg once weekly and risedronate 35 mg once weekly are the most commonly used bisphosphonates worldwide. In the Fracture Intervention study, alendronate was shown to reduce the incidence of vertebral, wrist and hip fractures by approximately half in women with prevalent vertebral fractures [173–175]. In women without prevalent vertebral fractures, there was no significant decrease in clinical fractures in the overall population, but the reduction was significant in one third of patients that had a baseline hip BMD T-score lower than −2.5 SD [176]. Risedronate in women with prevalent vertebral fractures has been shown to reduce the incidence of vertebral and non-vertebral fractures by 40–50 and 30–36 %, respectively [177, 178]. In a large population of elderly women, risedronate decreased significantly the risk of hip fractures (by 30 %), an effect that was greater in osteoporotic women aged 70–79 years (−40 %), while the decrease was not significant in women over the age of 80 years without documented evidence of osteoporosis [71].
Ibandronate given daily (2.5 mg) reduces the risk of vertebral fractures by 50–60 %, whereas an effect on non-vertebral fractures was only demonstrated in a post hoc analysis of women with a baseline of BMD T-score below −3 SD [179–181]. Bridging studies have shown that oral ibandronate 150 mg once monthly is equivalent or superior to daily ibandronate in increasing BMD and decreasing biochemical markers of bone turnover, giving rise to its approval for the prevention of vertebral fracture in postmenopausal osteoporosis [182]. Similarly, bridging studies comparing intermittent intravenous ibandronate to daily oral treatment have led to the approval of intravenous ibandronate 3 mg every 3 months for the same indication [183].
Based on the result of a phase II study [184], a large phase III trial in over 7,700 postmenopausal osteoporotic patients assessed the efficacy of yearly infusion of zoledronic acid 5 mg over 3 years. As compared to the placebo group, zoledronic acid was found to reduce the incidence of vertebral fractures by 70 % and that of hip fractures by 40 % [185], and is now available for the treatment of postmenopausal osteoporosis. Intravenous zoledronic acid has also been shown to decrease the risk of fracture and mortality when given shortly after a first hip fracture [186].
The overall safety profile of bisphosphonates is favourable. Oral bisphosphonates are associated with mild gastrointestinal disturbances, and some aminobisphosphonates (alendronate and pamidronate) can rarely cause oesophagitis. Intravenous amino-bisphosphonates can induce a transient acute-phase reaction with fever and bone and muscle pain that ameliorates or disappears after subsequent courses [187]. Osteonecrosis of the jaw has been described in cancer patients receiving high doses of intravenous pamidronate or zoledronate. The incidence in osteoporosis patients treated with oral and intravenous bisphosphonates appears to be very rare (in the order of 1/100,000 cases), and its causal relationship with bisphosphonate therapy has not been confirmed [157]. Recently, concerns have been raised about a possible association between bisphosphonate therapy and atrial fibrillation. Subsequent studies have produced conflicting results but have not excluded the possibility of such an association, and further investigation is warranted [188]. The possibility that bisphosphonate therapy is associated with increased risk of oesophageal cancer has been raised. Two recent studies from the General Practice Research Database in the UK have produced conflicting results, one failing to show any association but another concluding that there was an increased risk with extended use over 5 years [189, 190]. Finally, bisphosphonate use may be associated with atypical subtrochanteric fractures, but the case is unproven and requires further research [191]. Likewise, associations between bisphosphonate exposure and lower risks of mortality and cancer also require further scrutiny [192–195]. The risk–benefit ratio remains favourable for the use of bisphosphonates to prevent fractures [196].
A substantial body of evidence indicates that many generic formulations of alendronate are more poorly tolerated than the proprietary preparations which results in significantly poorer adherence and thus effectiveness [197].
Peptides of the parathyroid hormone family
The continuous endogenous production of parathyroid hormone (PTH), as seen in primary or secondary hyperparathyroidism, or its exogenous administration can lead to deleterious consequences for the skeleton, particularly on cortical bone. However, intermittent administration of PTH (e.g. with daily subcutaneous injections) results in an increase of the number and activity of osteoblasts, leading to an increase in bone mass and in an improvement in skeletal architecture at both cancellous and cortical skeletal sites.
The intact molecule (amino acids 1-84) and the 1-34 N-terminal fragment (teriparatide) are used for the management of osteoporosis. Based on their respective molecular weights, the equivalent dose of the teriparatide, relative to the 1-84 molecule, is 25 % (i.e. 20 and 40 μg of teriparatide is equivalent to 80 and 160 μg of 1-84 PTH, respectively). Treatment with either agent has been shown to reduce significantly the risk of vertebral fractures, whereas teriparatide has been shown to have an effect also on non-vertebral fractures. The recommended doses are, respectively, 20 μg of teriparatide and 100 μg of PTH (1-84) daily, given as a subcutaneous injection [198, 199]. Treatment with PTH has been studied when given for 18 to 24 months, and beneficial effects on non-vertebral fracture with teriparatide have been shown to persist for up to 30 months after stopping teriparatide [200].
The most common reported adverse events in patients treated with PTH or teriparatide are nausea, pain in the limbs, headache and dizziness. In normocalcaemic patients, slight and transient elevations of serum calcium concentrations have been observed following the injection PTH or teriparatide. Serum calcium concentrations reach a maximum between 4 and 6 h and return to baseline 16 to 24 h after each dose. The change is small, and routine monitoring of serum calcium during therapy is not required. PTH and teriparatide may cause small increases in urine calcium excretion, but the incidence of hypercalciuria does not differ from that in placebo-treated patients. However, these agents should be used with caution in patients with active or recent urolithiasis because of their potential to exacerbate the disorder. Isolated episodes of transient orthostatic hypotension are also reported. They typically resolve within minutes to a few hours and do not preclude continued treatment.
The use of peptides of the PTH family is contraindicated in conditions characterised by abnormally increased bone turnover (e.g. pre-existing hypercalcaemia; metabolic bone diseases other than primary osteoporosis, including hyperparathyroidism and Paget's disease of the bone; unexplained elevation of alkaline phosphatase; prior external beam or implant radiation therapy to the skeleton or in patients with skeletal malignancies or bone metastasis). Severe renal impairment is also a contraindication. Studies in rats have indicated an increased incidence of osteosarcoma, with long-term administration of very high doses of teriparatide from the time of weaning. These findings have not been considered relevant for patients treated with very much smaller doses of teriparatide.
Strontium ranelate
Strontium ranelate is registered and marketed for the treatment of postmenopausal osteoporosis, to reduce the risk of vertebral and hip fractures. Whilst animal studies suggest that strontium ranelate may uncouple the bone remodelling process, the mechanism of action in human subjects remains unclear. Nonetheless, studies conducted up to 5 years have shown fracture efficacy of strontium ranelate, at spinal and non-vertebral sites, in a wide range of patients, from osteopenia subjects to women over the age of 80 years, including osteoporotic patients with or without prior vertebral fractures [201, 202]. Like raloxifene, a meta-analysis of the phase 3 studies indicates that the efficacy of strontium ranelate appears independent of the level of fracture risk assessed by FRAX [203]. In contrast, a reduction in hip fracture rates has been reported in one study for women over the age of 74 years with low bone density at the femoral neck [202]. The decrease in fracture rates observed with strontium ranelate is of similar magnitude to that described for the oral bisphosphonates [201, 202]. In an open-label extension study, BMD increased continuously with strontium ranelate over 10 years in osteoporotic women. Vertebral (−35 %) and non-vertebral (−38 %) fracture incidence were lower between 5 and 10 years than those in a matched placebo group studied over 5 years [204].
The recommended daily dose is one 2-g sachet once daily by mouth. The absorption of strontium ranelate is reduced by food, milk and its derivative products, and the drug should be administered, therefore, between meals. Ideally, it should be taken at bedtime, preferably at least 2 h after eating. No dosage adjustment is required in relation to age or in patients with mild to moderate renal impairment (creatinine clearance 30–70 ml/min). Strontium ranelate is not recommended for patients with severe renal impairment (creatinine clearance below 30 ml/min).
Adverse events observed with strontium ranelate are usually mild and transient. The most common adverse events are nausea and diarrhoea which are generally reported at the beginning of treatment and usually disappear after the third month of treatment. An increase in the incidence of venous thromboembolism (VTE) (relative risk, 1.42; confidence interval, CI, 1.02, 1.98) has been reported when pooling all phase III studies in osteoporosis [205]. A causal relationship with VTE and the use of strontium ranelate has not been established. However, strontium ranelate is contraindicated in patients with a past history of thrombophlebitis. Treatment should be stopped in patients in high-risk situations for VTE such as prolonged immobilisation without appropriate preventive measures taken.
The post-marketing experience of patients treated with strontium ranelate reported cases of the drug reaction with eosinophilia and systemic symptoms syndrome (<20 for 570,000 patient-years of exposure) [206]. This incidence is in the vicinity of what has been previously reported as severe skin reactions, with most of the other currently marketed anti-osteoporosis medications [207]. A causative link has not been firmly established, as strontium is a trace element naturally present in the human body, and ranelic acid is poorly absorbed. Owing to the possible fatality linked to this syndrome, however, it is important to discontinue immediately strontium ranelate and other concomitant treatment known to induce the syndrome in the case of suspicious major skin disorders that occur within 2 months of starting treatment [208].
Denosumab
Critical molecules for the differentiation, activation and survival of osteoclasts are the receptor activator of nuclear factor NFkB (RANK); its ligand RANKL, a member of the tumour necrosis factor superfamily, and OPG, which acts as a decoy receptor for RANKL. A fully human antibody against RANKL has been developed. This antibody, denosumab, has been shown to specifically bind to RANKL with a very high affinity, preventing its interaction with the receptor RANK [209].
The anti-fracture efficacy of 60 mg denosumab given subcutaneously every 6 months has been evaluated in postmenopausal osteoporotic women. After 3 years, there was a 68 % reduction in the incidence of new vertebral fractures. The incidence of clinical vertebral fractures was similarly reduced by 69 %. The incidence of non-vertebral fractures was reduced by 20 % and of hip fractures by 40 % [210]. After completing the first 3 years of the study, women from the denosumab group had two more years of denosumab treatment (long-term group), and those from the placebo group had 2 years of denosumab exposure (cross-over group). In the long-term group, lumbar spine and total hip BMD increased further. Yearly fracture incidences for both groups were below rates observed in the placebo group of the 3-year trial and below rates projected for a ‘virtual untreated twin’ cohort [211]. The effects of denosumab on fracture risk are particularly marked in patients at high fracture probability [212].
Adverse events did not increase with long-term administration of denosumab. Two adverse events in the cross-over group were adjudicated as consistent with osteonecrosis of the jaw [211]. In a meta-analysis of four clinical trials, the relative risk of serious adverse events for the denosumab group compared with the placebo group was 1.33; of serious adverse events related to infection, 2.10; of neoplasm, 1.11; of study discontinuation due to adverse events, 1.10, and of death, 0.78. These risks were all non-significant [213].
The effects of the major pharmacological interventions on vertebral and hip fracture risk are summarised in Table 12.
Table 12.
Study details and anti-fracture efficacy (relative risk (RR) and 95 % CI) of the major pharmacological treatments used for postmenopausal osteoporosis when given with calcium and vitamin D, as derived from randomised controlled trials
| Intervention | Study | Entry criteria | Mean age (years) | Number of patients randomised | Fracture incidence (% over 3 years)a | RR (95%CI) | |
|---|---|---|---|---|---|---|---|
| Placebo | Drug | ||||||
| a. Vertebral fracture (high-risk population) | |||||||
| Alendronate, 5–10 mg | [173] | Vertebral fractures; BMD, ≤0.68 g/m2 | 71 | 2,027 | 15.0 | 8.0 | 0.53 (0.41–0.68) |
| Risedronate, 5 mg | [177] | 2 vertebral fractures or 1 vertebral fracture and T-score ≤−2.0 | 69 | 2,458 | 16.3 | 11.3 | 0.59 (0.43–0.82) |
| Risedronate, 5 mg | [178] | 2 or more vertebral fractures—no BMD entry criteria | 71 | 1,226 | 29.0 | 18.0 | 0.51 (0.36–0.73) |
| Raloxifene, 60 mg | [161] | Vertebral fractures—no BMD entry criteria | 66 | 7,705 | 21.2 | 14.7 | 0.70 (0.60–0.90) |
| Teriparatide, 20 μgc | [198] | Vertebral fractures and FN or LS T-score ≤−1 if less than 2 moderate fractures | 69 | 1,637 | 14.0 | 5.0 | 0.35 (0.22–0.55) |
| Ibandronate, 2.5 mg | [179] | Vertebral fractures and LS −5 < T-score ≤ −2.0 | 69 | 2,946 | 9.6 | 4.7 | 0.38 (0.25–0.59) |
| Ibandronate, 20 mg | [291] | Vertebral fractures and LS −5 < T-score ≤ −2.0 | 70 | 708 | 9.6 | 4.9 | 0.50 (0.34–0.74) |
| Strontium ranelate, 2 g | [201] | Vertebral fractures, LS BMD ≤0.840 g/m2 | 69 | 1,649 | 32.8 | 20.9 | 0.59 (0.48–0.73) |
| Zoledronic acid, 5 mg | [185] | FN T-score ≤−2.5, ± vertebral fracture, or T-score ≤−1.5 and 2+ mild or 1 moderate vertebral fracture | 73 | 7,765 | 10.9 | 3.3 | 0.30 (0.24–0.38) |
| b. Vertebral fracture (low-risk population) | |||||||
| Alendronate, 5–10 mgd | [176] | FN T-score ≤−2 | 68 | 4,432 | 3.8 | 2.1 | 0.56 (0.39–0.80) |
| Alendronate, 5–10 mg d | [176] | Subgroup of women, T-score <2.5 | NA | 1,631 | 4.0 | 2.0 | 0.50 (0.31–0.82) |
| Raloxifene, 60 mg | [161] | FN or LS T-score ≤−2.5, ± vertebral fractures | 66 | 7,705 | 4.5 | 2.3 | 0.50 (0.40–0.80) |
| Denosumab, 60 mg | [210] | TH or LS ≤−2.5 and >−4; 60–90 years | 72 | 7,868 | 7.2 | 2.3 | 0.32 (0.26–0.41) |
| c. Hip fracture | |||||||
| Alendronate, 5–0 mg | [173] | Vertebral fractures with BMD ≤0.68 g/m2 | 71 | 2,027 | 2.2 | 1.1 | 0.49 (0.23–0.99) |
| Alendronate, 5–10 mg d | [176] | FN T-score ≤−2b | 68 | 4,432 | 0.8 | 0.7 | 0.79 (0.43–1.44) |
| Alendronate, 5–10 mg d | [176] | FN T-score ≤−2.5b (subgroup analysis) | NA | 1,631 | 1.6 | 0.7 | 0.44 (0.18–1.97) |
| Risedronate, 2.5 and 5 mg | [71] | T-score <−3b or <−2b and ≥1 non-skeletal risk factor for hip fracture (subgroup analysis osteoporotic patients 70–79 years) | 77 | 9,331 | 3.2 | 1.9 | 0.60 (0.40–0.90) |
| Raloxifene, 60 and 120 mg | [161] | FN or LS T-score ≤−2.5, ± vertebral fractures | 66 | 7,705 | 0.7 | 0.8 | 1.10 (0.60–1.90) |
| Strontium ranelate, 2 g | [202] | Osteoporosis (T-score <−2.5) with or without prior fracture | 77 | 4,932 | 3.4 | 2.9 | 0.85 (0.61–1.19) |
| Strontium ranelate, 2 g | [202] | Age ≥74 with T-score ≤−2.4b (subgroup analysis) | 80 | 1,977 | 6.4 | 4.3 | 0.64 (0.412–0.997) |
| Zoledronic acid, 5 mg | [185] | FN T-score ≤−2.5 or less, ± vertebral fracture, or T-score ≤−1.5 and 2+ mild or 1 moderate vertebral fracture | 73 | 7,765 | 1.4 | 2.5 | 0.59 (0.42–0.83) |
| Denosumab, 60 mg | [210] | TH or LS ≤−2.5 and >−4; age 60–90 years | 72 | 7,868 | 1.2 | 0.7 | 0.60 (0.37–0.97) |
FN femoral neck, LS lumbar spine, NA not available
aExcept where indicated in column 1
bBMD adjusted to NHANES population
c20-month study
d4.2-year study
Combination and sequential treatments
These treatment regimens include the concomitant or sequential use of compounds sharing the same mode of action (e.g. two or more inhibitors of bone resorption) or agents with differing activities (e.g. an inhibitor of resorption plus an anabolic agent). The hope that synergies might be found by combination treatments has not yet been realised [2]. However, there are data that suggest that the administration of an inhibitor of resorption (bisphosphonate or SERM) after treatment with PTH analogues maintains or even potentiates the skeletal benefit observed during anabolic treatment [214, 215]. Conversely, the prior administration of bisphosphonates, particularly if associated with greater suppression of bone turnover, blunts or retards the effects of subsequent administration of bisphosphonates[216], PTH [217–219], denosumab [220] and strontium ranelate [221, 222].
Other pharmacological interventions
Calcitonin
Calcitonin is an endogenous polypeptide hormone that inhibits osteoclastic bone resorption [223]. Salmon calcitonin is approximately 40–50 times more potent than human calcitonin, and the majority of clinical trials have been performed with salmon calcitonin [224]. For clinical use, it can be administrated either by injection or nasal application, which provides a biological activity of 25–50 % compared with the injectable formulation (200 IU nasal calcitonin would be equivalent to 50 IU of the injectable formulation).
Calcitonin modestly increases bone mineral density at the lumbar spine and forearm [175, 225]. Calcitonin likely reduces the risk of vertebral fracture; however, the magnitude of the impact on these fractures remains questionable [175]. An effect on non-vertebral fractures remains equivocal [226, 227]. In addition, calcitonin may have an analgesic effect in women with acute vertebral fracture, which appears to be independent of its effect on osteoclastic resorption [224].
In conclusion, the drawbacks of repeated injections and the high costs of the nasal formulation preclude the long-term use of calcitonin as a first line in the treatment of osteoporosis. Analgesic properties may, however, be an interesting option for acute pain following a spinal fracture.
Hormone replacement therapy
Oestrogens reduce the accelerated bone turnover induced by menopause and prevent bone loss at all skeletal sites regardless of age and duration of therapy. Results from observational studies and randomised placebo controlled trials have shown that oestrogens decrease the risk of vertebral and non-vertebral fractures (including hip fracture) by about 30 %, regardless of baseline BMD [158, 228, 229]. When hormone replacement therapy (HRT) is stopped, bone loss resumes at the same rate as after menopause, but fracture protection may persist arguably for several years [230, 231].
The Women's Health Initiative suggests, however, that the long-term risks of HRT outweigh the benefits. In this large cohort of postmenopausal women in their 60s, the combined use of conjugated oestrogen and medroxyprogesterone acetate was associated with a 30 % increased risk of coronary heart disease (CHD) and breast cancer, and with a 40 % increase in stroke [232–234]. There was also a slight increase in the risk of dementia [235] and no clinically meaningful effect on health-related quality of life such as sleep disturbance or vasomotor symptoms [236]. In a subsequent analysis, the increase in breast cancer risk was much less in women not previously exposed to HRT [234]. In hysterectomized women receiving conjugated oestrogen alone, there was also a significant increase in stroke, but not of CHD and breast cancer, suggesting a deleterious effect of medroxyprogesterone acetate [237]. It has been postulated that the benefits of HRT outweigh the risks in younger postmenopausal women [238, 239], but so far, there is no placebo controlled study showing the long-term safety of such approaches. In most countries, HRT is only recommended for climacteric symptoms, at a dose as small as possible and for a limited period of time.
Etidronate
Etidronate is a weak bisphosphonate that has been shown to reduce vertebral fractures over 2 years but not subsequently, with no significant effect on non-vertebral fractures [240]. Thus, etidronate is not recommended as a first-line therapy for osteoporosis in most European countries.
Vitamin D derivatives
Alfacalcidol is a synthetic analogue of the vitamin D metabolite calcitriol (1,25-dihydroxyvitamin D3), and it is metabolized to calcitriol by its 25-hydroxylation in the liver. It is somewhat less potent than calcitriol. Both alfacalcidol and calcitriol are used in some countries for the treatment of osteoporosis. Several but not all studies show decreases in vertebral fracture risk [241–243]. The effects on bone mineral density have been less extensively studied. A few reports have suggested that alfacalcidol and calcitriol exert a direct action on muscle strength and decrease the likelihood of falling in elderly subjects [244].
The major problem with the use of the vitamin D derivatives is the risk of hypercalcaemia and hypercalciuria. Adverse effects of prolonged hypercalcaemia include impairment of renal function and nephrocalcinosis. The narrow therapeutic window demands the frequent surveillance of serum and possibly urine calcium in patients exposed to these agents. Calcium supplementation of the diet should be avoided or used with care.
Clodronate
Clodronate is a relatively weak bisphosphonate but has been shown to decrease the risk of vertebral and non-vertebral fractures in randomised controlled studies [245, 246]. It is widely available for the treatment of neoplastic bone disease but licenced for use in osteoporosis in only a few countries.
Vertebroplasty and kyphoplasty
In patients with recent vertebral fracture in whom pain persists for 2 to 3 weeks despite a well-conducted analgesic programme, injection of cement in the fractured vertebral body without (vertebroplasty) or with preceding balloon inflation (kyphoplasty) may lead to short-term reduction of pain. Whether this is related to the cement itself or to local anaesthetic is still unclear [247].
Adherence and monitoring of treatment
Adherence to treatment
When discussing adherence, there is a need to define the terminology [248], since a wide variety of definitions is used in the literature.
Adherence is a general term encompassing the aspects mentioned below.
Persistence describes for how long the medication is taken. Persistence could be expressed as number of days until drop-out or the proportion of the cohort still on the medication after a given time since first prescription. Non-persistence is assumed to be the same as discontinuation if a treatment gap is longer than a set number of days.
Compliance denotes the proximity to the treatment recommendation as given in the official product information (SPC). It is often simplified to mean the number of doses taken divided by the number of prescribed doses. This simplification does not include some important aspects of compliance, such as taking medication with food (for the oral bisphosphonates), at the correct time of the day, too-large doses to compensate for forgotten doses, pill dumping, etc.
Primary non-adherence is when the patient is prescribed a drug and then never fills the prescription.
Non-adherence to medical therapy is a widespread public health problem. It is estimated that only half of the patients comply with long-term therapy of which a substantial minority do not even redeem their prescription. Overcoming non-adherence presents particular challenges in asymptomatic bone diseases and other chronic, asymptomatic conditions. In such settings, the level of perceived threat to health does not motivate the patient to adhere to therapy. In addition, risk of non-adherence with any therapy increases with increased duration of treatment [249].
Poor adherence to medication is associated with adverse effects on outcomes in osteoporosis or osteopenia, and non-adherent patients have smaller decreases in rates of bone turnover, smaller gains in BMD and a significantly greater risk of fracture [182, 250–252]. Partial adherence also has a significant impact on cost-effectiveness [253]. Further, research is required to optimize thresholds of compliance and persistence, the impact of gap length, offset times and fraction of benefit [254].
Improving adherence to osteoporosis therapy requires effective patient/provider communication and close patient monitoring for the early identification of declining adherence. Patients' belief in a medication contributes to better adherence and can be improved by firmly associating treatment with expected benefits such as reduced risk of fracture and thereby an improved quality of life. Patients may be encouraged to adhere when presented with measurements of biochemical markers of bone turnover or their BMD results together with an explanation of how these measures relate to risk reduction. Another primary component of improving adherence is to use simplified or user-friendly treatment programmes [255, 256].
It should be noted that inadequate adherence can also take the form of improper drug administration, even when doses are not missed. An example is the malabsorption of oral bisphosphonates when taken with food. Such non-adherence poses the potential problems of decreased drug absorption and increased risk of adverse effects [257].
Monitoring of treatment with densitometry
The goal of bone-targeted drug therapy in a patient with osteoporosis is to significantly increase bone strength, in order to decrease the risk of fracture. In untreated men and women, BMDis one of the major determinants of bone strength, and low BMD is an important predictor of fracture. Whether the long-term anti-fracture efficacy of anti-osteoporotic drugs depends on the extent to which treatment can increase or maintain BMD is controversial [258]. Meta-regressions, based on summary statistics, demonstrate a stronger correlation between the change in BMD and fracture risk reduction than results based on the individual patient data [259, 260].
Whereas 16 % of vertebral fracture risk reduction after treatment with alendronate was attributed to an increase in BMD at the lumbar spine [261], larger increases in BMD at both the spine and hip, observed with alendronate, were associated with greater reductions in the risk of non-vertebral fractures. However, for patients treated with risedronate or raloxifene, changes in BMD predict even more poorly the degree of reduction in vertebral (raloxifene) or non-vertebral (risedronate) fractures. Of the effects of risedronate to reduce non-vertebral fractures, 12 and 7 % were attributed to changes in the spine and femoral neck BMD, respectively [262]. For raloxifene, the percentage changes in BMD accounted for 4 % of the observed vertebral fracture risk reduction [263]. Percent changes in total hip BMD at month 36 explained up to 35 % of the effect of denosumab to reduce new or worsening vertebral fractures and up to 84 % of the reduction in non-vertebral fracture risk [264]. It is reasonable to conclude, however, that early monitoring of BMD has limited value in the prediction of treatment responses with inhibitors of bone resorption.
For bone-forming agents, increases in BMD account for approximately one third of the vertebral fracture risk reduction with teriparatide [265]. Preliminary data suggest that a larger proportion (up to 74 %) of the anti-fracture efficacy of strontium ranelate might be explained by changes in total hip or femoral neck BMD [266, 267]. Further data are needed on the role of BMD monitoring in patients treated with bone-forming agents, but appear to be of greater value than their use with inhibitors of bone resorption.
In postmenopausal osteoporosis, treatment-induced increments in BMD with inhibitors of bone turnover are modest (typically 2 % per year) in comparison to the precision error of repeat measurements (typically 1–2 %) so that the time interval of repeat estimates must be sufficiently long in order to determine whether any change is real [268]. In the absence of other clinical imperatives, a 5-year interval may be appropriate. For other agents such as strontium ranelate and PTH derivatives, the treatment-induced increment (or apparent increment in the case of strontium ranelate) is much more rapid, and more frequent BMD tests may be considered.
Monitoring of treatment with biochemical markers of bone turnover
Several markers have been developed over the past 20 years that reflect the overall rate of bone formation and/or bone resorption. Most are immunoassays using antibodies that recognise specifically a component of bone matrix (i.e. type I collagen or non-collagenous proteins) that is released in the bloodstream during the process of either osteoblastic bone formation or osteoclastic resorption. Other assays recognise an enzymatic activity associated with the osteoblast (bone alkaline phosphatase) or the osteoclast (tartrate resistant acid phosphatase). The most informative ones for the monitoring of osteoporosis are procollagen I N-terminal extension peptide (P1NP) for assessing bone formation and C-telopeptide breakdown products (especially serum CTX) to assess bone resorption [72, 74, 269].
Treatment-induced changes in bone markers are more rapid than changes in BMD and are typically measured 3–6 months or so after starting treatment when treatment-induced changes are expected to be most evident. In a research setting, a significant association has been reported between the short-term decrease in markers of bone turnover with the use of antiresoptive agents and gains in BMD [270, 271]. More importantly, significant associations have been reported between the short-term decrease in markers of bone turnover and the reduction in risk of vertebral and non-vertebral fractures with the use of antiresorptive agents (raloxifene and bisphosphonates) [74, 272–276]. Changes in markers of bone turnover with strontium ranelate are of small magnitude and are unlikely to be clinically useful for the monitoring of treatment [201]. More research is required using standardised analytes before robust evidence-based recommendations can be given [74].
Investigation of patients with osteoporosis
Diagnostic workup
The same diagnostic approach should be undertaken in all patients with osteoporosis irrespective of the presence or absence of fragility fractures. However, the range of clinical and biological tests will depend on the severity of the disease, the age at presentation and the presence or absence of vertebral fractures. The aims of the clinical history, physical examination and clinical tests are:
To exclude a disease which can mimic osteoporosis (e.g. osteomalacia, myelomatosis)
To elucidate causes of osteoporosis and contributory factors
To assess the severity of osteoporosis to determine the prognosis of the disease, i.e. the risk of subsequent fractures
To select the most appropriate form of treatment
To perform baseline measurements for subsequent monitoring of treatment
The procedures that may be relevant to the investigation of osteoporosis are shown in Table 13. These investigations may be used to:
Establish the diagnosis of osteoporosis (e.g. DXA or X-rays)
Establish the cause (e.g. thyroid function tests for hyperthyroidism and urinary free cortisol for Cushing syndrome)
Establish differential diagnosis (e.g. protein electrophoresis for myeloma, and serum calcium and alkaline phosphatase for osteomalacia)
Table 13.
Routine procedures proposed in the investigation of osteoporosis
| Routine |
| History including the FRAX clinical risk factors |
| Examination including height and weight |
| Blood cell count, sedimentation rate, serum calcium, albumin, creatinine, phosphate, alkaline phosphatase and liver transaminases |
| Lateral radiograph of lumbar and thoracic spine |
| Bone densitometry (dual energy X-ray absorptiometry at hip and spine) |
| Other procedures |
| Lateral imaging DXA for vertebral fracture assessment (VFA) |
| Markers of bone turnover, when available |
Investigations commonly conducted in secondary care include a full blood count, ESR, serum calcium and phosphate, liver function tests and tests of renal function. Additional measurements include the biochemical indices of bone turnover, serum parathyroid hormone, serum 25-hydroxyvitamin D, serum or urine protein electrophoresis, fasting and 24-h urinary calcium, urinary free cortisol, thyroid function tests, IgA anti-tissue transglutaminase antibody or IgA endomysial antibody and (rarely) transiliac bone biopsy. Free testosterone, gonadotrophin and prolactin measurements may be of value in men. Assessment is guided by the clinical findings, and some patients who apparently have primary osteoporosis are subsequently found to have mild hyperparathyroidism or hyperthyroidism, systemic mastocytosis, the late appearance of osteogenesis imperfecta or osteomalacia.
Differential diagnosis of osteoporosis
Osteomalacia and malignancy commonly induce bone loss and fractures. Osteomalacia is characterised by a defect of mineralization of bone matrix most commonly attributable to impaired intake, production or metabolism of vitamin D. Other causes include impaired phosphate transport or the chronic use of some drugs such as aluminium salts (and other phosphate binding antacids), high doses of fluoride or etidronate and the chronic use of some anticonvulsants. In most cases, the diagnosis of osteomalacia is suspected by the clinical history and by abnormalities in biochemical tests such as low values of serum and urinary calcium, serum phosphate and 25-hydroxyvitamin D, and high values for alkaline phosphatase and parathyroid hormone. A transiliac bone biopsy after tetracycline labelling may be necessary to demonstrate unequivocally a defect in mineralization.
Diffuse osteoporosis with or without pathological fracture is common in patients with multiple myeloma, a condition suspected by the severity of bone pain, increased sedimentation rate and Bence Jones proteinuria, and identified by marrow aspirate and serum and urine (immuno) electrophoresis of proteins. Similarly, pathological fractures resulting from metastatic malignancies can mimic osteoporosis and can be excluded by clinical and radiological examination, biological tests such as tumour markers, and scintigraphy or other imaging techniques. Vertebral fractures in osteoporosis should be differentiated from vertebral deformities attributable to other disorders such as scoliosis, osteoarthrosis and Scheuermann's disease.
Health economics
There is an increasing need for management strategies to be placed in an appropriate health economic perspective for guideline development and for reimbursement. The type of evaluation used is principally cost-utility analysis as a measure of cost-effectiveness. In the context of evaluating treatments, this takes account not only of fractures avoided, but also of any change in morbidity and mortality from both beneficial and unwanted effects. Quality-adjusted life years (QALYs) are the accepted unit of measurement in health economic assessment of interventions using cost-utility analysis. In order to estimate QALYs, each year of life is valued according to its utility to the patient. Values range from 0, the least desirable health state, to 1, or perfect health. The decrement in utility associated with fractures is the cumulative loss of utility over time. There is, at present, little international consensus as to when treatment can be considered to be cost-effective [277–279]. One approach is to base the threshold value on a measure of a country's economic performance, and a value of about two times the GDP/capita has been suggested as a threshold that can be applied to Western economies [280]. On this basis, threshold values would be about €32,000 in the UK, close to the recommendation of the National Institute for Health and Clinical Excellence [50, 51]. Although the GDP per capita provides an index of affordability, there is also a marked heterogeneity in the proportion of GDP that countries are willing to devote to health care and in the proportion of the population at risk from osteoporotic fracture (i.e. elderly people). These factors will also affect what is an acceptable price to pay which need to be defined on a country by country basis [8].
Studies of intervention
There has been a rapid expansion of research on the cost-utility of interventions in osteoporosis which has been the subject of several reviews [50, 51, 118, 174, 281–283]. Despite the use of different models, different settings and payer perspectives, analyses suggest that there are cost-effective scenarios that can be found in the context of the management of osteoporosis for all but the most expensive interventions (Table 14). A pan-European study from 2004 estimated the cost-effectiveness of branded alendronate in nine countries [284]. In this study, alendronate was shown to be cost saving compared to no treatment in women with osteoporosis (with and without previous vertebral fracture) from the Nordic countries (Norway, Sweden and Denmark). The cost-effectiveness of alendronate compared to no treatment was also within acceptable ranges in Belgium, France, Germany, Italy, Spain, Switzerland and the UK. However, with the decreased price of generic alendronate, analyses based on a branded drug price have become obsolete and would require an update.
Table 14.
Comparison of the cost-effectiveness of alendronate with other interventions in women aged 70 years from the UK (data for treatments other than alendronate from [122], with permission from Elsevier)
| Intervention | T-score = −2.5 SD | No BMD | |
|---|---|---|---|
| No prior fracture | Prior fracture | Prior fracture | |
| Alendronate | 6,225 | 4,727 | 6,294 |
| Etidronate | 12,869 | 10,098 | 9,093 |
| Ibandronate daily | 20,956 | 14,617 | 14,694 |
| Ibandronate intermittent | 31,154 | 21,587 | 21,745 |
| Raloxifene | 11,184 | 10,379 | 10,808 |
| Raloxifene without breast cancer | 34,011 | 23,544 | 23,755 |
| Risedronate | 18,271 | 12,659 | 13,853 |
| Strontium ranelate | 25,677 | 18,332 | 19,221 |
| Strontium ranelate, post hoc analysis | 18,628 | 13,077 | 13,673 |
The advent of probability-based assessment has prompted the cost-effectiveness of interventions as a function of fracture probability. Several studies have examined the cost-effectiveness of intervention thresholds expressed in terms of fracture probability [109, 110, 117, 122, 285, 286]. In a study from the UK by Kanis et al. [122], generic alendronate was shown to be cost-effective in the prevention and treatment of fractures in postmenopausal women with a 10-year fracture probability for a major fracture that exceeded 7.5 % (Fig. 11). There was rather little difference in the threshold at different ages with a mean value of 7.0 %. Thus, the vast majority of treatment scenarios with alendronate can be considered as cost-effective (see Table 7).
Fig. 11.
Correlation between the 10-year probability of a major fracture (calculated with BMD) and cost-effectiveness of generic alendronate at the age of 50 years in women. Each point represents a particular combination of BMD and clinical risk factors (all possible combinations of CRFs at BMD T-scores between 0 and −3.5 SD in 0.5 SD steps—512 combinations) with a BMI set to 26 kg/m2. The horizontal line denotes the threshold for cost-effectiveness (a willingness to pay of £20,000/QALY gained) ([122], with permission from Elsevier)
Other drugs that are approved for osteoporosis are associated with higher cost-effectiveness ratios compared to no treatment mainly due to their higher price. A recent study by Borgström et al. [287], again conducted in a UK setting, showed that risedronate was cost-effective above a 10-year probability of 13 % for a major osteoporotic fracture. Other studies have examined strontium ranelate and denosumab in this way [288, 289]. However, the cost-effectiveness of different interventions will vary between countries due to differences in drug costs, fracture risk, costs of treating fractures, utility estimates and willingness to pay.
Despite differences in apparent cost-effectiveness, there is, however, no proven difference in efficacy between the majority of treatments [47, 290], and head-to-head comparisons of interventions with fracture outcomes are not available. For these reasons, the value of an incremental analysis between the individual treatments is questionable, since any resulting hierarchy of treatments is dependent largely on price, but otherwise meaningless in clinical terms. In addition, the large number of untreated patients makes ‘no treatment’ a relevant comparator. Notwithstanding, alendronate has been considered as a first-line intervention. The view arises, not because of apparent differences in efficacy between treatments, but because of cost. However, the poor effectiveness and side effect profile of many generic formulations challenge this view [197].
Acknowledgments
We are grateful to the IOF Committee of Scientific Advisors and the ESCEO Scientific Advisory Board for their review of this paper and its endorsement. The paper updates the earlier guidance of ESCEO [2] ‘European guidance for the diagnosis and management of osteoporosis in postmenopausal women’, and some sections of text are reproduced with kind permission from Springer Science+Business Media B.V. We would like to thank Emma McCloskey for assistance in referencing this manuscript.
Conflicts of interest
None.
References
- 1.Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D. Guidelines for diagnosis and management of osteoporosis. The European Foundation for Osteoporosis and Bone Disease. Osteoporos Int. 1997;7:390–406. doi: 10.1007/BF01623782. [DOI] [PubMed] [Google Scholar]
- 2.Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, Rizzoli R. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19:399–428. doi: 10.1007/s00198-008-0560-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int. 2004;15:767–778. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 4.Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006;35:293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Haaland DA, Cohen DR, Kennedy CC, Khalidi NA, Adachi JD, Papaioannou A. Closing the osteoporosis care gap: increased osteoporosis awareness among geriatrics and rehabilitation teams. BMC Geriatr. 2009;9:28. doi: 10.1186/1471-2318-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Consensus Development Conference Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-E. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organisation Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129. [PubMed] [Google Scholar]
- 8.Kanis JA, on behalf of the WHO Scientific Group . Assessment of osteoporosis at the primary health-care level. Technical Report. UK: WHO Collaborating Centre, University of Sheffield; 2008. [Google Scholar]
- 9.Nguyen T, Sambrook P, Kelly P, Jones G, Lord S, Freund J, Eisman J. Prediction of osteoporotic fractures by postural instability and bone density. BMJ. 1993;307:1111–1115. doi: 10.1136/bmj.307.6912.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B. Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int. 2000;11:669–674. doi: 10.1007/s001980070064. [DOI] [PubMed] [Google Scholar]
- 11.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 12.Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N. Assessment of fracture risk. Osteoporos Int. 2005;16:581–589. doi: 10.1007/s00198-004-1780-5. [DOI] [PubMed] [Google Scholar]
- 13.Strom O, Borgstrom F, Kanis JA, Compston JE, Cooper C, McCloskey E, Jonsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos doi:10.1007/s11657-011-0060-1 [DOI] [PubMed]
- 14.Kanis JA, Compston J, Cooper C, et al. The burden of fractures in the European Union in 2010. Osteoporos Int. 2012;23(Suppl 2):S57. [Google Scholar]
- 15.Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 16.Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32:468–473. doi: 10.1016/S8756-3282(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 17.Blake GM, Fogelman I. Role of dual-energy X-ray absorptiometry in the diagnosis and treatment of osteoporosis. J Clin Densitom. 2007;10:102–110. doi: 10.1016/j.jocd.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Engelke K, Gluer CC. Quality and performance measures in bone densitometry: part 1: errors and diagnosis. Osteoporos Int. 2006;17:1283–1292. doi: 10.1007/s00198-005-0039-0. [DOI] [PubMed] [Google Scholar]
- 19.Gluer CC, Lu Y, Engelke K. Quality and performance measures in bone densitometry. Part 2: fracture risk. Osteoporos Int. 2006;17:1449–1458. doi: 10.1007/s00198-005-0038-1. [DOI] [PubMed] [Google Scholar]
- 20.Ranjanomennahary P, Ghalila SS, Malouche D, Marchadier A, Rachidi M, Benhamou C, Chappard C. Comparison of radiograph-based texture analysis and bone mineral density with three-dimensional microarchitecture of trabecular bone. Med Phys. 2011;38:420–428. doi: 10.1118/1.3528125. [DOI] [PubMed] [Google Scholar]
- 21.Fouque-Aubert A, Boutroy S, Marotte H, Vilayphiou N, Lespessailles E, Benhamou CL, Miossec P, Chapurlat R. Assessment of hand trabecular bone texture with high resolution direct digital radiograph in rheumatoid arthritis: a case control study. Joint Bone Spine. 2011;79:379–383. doi: 10.1016/j.jbspin.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Hans D, Goertzen AL, Krieg MA, Leslie WD. Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res. 2011;26:2762–2769. doi: 10.1002/jbmr.499. [DOI] [PubMed] [Google Scholar]
- 23.Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA. Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom. 2011;14:302–312. doi: 10.1016/j.jocd.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Genant HK, Lang TF, Engelke K, Fuerst T, Gluer C, Majumdar S, Jergas M. Advances in the noninvasive assessment of bone density, quality, and structure. Calcif Tissue Int. 1996;59(Suppl 1):S10–S15. doi: 10.1007/s002239900169. [DOI] [PubMed] [Google Scholar]
- 25.Mazess RB, Collick B, Trempe J, Barden H, Hanson J. Performance evaluation of a dual energy x-ray bone densitometer. Calcif Tissue Int. 1998;44:228–232. doi: 10.1007/BF02556569. [DOI] [PubMed] [Google Scholar]
- 26.Schousboe JT, Ensrud KE, Nyman JA, Kane RL, Melton LJ., 3rd Potential cost-effective use of spine radiographs to detect vertebral deformity and select osteopenic post-menopausal women for amino-bisphosphonate therapy. Osteoporos Int. 2005;16:1883–1893. doi: 10.1007/s00198-005-1956-7. [DOI] [PubMed] [Google Scholar]
- 27.Schousboe JT, Ensrud KE, Nyman JA, Kane RL, Melton LJ., 3rd Cost-effectiveness of vertebral fracture assessment to detect prevalent vertebral deformity and select postmenopausal women with a femoral neck T-score >-2.5 for alendronate therapy: a modeling study. J Clin Densitom. 2006;9:133–143. doi: 10.1016/j.jocd.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 28.Vokes T, Bachman D, Baim S, Binkley N, Broy S, Ferrar L, Lewiecki EM, Richmond B, Schousboe J. Vertebral fracture assessment: the 2005 ISCD Official Positions. J Clin Densitom. 2006;9:37–46. doi: 10.1016/j.jocd.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Ferrar L, Jiang G, Schousboe JT, DeBold CR, Eastell R. Algorithm-based qualitative and semiquantitative identification of prevalent vertebral fracture: agreement between different readers, imaging modalities, and diagnostic approaches. J Bone Miner Res. 2008;23:417–424. doi: 10.1359/jbmr.071032. [DOI] [PubMed] [Google Scholar]
- 30.McCloskey EV, Vasireddy S, Threlkeld J, Eastaugh J, Parry A, Bonnet N, Beneton M, Kanis JA, Charlesworth D. Vertebral fracture assessment (VFA) with a densitometer predicts future fractures in elderly women unselected for osteoporosis. J Bone Miner Res. 2008;23:1561–1568. doi: 10.1359/jbmr.080515. [DOI] [PubMed] [Google Scholar]
- 31.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gluer CC. Quantitative ultrasound techniques for the assessment of osteoporosis: expert agreement on current status. The International Quantitative Ultrasound Consensus Group. J Bone Miner Res. 1997;12:1280–1288. doi: 10.1359/jbmr.1997.12.8.1280. [DOI] [PubMed] [Google Scholar]
- 33.Watts NB. Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA) Osteoporos Int. 2004;15:847–854. doi: 10.1007/s00198-004-1681-7. [DOI] [PubMed] [Google Scholar]
- 34.Kanis JA, Melton LJ, 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 35.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42:467–475. doi: 10.1016/j.bone.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Kanis JA, Gluer CC. An update on the diagnosis and assessment of osteoporosis with densitometry. Committee of Scientific Advisors, International Osteoporosis Foundation. Osteoporos Int. 2000;11:192–202. doi: 10.1007/s001980050281. [DOI] [PubMed] [Google Scholar]
- 37.Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr, Lindsay R. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8:468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]
- 38.Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185–1194. doi: 10.1359/JBMR.050304. [DOI] [PubMed] [Google Scholar]
- 39.De Laet CEDH, Van Hout BA, Burger H, Hofman A, Weel AE, Pols H. Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res. 1998;13:1587–1593. doi: 10.1359/jbmr.1998.13.10.1587. [DOI] [PubMed] [Google Scholar]
- 40.Kanis JA, Bianchi G, Bilezikian JP, Kaufman JM, Khosla S, Orwoll E, Seeman E. Towards a diagnostic and therapeutic consensus in male osteoporosis. Osteoporos Int. 2011;22:2789–2798. doi: 10.1007/s00198-011-1632-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lewiecki EM, Watts NB, McClung MR, Petak SM, Bachrach LK, Shepherd JA, Downs RW., Jr Official positions of the International Society for Clinical Densitometry. J Clin Endocrinol Metab. 2004;89:3651–3655. doi: 10.1210/jc.2004-0124. [DOI] [PubMed] [Google Scholar]
- 42.Binkley N, Bilezikian JP, Kendler DL, Leib ES, Lewiecki EM, Petak SM. Official positions of the International Society for Clinical Densitometry and Executive Summary of the 2005 Position Development Conference. J Clin Densitom. 2006;9:4–14. doi: 10.1016/j.jocd.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 43.Blake GM, Patel R, Knapp KM, Fogelman I. Does the combination of two BMD measurements improve fracture discrimination? J Bone Miner Res. 2003;18:1955–1963. doi: 10.1359/jbmr.2003.18.11.1955. [DOI] [PubMed] [Google Scholar]
- 44.Kanis JA, Johnell O, Oden A, et al. The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int. 2006;17:527–534. doi: 10.1007/s00198-005-0014-9. [DOI] [PubMed] [Google Scholar]
- 45.Leslie WD, Lix LM, Tsang JF, Caetano PA. Single-site vs multisite bone density measurement for fracture prediction. Arch Intern Med. 2007;167:1641–1647. doi: 10.1001/archinte.167.15.1641. [DOI] [PubMed] [Google Scholar]
- 46.Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone. 2000;27:585–590. doi: 10.1016/S8756-3282(00)00381-1. [DOI] [PubMed] [Google Scholar]
- 47.Osteoporosis: clinical guidelines for the prevention and treatment. London: RCP; 1999. [Google Scholar]
- 48.Glucocorticoid-induced osteoporosis. Guidelines on prevention and treatment. Bone and Tooth Society of Great Britain, National Osteoporosis Society and Royal College of Physicians. London: RCP; 2002. [Google Scholar]
- 49.Clinician's guide to prevention and treatment of osteoporosis. Washington: NOF; 2008. [Google Scholar]
- 50.NICE technology appraisal guidance 161 (amended). Alendronate, etidronate, risedronate, raloxifene, strontium ranelate and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women (amended) London: NICE; 2011. [Google Scholar]
- 51.NICE technology appraisal guidance 160 (amended). Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended) London: NICE; 2011. [Google Scholar]
- 52.Kanis JA, Johnell O, Oden A, Dawson A, De Laet C, Jonsson B. Ten year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int. 2001;12:989–995. doi: 10.1007/s001980170006. [DOI] [PubMed] [Google Scholar]
- 53.Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM. Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet. 1993;341:72–75. doi: 10.1016/0140-6736(93)92555-8. [DOI] [PubMed] [Google Scholar]
- 54.Moayyeri A, Adams JE, Adler RA, Krieg MA, Hans D, Compston J, Lewiecki EM. Quantitative ultrasound of the heel and fracture risk assessment: an updated meta-analysis. Osteoporos Int. 2012;23:143–153. doi: 10.1007/s00198-011-1817-5. [DOI] [PubMed] [Google Scholar]
- 55.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 56.Ribot C, Pouilles JM, Bonneu M, Tremollieres F. Assessment of the risk of post-menopausal osteoporosis using clinical factors. Clin Endocrinol (Oxf) 1992;36:225–228. doi: 10.1111/j.1365-2265.1992.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 57.Poor G, Atkinson EJ, O'Fallon WM, Melton LJ., 3rd Predictors of hip fractures in elderly men. J Bone Miner Res. 1995;10:1900–1907. doi: 10.1002/jbmr.5650101209. [DOI] [PubMed] [Google Scholar]
- 58.Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359:1929–1936. doi: 10.1016/S0140-6736(02)08761-5. [DOI] [PubMed] [Google Scholar]
- 59.Hui SL, Slemenda CW, Johnston C. Age and bone mass as predictors of fracture in a prospective study. J Clin Invest. 1998;81:1804–1809. doi: 10.1172/JCI113523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kanis JA, Johansson H, Oden A, et al. A family history of fracture and fracture risk: a meta-analysis. Bone. 2004;35:1029–1037. doi: 10.1016/j.bone.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 61.Kanis JA, Johansson H, Oden A, et al. A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res. 2004;19:893–899. doi: 10.1359/JBMR.040134. [DOI] [PubMed] [Google Scholar]
- 62.Kanis JA, Johansson H, Johnell O, Oden A, De Laet C, Eisman JA, Pols H, Tenenhouse A. Alcohol intake as a risk factor for fracture. Osteoporos Int. 2005;16:737–742. doi: 10.1007/s00198-004-1734-y. [DOI] [PubMed] [Google Scholar]
- 63.Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman J. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2006;16:155–162. doi: 10.1007/s00198-004-1640-3. [DOI] [PubMed] [Google Scholar]
- 64.De Laet C, Kanis JA, Oden A, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 65.Klotzbuecher CM, Ross PD, Landsman PD, Abbott TA, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 66.Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD. FRAX® with and without bone mineral density. Calcif Tissue Int. 2012;90:1–13. doi: 10.1007/s00223-011-9544-7. [DOI] [PubMed] [Google Scholar]
- 67.Schwartz AV, Vittinghoff E, Bauer DC, et al. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA. 2011;305:2184–2192. doi: 10.1001/jama.2011.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Giangregorio LM, Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA. FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res. 2012;27:301–308. doi: 10.1002/jbmr.556. [DOI] [PubMed] [Google Scholar]
- 69.Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV. Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int. 2008;19:1431–1444. doi: 10.1007/s00198-008-0588-0. [DOI] [PubMed] [Google Scholar]
- 70.Hippisley-Cox J, Coupland C. Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ. 2009;339:b4229. doi: 10.1136/bmj.b4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McClung MR, Geusens P, Miller PD, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344:333–340. doi: 10.1056/NEJM200102013440503. [DOI] [PubMed] [Google Scholar]
- 72.Delmas PD, Eastell R, Garnero P, Seibel MJ, Stepan J. The use of biochemical markers of bone turnover in osteoporosis. Committee of Scientific Advisors of the International Osteoporosis Foundation. Osteoporos Int. 2000;11(Suppl 6):S2–S17. doi: 10.1007/s001980070002. [DOI] [PubMed] [Google Scholar]
- 73.Johnell O, Oden A, De Laet C, Garnero P, Delmas PD, Kanis JA. Biochemical indices of bone turnover and the assessment of fracture probability. Osteoporos Int. 2002;13:523–526. doi: 10.1007/s001980200068. [DOI] [PubMed] [Google Scholar]
- 74.Vasikaran S, Eastell R, Bruyere O, et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int. 2011;22:391–420. doi: 10.1007/s00198-010-1501-1. [DOI] [PubMed] [Google Scholar]
- 75.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.WHO (2007) Assessment of osteoporosis at the primary health care level. WHO, Geneva. At: www.who.int/chp/topics/rheumatic/en/index.html. Accessed May 2012
- 77.Kanis JA, Oden A, Johnell O, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–1046. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 78.Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK. International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res. 2002;17:1237–1244. doi: 10.1359/jbmr.2002.17.7.1237. [DOI] [PubMed] [Google Scholar]
- 79.Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395–2411. doi: 10.1007/s00198-011-1713-z. [DOI] [PubMed] [Google Scholar]
- 80.Hans DB, Kanis JA, Baim S, et al. Joint official positions of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(®). Executive summary of the 2010 Position Development Conference on Interpretation and use of FRAX® in clinical practice. J Clin Densitom. 2011;14:171–180. doi: 10.1016/j.jocd.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 81.Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2000;15:993–1000. doi: 10.1359/jbmr.2000.15.6.993. [DOI] [PubMed] [Google Scholar]
- 82.Kanis JA, Johnell O, Oden A, et al. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2005;16:155–162. doi: 10.1007/s00198-004-1640-3. [DOI] [PubMed] [Google Scholar]
- 83.Kanis JA, Johansson H, Oden A, McCloskey EV. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int. 2011;22:809–816. doi: 10.1007/s00198-010-1524-7. [DOI] [PubMed] [Google Scholar]
- 84.Papaioannou A, Morin S, Cheung AM, et al. Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–1873. doi: 10.1503/cmaj.100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Orimo H, Nakamura T, Fukunaga M (2006) Japanese guidelines for the prevention and treatment of osteoporosis (Translated Abridged Edition)
- 86.Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, Silverman S. Official positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom. 2008;11:75–91. doi: 10.1016/j.jocd.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 87.Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA. Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int. 2011;22:839–847. doi: 10.1007/s00198-010-1461-5. [DOI] [PubMed] [Google Scholar]
- 88.Leslie WD, Kovacs CS, Olszynski WP, Towheed T, Kaiser SM, Prior JC, Josse RG, Jamal SA, Kreiger N, Goltzman D. Spine-hip T-score difference predicts major osteoporotic fracture risk independent of FRAX®: a population-based report from CAMOS. J Clin Densitom. 2011;14:286–293. doi: 10.1016/j.jocd.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A. Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int. 2008;19:1395–1408. doi: 10.1007/s00198-008-0712-1. [DOI] [PubMed] [Google Scholar]
- 90.Kanis JA, Reginster JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women—what is the current message for clinical practice? Pol Arch Med Wewn. 2008;118:538–540. [PubMed] [Google Scholar]
- 91.Physician's guide to prevention and treatment of osteoporosis. Washington DC: NOF; 2003. [Google Scholar]
- 92.Report on osteoporosis in the European Community. Strasbourg: EC; 1998. [Google Scholar]
- 93.Brixen K (2002) Consensus report on osteoporosis. Ugeskr Laeger Suppl. 10
- 94.Hellenic Foundation for Osteoporosis (2004) Kateufunthries gpammes gia th diagnwsh kai antimetwpisnh ths Osteopowshs sthn Ellada (Guidelines for diagnosis and management of osteoporosis in Greece). Athens
- 95.Collegio dei Reumatologi Ospedalieri, Società Italiana dell'Osteoporosi e delle Malattie del Metabolismo Minerale e Scheletrico, Società Italiana di Medicina Fisica e Riabilitativa, Società Italiana di Medicina Interna, Società Italiana di Ortopedia e Traumatologia, Società Italiana di Radiologia Medica, Società Italiana di Reumatologia (2006) Linee guida per la diagnosi, prevenzione e terapia dell'osteoporosi (Guidelines for the diagnosis, prevention and treatment of osteoporosis). SINOSSI. EDIMES., Pavia
- 96.Pols HA, Wittenberg J. CBO guideline 'Osteoporosis' (second revision] Ned Tijdschr Geneeskd. 2002;146:1359–1363. [PubMed] [Google Scholar]
- 97.SEIOMM (2003) Guía de Práctica: osteoporosis posmenopáusica (Practice guidelines: postmenopausal osteoporosis). Revista Clinica Española. pp 496–506 [PubMed]
- 98.Management of osteoporosis. Edinburgh: SIGN; 2003. [Google Scholar]
- 99.Dawson-Hughes B. A revised clinician's guide to the prevention and treatment of osteoporosis. J Clin Endocrinol Metab. 2008;93:2463–2465. doi: 10.1210/jc.2008-0926. [DOI] [PubMed] [Google Scholar]
- 100.Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int. 2005;16:229–238. doi: 10.1007/s00198-004-1811-2. [DOI] [PubMed] [Google Scholar]
- 101.Association Suisse contre l‘Ostéoporose (2010) Ostéoporose: Recommandations 2010. ASCO. http://www.svgo.ch/content/documents/SVGO_Empfehlungen2010_V19April2010.pdf. Accessed May 2012
- 102.Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M. Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas. 2009;62:105–108. doi: 10.1016/j.maturitas.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 103.Czerwinski E, Kanis JA, Trybulec B, Johansson H, Borowy P, Osieleniec J. The incidence and risk of hip fracture in Poland. Osteoporos Int. 2009;20:1363–1367. doi: 10.1007/s00198-008-0787-8. [DOI] [PubMed] [Google Scholar]
- 104.Badurski JE, Kanis JA, Johansson H, Dobrenko A, Nowak NA, Daniluk S, Jezienicka E. The application of FRAX® to determine intervention thresholds in osteoporosis treatment in Poland. Pol Arch Med Wewn. 2011;121:148–155. [PubMed] [Google Scholar]
- 105.Dawson-Hughes B, Tosteson AN, Melton LJ, 3rd, Baim S, Favus MJ, Khosla S, Lindsay RL. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–458. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 106.Fujiwara S, Nakamura T, Orimo H, Hosoi T, Gorai I, Oden A, Johansson H, Kanis JA. Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX) Osteoporos Int. 2008;19:429–435. doi: 10.1007/s00198-007-0544-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Grossman JM, Gordon R, Ranganath VK, American College of Rheumatology et al. Recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2010;62:1515–1526. doi: 10.1002/acr.20295. [DOI] [PubMed] [Google Scholar]
- 108.Kanis JA, Johnell O, Oden A, De Laet C, Oglesby A, Jonsson B. Intervention thresholds for osteoporosis. Bone. 2002;31:26–31. doi: 10.1016/S8756-3282(02)00813-X. [DOI] [PubMed] [Google Scholar]
- 109.Kanis JA, Johnell O, Oden A, Borgstrom F, Johansson H, De Laet C, Jonsson B. Intervention thresholds for osteoporosis in men and women: a study based on data from Sweden. Osteoporos Int. 2005;16:6–14. doi: 10.1007/s00198-004-1623-4. [DOI] [PubMed] [Google Scholar]
- 110.Kanis JA, Borgstrom F, Zethraeus N, Johnell O, Oden A, Jonsson B. Intervention thresholds for osteoporosis in the UK. Bone. 2005;36:22–32. doi: 10.1016/j.bone.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 111.Lekawasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgstrom F (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int (in press) [DOI] [PubMed]
- 112.Lippuner K, Johansson H, Kanis JA, Rizzoli R. FRAX assessment of osteoporotic fracture probability in Switzerland. Osteoporos Int. 2010;21:381–389. doi: 10.1007/s00198-009-0975-1. [DOI] [PubMed] [Google Scholar]
- 113.Clinician's guide to prevention and treatment of osteoporosis. Washington DC: NOF; 2008. [Google Scholar]
- 114.Neuprez A, Johansson H, Kanis JA, McCloskey EV, Oden A, Bruyere O, Hiligsmann M, Devogelaer JP, Kaufman JM, Reginster JY. A FRAX model for the assessment of fracture probability in Belgium. Rev Med Liege. 2009;64:612–619. [PubMed] [Google Scholar]
- 115.Socialstyrelsen (2010) Nationella riktlinjer för rörelseorganens sjukdomar 2010 - stöd för styrning och ledning. Preliminär version. Artikelnr 2010-11-15. Publicerad www.socialstyrelsen.se. Accessed June 2012
- 116.Briot K, Cortet B, Thomas T, et al. 2012 update of French guidelines for the pharmacological treatment of postmenopausal osteoporosis. Joint Bone Spine. 2012;79:304–313. doi: 10.1016/j.jbspin.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 117.Tosteson AN, Melton LJ, 3rd, Dawson-Hughes B, Baim S, Favus MJ, Khosla S, Lindsay RL. Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int. 2008;19:437–447. doi: 10.1007/s00198-007-0550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M. Glucocorticoid-induced osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess. 2007;11:1–256. doi: 10.3310/hta11070. [DOI] [PubMed] [Google Scholar]
- 119.Johansson H, Oden A, Johnell O, Jonsson B, de Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA. Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res. 2004;19:906–913. doi: 10.1359/jbmr.2004.19.6.906. [DOI] [PubMed] [Google Scholar]
- 120.Johansson H, Kanis JA, Oden A, Johnell O, McCloskey E. BMD, clinical risk factors and their combination for hip fracture prevention. Osteoporos Int. 2009;20:1675–1682. doi: 10.1007/s00198-009-0845-x. [DOI] [PubMed] [Google Scholar]
- 121.Johansson H, Kanis JA, Oden A, Compston J, McCloskey E. A comparison of case-finding strategies in the UK for the management of hip fractures. Osteoporos Int. 2012;23:907–915. doi: 10.1007/s00198-011-1864-y. [DOI] [PubMed] [Google Scholar]
- 122.Kanis JA, Adams J, Borgstrom F, Cooper C, Jonsson B, Preedy D, Selby P, Compston J. The cost-effectiveness of alendronate in the management of osteoporosis. Bone. 2008;42:4–15. doi: 10.1016/j.bone.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 123.Leslie WD, Morin S, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA. Fracture risk assessment without bone density measurement in routine clinical practice. Osteoporos Int. 2012;23:75–85. doi: 10.1007/s00198-011-1747-2. [DOI] [PubMed] [Google Scholar]
- 124.Leslie WD, Majumdar SR, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA. High fracture probability with FRAX usually indicates densitometric osteoporosis: implications for clinical practice. Osteoporos Int. 2012;23:391–397. doi: 10.1007/s00198-011-1592-3. [DOI] [PubMed] [Google Scholar]
- 125.Dachverband Osteologie e.V DVO guideline 2009 for prevention, diagnosis and therapy of osteoporosis in adults. Osteologie. 2011;20:55–74. [Google Scholar]
- 126.Collins GS, Mallett S, Altman DG. Predicting risk of osteoporotic and hip fracture in the United Kingdom: prospective independent and external validation of QFractureScores. BMJ. 2011;342:d3651. doi: 10.1136/bmj.d3651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kanis JA, Oden A, Johansson H, McCloskey E. Pitfalls in the external validation of FRAX. Osteoporos Int. 2012;23:423–431. doi: 10.1007/s00198-011-1846-0. [DOI] [PubMed] [Google Scholar]
- 128.Bonaiuti D, Shea B, Iovine R, Negrini S, Robinson V, Kemper HC, Wells G, Tugwell P, Cranney A (2002) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev CD000333 [DOI] [PubMed]
- 129.Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;11:CD004963. doi: 10.1002/14651858.CD004963.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev CD000333 [DOI] [PMC free article] [PubMed]
- 131.Myers AH, Young Y, Langlois JA. Prevention of falls in the elderly. Bone. 1996;18:87S–101S. doi: 10.1016/8756-3282(95)00384-3. [DOI] [PubMed] [Google Scholar]
- 132.Michael YL, Whitlock EP, Lin JS, Fu R, O'Connor EA, Gold R. Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2010;153:815–825. doi: 10.7326/0003-4819-153-12-201012210-00008. [DOI] [PubMed] [Google Scholar]
- 133.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 134.Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366:1885–1893. doi: 10.1016/S0140-6736(05)67604-0. [DOI] [PubMed] [Google Scholar]
- 135.Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, Vanoli A, Martin FC, Gosney MA. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334:82. doi: 10.1136/bmj.39049.706493.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gillespie WJ, Gillespie LD, Parker MJ (2010) Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev CD001255 [DOI] [PubMed]
- 137.Sawka AM, Boulos P, Beattie K, Thabane L, Papaioannou A, Gafni A, Cranney A, Zytaruk N, Hanley DA, Adachi JD. Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2005;16:1461–1474. doi: 10.1007/s00198-005-1932-2. [DOI] [PubMed] [Google Scholar]
- 138.Parker MJ, Gillespie WJ, Gillespie LD. Effectiveness of hip protectors for preventing hip fractures in elderly people: systematic review. BMJ. 2006;332:571–574. doi: 10.1136/bmj.38753.375324.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kiel DP, Magaziner J, Zimmerman S, Ball L, Barton BA, Brown KM, Stone JP, Dewkett D, Birge SJ. Efficacy of a hip protector to prevent hip fracture in nursing home residents: the HIP PRO randomized controlled trial. JAMA. 2007;298:413–422. doi: 10.1001/jama.298.4.413. [DOI] [PubMed] [Google Scholar]
- 140.Rizzoli R. Nutrition: its role in bone health. Best Pract Res Clin Endocrinol Metab. 2008;22:813–829. doi: 10.1016/j.beem.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 141.Bonjour JP, Guéguen L, Palacios C, Shearer MJ, Weaver CM. Minerals and vitamins in bone health: the potential value of dietary enhancement. Br J Nutr. 2009;101:1581–1596. doi: 10.1017/S0007114509311721. [DOI] [PubMed] [Google Scholar]
- 142.Food and Agricultural Organization of the United Nations/World Health Organization (2001) Human vitamin and mineral requirements. Report of a joint FAO/WHO expert consultation. Bangkok, Thailand. Washington, DC
- 143.Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet. 2007;370:657–666. doi: 10.1016/S0140-6736(07)61342-7. [DOI] [PubMed] [Google Scholar]
- 144.Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692. doi: 10.1136/bmj.b3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Smith H, Anderson F, Raphael H, Maslin P, Crozier S, Cooper C. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women—a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology (Oxford) 2007;46:1852–1857. doi: 10.1093/rheumatology/kem240. [DOI] [PubMed] [Google Scholar]
- 146.Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–1822. doi: 10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 147.Wang L, Manson JE, Song Y, Sesso HD. Systematic review: vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152:315–323. doi: 10.7326/0003-4819-152-5-201003020-00010. [DOI] [PubMed] [Google Scholar]
- 148.Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167:1730–1737. doi: 10.1001/archinte.167.16.1730. [DOI] [PubMed] [Google Scholar]
- 149.Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women's Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040. doi: 10.1136/bmj.d2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bolland MJ, Grey A, Reid IR. Misclassification does not explain increased cardiovascular risks of calcium supplements. J Bone Miner Res. 2012;27:959. doi: 10.1002/jbmr.1568. [DOI] [PubMed] [Google Scholar]
- 151.Grey A, Bolland M, Reid R. Calcium supplements and cardiovascular disease—picking the spin. Int J Clin Pract. 2011;65:226–227. doi: 10.1111/j.1742-1241.2010.02557.x. [DOI] [PubMed] [Google Scholar]
- 152.Bolland MJ, Grey A, Reid IR. Re: the calcium scare: what would Austin Bradford Hill have thought? Osteoporos Int. 2011;22:3079–3080. doi: 10.1007/s00198-011-1783-y. [DOI] [PubMed] [Google Scholar]
- 153.Lewis JR, Zhu K, Prince RL. Response to: misclassification does not explain increased cardiovascular risks of calcium supplements. J Bone Miner Res. 2012;27:960–961. doi: 10.1002/jbmr.1569. [DOI] [PubMed] [Google Scholar]
- 154.Lewis JR, Zhu K, Prince RL. Adverse events from calcium supplementation: relationship to errors in myocardial infarction self-reporting in randomized controlled trials of calcium supplementation. J Bone Miner Res. 2012;27:719–722. doi: 10.1002/jbmr.1484. [DOI] [PubMed] [Google Scholar]
- 155.Nordin BE, Lewis JR, Daly RM, Horowitz J, Metcalfe A, Lange K, Prince RL. The calcium scare—what would Austin Bradford Hill have thought? Osteoporos Int. 2011;22:3073–3077. doi: 10.1007/s00198-011-1680-4. [DOI] [PubMed] [Google Scholar]
- 156.Lewis JR, Calver J, Zhu K, Flicker L, Prince RL. Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.5-year follow-up. J Bone Miner Res. 2011;26:35–41. doi: 10.1002/jbmr.176. [DOI] [PubMed] [Google Scholar]
- 157.Rizzoli R, Burlet N, Cahall D, et al. Osteonecrosis of the jaw and bisphosphonate treatment for osteoporosis. Bone. 2008;42:841–847. doi: 10.1016/j.bone.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 158.Delmas PD. Treatment of postmenopausal osteoporosis. Lancet. 2002;359:2018–2026. doi: 10.1016/S0140-6736(02)08827-X. [DOI] [PubMed] [Google Scholar]
- 159.Boonen S, Body JJ, Boutsen Y, Devogelaer JP, Goemaere S, Kaufman JM, Rozenberg S, Reginster JY. Evidence-based guidelines for the treatment of postmenopausal osteoporosis: a consensus document of the Belgian Bone Club. Osteoporos Int. 2005;16:239–254. doi: 10.1007/s00198-004-1812-1. [DOI] [PubMed] [Google Scholar]
- 160.Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone. 2003;33:522–532. doi: 10.1016/S8756-3282(03)00241-2. [DOI] [PubMed] [Google Scholar]
- 161.Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. Jama. 1999;282:637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 162.Cummings SR, Eckert S, Krueger KA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. Jama. 1999;281:2189–2197. doi: 10.1001/jama.281.23.2189. [DOI] [PubMed] [Google Scholar]
- 163.Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. Jama. 2006;295:2727–2741. doi: 10.1001/jama.295.23.joc60074. [DOI] [PubMed] [Google Scholar]
- 164.Mosca L, Barrett-Connor E, Wenger NK, et al. Design and methods of the Raloxifene Use for The Heart (RUTH) study. AmJ Cardiol. 2001;88:392–395. doi: 10.1016/S0002-9149(01)01685-X. [DOI] [PubMed] [Google Scholar]
- 165.Barrett-Connor E, Mosca L, Collins P, Geiger MJ, Grady D, Kornitzer M, McNabb MA, Wenger NK. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125–137. doi: 10.1056/NEJMoa062462. [DOI] [PubMed] [Google Scholar]
- 166.Kanis JA, Johnell O, Black DM, Downs RW, Jr, Sarkar S, Fuerst T, Secrest RJ, Pavo I. Effect of raloxifene on the risk of new vertebral fracture in postmenopausal women with osteopenia or osteoporosis: a reanalysis of the Multiple Outcomes of Raloxifene Evaluation trial. Bone. 2003;33:293–300. doi: 10.1016/S8756-3282(03)00200-X. [DOI] [PubMed] [Google Scholar]
- 167.Kanis JA, Johansson H, Oden A, McCloskey EV. A meta-analysis of the efficacy of raloxifene on all clinical and vertebral fractures and its dependency on FRAX. Bone. 2010;47:729–735. doi: 10.1016/j.bone.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 168.Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, Constantine GD, Chines AA. Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res. 2008;23:1923–1934. doi: 10.1359/jbmr.080710. [DOI] [PubMed] [Google Scholar]
- 169.Silverman SL, Chines AA, Kendler DL, Kung AW, Teglbjaerg CS, Felsenberg D, Mairon N, Constantine GD, Adachi JD. Sustained efficacy and safety of bazedoxifene in preventing fractures in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled study. Osteoporos Int. 2012;23:351–363. doi: 10.1007/s00198-011-1691-1. [DOI] [PubMed] [Google Scholar]
- 170.Kanis JA, Johansson H, Oden A, McCloskey EV. Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX. Bone. 2009;44:1049–1054. doi: 10.1016/j.bone.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 171.de Villiers TJ, Chines AA, Palacios S, Lips P, Sawicki AZ, Levine AB, Codreanu C, Kelepouris N, Brown JP. Safety and tolerability of bazedoxifene in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled phase 3 trial. Osteoporos Int. 2011;22:567–576. doi: 10.1007/s00198-010-1302-6. [DOI] [PubMed] [Google Scholar]
- 172.Khan SA, Kanis JA, Vasikaran S, et al. Elimination and biochemical responses to intravenous alendronate in postmenopausal osteoporosis. J Bone Miner Res. 1997;12:1700–1707. doi: 10.1359/jbmr.1997.12.10.1700. [DOI] [PubMed] [Google Scholar]
- 173.Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/S0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 174.Stevenson M, Jones ML, De Nigris E, Brewer N, Davis S, Oakley J. A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Assess. 2005;9:1–160. doi: 10.3310/hta9220. [DOI] [PubMed] [Google Scholar]
- 175.Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C. Meta-analyses of therapies for postmenopausal osteoporosis. IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002;23:570–578. doi: 10.1210/er.2001-9002. [DOI] [PubMed] [Google Scholar]
- 176.Cummings SR, Black DM, Thompson DE, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. Jama. 1998;280:2077–2082. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 177.Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 178.Reginster J, Minne HW, Sorensen OH, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int. 2000;11:83–91. doi: 10.1007/s001980050010. [DOI] [PubMed] [Google Scholar]
- 179.Chesnut IC, Skag A, Christiansen C, et al. Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004;19:1241–1249. doi: 10.1359/JBMR.040325. [DOI] [PubMed] [Google Scholar]
- 180.Delmas PD, Recker RR, Chesnut CH, 3rd, Skag A, Stakkestad JA, Emkey R, Gilbride J, Schimmer RC, Christiansen C. Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int. 2004;15:792–798. doi: 10.1007/s00198-004-1602-9. [DOI] [PubMed] [Google Scholar]
- 181.Harris ST, Blumentals WA, Miller PD. Ibandronate and the risk of non-vertebral and clinical fractures in women with postmenopausal osteoporosis: results of a meta-analysis of phase III studies. Curr Med Res Opin. 2008;24:237–245. doi: 10.1185/030079908X253717. [DOI] [PubMed] [Google Scholar]
- 182.Reginster JY, Adami S, Lakatos P, et al. Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis. 2006;65:654–661. doi: 10.1136/ard.2005.044958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Delmas PD, Adami S, Strugala C, et al. Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum. 2006;54:1838–1846. doi: 10.1002/art.21918. [DOI] [PubMed] [Google Scholar]
- 184.Reid IR, Brown JP, Burckhardt P, et al. Intravenous zoledronic acid in postmenopausal women with low bone mineral density. N Engl J Med. 2002;346:653–661. doi: 10.1056/NEJMoa011807. [DOI] [PubMed] [Google Scholar]
- 185.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 186.Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. New Engl J Med. 2007;357:1–11. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rizzoli R, Reginster JY, Boonen S, Breart G, Diez-Perez A, Felsenberg D, Kaufman JM, Kanis JA, Cooper C. Adverse reactions and drug-drug interactions in the management of women with postmenopausal osteoporosis. Calcif Tissue Int. 2011;89:91–104. doi: 10.1007/s00223-011-9499-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Pazianas M, Compston J, Huang CL. Atrial fibrillation and bisphosphonate therapy. J Bone Miner Res. 2010;25:2–10. doi: 10.1359/jbmr.091201. [DOI] [PubMed] [Google Scholar]
- 189.Cardwell CR, Abnet CC, Cantwell MM, Murray LJ. Exposure to oral bisphosphonates and risk of esophageal cancer. JAMA. 2010;304:657–663. doi: 10.1001/jama.2010.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Green J, Czanner G, Reeves G, Watson J, Wise L, Beral V. Oral bisphosphonates and risk of cancer of oesophagus, stomach, and colorectum: case-control analysis within a UK primary care cohort. BMJ. 2010;341:c4444. doi: 10.1136/bmj.c4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25:2267–2294. doi: 10.1002/jbmr.253. [DOI] [PubMed] [Google Scholar]
- 192.Pazianas M, Abrahamsen B, Eiken PA, Eastell R, Russell RG (2012) Reduced colon cancer incidence and mortality in postmenopausal women treated with an oral bisphosphonate—Danish National Register Based Cohort Study. Osteoporos Int (in press) [DOI] [PubMed]
- 193.Hartle JE, Tang X, Kirchner HL, Bucaloiu ID, Sartorius JA, Pogrebnaya ZV, Akers GA, Carnero GE, Perkins RM. Bisphosphonate therapy, death, and cardiovascular events among female patients with CKD: a retrospective cohort study. Am J Kidney Dis. 2012;59:636–644. doi: 10.1053/j.ajkd.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 194.Bondo L, Eiken P, Abrahamsen B (2012) Analysis of the association between bisphosphonate treatment survival in Danish hip fracture patients-a nationwide register-based open cohort study. Osteoporos Int (in press) [DOI] [PubMed]
- 195.Chlebowski RT, Chen Z, Cauley JA, et al. Oral bisphosphonate use and breast cancer incidence in postmenopausal women. J Clin Oncol. 2010;28:3582–3590. doi: 10.1200/JCO.2010.28.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Rizzoli R, Akesson K, Bouxsein M, Kanis JA, Napoli N, Papapoulos S, Reginster JY, Cooper C. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporos Int. 2011;22:373–390. doi: 10.1007/s00198-010-1453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kanis JA, Reginster JY, Kaufman JM, Ringe JD, Adachi JD, Hiligsmann M, Rizzoli R, Cooper C. A reappraisal of generic bisphosphonates in osteoporosis. Osteoporos Int. 2012;23:213–221. doi: 10.1007/s00198-011-1796-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 199.Shrader SP, Ragucci KR. Parathyroid hormone (1-84) and treatment of osteoporosis. Ann Pharmacother. 2005;39:1511–1516. doi: 10.1345/aph.1G146. [DOI] [PubMed] [Google Scholar]
- 200.Prince R, Sipos A, Hossain A, Syversen U, Ish-Shalom S, Marcinowska E, Halse J, Lindsay R, Dalsky GP, Mitlak BH. Sustained nonvertebral fragility fracture risk reduction after discontinuation of teriparatide treatment. J Bone Miner Res. 2005;20:1507–1513. doi: 10.1359/JBMR.050501. [DOI] [PubMed] [Google Scholar]
- 201.Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–468. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 202.Reginster JY, Seeman E, De Vernejoul MC, et al. Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab. 2005;90:2816–2822. doi: 10.1210/jc.2004-1774. [DOI] [PubMed] [Google Scholar]
- 203.Kanis JA, Johansson H, Oden A, McCloskey EV. A meta-analysis of the effect of strontium ranelate on the risk of vertebral and non-vertebral fracture in postmenopausal osteoporosis and the interaction with FRAX®. Osteoporos Int. 2011;22:2347–2355. doi: 10.1007/s00198-010-1474-0. [DOI] [PubMed] [Google Scholar]
- 204.Reginster JY, Kaufman JM, Goemaere S, et al. Maintenance of antifracture efficacy over 10 years with strontium ranelate in postmenopausal osteoporosis. Osteoporos Int. 2012;23:1115–1122. doi: 10.1007/s00198-011-1847-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Stevenson M, Davis S, Lloyd-Jones M, Beverley C. The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women. Health Technol Assess. 2007;11:1–134. doi: 10.3310/hta11040. [DOI] [PubMed] [Google Scholar]
- 206.EMEA (2007) Questions and answers on the safety of Protelos/Osseor (strontium ranelate). European Medicines Agency. Accessed 24th January 2012
- 207.Musette P, Brandi ML, Cacoub P, Kaufman JM, Rizzoli R, Reginster JY. Treatment of osteoporosis: recognizing and managing cutaneous adverse reactions and drug-induced hypersensitivity. Osteoporos Int. 2010;21:723–732. doi: 10.1007/s00198-009-1097-5. [DOI] [PubMed] [Google Scholar]
- 208.Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003;206:353–356. doi: 10.1159/000069956. [DOI] [PubMed] [Google Scholar]
- 209.Lecart MP, Reginster JY. Current options for the management of postmenopausal osteoporosis. Expert Opin Pharmacother. 2011;12:2533–2552. doi: 10.1517/14656566.2011.618123. [DOI] [PubMed] [Google Scholar]
- 210.Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 211.Papapoulos S, Chapurlat R, Libanati C, et al. Five years of denosumab exposure in women with postmenopausal osteoporosis: results from the first two years of the FREEDOM extension. J Bone Miner Res. 2012;27:694–701. doi: 10.1002/jbmr.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.McCloskey EV, Johansson H, Oden A, Austin M, Siris E, Wang A, Lewiecki EM, Lorenc R, Libanati C, Kanis JA (2012) Denosumab reduces the risk of osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX(R). J Bone Miner Res Published online on Mar 19, 2012. doi:10.1002/jbmr.1606 [DOI] [PubMed]
- 213.von Keyserlingk C, Hopkins R, Anastasilakis A, Toulis K, Goeree R, Tarride JE, Xie F. Clinical efficacy and safety of denosumab in postmenopausal women with low bone mineral density and osteoporosis: a meta-analysis. Semin Arthritis Rheum. 2011;41:178–186. doi: 10.1016/j.semarthrit.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 214.Black DM, Bilezikian JP, Ensrud KE, Greenspan SL, Palermo L, Hue T, Lang TF, McGowan JA, Rosen CJ. One year of alendronate after one year of parathyroid hormone (1-84) for osteoporosis. N Engl J Med. 2005;353:555–565. doi: 10.1056/NEJMoa050336. [DOI] [PubMed] [Google Scholar]
- 215.Eastell R, Nickelsen T, Marin F, et al. Sequential treatment of severe postmenopausal osteoporosis after teriparatide: final results of the randomized, controlled European Study of Forsteo (EUROFORS) J Bone Miner Res. 2009;24:726–736. doi: 10.1359/jbmr.081215. [DOI] [PubMed] [Google Scholar]
- 216.McClung M, Recker R, Miller P, Fiske D, Minkoff J, Kriegman A, Zhou W, Adera M, Davis J. Intravenous zoledronic acid 5 mg in the treatment of postmenopausal women with low bone density previously treated with alendronate. Bone. 2007;41:122–128. doi: 10.1016/j.bone.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 217.Boonen S, Marin F, Obermayer-Pietsch B, et al. Effects of prior antiresorptive therapy on the bone mineral density response to two years of teriparatide treatment in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2008;93:852–860. doi: 10.1210/jc.2007-0711. [DOI] [PubMed] [Google Scholar]
- 218.Black DM, Greenspan SL, Ensrud KE, Palermo L, McGowan JA, Lang TF, Garnero P, Bouxsein ML, Bilezikian JP, Rosen CJ. The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N Engl J Med. 2003;349:1207–1215. doi: 10.1056/NEJMoa031975. [DOI] [PubMed] [Google Scholar]
- 219.Miller PD, Delmas PD, Lindsay R, et al. Early responsiveness of women with osteoporosis to teriparatide after therapy with alendronate or risedronate. J Clin Endocrinol Metab. 2008;93:3785–3793. doi: 10.1210/jc.2008-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kendler DL, Roux C, Benhamou CL, Brown JP, Lillestol M, Siddhanti S, Man HS, San Martin J, Bone HG. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res. 2010;25:72–81. doi: 10.1359/jbmr.090716. [DOI] [PubMed] [Google Scholar]
- 221.Middleton ET, Steel SA, Aye M, Doherty SM. The effect of prior bisphosphonate therapy on the subsequent therapeutic effects of strontium ranelate over 2 years. Osteoporos Int. 2012;23:295–303. doi: 10.1007/s00198-011-1547-8. [DOI] [PubMed] [Google Scholar]
- 222.Middleton ET, Steel SA, Aye M, Doherty SM. The effect of prior bisphosphonate therapy on the subsequent BMD and bone turnover response to strontium ranelate. J Bone Miner Res. 2010;25:455–462. doi: 10.1359/jbmr.090821. [DOI] [PubMed] [Google Scholar]
- 223.Reginster JY. Effect of calcitonin on bone mass and fracture rates. Am J Med. 1991;91:19S–22S. doi: 10.1016/0002-9343(91)90242-P. [DOI] [PubMed] [Google Scholar]
- 224.Plosker GL, McTavish D. Intranasal salcatonin (salmon calcitonin). A review of its pharmacological properties and role in the management of postmenopausal osteoporosis. Drugs Aging. 1996;8:378–400. doi: 10.2165/00002512-199608050-00006. [DOI] [PubMed] [Google Scholar]
- 225.Cranney A, Tugwell P, Zytaruk N, Robinson V, Weaver B, Shea B, Wells G, Adachi J, Waldegger L, Guyatt G. Meta-analyses of therapies for postmenopausal osteoporosis. VI. Meta-analysis of calcitonin for the treatment of postmenopausal osteoporosis. Endocr Rev. 2002;23:540–551. doi: 10.1210/er.2001-6002. [DOI] [PubMed] [Google Scholar]
- 226.Chesnut CH, 3rd, Silverman S, Andriano K, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. PROOF Study Group. Am J Med. 2000;109:267–276. doi: 10.1016/S0002-9343(00)00490-3. [DOI] [PubMed] [Google Scholar]
- 227.Kanis JA, Johnell O, Gullberg B, et al. Evidence for efficacy of drugs affecting bone metabolism in preventing hip fracture. BMJ. 1992;305:1124–1128. doi: 10.1136/bmj.305.6862.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Torgerson DJ, Bell-Syer SE. Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials. JAMA. 2001;285:2891–2897. doi: 10.1001/jama.285.22.2891. [DOI] [PubMed] [Google Scholar]
- 229.Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women's Health Initiative randomized trial. Jama. 2003;290:1729–1738. doi: 10.1001/jama.290.13.1729. [DOI] [PubMed] [Google Scholar]
- 230.Sornay-Rendu E, Garnero P, Munoz F, Duboeuf F, Delmas PD. Effect of withdrawal of hormone replacement therapy on bone mass and bone turnover: the OFELY study. Bone. 2003;33:159–166. doi: 10.1016/S8756-3282(03)00171-6. [DOI] [PubMed] [Google Scholar]
- 231.Bagger YZ, Tanko LB, Alexandersen P, Hansen HB, Mollgaard A, Ravn P, Qvist P, Kanis JA, Christiansen C. Two to three years of hormone replacement treatment in healthy women have long-term preventive effects on bone mass and osteoporotic fractures: the PERF study. Bone. 2004;34:728–735. doi: 10.1016/j.bone.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 232.Roussow JE, Anderson GL, Prentice RL, LaCroix A, Kooperberg C, Stefanick ML. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 233.Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women's Health Initiative: a randomized trial. Jama. 2003;289:2673–2684. doi: 10.1001/jama.289.20.2673. [DOI] [PubMed] [Google Scholar]
- 234.Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women's Health Initiative Randomized Trial. JAMA. 2003;289:3243–3253. doi: 10.1001/jama.289.24.3243. [DOI] [PubMed] [Google Scholar]
- 235.Shumaker SA, Legault C, Rapp SR, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003;289:2651–2662. doi: 10.1001/jama.289.20.2651. [DOI] [PubMed] [Google Scholar]
- 236.Hays J, Ockene JK, Brunner RL, et al. Effects of estrogen plus progestin on health-related quality of life. N Engl J Med. 2003;348:1839–1854. doi: 10.1056/NEJMoa030311. [DOI] [PubMed] [Google Scholar]
- 237.Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 238.Fenton A, Panay N. The Women's Health Initiative—a decade of progress. Climacteric. 2012;15:205. doi: 10.3109/13697137.2012.680255. [DOI] [PubMed] [Google Scholar]
- 239.Langer RD, Manson JE, Allison MA. Have we come full circle—or moved forward? The Women's Health Initiative 10 years on. Climacteric. 2012;15:206–212. doi: 10.3109/13697137.2012.666916. [DOI] [PubMed] [Google Scholar]
- 240.Watts NB, Harris ST, Genant HK, et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med. 1990;323:73–79. doi: 10.1056/NEJM199007123230201. [DOI] [PubMed] [Google Scholar]
- 241.Richy F, Ethgen O, Bruyere O, Reginster JY. Efficacy of alphacalcidol and calcitriol in primary and corticosteroid-induced osteoporosis: a meta-analysis of their effects on bone mineral density and fracture rate. Osteoporos Int. 2004;15:301–310. doi: 10.1007/s00198-003-1570-5. [DOI] [PubMed] [Google Scholar]
- 242.Richy F, Schacht E, Bruyere O, Ethgen O, Gourlay M, Reginster JY. Vitamin D analogs versus native vitamin D in preventing bone loss and osteoporosis-related fractures: a comparative meta-analysis. Calcif Tissue Int. 2005;76:176–186. doi: 10.1007/s00223-004-0005-4. [DOI] [PubMed] [Google Scholar]
- 243.Tilyard MW, Spears GF, Thomson J, Dovey S. Treatment of postmenopausal osteoporosis with calcitriol or calcium. N Engl J Med. 1992;326:357–362. doi: 10.1056/NEJM199202063260601. [DOI] [PubMed] [Google Scholar]
- 244.Gallagher JC, Rapuri PB, Smith LM. An age-related decrease in creatinine clearance is associated with an increase in number of falls in untreated women but not in women receiving calcitriol treatment. J Clin Endocrinol Metab. 2007;92:51–58. doi: 10.1210/jc.2006-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.McCloskey E, Selby P, Davies M, et al. Clodronate reduces vertebral fracture risk in women with postmenopausal or secondary osteoporosis: results of a double-blind, placebo-controlled 3-year study. J Bone Miner Res. 2004;19:728–736. doi: 10.1359/jbmr.040116. [DOI] [PubMed] [Google Scholar]
- 246.McCloskey EV, Beneton M, Charlesworth D, et al. Clodronate reduces the incidence of fractures in community-dwelling elderly women unselected for osteoporosis: results of a double-blind, placebo-controlled randomized study. J Bone Miner Res. 2007;22:135–141. doi: 10.1359/jbmr.061008. [DOI] [PubMed] [Google Scholar]
- 247.Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, Tillman JB, Eastell R, Talmadge K, Wardlaw D. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res. 2011;26:1627–1637. doi: 10.1002/jbmr.364. [DOI] [PubMed] [Google Scholar]
- 248.Lekkerkerker F, Kanis JA, Alsayed N, et al. Adherence to treatment of osteoporosis: a need for study. Osteoporos Int. 2007;18:1311–1317. doi: 10.1007/s00198-007-0410-4. [DOI] [PubMed] [Google Scholar]
- 249.Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Brookhart MA. Compliance with osteoporosis medications. Arch Intern Med. 2005;165:2414–2419. doi: 10.1001/archinte.165.20.2414. [DOI] [PubMed] [Google Scholar]
- 250.Hiligsmann M, Gathon HJ, Bruyere O, Ethgen O, Rabenda V, Reginster JY. Cost-effectiveness of osteoporosis screening followed by treatment: the impact of medication adherence. Value Health. 2010;13:394–401. doi: 10.1111/j.1524-4733.2009.00687.x. [DOI] [PubMed] [Google Scholar]
- 251.Rabenda V, Mertens R, Fabri V, Vanoverloop J, Sumkay F, Vannecke C, Deswaef A, Verpooten GA, Reginster JY. Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int. 2008;19:811–818. doi: 10.1007/s00198-007-0506-x. [DOI] [PubMed] [Google Scholar]
- 252.Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E. A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health. 2011;14:571–581. doi: 10.1016/j.jval.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 253.Strom O, Borgstrom F, Kanis JA, Jonsson B. Incorporating adherence into health economic modelling of osteoporosis. Osteoporos Int. 2009;20:23–34. doi: 10.1007/s00198-008-0644-9. [DOI] [PubMed] [Google Scholar]
- 254.Kanis JA, Cooper C, Hiligsmann M, Rabenda V, Reginster JY, Rizzoli R. Partial adherence: a new perspective on health economic assessment in osteoporosis. Osteoporos Int. 2011;22:2565–2573. doi: 10.1007/s00198-011-1668-0. [DOI] [PubMed] [Google Scholar]
- 255.Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C. The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int. 2004;15:1003–1008. doi: 10.1007/s00198-004-1652-z. [DOI] [PubMed] [Google Scholar]
- 256.Rabenda V, Reginster JY. Overcoming problems with adherence to osteoporosis medication. Expert Rev Pharmacoecon Outcomes Res. 2010;10:677–689. doi: 10.1586/erp.10.76. [DOI] [PubMed] [Google Scholar]
- 257.Carr AJ, Thompson PW, Cooper C. Factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis: a cross-sectional survey. Osteoporos Int. 2006;17:1638–1644. doi: 10.1007/s00198-006-0166-2. [DOI] [PubMed] [Google Scholar]
- 258.Rabenda V, Bruyere O, Reginster JY. Relationship between bone mineral density changes and risk of fractures among patients receiving calcium with or without vitamin D supplementation: a meta-regression. Osteoporos Int. 2011;22:893–901. doi: 10.1007/s00198-010-1469-x. [DOI] [PubMed] [Google Scholar]
- 259.Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD. Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab. 2002;87:1586–1592. doi: 10.1210/jc.87.4.1586. [DOI] [PubMed] [Google Scholar]
- 260.Delmas PD, Li Z, Cooper C. Relationship between changes in bone mineral density and fracture risk reduction with antiresorptive drugs: some issues with meta-analyses. J Bone Miner Res. 2004;19:330–337. doi: 10.1359/JBMR.0301228. [DOI] [PubMed] [Google Scholar]
- 261.Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, Black DM. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002;112:281–289. doi: 10.1016/S0002-9343(01)01124-X. [DOI] [PubMed] [Google Scholar]
- 262.Watts NB, Geusens P, Barton IP, Felsenberg D. Relationship between changes in BMD and nonvertebral fracture incidence associated with risedronate: reduction in risk of nonvertebral fracture is not related to change in BMD. J Bone Miner Res. 2005;20:2097–2104. doi: 10.1359/JBMR.050814. [DOI] [PubMed] [Google Scholar]
- 263.Sarkar S, Mitlak BH, Wong M, Stock JL, Black DM, Harper KD. Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res. 2002;17:1–10. doi: 10.1359/jbmr.2002.17.1.1. [DOI] [PubMed] [Google Scholar]
- 264.Austin M, Yang YC, Vittinghoff E, et al. Relationship between bone mineral density changes with denosumab treatment and risk reduction for vertebral and nonvertebral fractures. J Bone Miner Res. 2012;27:687–693. doi: 10.1002/jbmr.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH. Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res. 2006;21:1785–1790. doi: 10.1359/jbmr.060802. [DOI] [PubMed] [Google Scholar]
- 266.Bruyere O, Roux C, Detilleux J, et al. Relationship between bone mineral density changes and fracture risk reduction in patients treated with strontium ranelate. J Clin Endocrinol Metab. 2007;92:3076–3081. doi: 10.1210/jc.2006-2758. [DOI] [PubMed] [Google Scholar]
- 267.Bruyere O, Roux C, Badurski J, Isaia G, de Vernejoul MC, Cannata J, Ortolani S, Slosman D, Detilleux J, Reginster JY. Relationship between change in femoral neck bone mineral density and hip fracture incidence during treatment with strontium ranelate. Curr Med Res Opin. 2007;23:3041–3045. doi: 10.1185/030079907X242818. [DOI] [PubMed] [Google Scholar]
- 268.Baim S, Wilson CR, Lewiecki EM, Luckey MM, Downs RW, Jr, Lentle BC. Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom. 2005;8:371–378. doi: 10.1385/JCD:8:4:371. [DOI] [PubMed] [Google Scholar]
- 269.Garnero P, Delmas PD. Biochemical markers of bone turnover in osteoporosis. In: Marcus M, Feldman D, Kelsey J, editors. Osteoporosis. San Diego: Academic; 2001. pp. 459–477. [Google Scholar]
- 270.Ravn P, Hosking D, Thompson D, Cizza G, Wasnich RD, McClung M, Yates AJ, Bjarnason NH, Christiansen C. Monitoring of alendronate treatment and prediction of effect on bone mass by biochemical markers in the early postmenopausal intervention cohort study. J Clin Endocrinol Metab. 1999;84:2363–2368. doi: 10.1210/jc.84.7.2363. [DOI] [PubMed] [Google Scholar]
- 271.Eastell R, Christiansen C, Grauer A, et al. Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. J Bone Miner Res. 2011;26:530–537. doi: 10.1002/jbmr.251. [DOI] [PubMed] [Google Scholar]
- 272.Bjarnason NH, Sarkar S, Duong T, Mitlak B, Delmas PD, Christiansen C. Six and twelve month changes in bone turnover are related to reduction in vertebral fracture risk during 3 years of raloxifene treatment in postmenopausal osteoporosis. Osteoporos Int. 2001;12:922–930. doi: 10.1007/s001980170020. [DOI] [PubMed] [Google Scholar]
- 273.Eastell R, Barton I, Hannon RA, Chines A, Garnero P, Delmas PD. Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate. J Bone Miner Res. 2003;18:1051–1056. doi: 10.1359/jbmr.2003.18.6.1051. [DOI] [PubMed] [Google Scholar]
- 274.Eastell R, Krege JH, Chen P, Glass EV, Reginster JY. Development of an algorithm for using PINP to monitor treatment of patients with teriparatide. Curr Med Res Opin. 2006;22:61–66. doi: 10.1185/030079905X75096. [DOI] [PubMed] [Google Scholar]
- 275.Bauer DC, Black DM, Garnero P, Hochberg M, Ott S, Orloff J, Thompson DE, Ewing SK, Delmas PD. Change in bone turnover and hip, non-spine, and vertebral fracture in alendronate-treated women: the fracture intervention trial. J Bone Miner Res. 2004;19:1250–1258. doi: 10.1359/JBMR.040512. [DOI] [PubMed] [Google Scholar]
- 276.Reginster JY, Collette J, Neuprez A, Zegels B, Deroisy R, Bruyere O. Role of biochemical markers of bone turnover as prognostic indicator of successful osteoporosis therapy. Bone. 2008;42:832–836. doi: 10.1016/j.bone.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 277.Persson U, Hjelmgren J. Health services need knowledge of how the public values health. Lakartidningen. 2003;100:3436–3437. [PubMed] [Google Scholar]
- 278.Eichler HG, Kong SX, Gerth WC, Mavros P, Jonsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7:518–528. doi: 10.1111/j.1524-4733.2004.75003.x. [DOI] [PubMed] [Google Scholar]
- 279.Macroeconomics and health: investing in health for economic development: report of the Comission on Macroeconomics and Health. Geneva: WHO; 2001. [Google Scholar]
- 280.Kanis JA, Jonsson B. Economic evaluation of interventions for osteoporosis. Osteoporos Int. 2002;13:765–767. doi: 10.1007/s001980200106. [DOI] [PubMed] [Google Scholar]
- 281.Fleurence RL, Iglesias CP, Torgerson DJ. Economic evaluations of interventions for the prevention and treatment of osteoporosis: a structured review of the literature. Osteoporos Int. 2006;17:29–40. doi: 10.1007/s00198-005-1943-z. [DOI] [PubMed] [Google Scholar]
- 282.Zethraeus N, Borgstrom F, Strom O, Kanis JA, Jonsson B. Cost-effectiveness of the treatment and prevention of osteoporosis—a review of the literature and a reference model. Osteoporos Int. 2007;18:9–23. doi: 10.1007/s00198-006-0257-0. [DOI] [PubMed] [Google Scholar]
- 283.Kanis JA, McCloskey E, Jonsson B, Cooper C, Strom B, Borgstrom F. An evaluation of the NICE guidance for the prevention of osteoporotic fragility fractures in postmenopausal women. Arch Osteoporos. 2010;5:19–48. doi: 10.1007/s11657-010-0045-5. [DOI] [Google Scholar]
- 284.Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA. Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries—an economic evaluation based on the fracture intervention trial. Osteoporos Int. 2007;18:1047–1061. doi: 10.1007/s00198-007-0349-5. [DOI] [PubMed] [Google Scholar]
- 285.Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int. 2001;12:417–427. doi: 10.1007/s001980170112. [DOI] [PubMed] [Google Scholar]
- 286.Borgstrom F, Johnell O, Kanis JA, Jonsson B, Rehnberg C. At what hip fracture risk is it cost-effective to treat? International intervention thresholds for the treatment of osteoporosis. Osteoporos Int. 2006;17:1459–1471. doi: 10.1007/s00198-006-0107-0. [DOI] [PubMed] [Google Scholar]
- 287.Borgstrom F, Strom O, Coelho J, Johansson H, Oden A, McCloskey EV, Kanis JA. The cost-effectiveness of risedronate in the UK for the management of osteoporosis using the FRAX. Osteoporos Int. 2010;21:495–505. doi: 10.1007/s00198-009-0989-8. [DOI] [PubMed] [Google Scholar]
- 288.Borgstrom F, Strom O, Coelho J, Johansson H, Oden A, McCloskey E, Kanis JA. The cost-effectiveness of strontium ranelate in the UK for the management of osteoporosis. Osteoporos Int. 2010;21:339–349. doi: 10.1007/s00198-009-0971-5. [DOI] [PubMed] [Google Scholar]
- 289.Jonsson B, Strom O, Eisman JA, Papaioannou A, Siris ES, Tosteson A, Kanis JA. Cost-effectiveness of denosumab for the treatment of postmenopausal osteoporosis. Osteoporos Int. 2011;22:967–982. doi: 10.1007/s00198-010-1424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Update on pharmacological interventions and an algorithm for management. London: RCP; 2000. [Google Scholar]
- 291.Delmas PD, Recker RR, Chesnut CH, 3rd, Skag A, Stakkestad JA, Emkey R et al (2004) Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int 15:792–798 [DOI] [PubMed]