Abstract
Objective
Though children with attention-deficit/hyperactivity disorder (ADHD) are at risk for impulsive, health-endangering behavior, few studies have examined non-substance use-related risk-taking behaviors. This study examined whether adolescents and young adults with ADHD histories were more likely than those without ADHD histories to report frequent engagement in motorsports, a collection of risky driving-related activities associated with elevated rates of physical injury. Path analyses tested whether persistent impulsivity, comorbid conduct disorder or antisocial personality disorder (CD/ASP), and heavy alcohol use mediated this association. Analyses also explored whether frequent motorsporting was associated with unsafe and alcohol-influenced driving.
Method
Two-hundred and twenty-one adolescent and young adult males (16–25 years-old) diagnosed with ADHD in childhood and 139 demographically-similar males without ADHD histories reported their motorsports involvement. Persistent impulsivity, CD/ASP, heavy drinking, and hazardous driving were also measured in adolescence/young adulthood1
Results
Adolescents and young adults with ADHD histories were more likely to report frequent motorsports involvement than those without childhood ADHD. Impulsivity, CD/ASP and heavy drinking partially mediated this association, such that individuals with ADHD histories, who had persistent impulsivity or CD/ASP diagnoses, were more likely to engage in heavy drinking, which was positively associated with frequent motorsporting. Motorsports involvement was associated with more unsafe and alcohol-influenced driving, and this association was more often found among those with, than without, ADHD histories.
Conclusions
Adolescents and young adults with ADHD histories, especially those with persisting impulsivity, comorbid CD/ASP and heavy drinking tendencies, are more likely to engage in motorsports, which may heighten risk of injury.
Attention-deficit hyperactivity disorder (ADHD), a syndrome characterized by difficulties with paying attention and managing hyperactivity/impulsivity, is the most common mental health disorder of childhood (9.5% of 4–17 year-olds in U.S.; Center for Disease Control, 2010). Children with ADHD experience functional deficits across multiple settings (e.g., academic underperformance, interpersonal problems; Barkley, 2006). Though once considered a childhood-limited disorder (American Psychiatric Association [APA], 1994), ADHD symptoms and impairment are now known to persist for many through adolescence and into adulthood (APA, 2010). Individuals with persistent ADHD are at risk for comorbid disruptive behavior problems as adolescents (i.e. conduct disorder [CD]; Mannuzza, Klein, Abikoff, & Moulton, 2004) and as adults (i.e. antisocial personality disorder [ASP]; Barkley, Murphy & Fischer, 2008), as well as educational and occupational difficulties, discordant interpersonal relationships, and health and financial hardships (Barkley, Fischer, Edelbrock, & Smallish, 1990; Barkley et al., 2008; Mannuzza, Klein, Bessler, Malloy, & LaPadula, 1998; Weiss & Hechtman, 1993). Another area of concern for adolescents and young adults with a history of ADHD is engagement in risky or health-endangering behaviors.
Studies assessing risk-taking in this population have primarily focused on substance use and abuse/dependence (Molina, 2011). Recent meta-analytic reviews (Charach, Yeung, Climans, & Lillie, 2011; Lee, Humphreys, Flory, Liu, & Glass, 2011) identify increased risk of alcohol use disorder and non-alcohol substance use disorders among children with ADHD studied prospectively into adulthood. In our longitudinal study of children with ADHD (Pittsburgh ADHD Longitudinal Study, or PALS), we found more frequent heavy drinking and alcohol use disorder for adolescents (aged 15 to 17) with, than without, childhood ADHD. In early adulthood (18 to 25 year-olds), when drinking became common for all participants, only individuals with childhood ADHD and ASP reported more heavy drinking than those without ADHD histories (Molina, Pelham, Gnagy, Thompson, & Marshal, 2007). Others have similarly reported links between childhood ADHD, the development of CD/ASP, and the subsequent development of substance use problems (e.g., August et al., 2006; Gittelman, Mannuzza, Shenker, & Bonagura, 1985; Satterfield et al., 2007). Beyond these well-known outcomes, we and others have also reported other behavioral outcomes with an element of risk to self or others. Young adults with childhood ADHD are more likely to report having sexual intercourse at younger ages, with more partners (including ones they did not know or had just met), and more often without protection than those without childhood ADHD (Barkley, Fischer, Smallish, & Fletcher, 2006; Flory, Molina, Pelham, Gnagy, & Smith, 2006). Not surprisingly, ADHD has also been associated with thrill- or sensation-seeking tendencies (for review, see White, 1999). Despite these findings, few studies have explored whether childhood ADHD increases the likelihood of engaging in other risky and potentially health-endangering behaviors, especially those that are less clearly attached to the spectrum of deviant behavior.
A particularly relevant, unsafe behavior exhibited by adolescents and young adults, regardless of ADHD status, is hazardous driving. Automobile accidents are the leading cause of death for young people, causing one-third of all deaths for 15–20 year-olds (National Highway Traffic Safety Administration, 2006). It is not surprising that adolescents and young adults with childhood ADHD are involved in more automobile accidents and receive more traffic citations than those without ADHD histories (Barkley, Guevremont, Anastopoulos, DuPaul, & Shelton, 1993; Barkley et al., 2008; Thompson, Molina, Pelham & Gnagy, 2007; for review, see Barkley, 2004). On the other hand, results are less clear when examining self-reported risky driving behavior that requires subjective judgment (e.g., speeding, driving too close to other cars). Our research (Thompson et al., 2007) and that of Barkley and colleagues (1993, 2008) found that childhood ADHD did not increase reports of risky driving by adolescent or young adult drivers. In fact, young adults with ADHD have previously reported driving more safely than those without ADHD despite experiencing more automobile collisions and receiving more traffic citations (Knouse, Bagwell, Barkley, & Murphy, 2005). These findings may have been due to ADHD-related underreporting of behaviors with negative social stigma (i.e. inability to drive well). Examining risky driving behaviors with lower social stigma may allow for relevant differences to arise between individuals with and without expected risk for impulsive, thrill-seeking tendencies, such as individuals with ADHD histories.
One risky driving-related behavior that may have less social stigma than unsafe driving, and which is the subject of the current study, is motorsporting. Motorsports encompass a range of activities, including various types of auto racing (e.g., stock car, truck), all-terrain vehicle (ATV) riding, motorcycle trail bike racing, and four wheeling. Though motorsporting is a relatively popular thrill-seeking activity, the current literature highlights the potential dangers of frequent involvement in motorsports. Individuals, especially 18–24 year-old males, participating in motorsports are at risk of ejection from the vehicle and roll-overs, which often result in serious head or spine injuries (Finn & MacDonald, 2010; Gabbe, Finch, Cameron, & Williamson, 2005; Krauss, Dyer, Laupland, & Buckley, 2010). Not surprisingly, frequent motorsporters tend to have a proclivity for sensation seeking (Jack & Ronan, 1998; Straub, 1982), a characteristic closely intertwined with impulsivity (for review, see Zuckerman, 1994), which is a core symptom of ADHD. Adolescents and young adults with childhood ADHD, particularly those with persisting symptoms and impulsive risk-taking tendencies (e.g., heavy drinking, risky sex; Flory et al., 2006; Molina et al., 2007), might gravitate to motorsports given the exciting nature of those activities. However, studies have yet to examine whether ADHD histories are associated with frequent participation in motorsport activities in adolescence and young adulthood, or whether persisting impulsivity may explain this association.
Conduct problems in adolescence and young adulthood (CD/ASP) may also underlie potential associations between childhood ADHD and motorsporting. Studies have demonstrated the temporal precedence of ADHD to the onset of conduct problems for many children (e.g., Barkley et al., 1990) and have established childhood ADHD as a unique predictor of later engagement in antisocial behavior (Mannuzza et al., 2004; Sibley et al., 2011). Persistent or developing conduct problems (CD/ASP) have been shown to increase the likelihood of adolescents and young adults with ADHD histories engaging in health-endangering behavior, such as unsafe driving (Barkley et al., 1993) and substance use disorders (Gittelman et al., 1985; Molina et al., 2007). Thus, CD/ASP may also elevate the risk of individuals with childhood ADHD frequently engaging in motorsports. At the same time, because motorsporting activities are not conceptually tied to the presence of antisocial behaviors (i.e., there is no reason to expect that motorsporting occurs only among individuals with antisocial tendencies), childhood ADHD and/or persisting impulsivity may contribute to motorsport involvement by children with ADHD independent of any tendencies to later develop CD/ASP.
Heavy alcohol use may contribute to ADHD-related risk of engagement in motorsporting. As discussed by Molina (2011), the developmental progression towards alcohol use problems among those with ADHD histories is aided by the persistence of ADHD symptoms and development of conduct problems. Heavy drinking resulting from these tendencies may also contribute to other forms of thrill-seeking. For example, alcohol increases the risk of young adults, particularly those with elevated sensation-seeking tendencies, engaging in unprotected sex with nonmonogamous partners (Quinn & Fromme, 2010). Alcohol has also been shown to decrease expectations of negative outcomes that might result from risky activities (Fromme, Katz, & D'Amico, 1997), and it increases social disinhibition (Freeman, Friedman, Bartholow, & Wulfert, 2010) that may facilitate participation in risky sports with others. Importantly, alcohol impairs judgment and is associated with increased rates of injury in motorsport involvement (Tator, 2008). As such, the contribution of alcohol use in a population already vulnerable to thrill-seeking activities is important to understand. We hypothesize that one possible route to frequent motorsport involvement for children with ADHD may be through persisting impulsivity and/or conduct problems that contribute to heavy drinking.
Study Aims and Hypotheses
The primary goal of this study was to examine the prospective association between childhood ADHD and later motorsports involvement. We hypothesized that adolescents and young adults with ADHD histories would report more frequent motorsporting than those without ADHD histories. We hypothesized that impulsivity, CD/ASP and heavy drinking in adolescence/young adulthood (all measured at single time point) would mediate this association. These predictions are diagrammed in Figure 1. Given the limited research on relations between motorsporting and automobile driving, an exploratory goal of this study was to investigate whether frequent motorsporting was related to unsafe (traffic citations and accidents) and alcohol-influenced driving (traffic citations and accidents after drinking). We explored this in the full sample as well as separately among individuals with or without ADHD histories. In light of the potential hazards of driving motorsport vehicles for all adolescents and young adults, particularly those with driving skill deficiencies and thrill-seeking tendencies like those with ADHD (e.g., Barkley, Murphy, & Kwasnik, 1996), the outcomes of this study were believed to have significant clinical and policy implications.
Figure 1.
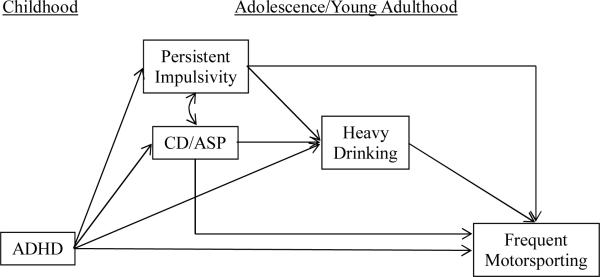
Path model proposed to explain prospective associations between childhood ADHD and frequent motorsporting in adolescence/young adulthood.
Method
Participants
ADHD group
Participants with childhood ADHD were recruited from a pool of 516 study-eligible participants diagnosed with DSM-III-R or DSM-IV ADHD in childhood and treated at the Attention Deficit Disorder clinic at the Western Psychiatric Institute and Clinic (WPIC) in Pittsburgh, PA from 1987 to 1996. Of the 516, 493 were re-contacted an average of 8.35 years later (SD = 2.79) to participate in annual interviews for the Pittsburgh ADHD Longitudinal Study (PALS). Of those contacted, 364 (70.5 %) enrolled in the follow-up study. At the first follow-up interview, participants with ADHD histories ranged in age from 11 to 28 with 99% falling between 11 and 25 years of age. They were admitted to the follow-up study on a rolling basis between the years 1999–2003 and completed their first follow-up interview immediately upon enrollment.
All adolescents and young adults with childhood ADHD participated in the Summer Treatment Program (STP) for children with ADHD, an 8-week intervention that included behavioral modification, parent training, and psychoactive medication trials where indicated (Pelham, Fabiano, Gnagy, Greiner, & Hoza, 2005). Diagnostic information for the participants with ADHD histories was collected at initial referral to the clinic in childhood (baseline) using parent and teacher DSM-III-R and DSM-IV symptom ratings scales (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992) and a semi-structured diagnostic interview administered to parents by a Ph.D. level clinician. The interview consisted of the DSM-III-R or DSM-IV descriptors for ADHD, ODD, and CD with supplemental probe questions regarding situational and severity factors. It also included queries about other comorbidities to determine whether additional assessment was needed. Following DSM guidelines, diagnoses of ADHD, ODD, and CD were made if a sufficient number of symptoms were endorsed (considering information from both parents and teachers) to result in diagnosis. Two Ph.D. level clinicians independently reviewed all ratings and interviews to confirm DSM diagnoses and when disagreement occurred, a third clinician reviewed the file and the majority decision was used. Exclusion criteria for participants with ADHD histories was assessed in childhood (baseline) and included a full-scale IQ < 80, a history of seizures, neurological problems, pervasive developmental disorder, schizophrenia, and/or other psychotic or organic mental disorders.
Participants in the follow-up study were compared with the eligible individuals who did not enroll on demographic (i.e., age at first treatment, race, parental education level, and marital status) and diagnostic (i.e., parent and teacher ratings of ADHD and related symptomatology) variables collected at baseline. Only one of 14 comparisons was statistically significant at the p<.05 significance level: PALS participants had a slightly lower average CD symptom rating on a four point scale as indicated by a composite of parent and teacher ratings (participants M = 0.43, non-participants M = 0.53).
Control group
Two-hundred and forty participants without ADHD (i.e. controls) were recruited for the PALS from the greater Pittsburgh community between 1999 and 2001. These individuals were recruited from several sources including pediatric practices in Allegheny County (40.8%), advertisements in local newspapers (27.5%), local universities and colleges (20.8%), and other methods (10.9%) such as Pittsburgh Public Schools and word of mouth. Control recruitment lagged three months behind the ADHD group enrollment in order to facilitate efforts to obtain demographic similarity (discussed below). A telephone screening interview was administered to parents of potential control participants to gather basic demographic characteristics, history of diagnosis or treatment for ADHD and other behavior problems, presence of exclusionary criteria as previously listed for the ADHD group, and a checklist of ADHD symptoms. Young adults (age 18+) also provided self-report of ADHD symptoms. ADHD symptoms were counted as present if reported by either the parent or the young adult. Controls, who met DSM-III-R criteria for ADHD, either currently or historically, were immediately excluded from study consideration.
If a potential control participant passed the initial phone screen, senior research staff members met to determine whether he/she was demographically appropriate for the study. Each potential control participant was examined on four demographic characteristics: 1) age, 2) gender, 3) race, and 4) parent education level. A control participant was deemed study-eligible if his/her enrollment increased the control group's demographic similarity to the participants diagnosed with ADHD. At the end of the recruitment process, the two groups were equivalent on the four demographic variables noted above.
Current study subsample
Data for the current study were provided by the 360 (n = 221 ADHD; n = 139 control) males who were of driving age (sp. 16–25 years-old) at the first follow-up interview (first interview for the control group). We excluded females from the current study because they reported motorsporting infrequently (n = 2). With a sample of this size, our study was sufficiently powered to detect any remotely moderate effects at p < .05 (correlation effect size = .30, power > .99).
Procedure
As noted, baseline diagnostic information was gathered for the ADHD group at initial referral to the clinic during childhood. Follow-up interviews in adolescence and early adulthood were conducted by post-baccalaureate research staff. All questionnaires (paper and pencil or web-based) in the current study were completed privately. During informed consent, participants were assured of the confidentiality of disclosed materials. In cases where distance prevented participant travel to WPIC, information was collected through mail, telephone correspondence, and home visits. PALS follow-up interviews were conducted yearly beginning in the year of enrollment. Data for the current study were from the first follow-up visit. Participants were permitted to take stimulant medication on the day of the assessment; however a minority of the ADHD group (<10%) were prescribed stimulant medication at the time of follow-up.
Measures
Motorsport activities
Motorsports involvement at follow-up was assessed via self-report on a 21-item questionnaire adapted from a measure used by Donovan (1993) assessing involvement in thrill-seeking sports activities such as skiing, rock climbing, and hunting. Item responses ranged from (1) “I have never done it, and I would not like to try it” to (7) “I do it now, very often.” Donovan (1993) reported that the risky sports measure demonstrated acceptable internal consistency (α = .72–.81) and convergent validity, as it was found to correlate significantly with risky driving (sp. drinking and driving, r =.41). Included in this scale are four items measuring involvement in motorsports, including auto racing, four wheeling, motorcycle trail biking, and all-terrain vehicle (ATV) driving. In this sample, the internal consistency of the 4-item motorsports subscale was acceptable (α = .75). Based on their responses to these motorsport items, participants were classified into one of two groups: Frequent motorsporters consisted of those who regularly engaged (“used to do it regularly” or “do it now, very often”) in one or more of the four motorsports, and infrequent motorsporters who did not engage or rarely engaged (“I have done it, but only once/twice” or “I do it now, once in a while”) in any motorsport. One response (“I do it now, whenever I can”) was dropped from all analyses because it could not be confidently classified in either group due to its ambiguity. This response option was infrequently selected (5.5% of all cases for four wheeling and <3.5% for all other motorsports), and there were no ADHD group differences in the percent dropped for this reason. The occurrence (yes/no) of frequent involvement in any motorsport was the main study outcome.
Persistent impulsivity
Impulsivity in adolescent/young adulthood was reported by the mothers of participants on the 23-item Eysenck Impulsivity Scale (EIS; Eysenck, Easting, & Pearson, 1984). White and colleagues (1994) adapted the original British items for American dialect and simplicity of vocabulary. Each question is scored as yes or no. Responses to the 12 items with the strongest face validity for measurement of impulsivity (e.g., “Do you act without thinking first?”) were summed to create an index of impulsivity. [Other items, such as those measuring attitudes or anger control, “Do you get mad every time someone keeps you waiting?” were disregarded.] Internal consistency was good for this measure (α = .88).
CD/ASP diagnoses
For participants younger than 18, parent and teacher-report of CD symptoms were measured at follow-up using the Disruptive Behavior Disorder rating Scale (DBD; Pelham et al., 1992) and the CD module of the Diagnostic Interview Schedule for Children, Version 4 (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Like all DSM-based symptom rating scales, the DBD rating scale has acceptable psychometric properties (e.g., α = .75 for CD; Pelham et al., 1992). The DISC also has well-established psychometrics, including moderate test-retest agreement (κ = .59) and good concurrent validity for CD diagnoses (κ = .74; Schwab-Stone, Shaffer, Dulcan, Jensen, & Fisher, 1996). To determine CD diagnoses, the higher of parent (mother unless not participating) DBD, parent DISC, and teacher DBD ratings for each symptom were used. Symptom counts were computed and diagnoses were made using DSM-IV cutoffs (sp. 3 or more clinically-significant symptoms). For participants 18 and older, young adults and their mothers reported symptoms of ASP via the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II; First, Gibbon, Spitzer, & Williams, 1997). ASP diagnoses were determined by summing the frequency of clinically-significant symptoms of ASP (out of 7) across the maximum item ratings provided by participants and/or their mothers. For the current study, participants with 3 or more ASP symptoms were coded as meeting diagnostic criteria for ASP per DSM-IV criteria (APA, 1994).
Heavy drinking
Heavy alcohol use was assessed at follow-up using self-report on the Substance Use Questionnaire (SUQ; Molina et al, 2007). The SUQ, an adaptation of items from the Health Behavior Questionnaire (Jessor, Donovan, & Costa, 1989) and National Household Survey of Drug Abuse interview (NHSDA, 1992), is comprised of both lifetime exposure and quantity/frequency questions. For this study, two items were of interest, (1) frequency of binge drinking (“In the past 12 months, how often did you drink 5 or more drinks when you were drinking?”); and (2) frequency of drunkenness (“In the past 12 months, how often have you gotten drunk or “very, very high” on alcohol?”). The response scale for both items ranged from (0)”Not at all” to (11) “Several times a day.” Participants were ensured their responses would be kept confidential. We re-administered these questions to a subset of our participants two weeks later. The reliability correlations were .84 (N = 222) for binge drinking and .87 (N = 219) for drunkenness. Because binge drinking and drunkenness were highly intercorrelated (r = .87), the mean score of both items was computed to form a composite “heavy drinking” variable.
Driving-related accidents and citations
Participants reported their history of problem driving behavior at follow-up on an adapted version of the Young Adult Driving Questionnaire (Donovan, 1993). For the purposes of this study, only items assessing the lifetime occurrence (yes/no) of traffic accidents and driving-related citations (tickets), as well as the lifetime occurrence (yes/no) of traffic accidents and tickets after consuming alcohol, were examined. [For additional data on risky driving in the PALS sample, see Thompson and colleagues (2007).] As with questions assessing heavy drinking, participants were ensured their responses to these questions would be kept confidential.
Analytic Overview
First, group differences in motorsport involvement were examined by comparing the rates of frequent (vs. infrequent) participation in any motorsports (chi-square tests) by youth with and without childhood ADHD. Next, path analyses were used to test whether persisting impulsivity, CD/ASP and heavy drinking (all measured at a single time point in adolescence/young adulthood) mediated prospective associations between childhood ADHD and frequent motorsporting in adolescence/young adulthood (see Figure 1). We estimated the path models using Mplus 6.0 (Muthen and Muthen, 2010) and the WLSMV estimator (weighted least squares with robust means and variances) because frequent motorsporting was a binary outcome. Following MacKinnon (2008), bootstrapping (with 5000 sample replacements) was used to determine point estimates and standard errors for the mediation model while bias-corrected confidence intervals were calculated to account for any non-normality of the parameter estimate distributions. Indirect effects were estimated for all potential pathways from childhood ADHD to frequent motorsporting. Based on simulation estimates by Fritz and MacKinnon (2007), our study is sufficiently powered to detect at least moderate indirect effects at p < .05. Finally, related to our exploratory aims, chi-square analyses compared the proportions of frequent vs. infrequent motorsporters reporting unsafe and alcohol-influenced driving. The tests were first done with the full sample (collapsing across ADHD groups) and then separately by childhood ADHD status. Because very few individuals without childhood ADHD reported frequent engagement in motorsports and unsafe/alcohol-influenced driving, we did not have the power to detect statistical interactions. Fisher's exact probability tests, which are well-powered to test for significant differences between groups with small cell sizes, were conducted instead to examine whether rates of unsafe and alcohol-influenced driving varied for frequent vs. infrequent motorsporters within ADHD groups.
Results
Sample Descriptives
As expected, given the procedure used to recruit demographically-similar groups, participants with and without childhood ADHD in our sample did not differ significantly by age (for ADHD group, M=19.15, SD=2.34; for control group, M=18.86, SD=2.12; t = 1.19, p = .24), ethnicity/racial minority (for ADHD group, 16.7% were minorities; for control group, 12.9% were minorities; χ2 = .95, p = .33), or highest parent education (for ADHD group, M=7.15, SD=1.62; for control group, M=7.34, SD=1.61, on a scale: 1=less than seventh-grade education to 9=graduate professional training; t = .99, p = .32). Conversely, relative to those without ADHD histories, participants with childhood ADHD were more likely to live at home with their parents (75.1% of ADHD group lives at home; 62.6% of control group lives at home; χ2 = 6.41, p < .05), less likely to be licensed drivers and/or to have driven in the past 6 months (76% of ADHD group with license/recent driving experience; 94% of control group with license/recent driving experience; χ2 = 20.14, p < .01), and less likely to be pursuing or to have already earned a post-secondary degree (37.3% of ADHD group reported at least some college experience; 57.2% of control group reported at least some college experience; χ2 = 13.67, p < .01).
Childhood ADHD and Frequent Motorsports Involvement
As expected, adolescents and young adults with ADHD histories were more than 3 times as likely as controls, on average, to report frequent participation in one or more motorsport activities (Table 1). When different types of motorsports were analyzed separately, participants with childhood ADHD reported frequently participating in four wheeling more often than controls. The chi-square statistic for auto racing could not be examined because the cell size for controls was zero. However, using a test powered to analyze between-group differences in categorical variables with small cell sizes (Fisher's exact probability test), the rate of auto racing differed significantly between participants with and without ADHD histories (two-tail p < .05). Frequent involvement in motorcycle trail biking and ATV driving did not differ significantly between groups.
Table 1.
Childhood ADHD Predicts Frequent Motorsports Involvement
| Controls (%) | ADHD (%) | χ 2 | p | OR (95% CI) | |
|---|---|---|---|---|---|
| Any Frequent Motorsports Involvement | 6.5 | 19.0 | 11.02 | <.01 | 3.39 (1.59, 7.21) |
| Auto Racing | 0.0 | 3.2 | - | - | - |
| Four Wheeling | 2.2 | 8.6 | 6.17 | <.05 | 4.26 (1.24, 14.69) |
| Motorcycle Trail Biking | 4.3 | 9.5 | 3.31 | .07 | 2.33 (.92, 5.92) |
| All-Terrain Vehicle Driving | 4.3 | 7.7 | 1.63 | .20 | 1.85 (.71, 4.81) |
Note. ADHD n=221, Control n=139. All percentages indicate endorsement of “frequent” involvement (sp. “used to do it regularly” or “do it now, very often”). OR = odds ratio and represents the likelihood of participants with childhood ADHD reporting frequent involvement in motorsport activities relative to controls. For auto racing, the chi-square statistic and odds ratio could not be computed because the cell size for controls was 0. However, Fisher's exact probability test indicated that individuals with ADHD were significantly more likely to engage in auto racing than controls.
Persistent Impulsivity, CD/ASP, and Heavy Drinking as Mediators
Correlations among potential covariates (age, education level, living at home, household income), predictors (childhood ADHD), hypothesized mediators (adolescent/young adult impulsivity, CD/ASP, heavy drinking), and frequent motorsporting are presented in Table 2. Because education level and household income were not significantly associated with motorsporting, they were not included as covariates in the path analyses. Relative to those without ADHD histories, adolescents and young adults with ADHD histories were more impulsive (ADHD group: M=7.22, SD=3.46; Control group: M=2.59, SD=2.72; t (275) = 11.88, p < .01), more likely to meet criteria for CD/ASP (ADHD group: 28.3%; Control group: 2.9%; χ2 = 36.58, p < .01), but not more likely to report heavy drinking (ADHD group: M=2.43, SD=2.69; Control group: M=2.25, SD=2.47; t (356) = .61, p = .54).
Table 2.
Correlations among Covariates, Predictor and Outcome Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | - | |||||||
| 2. Level of Education | .60** | - | ||||||
| 3. Living at Home | −.40** | −.42** | - | |||||
| 4. Parent's Household Income | .08 | .14* | −.05 | - | ||||
| 5. Childhood ADHD | .06 | −.27** | .13* | −.07 | - | |||
| 6. Persistent Impulsivity | .02 | −.22** | .14* | −.05 | .58** | - | ||
| 7. CD/ASP | .09 | −.18** | −.06 | −.05 | .32** | .31** | - | |
| 8. Heavy Drinking | .22** | .19** | −.24** | −.02 | .03 | .14* | .24** | - |
| 9. Frequent Motorsports Involvement? | .14* | −.09 | −.08 | −.06 | .18** | .10 | .22** | .20** |
Notes: n=358, except for correlations with maternal-reported impulsivity (n=277); Level of education= did participant report any years of college education (0=no, 1=yes)?; Living at Home=Does participant live with parents (0=no, 1=yes)?; Childhood ADHD (0=Control, 1=ADHD); Persistent Impulsivity=Sum of items from Eysenck Impulsivity Scale; CD/ ASP=Did participant have conduct disorder (if 16/17 years-old) or antisocial personality disorder (if 18–25 years-old; 0=no, 1=yes)?; Heavy drinking=Mean of rate of binge drinking and/or drunkenness in past 12 months (0=Not at all to 11=Several times/day); Frequent Motorsports Involvement?=Did participant endorse regular involvement (“used to do it regularly” or “do it now, very often”) in at least one motorsport (0=no, 1=yes)?
p < .05;
p < .01
Results of the path analyses are presented in Figure 2. Because this model had no constraints, it was just identified, having no degrees of freedom and perfect fit. Childhood ADHD (95% confidence interval [CI] = .18–1.16) continued to uniquely predict the propensity to engage frequently in motorsports during adolescence/young adulthood over and above proposed mediators. However, three mediational pathways were statistically significant. One pathway was through persisting impulsivity and heavy drinking (Indirect effect estimate = .046, 95% CI = .009–.115). Childhood ADHD predicted impulsivity (95% CI = 3.81–5.32), which was associated with heavy drinking (95% CI = .034–.208), which was associated with frequent motorsporting (95% CI = .019–.143). A second pathway was through CD/ASP and heavy drinking (Indirect effect estimate = .029, 95% CI = .007–.069). Childhood ADHD predicted CD/ASP (95% CI = .197–.332), which was associated with heavy drinking (95% CI = .50–2.13), which was associated with frequent motorsporting (95% CI = .019–.143). A third pathway was through CD/ASP (Indirect effect estimate = .111, 95% CI = .001–.221). Childhood ADHD predicted CD/ASP (95% CI = .197–.332), which was associated with frequent motorsporting (95% CI = .001–.787). The path from childhood ADHD to frequent motorsporting via persisting impulsivity-only was not statistically significant.
Figure 2.
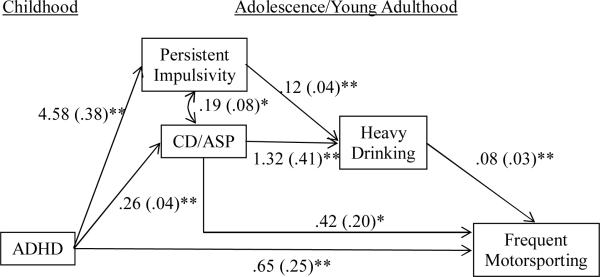
Results of path analyses investigating potential mediators between childhood ADHD and frequent motorsporting in adolescence/young adulthood. Non-significant paths included in the model have been omitted from the graphic to improve clarity. Age and living at home status were covaried. Unstandardized betas and bootstrapped standard errors are provided. * p < .05; ** p < .01
Frequent Motorsport Involvement and Driving-Related Accidents and Citations
As shown in Table 3, the associations between frequent motorsporting and accidents/citations were each statistically significant when examined for the full sample. Specifically, when compared to infrequent motorsporters, frequent motorsporters were more likely to have been in a traffic accident, to have been in an accident after drinking, to have received a traffic ticket, and to have received a ticket after drinking. Next, associations between frequent motorsporting and unsafe driving behavior were examined separately by ADHD status. For adolescents and young adults with childhood ADHD, frequent motorsporters were more likely than infrequent motorsporters to have been in accidents and to have received tickets, including after drinking (Table 3). However, for those without ADHD histories, only one of four associations was statistically significant: frequent motorsporters were more likely than infrequent motorsporters to have received a traffic ticket. Otherwise, unsafe driving behavior did not differ significantly between frequent and infrequent motorsporters without childhood ADHD. Finally, repeating the set of analyses with only participants who had driver's licenses or driving experience in the past 6 months uncovered the same pattern of results—that is, frequent motorsporters were more likely to report driving-related tickets and accidents, and frequent motorsporters with childhood ADHD histories were at risk of tickets and accidents whereas those without ADHD histories were not.
Table 3.
Frequent Motorsports Participation Is Associated with Unsafe and Alcohol-Influenced Driving
| Frequent Motorsporters | Infrequent Motorsporters | χ 2 | p | OR (95% CI) | |
|---|---|---|---|---|---|
| History of Being in a Traffic Accident | 62.5% (30/48) | 41.5% (102/246) | 7.18 | < .01 | 2.35 (1.24, 4.45) |
| ADHD | 61.5% (24/39) | 40.9% (52/127) | - | < .05 | - |
| Control | 66.7% (6/9) | 42.0% (50/119) | - | .18 | - |
| In an Accident after Drinking | 20.0% (6/30) | 6.9% (7/102) | 4.51 | < .05 | 3.39 (1.04, 11.03) |
| ADHD | 25.0% (6/24) | 3.8% (2/52) | - | < .05 | - |
| Control | 0.0% (0/6) | 10.0% (5/50) | - | 1.00 | - |
| History of Receiving a Traffic Ticket | 75.0% (36/48) | 38.0% (93/245) | 22.35 | < .01 | 4.90 (2.43, 9.90) |
| ADHD | 71.8% (28/39) | 44.0% (55/125) | - | < .01 | - |
| Control | 88.9% (8/9) | 31.7% (38/120) | - | < .01 | - |
| Received a Ticket after Drinking | 17.1% (6/35) | 4.3% (4/92) | 5.72 | < .05 | 4.55 (1.20, 17.26) |
| ADHD | 14.3% (4/28) | 1.9% (1/54) | - | < .05 | - |
| Control | 28.6% (2/7) | 7.9% (3/38) | - | .17 | - |
Notes: Frequent motorsporting = being regularly engaged (“used to do it regularly” or “do it now, very often”) in one or more motorsports. Numbers in the parentheses represent the frequency of participants endorsing the unsafe or alcohol-influenced driving divided by the total frequency of participants with the same level of motorsport involvement. Chi-squares were computed for main analyses; Fisher's exact probability tests were conducted to examine whether associations between motorsporting and driving behavior differed for participants with and without ADHD histories. OR = odds ratio and represents the likelihood of frequent motorsporters reporting unsafe or alcohol-influenced driving relative to infrequent motorsporters.
Discussion
The present study investigated whether adolescents and young adults diagnosed with ADHD in childhood were more likely to frequently engage in a risky driving activity with thrill-seeking characteristics and a documented increased risk of injury: motorsports. Between-group testing revealed that adolescents and young adults with ADHD histories endorsed more frequent participation in motorsports, particularly four wheeling and auto racing, than those without ADHD histories. Path analyses showed that childhood ADHD was prospectively associated with frequent motorsporting via connections with persisting impulsivity, CD/ASP, and heavy drinking. Specifically, adolescents and young adults with ADHD histories and current CD/ASP were more likely to frequently engage in motorsport activities. Moreover, those with childhood ADHD who reported elevated impulsivity or comorbid CD/ASP in adolescence/young adulthood were also more likely to endorse elevated rates of heavy drinking, which was associated with frequent motorsports involvement. Exploratory analyses indicated that frequent motorsporters were likely to report driving-related accidents and citations, including those occurring after drinking alcohol. When examined separately by ADHD status, associations between frequent motorsporting and unsafe driving were more often found among individuals with, than without, ADHD histories.
Our findings build on prior research by revealing that adolescents and young adults with ADHD histories are not only at risk of engaging in health-endangering behaviors typically associated with deviance, such as substance abuse (Molina, 2011) and risky sex (Barkley et al., 2006; Flory et al., 2006), but also risk-taking behaviors that are not inherently “deviant” or illegal -- in this case, motorsports. At the same time, our findings contrast with those of prior studies, including one using the same data set (Thompson et al., 2007), which found no differences in rates of self-reported risky driving (e.g., speeding, driving too close to other cars) among those with and without childhood ADHD. We speculate that, because there is less social stigma attached to the reporting of motorsports, adolescents and young adults with ADHD may be more willing to divulge engaging in this risky driving-related behavior. Investigations are needed to replicate and extend these findings. For example, considering the serious health risks for 16 year-olds (and younger children) participating in motorsports (American Academy of Pediatrics, 2000; U.S. Consumer Product Safety Commission, 2010), studies are needed to evaluate whether rates of motorsports participation, as well as accidents resulting from motorsporting, differ among pre- and early-adolescents with and without childhood ADHD.
Contrary to our hypothesis, impulsivity persisting into adolescence/young adulthood was not directly correlated with frequent motorsporting. It may be that a related but distinct facet of disinhibition, sensation seeking, is more directly linked with engagement in motorsports. Sensation seeking has been shown to be positively associated with deviant (e.g., alcohol abuse; Hittner & Swickert, 2006) and non-deviant forms of risk-taking (e.g., risky sports; Zuckerman, 2007). Sensation seeking, as opposed to impulsivity, has also been shown to increase with age into adolescence (Pedersen, Molina, Belendiuk, & Donovan, 2012). Indeed, it may be that individuals with childhood ADHD have increased thrill-seeking tendencies that are not fully dependent upon persistent impulsivity, as suggested by the fact that the direct effect of childhood ADHD on frequent motorsporting was only partially mediated. As sensation seeking data were not available for us to test this hypothesis, we recommend that future studies examine sensation seeking as a potential mediator of prospective associations between childhood ADHD and risky driving behaviors, including motorsport activities.
On the other hand, CD/ASP diagnosis in adolescence/young adulthood was both directly and indirectly (through heavy drinking) associated with frequent motorsporting. Individuals with ADHD histories and CD/ASP may be more likely to engage in motorsports because those who worry less about conventionality/rules have increased likelihood of involvement in thrill-seeking activities that may include illegal behavior (e.g., road racing). Youth with childhood ADHD who develop CD/ASP are more likely to engage in other risk-taking behaviors as adolescents and young adults, such as other forms of unsafe driving (e.g., tailgating; Barkley et al., 1993). Still, as individuals with ADHD and comorbid conduct problems tend to have more severe and persistent symptoms of behavioral disinhibition than those with ADHD-only (Waschbusch, 2002), it is unclear whether CD/ASP would continue to mediate this effect if sensation-seeking was controlled. Moreover, as there are individual differences in the developmental trajectory and expression of conduct problems (e.g., childhood- vs. adolescent-onset, presence vs. absence of callous-unemotional traits; Frick, 2012), future studies should consider examining conduct problems as a multi-dimensional, rather than a dichotomous, risk factor for frequent motorsporting.
Our findings suggested the potential importance of heavy drinking in a behavioral risk profile that includes frequent motorsporting. Though excessive drinking may have identified individuals likely to participate in multiple risky behaviors, it also may have been a proxy measure for related constructs that better explain involvement in motorsports. For example, research has shown that sensation seekers often abuse alcohol (Curcio & George, 2011; Quinn, Stappenbeck, & Fromme, 2011) and engage in multiple forms of risk-taking (Zuckerman, 2007). Alternatively, heavy drinking during this developmental window may contribute to risk for additional thrill-seeking by decreasing expectations of negative outcomes of these activities (Fromme et al., 1997). Examinations of mechanisms underlying associations between heavy alcohol use and risky driving-related behavior, as well as studies of motorsporting accidents and injuries among those reporting multiple risk behaviors (e.g., heavy drinking and sky diving), seem warranted.
We did not measure alcohol consumption while engaging in motorsporting activities. For this reason, we cannot conclude that alcohol directly contributed to the decision to participate in motorsports. However, studies suggest that alcohol impairs driving skill significantly (e.g., leaving lane, delayed reaction time, speeding; Linnoila, Stapleton, Lister, Guthrie, & Eckardt, 1986; National Institute on Alcohol Abuse and Alcoholism, 1996) and that individuals with ADHD appear to be more disinhibited by the effects of alcohol (Weafer, Fillmore, & Milich, 2009), including when driving (Weafer, Camarillo, Fillmore, Milich, & Marczinski, 2009). In light of these preliminary findings, and the potential safety risks of motorsporting under the influence of alcohol, future investigations should assess whether histories of ADHD and/or conduct problems increase risk of motorsporting while inebriated.
To our knowledge, no studies have assessed links between motorsports involvement and problematic driving behaviors. The relative lack of research in this area is surprising given the typicality and widespread acceptance of risky motorsport activities. Our exploratory analyses revealed significant connections between motorsporting, citations and accidents, and alcohol-affected driving outcomes. As such, adolescents or young adults who are risk-takers off the road also take greater risks on the road. Preliminary tests also indicated that frequent motorsporting was associated with unsafe and alcohol-influenced driving among adolescents and young adults with childhood ADHD, but not among those without ADHD histories. Frequent motorsporters with childhood ADHD may have vigilance and inhibitory control problems behind the wheel of any vehicle, and therefore may be at increased risk of accidents while on their ATV relative to those without childhood ADHD. That said, comparisons between those with and without ADHD histories should be interpreted with some degree of caution because ADHD status was not formally tested as a moderator of the association between frequent motorsporting and unsafe or alcohol-influenced driving. The small number of participants without childhood ADHD who reported frequent involvement in motorsport activities and unsafe or alcohol-influenced driving limited our power to detect significant interactions.
The present study has several strengths (e.g., large group of adolescents and young adults rigorously diagnosed with ADHD in childhood using evidence-based practices), yet certain factors limit the generalizability of our findings. First, because reports of impulsivity, CD/ASP, and heavy drinking were collected at the same time as reports of motorsports, we cannot conclude that these mediators preceded the motorsporting. Additional research that tracks the unfolding of these behaviors over time would clarify the temporal ordering of these associations. Second, our assessment of conduct problems among the 16 and 17 year-olds did not include a measure of self-reported antisociality. Our findings may have differed if conduct problems unobserved by parents or teachers were recounted by the adolescents. Third, this study describes data collected from 16–25 year-old males. Studies are needed that investigate driving-related risky behavior among younger and older men or women as they may uncover different results. Fourth, acknowledging the tendency for individuals with ADHD to under-report their symptoms and impairment (e.g., Hoza, Murray-Close, Arnold, Hinshaw, & Hechtman, 2010; Knouse et al., 2005), rates of traffic accidents, tickets and heavy drinking may have been under-reported. Fifth, our assessment of motorsporting is somewhat limited. Future studies should not only assess rates of injuries and substance use in the context of motorsporting, but also motives for motorsporting (e.g., recreational vs. occupational use), circumstances of involvement (e.g., solo, with peers, competition), and safety precautions taken (e.g., rate of helmet use). Finally, this sample includes adolescents and young adults with childhood ADHD who received intensive, short-term treatment for ADHD as children (Pelham et al., 2005). Our results could vary from those found with individuals diagnosed with, but not treated for, ADHD in childhood or those diagnosed with ADHD in adulthood as they may have less severe functional deficits (e.g., Barkley et al., 2008).
This study contributes to an emerging evidence base highlighting the likelihood of adolescents and young adults with childhood ADHD to engage in risk-taking. Due to their driving skill deficiencies and proclivity for thrill-seeking, adolescent and young adult motorsporters with ADHD histories may be prone to more accidents and injuries which, if prevented, could lessen their medical costs and/or costs to society (in the form of SSI). To this end, components of psychosocial interventions (Fabiano et al., 2011) and stimulant medications (Biederman et al., 2012; Cox et al., 2008) found to reduce automobile driving misbehavior among adolescents and young adults with ADHD should be investigated as potentially useful methods to curb risks associated with frequent motorsporting. Targeting injury prevention programs for those with persisting impulsivity, comorbid conduct problems and heavy drinking tendencies may be especially important. We hope this work draws the attention of researchers to continue studying risk-taking among individuals with childhood ADHD, with the ultimate goal of developing and disseminating safety or injury-prevention strategies for those who are most at risk.
Acknowledgments
Grants from the National Institute on Alcohol Abuse and Alcoholism (AA011873 and AA00202) and the National Institute on Drug Abuse (DA12414), awarded to Drs. Brooke Molina and William Pelham, funded the Pittsburgh ADHD Longitudinal Study, which was the data source for this project. Portions of this study were presented at the 2008 Joint RSA/ISBRA Scientific Conference, Washington DC.
References
- American Academy of Pediatrics All-terrain vehicle injury prevention: Two-, three-, and four-wheeled unlicensed motor vehicles. Pediatrics. 2000;105:1352–1354. doi: 10.1542/peds.105.6.1352. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Ed. Author; Washington, DC: 1994. [Google Scholar]
- American Psychiatric Association Proposed revisions to 314.0X Attention Deficit/Hyperactivity Disorder. 2010 www.DSM5.org.
- Arnett JJ. Young Adulthood: The Winding Road from the Late Teens through the Twenties. Oxford University Press; New York: 2004. [Google Scholar]
- August GJ, Winters KC, Realmuto GM, Fahnhorst T, Botzet A, Lee S. Prospective study of adolescent drug use among community samples of ADHD and Non-ADHD participants. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:824–832. doi: 10.1097/01.chi.0000219831.16226.f8. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Driving impairment in teens and adults with attention-deficit/hyperactivity disorder. Psychiatric Clinics of North America. 2004;27:233–260. doi: 10.1016/S0193-953X(03)00091-1. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3rd ed. Guilford Press; New York, NY, US: 2006. [Google Scholar]
- Barkley R, Fischer M, Edelbrock C, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barkley R, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, Dupaul GJ, Shelton TL. Driving-related risks and outcomes of attention-deficit hyperactivity disorder in adolescents and young adults: A 3- to 5-year follow-up survey. Pediatrics. 1993;92:212–218. [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. The Guilford Press; New York: 2008. [Google Scholar]
- Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98:1089–1095. [PubMed] [Google Scholar]
- Biederman J, Fried R, Hammerness P, Surman C, Mehler B, Petty CR, Faraone SV, Miller C, Bourgeois M, Meller B, Godfrey KM, Reimer B. The effects of lisdexamfetamine dimesylate on the driving performance of young adults with ADHD: A randomized, double-blind, placebo-controlled study using a validated driving simulator paradigm. Journal of Psychiatric Research. 2012;46:484–491. doi: 10.1016/j.jpsychires.2012.01.007. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control Increasing prevalence of attention-deficit/hyperactivity disorder among children—United States, 2003 and 2007. Morbidity and Mortality Weekly Report. 2010;59:1439–1443. [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: Comparative meta-analyses. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:9–21. doi: 10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Moore M, Burket R, Merkel RL, Mikami AY, Kovatchev B. Rebound effects with long-acting amphetamine or methylphenidate stimulant medication preparations among adolescent male drivers with attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2008;18:1–10. doi: 10.1089/cap.2006.0141. [DOI] [PubMed] [Google Scholar]
- Curcio AL, George AM. Selected impulsivity facets with alcohol use/problems: The mediating role of drinking motives. Addictive Behaviors. 2011;36:959–964. doi: 10.1016/j.addbeh.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Donovan JE. Young adult drinking-driving: Behavioral and psychosocial correlates. Journal of Studies on Alcohol. 1993;54:600–613. doi: 10.15288/jsa.1993.54.600. [DOI] [PubMed] [Google Scholar]
- Eysenck SBG, Easting G, Pearson PR. Age norms for impulsiveness, venturesomeness, and empathy in children. Personality and Individual Differences. 1984;5:315–321. [Google Scholar]
- Fabiano GA, Hulme K, Linke S, Nelson-Tuttle C, Pariseau M, Gangloff B, Lewis K, Pelham WE, Waschbusch DA, Waxmonsky JG, Gormley M, Gera S, Buck M. The Supporting a Teen's Effective Entry to the Roadway (STEER) program: Feasibility and preliminary support for a psychosocial intervention for teenage drivers with ADHD. Cognitive and Behavioral Practice. 2011;18:267–280. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) American Psychiatric Publishing Inc.; Arlington, VA: 1997. [Google Scholar]
- Finn MA, MacDonald JD. A population-based study of all-terrain vehicle-related head and spinal injuries. Neurosurgery. 2010;67:993–997. doi: 10.1227/NEU.0b013e3181f209db. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina B, Pelham W, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Freeman N, Friedman RS, Bartholow BD, Wulfert E. Effects of alcohol priming on social disinhibition. Experimental and Clinical Psychopharmacology. 2010;18:135–144. doi: 10.1037/a0018871. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Developmental pathways to conduct disorder: Implications for future directions in research, assessment, and treatment. Journal of Clinical Child and Adolescent Psychology. 2012;41:378–389. doi: 10.1080/15374416.2012.664815. [DOI] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fromme K, Katz E, D'Amico E. Effects of alcohol intoxication on the perceived consequences of risk taking. Experimental and Clinical Psychopharmacology. 1997;5:14–23. doi: 10.1037//1064-1297.5.1.14. [DOI] [PubMed] [Google Scholar]
- Gabbe BJ, Finch CF, Cameron PA, Williamson OD. Incidence of serious injury and death during sport and recreation activities. British Journal of Sports Medicine. 2005;39:573–577. doi: 10.1136/bjsm.2004.015750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up: I. Psychiatric status. Archives of General Psychiatry. 1985;42:937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- Hittner JB, Swickert R. Sensation seeking and alcohol use: A meta-analytic review. Addictive Behaviors. 2006;31:1383–1401. doi: 10.1016/j.addbeh.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L. Time-dependent changes in positively biased self-perceptions of children with attention-deficit/hyperactivity disorder: A developmental psychopathology perspective. Development and Psychopathology. 2010;22:375–390. doi: 10.1017/S095457941000012X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack SJ, Ronan KR. Sensation seeking among high- and low-risk sports participants. Personality and Individual Differences. 1998;25:1063–1083. [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Institute of Behavioral Science, University of Colorado; Boulder, CO.: 1989. [Google Scholar]
- Knouse LE, Bagwell CL, Barkley RA, Murphy KR. Accuracy of self-evaluation in adults with attention-deficit hyperactivity disorder. Journal of Attention Disorders. 2005;8:221–234. doi: 10.1177/1087054705280159. [DOI] [PubMed] [Google Scholar]
- Krauss EM, Dyer DM, Laupland KB, Buckley R. Ten years of all-terrain vehicle injury, mortality, and healthcare costs. Journal of Trauma: Injury, Infection, and Critical Care. 2010;69:1338–1343. doi: 10.1097/TA.0b013e3181fc5e7b. [DOI] [PubMed] [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review. 2011;31:328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnoila M, Stapleton JM, Lister R, Guthrie S, Eckardt M. Effects of alcohol on accident risk. Pathologist. 1986;40:36–41. [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. Lawrence Erlbaum Associates; New York: 2008. [Google Scholar]
- Mannuzza S, Klein RG, Abikoff HB, Moulton JL. Significance of childhood conduct problems to later development of conduct disorder among children with ADHD: A prospective follow-up study. Journal of Abnormal Child Psychology. 2004;32:565–573. doi: 10.1023/b:jacp.0000037784.80885.1a. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. The American Journal of Psychiatry. 1998;155:493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- Molina BSG. Delinquency and substance use in ADHD: Adolescent and young adult outcomes in developmental context. In: Evans SW, Hoza B, editors. Attention Deficit Hyperactivity Disorder: State of the Science & Best Practices. Vol. 2. Civic Research Institute; New York: 2011. [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, Marshal MP. ADHD risk for heavy drinking and alcohol use disorder is age-specific in adolescence and young adulthood. Alcoholism: Experimental and Clinical Research. 2007;31:1–12. doi: 10.1111/j.1530-0277.2007.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Sixth Edition. Muthén & Muthén; Los Angeles, CA: 2010. [Google Scholar]
- National Highway Traffic Safety Administration . Teen Unsafe Driving Behaviors: Focus Group Final Report. US Department of Transportation; Washington, DC: 2006. [DOI] [PubMed] [Google Scholar]
- NHSDA . National Household Survey on Drug Abuse. U.S. Department of Health and Human Services, Public Health Service. Alcohol, Drug Abuse and Mental Health Administration. National Institute on Drug Abuse; Rockville, MD: 1992. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism Drinking and driving. Alcohol Alert. 1996;31 [Google Scholar]
- Pedersen SL, Molina BSG, Belendiuk KA, Donovan JE. Racial differences in the development of impulsivity and sensation seeking from childhood into adolescence and their relation to alcohol use. Alcoholism: Clinical and Experimental Research. 2012;36:1794–1802. doi: 10.1111/j.1530-0277.2012.01797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Gnagy EM, Greiner AR, Hoza B. The role of summer treatment programs in the context of comprehensive psychosocial treatment for attention-deficit/hyperactivity disorder. In: Hibbs E, Jensen P, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. 2nd ed. American Psychiatric Association; Washington, DC: 2005. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-IIIR symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Quinn PD, Fromme K. Self-regulation as a protective factor against risky drinking and sexual behavior. Psychology of Addictive Behaviors. 2010;24:376–385. doi: 10.1037/a0018547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn PD, Stappenbeck CA, Fromme K. Collegiate heavy drinking prospectively predicts change in sensation seeking and impulsivity. Journal of Abnormal Psychology. 2011;120:543–556. doi: 10.1037/a0023159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterfield JH, Faller KJ, Crinella FM, Schell AM, Swanson JM, Homer LD. A 30-year prospective follow-up study of hyperactive boys with conduct problems: Adult criminality. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(5):601. doi: 10.1097/chi.0b013e318033ff59. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P. Criterion validity of the NIMH Diagnostic Interview for Children Version 2.3 (DISC 2.3) Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Biswas A, et al. The delinquency outcomes of boys with ADHD with and without comorbidity. Journal of Abnormal Child Psychology. 2011;39:21–32. doi: 10.1007/s10802-010-9443-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straub WF. Sensation seeking among high and low-risk male athletes. Journal of Sport Psychology. 1982;4:246–253. [Google Scholar]
- Tator CH. Catastrophic Injuries in Sports and Recreation: Causes and Prevention – A Canadian Study. University of Toronto Press; Toronto, Canada: 2008. [Google Scholar]
- Thompson AL, Molina BSG, Pelham WE, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. Journal of Pediatric Psychology. 2007;32:745–759. doi: 10.1093/jpepsy/jsm002. [DOI] [PubMed] [Google Scholar]
- U.S. Consumer Product Safety Commission . 2008 Annual Report of ATV-Related Deaths and Injuries. CPSC; Bethesda, MD: 2010. [Google Scholar]
- Waschbusch Daniel A. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Weafer J, Camarillo D, Fillmore MT, Milich R, Marczinski CA. Simulated driving performance of adults with ADHD: Comparisons with alcohol intoxication. Experimental and Clinical Psychopharmacology. 2008;16:251–263. doi: 10.1037/1064-1297.16.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weafer J, Fillmore MT, Milich R. Increased sensitivity to the disinhibiting effects of alcohol in adults with ADHD. Experimental and Clinical Psychopharmacology. 2009;17:113–121. doi: 10.1037/a0015418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss G, Hechtman LT. Hyperactive Children Grown Up: ADHD in Children, Adolescents, and Adults. 2nd Ed. The Guilford Press; New York: 1993. [Google Scholar]
- White JD. Personality, temperament and ADHD: A review of the literature. Personality and Individual Differences. 1999;27:589–598. [Google Scholar]
- White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology. 1994;103:1922–1935. doi: 10.1037//0021-843x.103.2.192. [DOI] [PubMed] [Google Scholar]
- Zuckerman M. Impulsive unsocialized sensation seeking: The biological foundations of a basic dimension of personality. In: Bates JE, Wachs TD, editors. Temperament: Individual differences at the interface of biology and behavior. American Psychological Association; Washington, DC: 1994. pp. 219–255. [Google Scholar]
- Zuckerman M. Sensation seeking and risky driving, sports and vocations. In: Zuckerman M, editor. Sensation Seeking and Risky Behavior. American Psychological Association; Washington, DC: 2007. pp. 73–106. [Google Scholar]


