Abstract
Although coronary artery disease (CAD) is not common among individuals younger than 40–45 years of age, a small percentage of this age group needs to undergo surgical revascularization because of CAD. Why some people are at higher risk of developing premature CAD is not clearly known. Increased number of traditional risk factors or genetic predisposition may play significant roles in this regard.
A 22-year-old man with a negative history for all traditional risk factors except for a family history of premature CAD referred to our center due to an episode of myocardial infarction of one month’s duration. He had no congenital heart disease and no hypercoagulable state, and there was a negative history of drug abuse.
His coronary angiography showed extensive CAD. He underwent coronary artery bypass grafting and he left the hospital in good healthy condition. One year after surgery, his follow-up showed that he was symptom free and he still had no new traditional risk factor. It seems that a positive family history of premature CAD is an important and independent risk factor for developing premature CAD and individuals with this type of history should be treated more cautiously.
Keywords: Coronary artery disease, Myocardial infarction, Coronary artery bypass, Young adult, Treatment outcome
Introduction
Although individuals younger than 40 years of age account for only 3% of all patients with coronary heart disease (CHD)1 and also myocardial infarction (MI) mainly occurs in individuals older than 45 years old, the young are not completely immune from these cardiac diseases.2 The causes of MI among patients aged less than 45 years can be divided into four groups: 1) atheromatous coronary artery disease (CAD); 2) non-atheromatous coronary artery abnormalities; 3) hypercoagulable states; and 4) MI secondary to substance misuse.2 Cigarette smoking appears to be the most common risk factor for heart disease,3–5 and a positive family history of CAD (defined as the occurrence of premature CAD in a first-degree relative) is a major risk factor for MI in young individulas.6 The prevalence of a positive family history among these patients ranges from 14% to 69%.1 Siblings of a young patient with MI have up to a tenfold increased risk of developing CAD,7 and approximately half of young patients with MI have single-vessel coronary disease.4
We herein introduce a very young patient with extensive premature CAD without congenital heart abnormality, hypercoagulable state, substance misuse, and traditional risk factors (except for a positive family history of premature CAD) who underwent coronary artery bypass grafting (CABG) at Tehran Heart Center.
Case Presentation
A 22-year-old man was referred to our center for CABG. The patient’ illness had started one month before admission with an onset of acute MI. His past medical history did not present any positive clue of CHD. He was 71 kg in weight and 180 cm in height, which meant that his body mass index (BMI) was in safe limits (21.91 kg/m2). Risk factors such as diabetes, smoking, obesity, and dyslipidemia were not seen in his history, but his family history for CHD was positive. His father had died at 38 years of age because of sudden cardiac death and his mother was a known case of ischemic heart disease. The patient had no history of the use of legal or recreational drugs, and his family history was negative for any hereditary or metabolic disorders.
The results of laboratory tests conducted on admission were as follows: normal complete blood count (white blood cell [WBC] = 6600 / mm3, red blood cell [RBC] = 5.39 × 106 / mm3, hemoglobin [Hgb] = 16.1 mgr/dl, and hematocrit [Hct] = 45.7%); normal hepatic transaminases (alanine aminotransferase [ALT] = 29 IU/L and aspartate aminotransferase [AST] = 20 IU/L); normal-range blood serum electrolytes; total cholesterol of 126 mg/dl; triglyceride of 92 mg/dl; high-density lipoprotein (HDL) of 26 mg/dl; low-density lipoprotein (LDL) of 84 mg/dl; very low-density lipoprotein (VLDL) of 18.4 mg/dl; LDL/HDL ratio of 3.2; and cholesterol/HDL ratio of 4.8. Additionally, creatine kinase MB (CKMB) and troponin on the day before surgery were 5.41 ng/ml and less than 3 ng/l, respectively, and coagulative tests showed a normal span. The patient’s blood group and Rh was O positive.
On physical examination, the patient’s blood pressure was 105/80 mmHg with a heart rate of 100 beats per minute. In heart auscultation, S1 and S2 were normal and the respiratory system was clear on examination. Preoperative electrocardiography revealed nonspecific changes in T wave.
Echocardiography demonstrated a left ventricular end diastolic volume (LDEDV) of 96 cc, left ventricular end systolic volume (LVESV) of 48 cc, and ejection fraction (EF) of 42%. Furthermore, there was an abnormal septal motion, hypokinesia, in the septal wall and the mid-portion of the anteroseptal wall. The heart valves had mild mitral regurgitation and trivial tricuspid regurgitation.
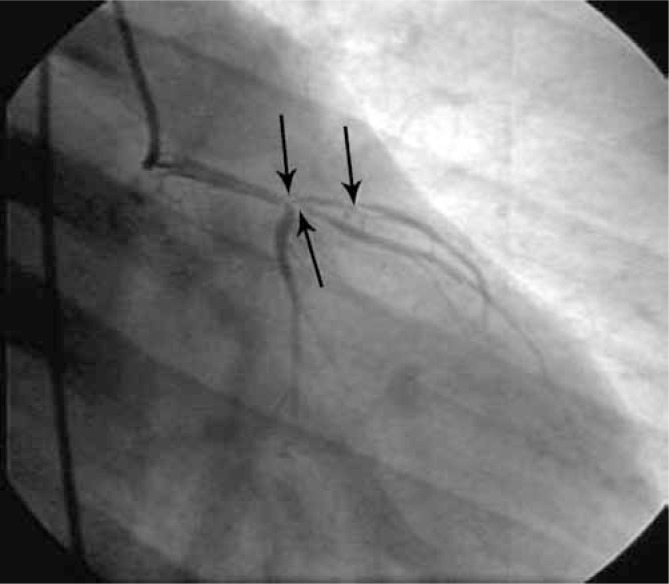
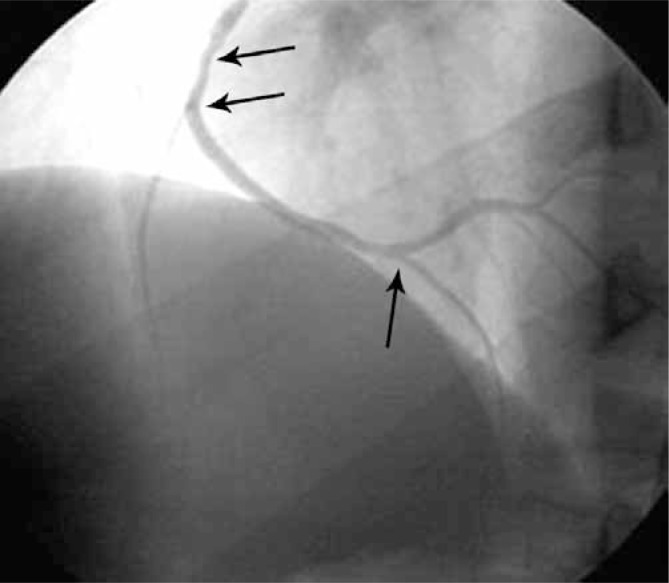
Angiography demonstrated that the left main coronary artery was 70% diseased. Three other coronary arteries, i.e. the left anterior descending artery, diagonal 1 artery, and right coronary artery, had severe stenosis (Figures 1 & 2). There was also ostial stenosis in the ramus intermedius. The left circumflex coronary artery was patent, and the EF based on angiography was 45%.
Figure 1.
Right anterior oblique coronary angiography view of the patient. The arrows point to the stenotic sites, including the distal stenosis of the left main coronary artery, severe ostial stenosis of the left anterior descending artery, ramus intermedius artery, and left circumflex artery
Figure 2.
Left anterior oblique coronary angiography view of the patient, showing multiple stenosis at mid and distal parts of the right coronary artery (arrows)
The patient underwent CABG without any complication. Two days after surgery, laboratory tests revealed CKMB of 4.74 ng/ml and troponin of 437.7 mcg/l.
On postoperative electrocardiography, the ST segment was slightly elevated in leads II, III, AVF, V5, and V6. The patient was discharged from the hospital in good healthy condition five days after surgery. Postoperative follow-up of the patient, conducted one year later, showed that he was still symptom free and that he had no traditional risk factors other than a positive family history of premature CAD. Additionally, he was on stating β blocker and amino salicylic acid.
Discussion
CHD represents the leading cause of death in adults. Fortunately, its incidence is not common in individuals younger than 45 years of age. However, the disease carries significant morbidity, psychological effects, and financial constraints for the person and the family when it occurs at a young age. The protection offered by young age has been gradually eroded by the increased prevalence of risk factors for CHD in adolescents such as smoking, obesity, and lack of physical activity.2 The risk factors of CAD are no different between individuals younger or older than 40 years old, but the increased incidence of a positive family history of CAD and lipid abnormalities in younger individuals with early onset coronary atherosclerosis renders them unique.8 About 40% of young CAD patients have a first-degree relative with premature atherosclerosis.9 Although for a long time a family history of ischemic heart disease has been deemed a main risk factor a risk factor for developing CAD in patients,10, 11 there are two different viewpoints about this concept: some researchers strongly believe that dominancy of a family history of CAD in a family is accompanied by other risk factors like hypertension and hyperlipidemia12, 13 whereas others maintain that a family history is an independent risk factor and its presence is not necessarily related to the other factors.14 In our patient, the only detectable traditional risk factor was a positive family history of premature CAD. He was a normotensive, non-diabetic, non-smoking, and non-hyperlipidemic patient. Also, he had no congenital heart disease and hypercoagulable state, and nor was he a drug abuser. Emotional stress and aggressive nature in the young age group are thought to be related to the prevalence of CAD.15 The CARDIA study offered an explanation for the association between aggression and CHD mortality.16 Acute physical or emotional stress increases shear forces and thus causes a previously non-significant plaque to rupture, triggering acute MI.17
The classic presentation of worsening angina culminating in MI is rare in younger patients. The first onset of angina that rapidly progresses to fully evolved MI is often the case in patients less than 45 years of age.2 In our patient, MI was the first presentation of his coronary problems too. As secondary prevention, antiplatelet agents such as Aspirin and Clopidogrel should be used as per the guidelines for adults. Warfarin is necessary in patients with recurrent ischemic events. Statins should invariably be prescribed in all patients with MI insofar as their clinical effects extend beyond lipid lowering. Statins are believed to stabilize plaques in patients with atheromatous CHD, thereby improving their outcome and reducing recurrent events.2 In patients with established MI, exercise stress testing could well be a useful tool for risk stratification. Echocardiographic assessment of the LV function should be done in all patients. However, angiographic assessment has a defining and leading role for deciding about the next step in a patient management program.2 It is advisable that CABG be offered to patients with triple-vessel disease, complex coronary artery abnormalities, and impaired LV function. CABG is believed to confer better results in young patients: survival rates of 92% at five years and 86% at ten years, which are significantly better than 75% and 58% for patients over 65 years old.18, 19
Conclusion
A positive family history of CAD can be deemed a very important risk factor for developing premature CAD and patients with this predisposing risk factor should be treated more conservatively and diagnostic measures must be considered more frequently when there is a possibility of premature CAD.
References
- 1.Jalowiec DA, Hill JA. Myocardial infarction in the young and in women. Cardiovasc Clin. 1989;20:197–206. [PubMed] [Google Scholar]
- 2.Egred M, Viswanathan G, Davis GK. Myocardial infarction in young adults. Postgrad Med J. 2005;81:741–745. doi: 10.1136/pgmj.2004.027532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbash GI, White HD, Modan M, Diaz R, Hampton JR, Heikkila J, Kristinsson A, Moulopoulos S, Paolasso EA, Van der Werf T. Acute myocardial infarction in the young--the role of smoking. The Investigators of the International Tissue Plasminogen Activator/Streptokinase Mortality Trial. Eur Heart J. 1995;16:313–316. [PubMed] [Google Scholar]
- 4.Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107:254–261. doi: 10.1016/s0002-9343(99)00218-1. [DOI] [PubMed] [Google Scholar]
- 5.Hong MK, Cho SY, Hong BK, Chang KJ, Mo-Chung I, Hyoung-Lee M, Wook-Lim S, Kwon HM, Jang YS, Chung NS. Acute myocardial infarction in the young adults. Yonsei Med J. 1994;35:184–189. doi: 10.3349/ymj.1994.35.2.184. [DOI] [PubMed] [Google Scholar]
- 6.Farmer JA, Gotto AM. Dyslipidemia and other risk factors for coronary artery disease. In: Bonow RO, Mann DL, Zipes DP, Libby P, editors. Heart Disease: A Textbook of Cardiovascular Medicine. 5th ed. Philadelphia: WB Saunders; 1997. pp. 1126–1160. [Google Scholar]
- 7.Cremer P, Nagel D, Mann H, Labrot B, Müller-Berninger R, Elster H, Seidel D. Ten-year follow-up results from the Goettingen Risk, Incidence and Prevalence Study (GRIPS). I. Risk factors for myocardial infarction in a cohort of 5790 men. Atherosclerosis. 1997;129:221–230. doi: 10.1016/s0021-9150(96)06030-3. [DOI] [PubMed] [Google Scholar]
- 8.Samuels LE, Sharma S, Kaufman MS, Morris RJ, Brockman SK. Coronary artery bypass grafting in patients in their third decade of life. J Card Surg. 1996;11:402–407. doi: 10.1111/j.1540-8191.1996.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen L, Chester M, Kaski JC. Clinical factors and angiographic features associated with premature coronary artery disease. Chest. 1995;108:364–369. doi: 10.1378/chest.108.2.364. [DOI] [PubMed] [Google Scholar]
- 10.Herapath CE, Perry CB. The coronary arteries in a case of familial liability to sudden death. Br Med J. 1930;1:685–687. doi: 10.1136/bmj.1.3614.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas CB, Cohen BH. The familial occurrence of hypertension and coronary artery disease, with observations concerning obesity and diabetes. Ann Intern Med. 1955;42:90–127. doi: 10.7326/0003-4819-42-1-90. [DOI] [PubMed] [Google Scholar]
- 12.Rissanen AM, Nikkilä EA. Coronary artery disease and its risk factors in families of young men with angina pectoris and in controls. Br Heart J. 1977;39:875–883. doi: 10.1136/hrt.39.8.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rissanen AM, Nikkilä EA. Aggregation of coronary risk factors in families of men with fatal and non-fatal coronary heart disease. Br Heart J. 1979;42:373–380. doi: 10.1136/hrt.42.4.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Snowden CB, McNamara PM, Garrison RJ, Feinleib M, Kannel WB, Epstein FH. Predicting coronary heart disease in siblings-a multivariate assessment The Framingham Heart Study. Am J Epidemiol. 1982;115:217–222. doi: 10.1093/oxfordjournals.aje.a113293. [DOI] [PubMed] [Google Scholar]
- 15.Iribarren C, Sidney S, Bild DE, Liu K, Markovitz JH, Roseman JM, Matthews K. Association of hostility with coronary artery calcification in young adults. JAMA. 2000;283:2546–2551. doi: 10.1001/jama.283.19.2546. [DOI] [PubMed] [Google Scholar]
- 16.Scherwitz LW, Perkins LL, Chesney MA, Hughes GH, Sidney S, Manolio TA. Hostility and health behaviors in young adults: the CARDIA Study. Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol. 1992;136:136–145. doi: 10.1093/oxfordjournals.aje.a116480. [DOI] [PubMed] [Google Scholar]
- 17.Fournier JA, Sánchez A, Quero J, Fernández-Cortacero JA, González-Barrero A. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. 1996;19:631–636. doi: 10.1002/clc.4960190809. [DOI] [PubMed] [Google Scholar]
- 18.Ng WK, Vedder M, Whitlock RM, Milsom FP, Nisbet HD, Smith WM, Kerr AR, French JK. Coronary revascularisation in young adults. Eur J Cardiothorac Surg. 1997;11:732–738. doi: 10.1016/s1010-7940(97)01153-6. [DOI] [PubMed] [Google Scholar]
- 19.Floten HS, Ahmad A, Swanson JS, Wood JA, Chapman RD, Fessler CL, Starr A. Long-term survival after postinfarction bypass operation: early versus late operation. Ann Thorac Surg. 1989;48:757–762. doi: 10.1016/0003-4975(89)90666-8. [DOI] [PubMed] [Google Scholar]