Abstract
When epilepsy does not remit in childhood, transition and transfer to adult care is eventually required. Youth must leave the family-centered approach of pediatric care for the individual focus of adult medicine. Evidence from population-based studies indicates that many of those with childhood-onset epilepsy have major social difficulties in adulthood even if their epilepsy has resolved. Epilepsy may have major effects on normal adolescent development, and societal attitudes confound this difficult period in the lives of young people with epilepsy. Very little objective data are available to assist in the designing of models of care for youth with epilepsy; however, based on our clinical experience and the limited available literature, it appears that a transition program to prepare children for adult care is best started during childhood and adolescence. The formal transfer to adult services may be assisted by a transition clinic jointly attended by pediatric and adult epilepsy specialists.
About fifty to sixty percent of children with epilepsy have remission of their seizures during childhood and are able to discontinue antiepileptic drug (AED) treatment. The other forty to fifty percent continue to have epilepsy well into adulthood, possibly for their entire lives. Epilepsy may have serious effects on adolescent development, and long-term follow-up studies suggest that many have significant social problems in adult life (1). As young people with epilepsy struggle with adolescence, most will have their healthcare providers change from the nurturing, family-centered style of pediatrics to the very individualistic, “autonomous” approach of adult healthcare. In this article, we consider how epilepsy might affect adolescent development and what may be the most effective ways to assist youth with epilepsy in making a smooth transition to adult care. Most of our comments are impressionistic, based on personal experience and influenced by a pilot project involving 50 youth with epilepsy and a transition clinic. There is very little published evidence to guide the process of transition.
“Transfer” and “transition” should be distinguished. Transfer is fairly straightforward. The pediatric physician arranges an appointment with an adult physician and asks that care be transferred. A summary letter of referral is sent, and the pediatric physician says goodbye to the patient and family. Transition is a more complex process to prepare the young person for transfer to adult healthcare. Transition teaching may begin as soon as it is clear that the child/adolescent's epilepsy is unlikely to remit. The goal is to help the patient and family to understand the epilepsy well enough to allow them to seek appropriate care as issues arise.
Parents play a large role in the transition/transfer process. During the pediatric years, much of the physician visit is focused on their concerns. Pediatrics is very family centered. In adult care, the focus is on the independent individual; the young person sees the physician by his- or herself, and if parents attend the visit, they are expected to remain in the waiting room. Relinquishing their controlling role is difficult for many parents, and their needs are best included in the transition process.
There are three patterns of epilepsy evolution to be considered in the transition process. First, epilepsy that begins in early childhood and persists into adulthood is strongly associated with mental handicap, which has enormous influence on adult epilepsy care and social outcome (2). The epilepsy syndromes that characterize this first group tend to be in the broad categories of symptomatic partial or symptomatic generalized. Second, epilepsy may begin in early childhood with remission of seizures, but with the persistence of other associated comorbidities (i.e., cognitive deficits, behaviour disorders, motor impairments). As noted below, remission of epilepsy in childhood does not guarantee a successful adulthood. It is very difficult to provide appropriate adult follow-up for the comorbid disorders when the epilepsy is in remission and no longer requires treatment. Third, epilepsy may develop in adolescence and persist into adulthood—in fact, epilepsy that begins after 12 years of age is unlikely to remit (3, 4). Juvenile Myoclonic Epilepsy (JME) is an important contributor to this group.
Why Might Epilepsy Interfere With the Normal Maturation of Adolescence?
The psychoanalyst, Erik Erikson, wrote about the life cycle (5). He suggested that adolescence is a time of conflict between identity and identity confusion and pointed to “fidelity” as a key characteristic that needs to develop in normal adolescence. In young adulthood, there is conflict between intimacy and isolation, and “love” is a key attribute to develop. In adulthood, the essential conflict is between generativity and stagnation, with “care” being a key attribute to success. For adolescents to move to successful young adulthood and then complete their adult development, they need to master issues in at least four domains including autonomy, body image, peer group identity, and identity (6). It is relatively easy to understand how epilepsy could interfere with these four factors.
Autonomy is affected by epilepsy. Adolescents expressed to us: “Think of the things that I can no longer do without supervision—take a bath, swim, stay up late, drink beer, drive, have babies, become a pilot, join the armed forces, take aspirin, scuba dive, go to dances with strobe lights, play video games, go on the school trip. Think of all the things that I have to do everyday—yes, everyday: take my pills twice a day, go to the stupid doctor, have EEGs that mess up my hair, watch my weight.”
Body image is very important to adolescents. The following are common complaints heard in our practice: “There is something terribly wrong with me (remember I have never seen my seizures). The pills will somehow mess up my hormones. The pills will somehow mess up my bones. The pills will make me fat. My hair will fall out.”
Peer group identity may be profoundly upset by epilepsy. “No will go on a date with me. No one else has this stupid problem. No one else has the tremor from medication. How can I avoid the strobe lights and ever go out in public? What happens if I have a seizure at school and wet my pants? No one will ever marry me.”
Identity issues may be very troublesome. It is common to hear: “I am not supposed to do most of the things that my friends do—drinking, drugs, sex (the pill apparently does not work). There are many professions that I am blocked from—how will I cope with life? I will die during sleep from SUDEP.”
These concerns of adolescents with epilepsy are realistic and confirmed by a 2001 U.S. survey of 19,441 “normal” high school students, which provided startling revelations about perceptions of epilepsy (7). Nineteen percent thought that epilepsy was a mental illness and 30% were unsure. Fifty percent were uncertain if people with epilepsy could drive cars, marry, have children or work, and 51% thought that people die during seizures. One-half of respondents were unsure if epilepsy is contagious and only one-third would date someone with epilepsy. Perhaps most frightening was the report by 50% that you could look at a person and tell if they have epilepsy.
We surveyed 271 medical and law students, physicians, childcare workers, the general public, and people with epilepsy in 1981, and again in 2006 (8). Nearly half of respondents believed that capricious and severe violence was possible or likely during a seizure. It is not surprising that adolescents with epilepsy have problems coming to grips with the attitudes of their peers.
Evidence That Social Outcome Is Often Unsatisfactory
There is evidence that adults with childhood-onset epilepsy have significant problems in achieving objective and simple markers of successful adulthood—employment, marriage or cohabitation, participation in a social life, and some hobbies or activities other than work and family life. A 30-year follow-up of a Finnish population-based cohort examined the adult social outcome of 100 patients with childhood-onset epilepsy but no other neurologic problems (9). Compared with a national random sample of age- and sex-matched controls and another occupation control group, adults with “epilepsy only” had less education and lower rates of employment and marriage. They were much more likely to rate their own ability to control their lives as “poor or missing.” Polytherapy and continuing seizures were associated with decreased life satisfaction and poor general health; however, these epilepsy factors did not account for most of the variance.
In Nova Scotia, we have documented the long-term social outcome of several childhood-onset syndromes. The Nova Scotia Childhood Epilepsy Cohort is population-based and includes all children <16 years of age who developed epilepsy between 1977 and 1985 in this population of about 850,000. All of the children in Nova Scotia who developed childhood absence epilepsy were compared at an average age of 23 years with a group of children with juvenile rheumatoid arthritis who formed a chronic disease control group (10). Those with absence were much less likely to complete high school and be employed, particularly in work that involved more skills than manual labor. Absence patients had significantly more problems with alcohol abuse (particularly binge drinking) and more mental health assessments. A third of the girls with absence had an inadvertent pregnancy compared with only 3% of controls. As in the Finnish study, those with continuing seizures and requirement for ongoing AEDs were more likely to have social problems. The lack or remission, however, did not explain the majority of the social problems.
In the Nova Scotia cohort, we compared the adult social outcome of all patients with juvenile myoclonic epilepsy (JME) (n = 24) and those with idiopathic generalized epilepsy with generalized tonic-clonic seizures only (IGE-GTC) (n = 40) (11, 12). All patients had normal intelligence and normal neurologic examinations. After an average follow-up of ~25 years, the seizure remission rate was higher for IGE-GTC (75% vs 38%, p = 0.005), but those with JME were more likely to graduate from high school (87% vs 60%, p = 0.002). A discouraging number were unemployed—about one-third of each group compared with a population rate of about 7%. We noted that 75% of each group had =1 major indicator for poor adult social outcome (no high school graduation, unemployment, psychiatric diagnosis, no romantic relationships >3 months, living alone, conviction of a crime, and pregnancy outside of a stable relationship). In the IGE-GTC group there were 13 pregnancies, and 85% had occurred outside of a stable relationship (defined as ≥6 months). Of the 15 pregnancies in the JME group, 73% were also outside of a stable relationship.
Assessing the social outcome of patients with mental handicap and epilepsy is complex because complete social independence is very unusual. Miller and Chan suggested that a good outcome should include significant social support from a large network including professional staff, family, and friends (13). Self-determination and perceived control should be maximized. Productive work is important, with competitive and supported employment more successful than activities in a sheltered workshop or home. Adaptive behavior including independent living skills, social skills, communication, and academic skills are clearly valuable. In the Nova Scotia study, virtually all people with epilepsy and mental retardation (20% of the cohort) had a social outcome that included significant dependency for activities of daily living and financial support. Similar findings were noted in a population-based study from Japan (14). Of special personal concern in Nova Scotia, was the observation that only 25% of young adults with symptomatic generalized epilepsy (SGE) and 28% of those with intractable SGE had ever seen an adult neurologist; the remainder did not have an opportunity to receive any of the newer AEDs. These patients did not receive appropriate adult epilepsy care, even though there were no financial barriers in the Canadian healthcare system.
What Are Barriers for Successful Transition of Young People With Childhood Onset Epilepsy to Adult Care?
Treatment of childhood epilepsy involves a very close and comfortable relationship between the family and epilepsy specialist. The family is unlikely to trust the opinion of their primary care provider about matters relating to epilepsy as they have always sought more expert care. The child neurologist/epileptologist may doubt that adult epilepsy services will care adequately for their patient, particularly the comorbid problems. Adult epileptologists often feel “unfamiliar” and overwhelmed by the complexity of pediatric epilepsy syndromes and their associated comorbidities. The adolescent often has insufficient knowledge about his/her epilepsy, and even the simplest parts of their care have been attended to by the parents—for example, refilling a prescription. When epilepsy begins early in life, explanations are directed to the parents and may not be repeated for the children as they develop appropriate cognitive skills to comprehend. We have been impressed by how often adolescents with epilepsy are unable to explain their diagnosis in a few sentences that include their epilepsy syndrome and its treatment.
Adolescents with epilepsy and mental handicap present a significant problem for transition/transfer. Interview and observation data indicate that adult neurology/epilepsy services are ill prepared to cope with the types of challenging behavior that may characterize a young adult with mental handicap (15). Physician waiting rooms and offices are bereft of toys or activities that are developmentally appropriate. Concern about aggression or overly friendly behavior may be intimidating from others in the waiting area, and adult physicians feel that they are inadequately trained to deal with issues related to mental handicap (15). We have been repeatedly amazed that if a young adult with mental retardation presents to an adult emergency room, the parents are often not permitted to accompany them into the examination area.
How Can Transition/Transfer Be Facilitated?
There is no objective data to answer this question. The process of transition must begin in the pediatric world with education and adjustment of expectations. A prerequisite for transition teaching is factual data about the natural history of childhood epilepsy as it persists into adulthood, data that are limited at present. The pediatric physician must have a realistic understanding of the type of care that will be offered in an adult office or clinic, and the adult physician should understand the type of care that has been offered to date. In our own experience, there was real value in the pediatric physician spending time in the adult clinic as an observer, and vice versa. During a sabbatical, we interviewed 50 adult and pediatric epilepsy physicians in 11 centers in 7 countries. There was a prevalent attitude amongst adult providers that pediatricians were too controlling and indulgent to their epilepsy patients. Pediatricians perceived adult medicine as uncaring. A few afternoons spent in each other's clinic can remedy misconceptions.
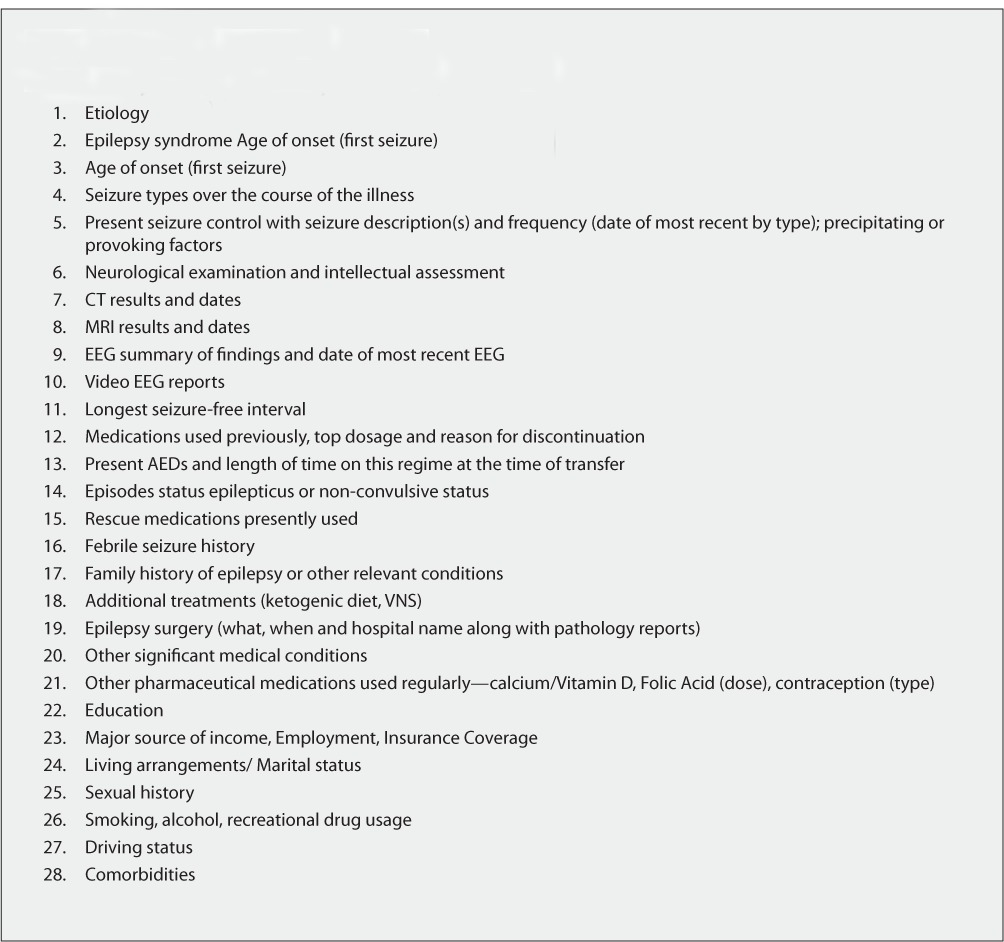
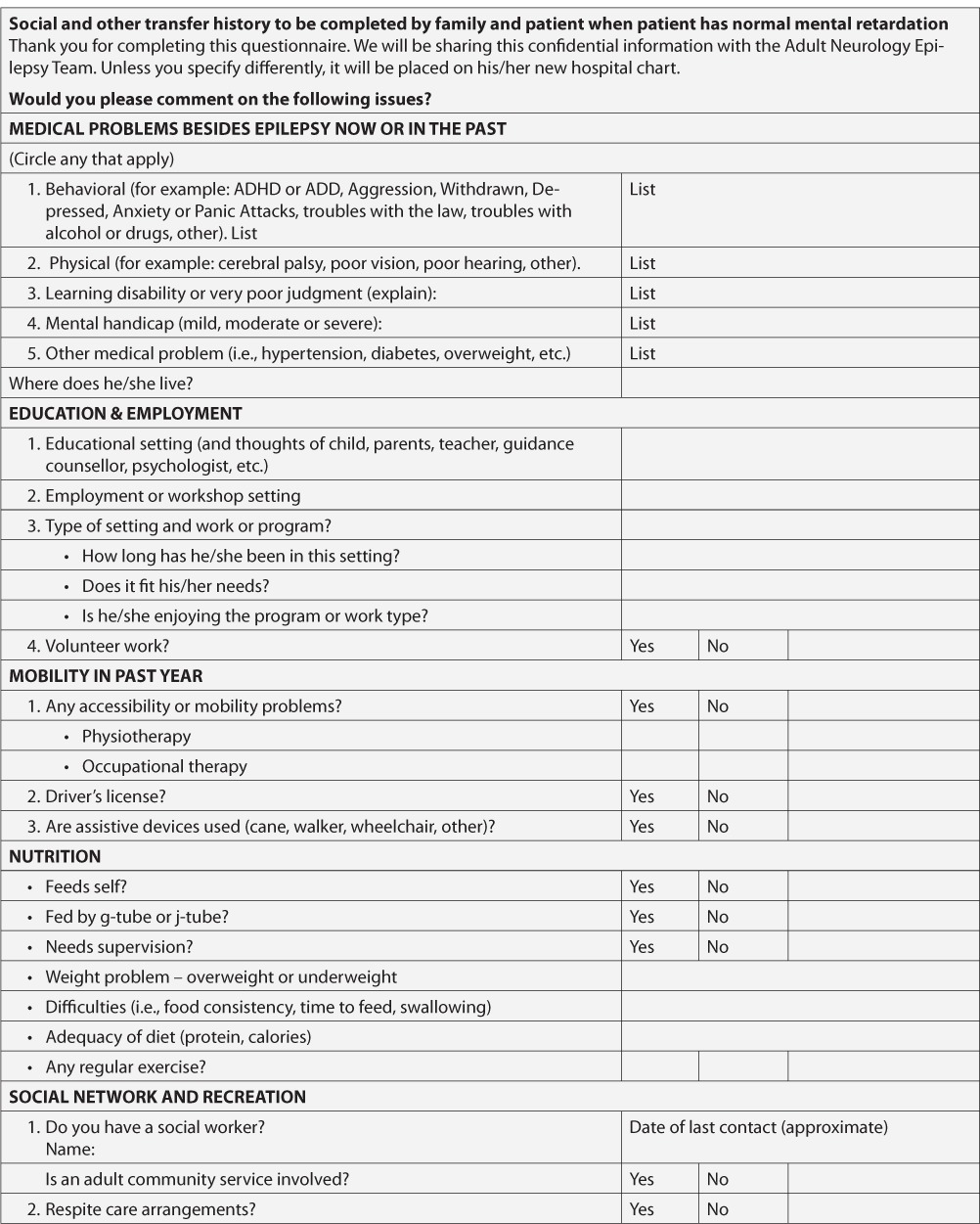
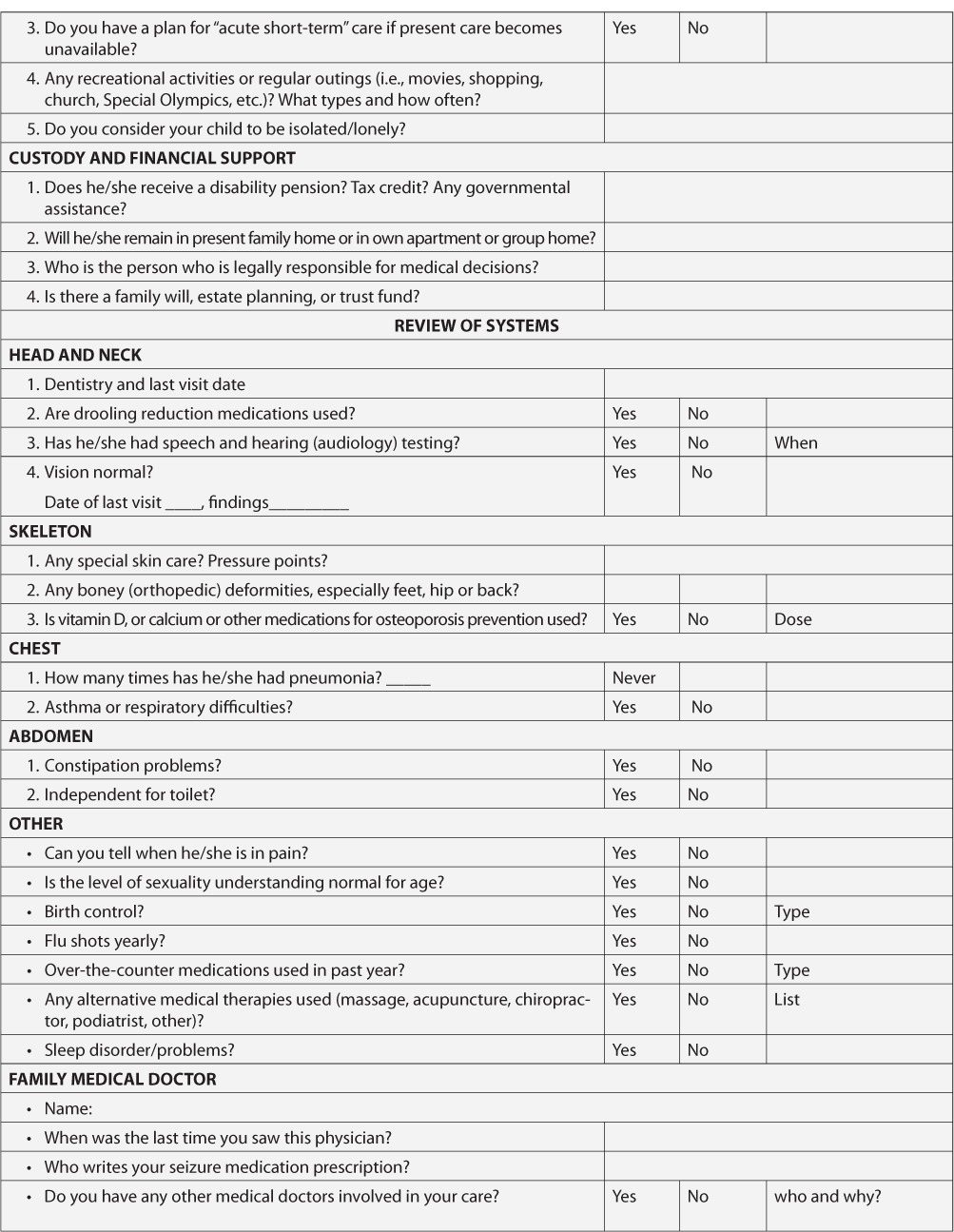
There are a number of models for transition/transfer, but all require accurate transfer of relevant medical and social information. We developed three forms (see Appendix) that summarize the clinical course: a medical form to be completed by the pediatric physician and a social form to be completed by the family (with versions for those with normal intelligence and mental handicap). These forms are sent to the physician accepting transfer of the patient's care, and copies are given to the family and patient for their records. Our informal impression is that they are effective.
Simple referral back to the primary care provider may be not satisfactory, since that person often has not been involved in the epilepsy care and is unlikely to be “up-to-date” with newer treatments. Referral to a private practice adult neurologist may be the only option, but visits are typically short (<30 minutes) and ongoing care may not be offered (16). In Canada, most neurology practices operate by referral only; the patient is seen, and then returned to the primary care physician with treatment suggestions. A new referral is required for another specialty visit. Given the chronic and fluctuating nature of epilepsy, this is an awkward arrangement.
When epilepsy is only a part of a complex pediatric disorder, pediatric care is often delivered in a multidisciplinary clinic. This model of care is uncommon in adult medicine, but it may be available through a rehabilitation program.
In our opinion, the best arrangement is a formal transition/transfer clinic. This clinic is jointly attended by the adult and pediatric epilepsy specialists but takes place in the adult setting. Reimbursement for such activities may be challenging in systems of care dominated by insurance companies; however, our impression is that the model works well. Patients and parents are comforted to meet a familiar face in an unfamiliar setting. Communication is good. The young person is seen for several visits to be sure that they are able to manage their problem adequately and independently when possible. At that point, a more long-term care arrangement needs to be set up. It may be continuation with the adult provider of the transition clinic or with someone else; in any case, the “apron strings” with pediatrics must be eventually severed. There are two published accounts of such clinics in the U.K. (17, 18). It is interesting that JME and SGE syndromes were the most common in these transitioned patients. The joint transition clinic is not just for teaching and maturation, but also for a careful review of the epilepsy diagnosis and treatment. In one description of such a clinic, 10% of patients were found not to have epilepsy and about 25% had a change of AEDs (16).
Another model was recently described in Edmonton, Alberta (19). Here the transition/transfer process is managed by the pediatric and adult epilepsy nurses who meet together with the family and patient independently from the adult and pediatric neurologists. The nurses provide information about transition and provide some continuity of care. The actual transfer of care is based on a referral note to the adult service and then a physician visit. This model is less “expensive” for physician time, and families indicated some satisfaction.
Clearly, the process of transition/transfer for young people with epilepsy is a complex one. We urge physicians to support and direct their patients to their local family support groups, specific interest groups such as the IDEA league for Dravet Syndrome, or national associations such as the Epilepsy Foundation of America, who have a mandate to be sure that patients are up-to-date and able to ask for newer treatments as they become available. In the end, it is the patient and family who need to direct the process, ensure that they receive the best care, and develop a trusting relationship with the adult medical care system.
Acknowledgments
Our thanks go to Susan Rahey Adult Epilepsy Coordinator who assisted with our pilot transition program and to Dr. Mark Sadler who helped to develop the medical and social forms for transition/transfer.
Appendix 1.
#1 Medical Transfer History for Physician to complete
Appendix 2.
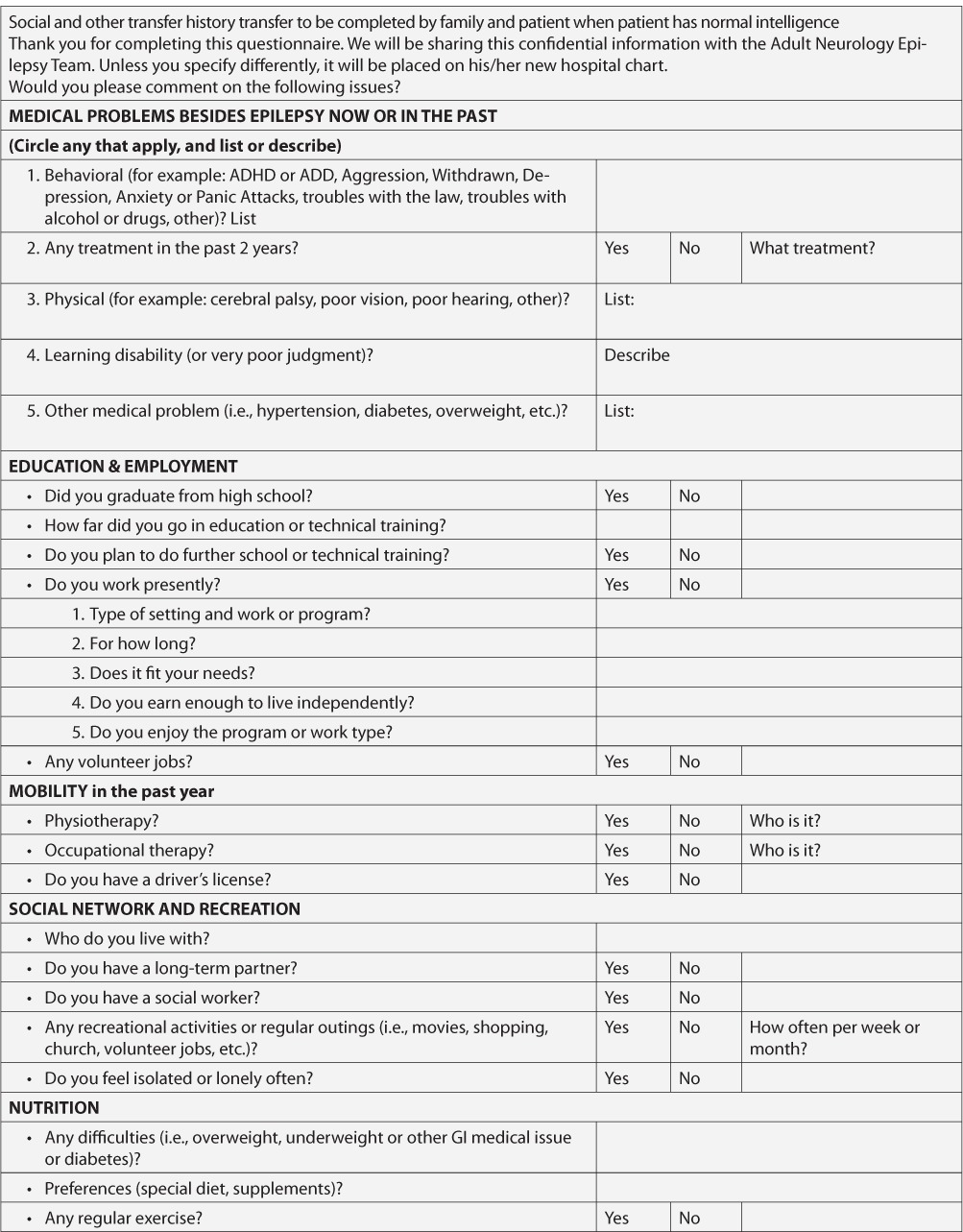
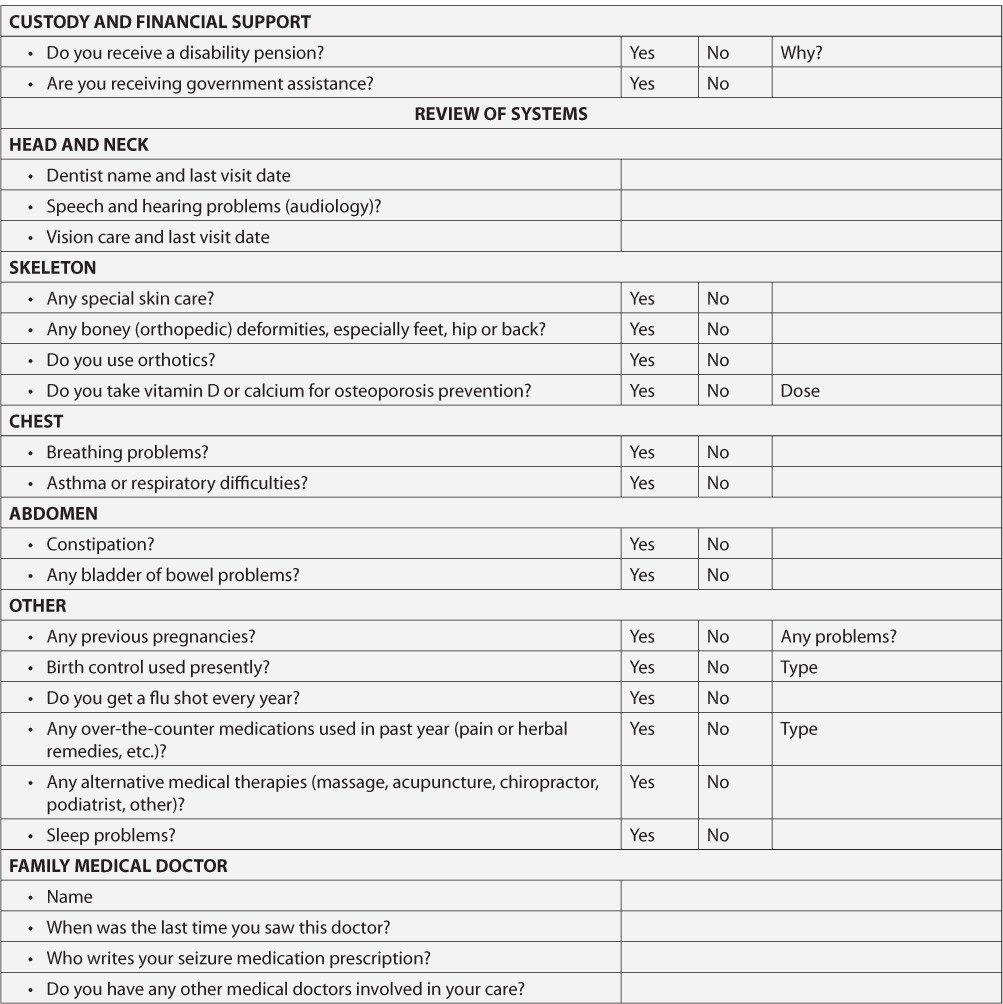
Appendix 3.
References
- 1.Camfield CS, Camfield PR. Long-term social outcomes for children with epilepsy. Epilepsia. 2007;48(suppl):3–5. doi: 10.1111/j.1528-1167.2007.01390.x. [DOI] [PubMed] [Google Scholar]
- 2.Camfield C, Camfield P. Twenty years after childhood-onset symptomatic generalized epilepsy the social outcome is usually dependency or death: A population-based study. Dev Med Child Neurol. 2008;50:859–863. doi: 10.1111/j.1469-8749.2008.03165.x. [DOI] [PubMed] [Google Scholar]
- 3.Camfield C, Camfield P, Gordon K, Smith B, Dooley J. Outcome of childhood epilepsy: A population-based study with a simple predictive scoring system for those treated with medication. J Pediatr. 1993;122:861–868. doi: 10.1016/s0022-3476(09)90008-7. [DOI] [PubMed] [Google Scholar]
- 4.Geerts A, Arts WF, Stroink H, Peeters E, Brouwer O, Peters B, Laan L, van Donselaar C. Course and outcome of childhood epilepsy: A 15-year follow-up of the Dutch Study of Epilepsy in Childhood. Epilepsia. 2010;51:1189–1197. doi: 10.1111/j.1528-1167.2010.02546.x. [DOI] [PubMed] [Google Scholar]
- 5.Erik Erikson. The Life Cycle Completed. New York: W. W. Norton; 1998. [Google Scholar]
- 6.Ingersoll GM. Psychological and social development. In: McAnarney E, editor. Textbook of Adolescent Medicine. London: Elsevier; 1992. In. ed. [Google Scholar]
- 7.Austin JK, Shafer PO, Deering JB. Epilepsy familiarity, knowledge, and perceptions of stigma: Report from a survey of adolescents in the general population. Epilepsy Behav. 2002;3:368–375. doi: 10.1016/s1525-5050(02)00042-2. [DOI] [PubMed] [Google Scholar]
- 8.Collins TB, Camfield PR, Camfield CS, Lee K. People with epilepsy are often perceived as violent. Epilepsy Behav. 2007;10:69–76. doi: 10.1016/j.yebeh.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Jalava M, Sillanpää M, Camfield C, Camfield P. Social adjustment and competence 35 years after onset of childhood epilepsy: A prospective controlled study. Epilepsia. 1997;38:708–715. doi: 10.1111/j.1528-1157.1997.tb01241.x. [DOI] [PubMed] [Google Scholar]
- 10.Wirrell EC, Camfield CS, Camfield PR, Dooley JM, Gordon KE, Smith B. Long-term psychosocial outcome in typical absence epilepsy: Sometimes a wolf in sheep's clothing. Arch Pediatr Adolesc Med. 1997;151:152–158. doi: 10.1001/archpedi.1997.02170390042008. [DOI] [PubMed] [Google Scholar]
- 11.Camfield CS, Camfield PR. Juvenile myoclonic epilepsy 25 years after seizure onset: A population-based study. Neurology. 2009;73:1041–1045. doi: 10.1212/WNL.0b013e3181b9c86f. [DOI] [PubMed] [Google Scholar]
- 12.Camfield P, Camfield C. Idiopathic generalized epilepsy with generalized tonic-clonic seizures (IGE-GTC): A population-based cohort with >20 year follow up for medical and social outcome. Epilepsy Behav. 2010;18:61–63. doi: 10.1016/j.yebeh.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Miller SM, Chan F. Predictors of life satisfaction in individuals with intellectual disabilities. J Intellect Disabil Res. 2008;52:1039–1047. doi: 10.1111/j.1365-2788.2008.01106.x. [DOI] [PubMed] [Google Scholar]
- 14.Wakamoto H, Nagao H, Masatoshi H, Takehiko M. Long-term medical, educational, and social prognoses of childhood-onset epilepsy: A population-based study in a rural district of Japan. Brain Dev. 2000;22:246–255. doi: 10.1016/s0387-7604(00)00121-2. [DOI] [PubMed] [Google Scholar]
- 15.Gilliam F, Penovich PE, Eagan CA, Stern JM, Labiner DM, Onofrey M, Holmes GL, Mathis E, Cramer J. Conversations between community-based neurologists and patients with epilepsy: Results of an observational linguistic study. Epilepsy Behav. 2009;16:315–320. doi: 10.1016/j.yebeh.2009.07.039. [DOI] [PubMed] [Google Scholar]
- 16.Schappert S. Office visits to neurologists, United States 1900–1992: Vital and health statistics of the National Centre for Health Statistics. Advance Data. 1995;267:1–20. [PubMed] [Google Scholar]
- 17.Appleton RE, Chadwick D, Sweeney A. Managing the teenager with epilepsy: Paediatric to adult care. Seizure. 1997;6:27–30. doi: 10.1016/s1059-1311(97)80049-0. [DOI] [PubMed] [Google Scholar]
- 18.Smith PE, Myson V, Gibbon F. A teenager epilepsy clinic: Observational study. Eur J Neurol. 2002;9:373–376. doi: 10.1046/j.1468-1331.2002.00418.x. [DOI] [PubMed] [Google Scholar]
- 19.Jurasek L, Ray L, Quigley D. Development and implementation of an adolescent epilepsy transition clinic. J Neurosci Nurs. 2010;42:181–189. doi: 10.1097/jnn.0b013e3181e26be6. [DOI] [PubMed] [Google Scholar]


