Abstract
Aims
This paper examines differences in cardiovascular disease risk factor control among racial/ethnic minorities (Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, Hispanic/Latino, Black/African Americans) with type 2 diabetes compared to Non-Hispanic Whites with type 2 diabetes in an insured, outpatient setting.
Methods
A three-year, cross-sectional sample of 15,826 patients with type 2 diabetes was studied between 2008 and 2010. Goal attainment rates for three cardiovascular disease risk factors (HbA1c, BP, LDL) were estimated. Logistic regression was used to determine the association between patient characteristics and control of risk factors.
Results
Only one fifth (21.1%) of patients achieved simultaneous goal attainment (HbA1c, BP, LDL). After adjustment for patient characteristics and treatment, Black/African American women and men, and Filipino and Hispanic/Latino men were significantly less likely to simultaneously achieve all three goals, compared to Non-Hispanic Whites. Of the three goals, patients were more likely to achieve HbA1c goals (68.7%) than BP (45.7%) or LDL (58.5%) goals. Racial/ethnic differences were more apparent in risk factors that were under better control (i.e. HbA1c).
Conclusions
Cardiovascular risk factor control in type 2 diabetes is suboptimal, even in an insured population. Special attention may be required for specific racial/ethnic/gender groups.
Keywords: Race/ethnicity, Primary prevention, Cardiovascular diseases, Disparities, Type 2 diabetes
1. Introduction
Over 20 million Americans are diagnosed with type 2 diabetes (Centers for Disease Control and Prevention, National Center for Health Statistics, 2009), and that number is projected to triple over the next couple of decades (Boyle, Thompson, Gregg, Barker, & Williamson, 2010). This increase is due in large part to the growing number of high-risk racial/ethnic minorities in the U.S. The Asian and Hispanic/Latino American populations are expected to see the most growth, doubling in size between 2010 and 2050 to approximately 9% and 30% of the U.S. population respectively (U.S. Census Bureau, 2009). Asian, Hispanic/Latino, and Black/African Americans are all more likely to develop type 2 diabetes than Non-Hispanic Whites (NHWs) (Choi, Chow, Chung, & Wong, 2011; Cowie et al., 2010; Wang et al., 2011). Among the Asian American subgroups (Asian Indian, Chinese, Filipino, Korean, Japanese, and Vietnamese), Asian Indians and Filipinos have the highest rates of types 2 diabetes (Choi et al., 2011; Wang et al., 2011).
Patients with type 2 diabetes have double the risk of developing and dying from heart disease (American Diabetes Association, 2010; Centers for Disease Control and Prevention, National Center for Health Statistics, 2011), and control of cardiovascular risk factors is critical for primary and secondary prevention of heart disease. While some improvements have been made over the past few decades in controlling the three major cardiovascular disease risk factors (HbA1c, BP, and LDL) (Ford, 2011), research suggests that racial/ethnic disparities exist (Chatterji, Joo, & Lahiri, 2012; Malik, Lopez, Chen, Wu, & Wong, 2007). Disparities in risk factor control may be more prominent for risk factors that are at better control, compared to other risk factors. On average, control of HbA1c has been better, compared to control of BP and LDL (Chatterji et al., 2012; Cheung et al., 2006; Jackson, Edelman, & Weinberger, 2006; McWilliams, Meara, Zaslavsky, & Ayanian, 2009).
Despite the growing number of racial/ethnic minorities in the U.S. and their increased risk for type 2 diabetes, knowledge of cardiovascular risk factor control for these populations is inadequate. The majority of research regarding cardiovascular risk factor control has focused on Black/African Americans, while Asian Americans have not been studied. Previous studies have primarily utilized National Health Examination and Nutrition Survey (NHANES) data and are limited by self-report, exclusion of some racial/ethnic groups (Asian American) and subgroups (e.g., Asian Indian, Chinese), (Ford, 2011; Malik et al., 2007; Saydah, Fradkin, & Cowie, 2004) and variable access to healthcare for the participants. There is a need to examine whether cardiovascular risk factor control within a healthcare system, where all patients have access and regularly access the clinic for visits, is significantly better than national cardiovascular risk factor control rates reported using NHANES data. The objective of our study was to examine differences in cardiovascular disease risk factor control (HbA1c, BP, and LDL), and patient characteristics associated with better or worse risk factor control, using electronic health record data in a diverse patient population, with type 2 diabetes in a multi-specialty, insured, outpatient setting.
2. Subjects, materials and methods
2.1. Setting
The study was conducted in a mixed-payer, outpatient health care organization serving approximately 600,000 active patients, in the San Francisco Bay Area of Northern California. The demographic characteristics of the clinical population are similar to those of residents in the underlying service area in Northern California (Alameda, San Mateo and Santa Clara counties) with respect to race/ethnicity and age distribution, but the clinical population has a slightly higher proportion of women, NHWs and Asian Americans, and a lower proportion of Hispanic/Latino and Black/African Americans. Among Asian Americans, the representation of Koreans and Vietnamese in the clinic is disproportionately lower when compared to the service area. The patient population is insured with 58% preferred provider organization (PPO), 23% health maintenance organization (HMO), 16% Medicare, 2% self-payer, and 1% Medicaid and thus under-represents the medically underserved. Accordingly, access to care is unlikely to confound subgroup comparisons.
2.2. Study design
A three-year, cross-sectional sample of active patient electronic health records (EHR) was studied from January 1, 2008 to December 31, 2010. Active patients aged 35 years or older with type 2 diabetes, and no diagnosis of type 1 diabetes (defined as physician recorded International Classification of Diseases, version 9 (ICD-9) codes 250.X1-250.X3) were included in the analyses. Patients with type 2 diabetes were identified using at least one physician recorded diagnosis code (ICD-9 codes 250.X0-250.X2, 89.3%), any two abnormal laboratory values (HbA1c≥6.5%, fasting blood glucose ≥126 mg/dL, random blood glucose≥200 mg/dL, or oral glucose tolerance test≥200 mg/dL) according to American Diabetes Association (American Diabetes Association, 2010) guidelines (additional 6.2%) or use of any anti-diabetic medications (oral agents, insulin and non-insulin injectables, additional 4.5%). The formulary of anti-diabetic medications was selected by expert physician review (LP).
Over 86% of patients with type 2 diabetes in our population had HbA1c, BP and LDL all measured at least once during the observation period, ranging from 84.1% for NHWs to 91.1% for Black/African Americans. Data on patient demographics, anthropometric measures, physician diagnoses, laboratory results and prescription medications were extracted from the EHR. Patients identified as Asian (Asian Indian, Chinese, Filipino, Japanese, Korean or Vietnamese), Hispanic/Latino, Black/African Americans or Non-Hispanic Whites (NHWs) through self- report (Palaniappan, Wong, Shin, Moreno, & Otero-Sabogal, 2009) (76%) or by names (Wong, Palaniappan, & Lauderdale, 2010) (24%) were included in analyses. Results were presented for Asian Americans as an aggregated group and across 6 individual Asian American racial/ethnic subgroups, Hispanic/Latino and Black/African Americans, all compared to NHWs. All data sets analyzed by the research team were de-identified according to the Health Insurance Portability and Accountability Act (HIPAA) standard, approved by the Palo Alto Medical Foundation Institutional Review Board (PAMF IRB).
Goal attainment for the three cardiovascular risk factors was the main outcome of interest. We defined goal attainment by the American Diabetes Association (American Diabetes Association, 2010) guidelines: (1) HbA1c<7.0% (2) systolic BP<130 mmHg and diastolic BP<80 mmHg (3) LDL<100 mg/dL. We also defined simultaneous goal attainment as achieving HbA1c, BP and LDL goals during the observation period. We used the last available value for all goal attainment analyses. Patients who did not have at least one HbA1c, BP and LDL value were excluded from the simultaneous goal attainment analysis. We also examined the distance from goal for the patients who did not achieve their goal attainment as the absolute value difference between their risk factor values and target goals.
The following clinical patient characteristics were identified: patient race/ethnicity, age, primary insurance (preferred provider organization [PPO], health maintenance organization [HMO], and others), number of total primary care office visits during the study period, weight status based on BMI values (in kg/m2, underweight: <18.5, normal weight: ≥18.5 and <25, overweight: ≥25 and <30, and obese: ≥30) (National Heart Lung and Blood Institute, the National Institute of Diabetes and Digestive and Kidney Diseases, 1998), smoking status (self-reported), and treatment status (anti-diabetic medication usage for HbA1c management, anti-hypertensive medications for BP management and lipid modifying agents for LDL control). Drug treatment was identified through physician prescriptions in the electronic health record system. If one lab test was taken between the start and end date of a medication order, then the measurement (HbA1C, BP, LDL) was regarded as on treatment.
2.3. Statistical methods
The analyses sought to estimate the unadjusted and age- and sex-adjusted goal attainment rates for the three cardiovascular disease risk factors and investigate the patient characteristics associated with better or worse risk factor control. Patient demographics, clinical characteristics, and treatment rates were compared based on non-overlapping Wilson confidence intervals or non-parametric Wilcoxon tests. Age–sex standardized goal attainment rates were calculated using direct standardization to the PAMF NHW population. Broad age categories (35–44, 45–54, 55–64, 65–74, 75+ (years)), and sex categories (male vs. female) were used to achieve stratum-specific rates for direct standardization. Odds ratios calculated from logistic regression were employed in the multivariate analysis to determine the relative association of goal attainment with multiple patient characteristics, including race/ethnicity, age, primary insurance (PPO, HMO, Medicare, and others), frequency of office visits, weight status, self-reported smoking status and treatment status. Regression models were calculated separately for women and men with goal attainment as the outcome. NHW was the referent group in all models. For all analyses, statistical significance was determined at P<0.05, and 95% confidence intervals are reported when appropriate. Statistical analyses were performed using SAS 9.3 (Cary, NC).
3. Results
A total of 15,826 patients with type 2 diabetes (52.6% Non-Hispanic Whites, 32.9% Asian, 11.7% Hispanic/Latino, and 2.8% Black/African Americans) out of 210,870 total active patients over age 35 were included in the analysis (Table 1). Asian, Hispanic/Latino, and Black/African Americans, were younger compared to NHWs. All Asian American subgroups had significantly lower BMI values, whereas Hispanic/Latino and Black/African Americans had higher BMI values, compared to NHWs. Among the Asian American subgroups, Filipinos exhibited the highest mean HbA1c and systolic BP values, while Vietnamese had the lowest values. Black/African Americans had higher mean HbA1c, BP and LDL values, and Hispanic/Latino Americans had higher HbA1c and LDL values, compared to NHWs. Care utilization differed, with fewer office visits for Asian and Hispanic/Latino Americans, and more office visits for Black/African Americans, compared to NHWs over the three year study period.
Table 1.
Characteristics of type 2 diabetes patients aged 35 years or older (N=15,826).
| Non-hispanic whites | Asians (all) | Asian indians | Chinese | Filipinos | Japanese | Koreans | Vietnamese | Black/africans | Hispanic/latinos | |
|---|---|---|---|---|---|---|---|---|---|---|
| N | 8323 | 5199 | 1809 | 1615 | 1065 | 416 | 133 | 161 | 449 | 1855 |
| Women (%) | 46.0% | 44.7% | 34.8%* | 47.3% | 54.6%* | 51.2% | 45.9% | 46.0% | 57.9%* | 50.8%* |
| Age, y, mean (SD) | 63.0 (13.5) | 57.0 (14.1)* | 50.8 (12.5)* | 61.8 (14.0)* | 57.7 (12.5)* | 65.0 (14.4)* | 55.2 (14.1)* | 56.0 (13.1)* | 58.3 (12.2)* | 57.7 (13.6)* |
| BMI | ||||||||||
| BMI (mean, SD) | 31.9 (7.0) | 26.9 (4.7)* | 27.3 (4.5)* | 25.8 (4.5)* | 27.9 (5.0)* | 27.6 (5.3)* | 26.2 (4.0)* | 25.3 (4.0)* | 32.9 (7.4)* | 32.3 (6.6)* |
| Underweight (%) | 0.5% | 0.8% | 0.6% | 1.4%* | 0.4% | 0.7% | 0.8% | 1.2% | 0.4% | 0.1%* |
| Normal weight (%) | 11.3% | 33.4%* | 30.6%* | 41.4%* | 25.5%* | 28.8%* | 32.3%* | 48.4%* | 9.1% | 8.0%* |
| Overweight (%) | 26.6% | 36.9%* | 39.7%* | 33.1%* | 39.7%* | 33.4%* | 45.1%* | 28.0% | 26.9% | 28.2% |
| Obese (%) | 47.7% | 18.6%* | 20.6%* | 12.9%* | 24.6%* | 22.4%* | 11.3%* | 9.3%* | 56.3%* | 53.3%* |
| Missing BMI (%) | 13.9% | 10.3%* | 8.5%* | 11.3%* | 9.8%* | 14.7% | 10.5% | 13.0% | 7.1%* | 10.4%* |
| Last available measure (mean, SD) | ||||||||||
| HbA1c | 6.8 (1.4) | 6.9 (1.2)* | 6.9 (1.2)* | 6.7 (1.0) | 7.1 (1.4)* | 6.9 (1.4)* | 6.9 (1.1)* | 6.8 (1.1) | 7.2 (1.7)* | 7.2 (1.7)* |
| diastolic BP | 73.4 (10.7) | 73.4 (10.6) | 74.3 (9.9)* | 71.9 (10.8)* | 74.3 (10.8)* | 73.2 (11.1) | 74.8 (11.6) | 71.6 (9.9)* | 76.3 (10.2)* | 74.1 (10.5)* |
| systolic BP | 128.1 (16.5) | 124.5 (16.5)* | 122.8 (15.8)* | 124.0 (16.8)* | 128.1 (16.5) | 126.7 (15.8) | 122.1 (16.8)* | 122.1 (17.5)* | 130.6 (16.5)* | 126.9 (15.9)* |
| LDL | 96.6 (34.0) | 97.1 (32.4)* | 98.1 (31.1)* | 95.4 (32.4) | 98.3 (34.5) | 95.1 (33.2) | 97.4 (32.0) | 101.2 (31.3)* | 102.7 (35.7)* | 100.1 (33.3)* |
| Utilization (mean, SD) | ||||||||||
| Number of office visits | 17.3 (16.2) | 13.1 (11.8)* | 11.1 (10.2)* | 14.0 (12.0)* | 14.3 (12.5)* | 15.7 (14.1) | 12.4 (12.3)* | 11.7 (10.6)* | 18.6 (15.5)* | 15.6 (14.1)* |
| Number of primary care/endocrinology visits | 9.1 (7.6) | 8.1 (5.9)* | 7.1 (5.0)* | 8.5 (6.3) | 8.9 (6.3) | 8.9 (6.9) | 7.2 (5.0)* | 7.3 (5.2)* | 10.2 (7.5)* | 9.4 (7.2)* |
| Primary Insurance | ||||||||||
| PPO | 65.4% | 66.4% | 72.3%* | 68.2% | 56.6%* | 58.4%* | 63.9% | 69.6% | 54.6%* | 54.7%* |
| HMO | 32.1% | 30.1% | 22.1%* | 28.4%* | 42.0%* | 40.6%* | 33.1% | 29.8% | 42.3%* | 41.3%* |
| Other | 1.1% | 2.0%* | 2.7%* | 2.5%* | 0.9% | 0.0% | 1.5% | 0.0% | 2.0% | 2.0%* |
| Last available Smoking Status (%) | ||||||||||
| Ever | 37.0% | 20.8%* | 16.7%* | 16.7%* | 30.1%* | 28.4%* | 33.1% | 16.8%* | 39.2% | 32.5%* |
| Never | 52.4% | 72.0%* | 75.7%* | 76.2%* | 63.7%* | 63.5%* | 59.4% | 76.4%* | 56.1% | 59.7%* |
| Missing | 10.6% | 7.2%* | 7.6%* | 7.1%* | 6.2%* | 8.2% | 7.5% | 6.8% | 4.7%* | 7.8%* |
| Taking anti-diabetic medications at HbA1c measurement | 64.2% | 64.0% | 66.2% | 60.6%* | 67.4% | 61.2% | 59.4% | 62.3% | 68.0% | 70.6%* |
| Insulin | 9.6% | 6.7%* | 6.7%* | 6.8%* | 6.4%* | 7.4% | 10.2% | 4.6% | 13.9%* | 11.4% |
| Oral medications | 60.9% | 61.9% | 64.5%* | 58.0% | 65.5%* | 58.9% | 56.3% | 59.6% | 61.4% | 67.1%* |
| Taking anti-hypertensive medications at BP measurement | 66.5% | 55.3%* | 44.5%* | 56.0%* | 71.3* | 65.7% | 44.3%* | 45.4%* | 72.5%* | 61.4%* |
| 1 med | 31.6% | 30.2% | 27.8%* | 29.0% | 35.6%* | 32.6% | 26.7% | 28.2% | 25.8%* | 34.30% |
| 2 med | 20.5% | 16.0%* | 10.2%* | 17.4%* | 22.2% | 22.7% | 13.0% | 11.7%* | 25.8%* | 17.3%* |
| 3+ med | 14.4% | 9.1%* | 6.5%* | 9.6%* | 13.5% | 10.4% | 4.6%* | 5.5%* | 21.0%* | 9.8%* |
| Taking LMAs at LDL measurement | 56.0% | 49.4%* | 44.0%* | 47.1%* | 56.5% | 60.5% | 46.8% | 60.8% | 52.4% | 49.7%* |
BMI=body mass index; BP=blood pressure; HbA1C=glycosylated hemoglobin; HMO=health maintenance organization; LDL=low-density lipoprotein cholesterol; LMA=lipid modifying agent; PPO=preferred provider organization.
Statistically significant with Non-Hispanic Whites, by 95% Wilson CI for categorical variables and pairwise Wilcoxon test for continuous variables.
Treatment rates across racial/ethnic subgroups for anti-diabetic medications (insulin and oral medications), anti-hypertensive medications (number of concurrent medications categorized as 1, 2 and 3+) and lipid modifying agents (LMAs) were also examined and reported in Table 1. When treatment was examined, Asian Indians, Chinese and Filipinos were less likely, and Black/African Americans more likely, to be on insulin treatment compared to NHWs. While most racial/ethnic groups had similar treatment rates for oral anti-diabetic medications, Asian Indians, Filipinos, and Hispanic/Latino Americans had significantly higher rates, compared to NHWs. Asian Indians, Chinese, and Hispanic/Latino Americans, had lower rates of cholesterol treatment compared to NHWs. Black/African Americans were more likely to be treated with 2+ antihypertensive medications, compared to NHWs.
For all patients with type 2 diabetes, HbA1c goal attainment (68.7%) was highest, compared to the other risk factors, including BP (45.7%) and LDL (58.5%). Age- and sex-adjusted rates of goal attainment across different racial/ethnic subgroups are shown in Table 2. For HbA1c goal attainment, racial/ethnic minorities (Asian (all), Hispanic/Latino, and Black/African Americans) all had worse control compared to NHWs. Differences in HbA1c compared to NHWs were greater when the Asian American subgroups were examined separately. Chinese were the only subgroup that demonstrated significantly better HbA1c goal attainment compared to NHWs, while Asian Indians and Filipinos had significantly worse control. Less than half of the patients achieved BP goal attainment in most of the racial/ethnic subgroups. Nevertheless, Asian American subgroups had better BP control than NHWs, with significantly higher goal attainment rates for Asian Indians, Chinese and Vietnamese whereas Black/African Americans demonstrated the lowest goal attainment rate. There was no significant difference in LDL goal attainment across racial/ethnic groups. Only one fifth (21.1%) of patients with all three measures achieved simultaneous goal attainment for HbA1c, BP, and LDL. Black/African Americans had significantly poorer simultaneous goal attainment than NHWs.
Table 2.
Directly standardized goal attainment rates across racial/ethnic subgroups with 95% confidence intervals.
| Goal | Non-hispanic whites | Asians (all) | Asian indians | Chinese | Filipinos | Japanese | Koreans | Vietnamese | Black/africans | Hispanic/latinos |
|---|---|---|---|---|---|---|---|---|---|---|
| Simultaneous | 21.4% | 24.2%* | 24.2% | 25.6%* | 20.5% | 24.3% | 27.4% | 24.3% | 14.8%* | 18.6% |
| 20.5%–22.4% | 22.9%–25.6% | 21.1%–27.3% | 23.4%–27.9% | 17.5%–23.5% | 19.8%–28.7% | 19.0%–35.8% | 16.8%–31.9% | 10.3%–19.3% | 16.5%–20.8% | |
| HbA1c | 71.9% | 69.4%* | 66.1%* | 75.6%* | 61.5%* | 71.9% | 64.6% | 78.4% | 62.3%* | 61.3%* |
| 70.9%–72.9% | 68.0%–70.8% | 62.7%–69.5% | 73.4%–77.7% | 58.2%–64.8% | 67.3%–76.5% | 54.4%–74.8% | 71.9%–84.9% | 56.9%–67.7% | 58.8%–63.7% | |
| BP | 43.8% | 49.5%* | 48.6%* | 53.0%* | 41.7% | 45.8% | 51.6% | 59.2%* | 36.7%* | 44.8% |
| 42.7%–44.8% | 48.0%–51.0% | 45.2%–52.0% | 50.5%–55.5% | 38.4%–45.1% | 40.9%–50.7% | 41.4%–61.8% | 50.9%–67.5% | 31.3%–42.1% | 42.3%–47.2% | |
| LDL | 60.3% | 61.1% | 60.7% | 60.3% | 62.7% | 61.8% | 53.4% | 51.2% | 56.6% | 58.8% |
| 59.2%–61.4% | 59.6%–62.5% | 57.3%–64.1% | 57.8%–62.7% | 59.4%–66.0% | 56.9%–66.7% | 44.1%–62.7% | 40.4%–62.0% | 51.2%–62.1% | 56.4%–61.3% |
P=blood pressure; HbA1C=glycosylated hemoglobin; LDL=low-density lipoprotein cholesterol.
Significant at P<0.05, compared to Non-Hispanic Whites.
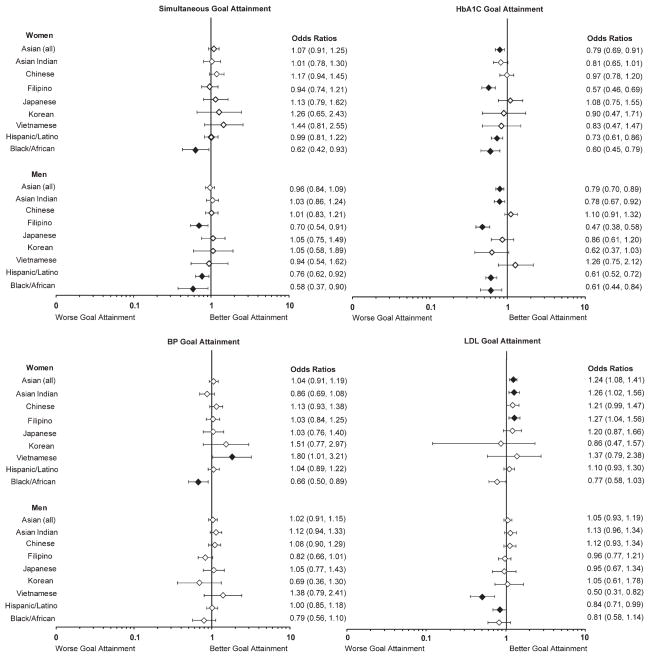
Adjusted odds ratios by race/ethnicity were estimated based on multivariate logistic regression models as described previously and reported in Fig. 1. Patient characteristics associated with significantly better simultaneous goal attainment included: age≥65 (for men only), normal BMI and increased number of office visits. Racial/ethnic minority women (Black/African American) and men (Filipino, Hispanic/Latino and Black/African American) were less likely to have simultaneous goal attainment. For HbA1c goal attainment, Asian Indian (men only), Filipino, Hispanic/Latino and Black/African American race/ethnicity was associated with worse control, compared to NHWs, after multivariate adjustment. Fewer racial/ethnic differences were found for BP control, with worse goal attainment only found for Black/African American women. Vietnamese and Hispanic/Latino American men had worse LDL control compared to NHWs.
Fig 1.
Multivariate ORs for risk factor control relative to NHW are presented, after adjustment for covariates (age, body-mass index (BMI), primary insurance, number of office visits, smoking status and treatment status). The diamond indicates the point estimate and the bar represents the 95% CI. Filled diamonds indicate statistical significance compared with NHWs at p<0.05. BP=Blood Pressure; HbA1C=glycosylated hemoglobin; LDL=low-density lipoprotein cholesterol.
When we examined the association between treatment and goal attainment we found that patients on treatment (compared to not on treatment) had worse goal attainment for HbA1c or BP, but better goal attainment for LDL. In multivariate models, insulin (0.10 [0.09–0.12]) and oral (0.44 [0.40–0.50]) medication usage was associated with worse HbA1c goal attainment. The association between anti-hypertensive medication treatment differed by the number of medications. Treatment with more than one anti-hypertensive medication was associated with worse BP goal attainment (0.88 [0.80–0.98] for two antihypertensives; 0.85 [0.86–0.96] for three or more antihypertensives), whereas treatment with one antihypertensive was associated with better BP goal attainment (1.09 [1.00–1.20]). Cholesterol treatment was associated with better LDL goal attainment (3.35 [3.11–3.61]).
When distance from goal was studied we found that Asian Americans had significantly smaller mean distance from HbA1c goal compared to NHWs (1.1% vs. 1.4%, p<0.05) despite lower rates of goal attainment. Patients taking insulin had larger mean distance from goals in HbA1c while patients taking oral anti-diabetic medications had smaller distance compared to untreated patients (insulin: 1.8%, orals: 1.2% vs. untreated: 1.4%, p<0.05).
4. Discussion
We found poor control of cardiovascular risk factors in our cohort of diverse patients with type 2 diabetes in an insured, outpatient setting, with racial/ethnic minorities at particular risk. While the percentage achieving simultaneous goal attainment in our population was greater than the national average (~10%) (Malik et al., 2007; Saydah et al., 2004), control was generally poor, with only one-fifth of patients meeting targets for the three major cardiovascular disease risk factors (HbA1c, BP, and LDL). Simultaneous goal attainment was significantly worse for Filipino men, Hispanic/Latino men and Black/African American men and women, compared to NHWs. Most racial/ethnic differences remained even after adjustment for clinical factors. Our findings add to the literature regarding racial/ethnic disparities in cardiovascular risk factor control among patients with type 2 diabetes, demonstrating that despite access to care, cardiovascular risk factor control, especially HbA1c control, remains worse for racial/ethnic minorities, compared to NHWs. Additionally, this is the first study to our knowledge to examine cardiovascular risk factor control for Asian Americans with type 2 diabetes, identifying Asian Indians and Filipinos, in addition to Hispanic/Latinos and Black/African Americans, as groups with worse control of HbA1c.
These findings support previous research that has found that racial/ethnic minorities with type 2 diabetes have worse control of cardiovascular risk factors than NHWs. Previous studies have found that approximately 15%–20% fewer Hispanic/Latino and Black/African American patients with type 2 diabetes achieve HbA1c control (Cheung et al., 2006; McWilliams et al., 2009), compared to NHWs. The disparity between racial/ethnic minorities and NHWs who attained glycemic control was slightly lower in our study (~10%) compared to nationally reported disparities (15%–20%) (Cheung et al., 2006; McWilliams et al., 2009). Overall the proportions of patients achieving cardiovascular risk factor control were higher, compared to the national averages, which may explain the slightly smaller difference among racial/ethnic minorities, compared to NHWs, in our cohort. We have extended the work in racial/ethnic minorities with type 2 diabetes to Asian Americans, identifying Asian Indians and Filipinos as additional high risk racial/ethnic groups. Similar to other studies that have found that racial/ethnic differences in cardiovascular risk factor control were not fully explained by adjusting for demographic and clinical factors (Ford, 2011; Winston, Barr, Carrasquillo, Bertoni, & Shea, 2009). Our findings also demonstrate that in an insured population with access to care, racial/ethnic disparities in risk factor control still persist.
Racial/ethnic difference in cardiovascular risk factor control may be explained by variations in cultural values and lifestyle behaviors. Using California Health Interview Survey data (2007), August and Sorkin (2011) found that the majority of middle-aged racial/ethnic minorities had lower physical activity levels and worse dietary behaviors, compared to NHWs. In our study, normal BMI was associated with better risk factor control, highlighting the benefits of attaining and maintaining health weight. Weight loss counseling may be particularly beneficial for racial/ethnic minorities, as most high-risks groups were overweight, compared to NHWs. Diet and physical activity modifications may be particularly challenging for Asian Indian and Filipino, Hispanic/Latino, and Black/African Americans, compared to NHWs, due to the lack of culturally relevant health education materials (Hawthorne, Robles, Cannings-John, & Edwards, 2008) and greater social and cultural importance of ethnic foods (Caballero, 2007; Finucane & McMullen, 2008; Gavin & Wright, 2007; Hsu & Yoon, 2007; Lawton et al., 2008). However, culturally competent health care education has been shown to improve glycemic and cholesterol control, compared to usual care (Hawthorne et al., 2008), and health care providers may consider this approach for racial/ethnic minorities in the management of type 2 diabetes.
Type 2 diabetes management may improve over time with greater contact with the healthcare system. Patient characteristics associated with better cardiovascular risk factor goal attainment included older age, increased physician office visits, and normal BMI. The majority of Asian American subgroups and Hispanic/Latino Americans had fewer office visits, as well as worse HbA1c control, compared to NHWs. A coordinated, multidisciplinary health care approach to the management of type 2 diabetes may be required to achieve targeted goals, particularly among racial/ethnic minorities. A physician survey found that primary care physicians are much less likely to initiate and intensify insulin treatment, compared to specialists, and often cite lack of time to educate patients (Cuddihy, Philis-Tsimikas, & Nazeri, 2011). Additionally, community health approaches have been particularly helpful in lowering HbA1c for Hispanic/Latino and Black/African American patients with type 2 diabetes (Spencer et al., 2011). Coordinated efforts by primary care physicians and specialists, enhanced by the use of health educators and dieticians may improve management of type 2 diabetes and cardiovascular risk factors.
Management of type 2 diabetes and cardiovascular risk factors with medication treatment is an area that may need improvement and further investigation. Medication treatment was associated with worse control for HbA1c and BP, and medication use was likely an indicator of disease severity (Malik et al., 2007). Adherence to treatment has been also been found to decrease with an increase in the number of medications, which may explain our findings of poor control with more medications for blood pressure (Chapman et al., 2005). Our study also corroborates findings from other studies which have found that persons with type 2 diabetes treated with insulin have worse HbA1c control rates compared to untreated patients (Cheung et al., 2006; Weinstock et al., 2011).
The association between treatment and control may be explained by late initiation of insulin treatment, lack of intensification of treatment, low medication adherence, or lifestyle and cultural differences among racial/ethnic minorities. Insulin is often seen as a last resort for physicians, and therefore may be used only when HbA1c levels are quite high and not adequately controlled by oral agents alone (Marshall, 2007). Delay of insulin treatment or non-adherence may be due to cultural barriers, including aversion to needle injections and glucose monitoring, greater fear of hypoglycemic events, and mistrust of providers and the healthcare system (Marshall, 2007; Weinstock et al., 2011). Additionally, complexities of treatment, lack of treatment education, and cultural beliefs have been associated with low medication adherence (Yang et al., 2009). Adherence may also explain some of the disparities in risk factor control, as Asian, Hispanic/Latino, and Black/African American patients are less likely than NHW patients to adhere to their cardiovascular disease risk factor controlling medications (diabetes, cholesterol and hypertension medications) (Traylor, Schmittdiel, Uratsu, Mangione, & Subramanian, 2010). Schmittdiel et al. (2008) demonstrated that poor adherence and/or lack of therapy intensification was evident in 53%–68% of patients with type 2 diabetes above target levels across conditions (Schmittdiel et al., 2008).
Limitations of this study include a single geographic area, with somewhat limited sample size in the smaller Asian American subgroups (i.e. Korean and Vietnamese populations) and nouninsured patients, which may impact generalizability to these populations. Additionally, we were not able to adjust for some demographic variables, including income and education levels, behavioral characteristics (diet and physical activity) and clinical factors, including medication adherence. However, the relative homogeneity in economic status in this clinical population (all insured, with access to healthcare) improves the internal validity of our comparisons. The majority of studies examining cardiovascular risk factor control in patients with type 2 diabetes have relied on self-report, mainly from the NHANES, to identify demographic variables and treatment status. A strength of this clinical data is that it gathers treatment data, among other clinical factors (e.g., office visits), from the EHRs rather than patient self-report, thus addressing limitations of previous studies and improving the data quality/reliability and validity of the findings. While we did not conduct a validation study, previous studies have found high positive predictive value (~90%) for ICD-9 codes in identifying cases of diabetes using similar outpatient administrative and clinical data (Twombly et al., 2011; Zgibor et al., 2007). Finally, the consistency of laboratory measurement of HbA1c, lipids, and other risk factors, as well as standardized criteria to define diabetes, was an advantage of our study.
To our knowledge this is the first study to obtain estimates of cardiovascular risk factor goal attainment for Asian Americans with type 2 diabetes in the United States. Our findings indicate that Asian Indian men and Filipinos, in addition to Hispanic/Latino and Black/African Americans, are additional high risk groups with poor cardiovascular risk factor control. These findings further highlight the need to study Asian American subgroups separately, as their health risks and behaviors differ greatly. Because, Asian Indian and Filipino Americans are at increased risk of type 2 diabetes (Choi et al., 2011; Wang et al., 2011) and cardiovascular disease (Holland, Wong, Lauderdale, & Palaniappan, 2011; Klatsky & Tekawa, 2005), these populations in particular would benefit from targeted interventions for type 2 diabetes and cardiovascular risk management. While previous studies have implicated access to care and insurance coverage in racial/ethnic disparities for cardiovascular risk factor control, in our insured population these disparities persisted. An emphasis on cultural competency among health care providers, acknowledging cultural differences in beliefs and attitudes toward health, may impact treatment adherence and self-management practices among racial/ethnic minorities with type 2 diabetes.
Footnotes
Conflict of Interest Statement: Nathan Wong receives current research support through UC Irvine from Bristol Myers Squibb in the area of diabetes. The other authors declare that they have no conflict of interest.
Ethical approval: This study was approved by the Palo Alto Medical Foundation Institutional Review Board (PAMF IRB).
The Pan Asian Cohort Study is funded by the National Institutes of Health, National Institute of Diabetes and Digestive Kidney Diseases grant 5R01DK081371.
Preliminary findings were presented at the American Heart Association Epidemiology and Prevention/Nutrition, Physical Activity and Metabolism 2012 Scientific Sessions; March 13–15, 2012; San Diego, CA.
References
- American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;3:S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- August KJ, Sorkin DH. Racial/ethnic disparities in exercise and dietary behaviors of middle-aged and older adults. Journal of General Internal Medicine. 2011;26:245–250. doi: 10.1007/s11606-010-1514-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metrics. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero AE. Type 2 diabetes in the Hispanic or Latino population: challenges and opportunities. Current Opinion in Endocrinology, Diabetes, and Obesity. 2007;14:151–157. doi: 10.1097/MED.0b013e32809f9531. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Age-adjusted percentage of civilian, noninstitutionalized population with diagnosed diabetes, by race and sex, United States, 1980–2009. Data from the National Health Interview Survey. 2009 http://www.cdc.gov/diabetes/statistics/prev/national/figraceethsex.htm.
- Centers for Disease Control and Prevention, National Center for Health Statistics. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. 2011. [Google Scholar]
- Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Archives of Internal Medicine. 2005;165:1147–1152. doi: 10.1001/archinte.165.10.1147. [DOI] [PubMed] [Google Scholar]
- Chatterji P, Joo H, Lahiri K. Racial/Ethnic- and education-related disparities in the control of risk factors for cardiovascular disease among individuals with diabetes. Diabetes Care. 2012;35:305–312. doi: 10.2337/dc11-1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. American Journal of Medicine. 2006;122:443–453. doi: 10.1016/j.amjmed.2008.09.047. [DOI] [PubMed] [Google Scholar]
- Choi SE, Chow VH, Chung SJ, Wong ND. Do risk factors explain the increased prevalence of type 2 diabetes among California Asian adults? Journal of Immigrant and Minority Health. 2011;13:803–808. doi: 10.1007/s10903-010-9397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care. 2010;33:562–568. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuddihy RM, Philis-Tsimikas A, Nazeri A. Type 2 diabetes care and insulin intensification: is a more multidisciplinary approach needed? Results from the MODIFY survey. The Diabetes Educator. 2011;37:111–123. doi: 10.1177/0145721710388426. [DOI] [PubMed] [Google Scholar]
- Finucane ML, McMullen CK. Making diabetes self-management education culturally relevant for Filipino Americans in Hawaii. The Diabetes Educator. 2008;34:841–853. doi: 10.1177/0145721708323098. [DOI] [PubMed] [Google Scholar]
- Ford ES. Trends in the control of risk factors for cardiovascular disease among adults with diagnosed diabetes: findings from the National Health and Nutrition Examination Survey 1999–2008. Journal of Diabetes. 2011;3:337–347. doi: 10.1111/j.1753-0407.2011.00148.x. [DOI] [PubMed] [Google Scholar]
- Gavin JR, III, Wright EE., Jr Building cultural competency for improved diabetes care: African Americans and diabetes. Journal of Family Practice. 2007;56:S22–S28. [PubMed] [Google Scholar]
- Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database of Systematic Reviews. 2008;16:CD006424. doi: 10.1002/14651858.CD006424.pub2. [DOI] [PubMed] [Google Scholar]
- Holland AT, Wong EC, Lauderdale DS, Palaniappan LP. Spectrum of cardiovascular diseases in Asian–American racial/ethnic subgroups. Annals of Epidemiology. 2011;21:608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu WC, Yoon HH. Building cultural competency for improved diabetes care: Asian Americans and diabetes. Journal of Family Practice. 2007;56:S15–S21. [PubMed] [Google Scholar]
- Jackson GL, Edelman D, Weinberger M. Simultaneous control of intermediate diabetes outcomes among Veterans Affairs primary care patients. Journal of General Internal Medicine. 2006;21:1050–1056. doi: 10.1111/j.1525-1497.2006.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL, Tekawa I. Health problems and hospitalizations among Asian–American ethnic groups. Ethncity and Disease. 2005;15:753–760. [PubMed] [Google Scholar]
- Lawton J, Ahmad N, Hanna L, Douglas M, Bains H, Hallowell N. We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethnicity & Health. 2008;13:305–319. doi: 10.1080/13557850701882910. [DOI] [PubMed] [Google Scholar]
- Malik S, Lopez V, Chen R, Wu W, Wong ND. Undertreatment of cardiovascular risk factors among persons with diabetes in the United States. Diabetes Research and Clinical Practice. 2007;77:126–133. doi: 10.1016/j.diabres.2006.10.016. [DOI] [PubMed] [Google Scholar]
- Marshall MC., Jr Overcoming barriers to glycemic control in African Americans with type-2 diabetes: benefits of insulin therapy. Journal of the National Medical Association. 2007;99:868–875. [PMC free article] [PubMed] [Google Scholar]
- McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Annals of Internal Medicine. 2009;150:505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- National Heart Lung and Blood Institute, the National Institute of Diabetes and Digestive and Kidney Diseases. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obesity Research. 1998;6:51S–209S. [PubMed] [Google Scholar]
- Palaniappan LP, Wong EC, Shin JJ, Moreno MR, Otero-Sabogal R. Collecting patient race/ethnicity and primary language data in ambulatory care settings: a case study in methodology. Health Services Research. 2009;44:1750–1761. doi: 10.1111/j.1475-6773.2009.00992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. Journal of the American Medical Association. 2004;291:335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- Schmittdiel JA, Uratsu CS, Karter AJ, Heisler M, Subramanian U, Mangione CM, et al. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. Journal of General Internal Medicine. 2008;23:588–594. doi: 10.1007/s11606-008-0554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. American Journal of Public Health. 2011;101:2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient–provider race/ethnicity and language concordance matter? Journal of General Internal Medicine. 2010;25:1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twombly JG, Long Q, Zhu M, Fraser LA, Olson DE, Wilson PW, et al. Validity of the primary care diagnosis of diabetes in veterans in the southeastern United States. Diabetes Research and Clinical Practice. 2011;91:395–400. doi: 10.1016/j.diabres.2010.11.001. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Projections of the population by sex, race, and Hispanic origin for the United States: 2010 to 2050. 2009. [Google Scholar]
- Wang EJ, Wong EC, Dixit AA, Fortmann SP, Linde RB, Palaniappan LP. Type 2 diabetes: identifying high risk Asian American subgroups in a clinical population. Diabetes Research and Clinical Practice. 2011;93:248–254. doi: 10.1016/j.diabres.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock RS, Teresi JA, Goland R, Izquierdo R, Palmas W, Eimicke JP, et al. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabetes Care. 2011;34:274–279. doi: 10.2337/dc10-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winston GJ, Barr RG, Carrasquillo O, Bertoni AG, Shea S. Sex and racial/ethnic differences in cardiovascular disease risk factor treatment and control among individuals with diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2009;32:1467–1469. doi: 10.2337/dc09-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong EC, Palaniappan LP, Lauderdale DS. Using name lists to infer Asian racial/ethnic subgroups in the healthcare setting. Medical Care. 2010;48:540–546. doi: 10.1097/MLR.0b013e3181d559e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Thumula V, Pace PF, Banahan BF, III, Wilkin NE, Lobb WB. Predictors of medication nonadherence among patients with diabetes in Medicare Part D programs: a retrospective cohort study. Clinical Therapeutics. 2009;31:2178–2188. doi: 10.1016/j.clinthera.2009.10.002. [discussion 2150–2171] [DOI] [PubMed] [Google Scholar]
- Zgibor JC, Orchard TJ, Saul M, Piatt G, Ruppert K, Stewart A, et al. Developing and validating a diabetes database in a large health system. Diabetes Research and Clinical Practice. 2007;75:313–319. doi: 10.1016/j.diabres.2006.07.007. [DOI] [PubMed] [Google Scholar]