Abstract
Background
Latent adenocarcinoma of prostate refers to cases who present no obvious sign or symptom during their life spans and the tumor is incidentally found at postmortem examination. Its frequency can be very important in epidemiologic investigations, prevention and treatment. No previous study has been done in this regard in Iran and the studies performed in other countries show various results. The aim of present study is to determine the frequency of latent prostate carcinoma by studying the corpora of men above 50 years old referred to forensic medicine organization in Tehran in 2008 and 2009.
Methods
In this study, 149 men aged above 50 who had died of different reasons and undergone autopsy were examined. Their prostates were excised and the slides were studied for the presence of adenocarcioma and prostatic intraepithelial neoplasia (PIN). In each case, age, weight of prostate, location of lesion, and grading according to Gleason's system were determined and the results were analyzed by SPSS software (version 16).
Results
Out of 149 cases, 34(22.8%) had low grade PIN, 26(17.4%) high grade PIN, and 14(9.4%) invasive adenocarcinoma. Most of the tumors were located in posterior lobe of prostate and they were more frequent in older cases (>65 years of age) and heavier prostates (p value <0.05). All invasive adenocarciomas were accompanied by PIN.
Conclusion
Worldwide studies show lower prevalence of latent carcinoma of prostate in Asian men than white European ones. Considering the absence of such studies in Iran, a larger study to compare and find out the precise rate of this kind of carcinoma, is recommended.
Keywords: Prostate, Cancer, Autopsy, Prevalence, Iran
Introduction
The overall incidence rate of prostate cancer is on increase in the world. Earlier detection of cases in the process of screening and primary stages of the disease is probable reason for this issue. It is estimated that one out of 6 male Americans will experience prostate cancer in his lifespan (1). The disease has been increasing faster since 1990s, after introducing PSA (prostate-specific antigen) test. However, prevalence rate varies in different parts of the world. Although some differences in the incidence rate of prostate cancer relate to the variation in screening plans, the r ole of genetic and environmental factors should not be underestimated. The incidence rate of prostate cancer among immigrants from some Asian countries (such as china, the Philippines and Japan) is lower than native Americans. That is why its incidence rate in countries which are open to immigrants (such as America) seems to be higher. It is hard to determine the incidence rate of prostate cancer, because high percentage of the cases are latent and are not detected using usual screening methos (2). Based on cancer registry reports, Iran (like most of Asian countries) is known to have a low incidence rate of prostate cancer (3). Therefore, the present study was designed to determine the actual incidence rate of prostate cancer in autopsy biopsies taken from the males above 50 years old who were referred to the forensic medicine organization in Tehran between 2008 and 2009.
Methods
The present cross-sectional study included 184 corpora samples of men aged above 50 years, sent to Tehran's forensic medicine organization (which is affiliated to Judicial system of Iran and located in south of Tehran) in 2008 and 2009, who presented any kind of disease, except for prostate carcinoma. Having performed microscopic and macroscopic studies, 35 cases were excluded due to serious deterioration of the specimens and the study performed in 149 cases. Then the prostates were excised, weighed precisely, and put in 10% formalin for fixation. After a period ranging from one week to one month, the specimens underwent macroscopic investigation to study external surfaces and sections. The following steps were gone through to cut sections through the prostate: In the first place, through a sagittal section the prostate was split into right and left halves and the posterior side was inked to determine the location of any probable lesion. Then various consecutive coronal sections were cut through the prostate, from the apex to the base at a distance of 3-5 mm. If observing any suspicious areas in terms of color and consistency, a sample was taken. Otherwise, 3 samples were randomly taken from the right and left halves. In this way, at least 6 sections were obtained from each prostate for the purpose of staining and preparing slides. Through processing steps the samples were turned into paraffin blocks, and after cutting sections by microtome and preparing slides, they were stained by hematoxylin and eosin (H&E). A single pathologist reviewed all slides for identifying low and high grade prostatic intraepithelial neoplasia (LGPIN & HGPIN), invasive adenocarcinoma and its grade (according to Gleason scoring system) as well as location of them. The classification of PIN into low grade and high grade is based mainly on the cytological characteristics of the cells. The nuclei of cells composing low grade PIN are enlarged, vary in size, have normal or slightly increased chromatin content, and possess small or inconspicuous nucleoli. High grade PIN is characterized by cells with large nuclei of relatively uniform size, an increased chromatin content, which might be irregularly distributed, and prominent nucleoli that are similar to those of carcinoma cells (4).
Statistical Analysis
The data were statistically analyzed through the chi-square test to determine the differences in proportion at a significance level of (p< 0.05) by SPSS software (version 16).
Results
The cases ranged in age from 50 to 91 with an average of 64.5 (SD = 3.8) years. Out of 149 prostate samples, the lowest and highest in terms of weight were 20 and 112.3 gr respectively with an average of 44.5 (SD = 6.1)gr. Considering a weight cut off of 30 gr (5), 83% of the cases were suggestive of nodular hyperplasia (BPH).
Low grade prostatic intraepithelial neoplasia (LPIN) was found in 34 cases (22.8%) consist of 29(85%) in the posterior and 5 (15%) in the anterior lobes of prostate. In this group, the minimum and maximum ages of the subjects were 50 and 87 with an average of 68.7(SD = 4.3) years. The average weight of prostates was 52.1 (SD = 6.8) gr.
High grade prostatic intraepithelial neoplasia (HPIN) was seen in 26 cases (17.4%) including 22 (84.5%) in the posterior and 4 (15.5%) in the anterior lobes of prostate. In this group, the minimum and maximum ages of the subjects were 50 and 82 with an average of 67.3 (SD = 4.1) years. The average weight of prostates was 53 (SD = 6.7) gr.
Invasive adenocarcinoma was detected in 14 (9.4%) out of all studied cases including 9 cases (64%) in the posterior, 1 case (7%) in the anterior, and 4 cases (29%) in both posterior and anterior lobes of prostate. In this group, the minimum and maximum ages of the subjects were 50 and 87 with an average of 71.6 years (SD = 4.4). In this group, 9 cases (64%) were over 65 years old whereas 5 cases were detected in younger subjects (50-65 years old) (p value =0.03). The average weight of prostates with malignancy was 54.2 gr (SD = 6.1) showing significantly higher than mean weight of total group (p value =0.005). In this group, lack of history of prostate carcinoma was confirmed by reviewing of the existing files. The obtained Gleason scores (GS) in adenocarcinoma groups were4 (2 + 2), 6 (3 + 3), 7 (3 + 4 or 4 + 3), and 9 (5 + 4), in 3, 6, 4 and 1 cases, respectively. Therefore, in terms of histological classification (6), 3 cases (21%) were well-differentiated, 6 cases (43%) moderately-differentiated, and 5 cases (36%) poorly-differentiated. The average ages in these 3 groups were 78.5, 66.8, and 74.3 respectively. All cases (100%) of adenocarcioma were accompanied by PIN: 3 cases by LPIN, 2 cases by HPIN, and 9 cases by both LPIN and HPIN. 98 cases had neither intraepithelial neoplasia nor invasive adenocarcinoma. Table 1 displays characteristics of 3 groups of neoplasia.
Table 1.
Distribution of cases in 3 groups of neoplasia.
| No. of cases (%) | Mean age of the cases (years) | Mean weight of prostate (gr) | |
|---|---|---|---|
| LGPIN* | 34 (22.8%) | 68.7 (SD = 4.3) | 52.1 (SD = 6.8) |
| HGPIN** | 26 (17.4%) | 67.3 (SD = 4.1) | 53 (SD = 6.7) |
| Invasive adenocarcinoma | 14(9.4%) | 71.6 (SD = 4.4) | 54.2 (SD = 6.1) |
Low grade prostatic intraepithelial neoplasia.
High grade prostatic intraepithelial neoplasia.
Discussion
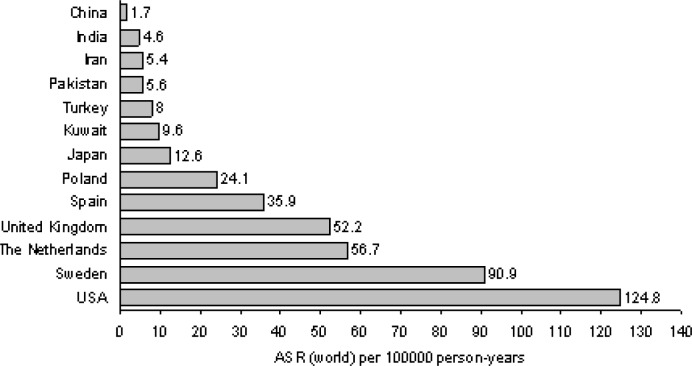
Prostate cancer is the third common cancer among males worldwide. Every year, half a million cases of prostate cancer are seen all over the world, which accounts for approximately 10% of cancer incidence rates in the world (7). Although in most industrial countries the incidence rate of prostate cancer is increased, its overall mortality rate is decreasing. The main reason for this reduction is the improvements in medical health care and screening plans (2). In the countries where screening methods for prostate cancer are not common yet, our knowledge of its incidence rate is slight. In China, the incidence rate of prostate cancer was reported to be 26 times lower than America in 1991 (8). However, the improvements in screening methods have helped increase the identification of prostate cancer cases in china and other Asian countries (9). Most of our information about the incidence rate of prostate cancer is related to the cancer registry reports in different countries. According to these studies, Iran is considered to have a low prevalence rate of prostate cancer. While the incidence rates of prostate cancer are 119/100000, 11/100000, 1.6/100000 and 5.1/100000 in the United States of America, west Asia, China and Iran, respectively (2, 3) (10, Fig. 1). Although genetic and environmental variations may account for these statistical differences to some extent, some experts attribute these differences to uncommon screening plans and insufficient identification of the cases. Therefore, some studies have been designed to determine the incidence rate of latent prostate cancer in different countries. Latent carcinoma is a kind of cancer which only can be identified through examination after death (2). Studies reveal that the incidence rate of latent carcinoma is higher in western societies (11, 12). In United States of America, 34-36% of autopsy specimens taken from men above 30 years old revealed prostate cancer (12). But this rate is lower in European countries especially in the areas around the Mediterranean sea (for example, 18.5% in Spain (13) and 18.8%. in Greece (6)). Among Asian countries, the incidence rate of latent carcinoma is 20.5% in Japan, but in other countries such as Hong Kong, Singapore and China it is much lower (2, 14). Other studies carried out (for treatment of bladder cancer) on the cystoprostatectomy specimens, showed almost the same results for incidentally-found prostate carcinoma (10, 15–18). In 2 separate studies done by Lee and Liu, the incidence rate of the cancer in Chinese and Taiwanese men were 4% and 8.2% respectively (15, 16). Another study carried out in India (by Desai et al. 2002), showed that the incidence rate of latent carcinoma was 6.8% in Indian men (17). In Iran no study has been done to determine the incidence rate of latent carcinoma in autopsy specimens. However, one study was carried out (by Hosseini et al.) on the cystoprostatectomy samples from the patients with the bladder cancer suggesting that the incidence rate of latent carcinoma was 14% (18). Table 2 shows a comparison between the results of the our study and other studies in Asian countries (2, 10, 15–18).
Fig. 1.
Age-standardized (to world population) incidence rates of prostate cancer among men (3).
Table 2.
| Nations/ regions | Authors | Sample type | Number of Samples | Patients’ mean age (years) | PCa (%) |
|---|---|---|---|---|---|
| Mainland China | Liu et al (16) | Cystoprostatectomy | 49 | 65.3 | 4 (8.2) |
| Taiwan, China | Lee et al (15) | Cystoprostatectomy | 248 | 63 | 10 (4) |
| India | Desai et al (17) | Cystoprostatectomy | 44 | 54.7 | 3 (6.8) |
| China | Yi-Ping Zhu et al (10) | Cystoprostatectomy | 92 | 67.1 | 3 (3.3) |
| Japan | Yatani et al (2) | Autopsy | 576 | NA* | 119 (20.5) |
| Iran | Hosseini et al (18) | Cystoprostatectomy | 50 | 62.5 | 7 (14) |
| Present study | Autopsy | 149 | 64.5 | 14(9.4) |
Not assigned
Conclusion
Based on the results of the present study, although the incidence rate of latent carcinoma is almost low in Iranian men - like most Asian countries -, the development of screening programs to detect the latent cases of the disease is recommended. The limitation of our study was lack of total submission of the samples, therefore, we suggest a larger study, and also with total sampling of prostates.
Acknowledgements
This study was funded and supported by Tehran University of medical Sciences (TUMS); Grant No. 930. The authors also thank the deputy of research and staff of Tehran's forensic medicine organization who assisted with this study.
References
- 1.Edwards BK, Brown ML, Wingo PA, Howe HL, Ward E, Ries LAG, et al. Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005;97:1407–1427. doi: 10.1093/jnci/dji289. [DOI] [PubMed] [Google Scholar]
- 2.Nicolas B. Delongchamps, Amar Singh and Gabriel P. Haas. The Role of Prevalence in the Diagnosis of Prostate Cancer. Cancer Control. 2006 Jul;13(3):158–168. doi: 10.1177/107327480601300302. [DOI] [PubMed] [Google Scholar]
- 3.Sadjadi A, Nooraie M, Ghorbani A, Alimohammadian M, Zahedi MJ, Darvish-Moghadam S, et al. The incidence of prostate cancer in Iran: results of a population-based cancer registry. Arch Iran Med. 2007 Oct;10(4):481–5. [PubMed] [Google Scholar]
- 4.Montironi R, Mazzucchelli R, Algaba F, Lopez-Beltran A. Morphological identification of the patterns of prostatic intraepithelial neoplasia and their importance. J Clin Pathol. 2000;53:655–65. doi: 10.1136/jcp.53.9.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Safarinejad MR. Prevalence of benign prostatic hyperplasia in a population-based study in Iranian men 40 years old or older. Int Urol Nephrol. 2008;40:921–31. doi: 10.1007/s11255-008-9338-7. [DOI] [PubMed] [Google Scholar]
- 6.Stamatiou K, Alevizos A, Perimeni D, Sofras F, Agapitos E. Frequency of impalpable prostate adenocarcinoma and precancerous conditions in Greek male population: an autopsy study. Prostate Cancer Prostatic Dis. 2006;9(1):45–9. doi: 10.1038/sj.pcan.4500847. [DOI] [PubMed] [Google Scholar]
- 7.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 8.Yu H, Harris RE, Gao YT, Gao R, Wynder EL. Comparative epidemiology of cancers of the colon, rectum, prostate and breast in Shanghai, China versus United States. Int J Epidemiol. 1991;20:76–81. doi: 10.1093/ije/20.1.76. [DOI] [PubMed] [Google Scholar]
- 9.Gu F. Epidemiological survey of benign prostatic hyperplasia and prostatic cancer in China. Chin Med J (Engl) 2000;113:299–302. [PubMed] [Google Scholar]
- 10.Yi-Ping Zhu, Ding-Wei Ye, Xu-Dong Yao, Shi-Lin Zhang, Bo Dai, Hai-Liang Zhang, et al. Psrostate cancer in patients undergoing radical cystoprostatectomy: data from China and other Asian countries. Asian Journal of Andrology. 2009;11:104–108. doi: 10.1038/aja.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matzkin H, Soloway MS. Cigarette smoking: a review of possible associations with benign prostatic hyperplasia and prostate cancer. Prostate. 1993;22:277–290. doi: 10.1002/pros.2990220402. [DOI] [PubMed] [Google Scholar]
- 12.Shiraishi T, Watanabe M, Matsuura H, Kusano I, Yatani R, Stemmermann GN. The frequency of latent prostatic carcinoma in young males: the Japanese experience. In Vivo. 1994;8:445–447. [PubMed] [Google Scholar]
- 13.Sánchez-Chapado M, Olmedilla G, Cabeza M, Donat E, Ruiz A. Prevalence of prostate cancer and prostatic intraepithelial neoplasia in Caucasian Mediterranean males: an autopsy study. Prostate. 2003;54:238–247. doi: 10.1002/pros.10177. [DOI] [PubMed] [Google Scholar]
- 14.Koug XT, Xia TL, Gu FL. Study of the latent carcinoma of prostate in China. BJU. 1997;80(suppl 2):A895. [Google Scholar]
- 15.Lee SH, Chang PL, Chen SM, Sun GH, Chen CL, Shen BY, et al. Synchronous primary carcinomas of the bladder and prostate. Asian J Androl. 2006;8:357–9. doi: 10.1111/j.1745-7262.2006.00129.x. [DOI] [PubMed] [Google Scholar]
- 16.Liu R, Shao GX, Qin RL, FX K. Coexistence of transitional cell carcinoma of bladder and adenocarcinoma of prostate (report of 5 cases) Chin J Urol. 1996;17:738–9. [Google Scholar]
- 17.Desai SB, Borges AM. The prevalence of high-grade prostatic intraepithelial neoplasia in surgical resection specimens: an Indian experience. Cancer. 2002;94:2350–2. doi: 10.1002/cncr.10495. [DOI] [PubMed] [Google Scholar]
- 18.Hosseini SY, Danesh AK, Parvin M, Basiri A, Javadzadeh T, Safarinejad MR, et al. Incidental prostatic adenocarcinoma in patients with PSA less than 4 ng/mL undergoing radical cystoprostatectomy for bladder cancer in Iranian men. Int Braz J Urol. 2007;33:167–73. doi: 10.1590/s1677-55382007000200006. Discussion 73–5. [DOI] [PubMed] [Google Scholar]