Abstract
Background
Cholera is endemic in Malawi with seasonal outbreaks during the wet season. People living around Lake Chilwa rely on the lake for their water supply. From May 2009 to May 2010, a cholera outbreak occurred in fishing communities around Lake Chilwa. This paper describes the outbreak response and lessons learned for prevention and management of future outbreaks.
Methods
Starting in January 2010, Médecins Sans Frontières (MSF) helped District Health Management Teams (DHMTs) to distribute educational materials, water disinfectant and hygiene supplies, and oral rehydration solution (ORS) in fishing communities. MSF also supported case management by mentoring health workers and providing equipment and supplies.
Results
A total of 1,171 cholera cases and 21 deaths were reported in the districts around the lake, with cases also being reported on the Mozambican side of the lake. The attack rate was highest among people living on or around the lake, particularly among fishermen. Samples of lake water had high turbidity conducive to the propagation of Vibrio cholerae.
Conclusion
A number of practical measures could be taken to prevent future outbreaks and to manage outbreaks more effectively. These measures should address surveillance, environmental management, outbreak preparedness, and case management.
Background
Cholera is endemic in Malawi with seasonal outbreaks.1 Cholera was first reported in 1973 when the seventh pandemic wave hit east Africa.1–2 The first major outbreak occurred in 1989–1990.1
This was followed by major outbreaks in 1993 and 1999. The largest outbreak occurred from October 2001 to April 2002, and affected 26 of the 28 districts. From May 2009 to May 2010, a cholera outbreak occurred in fishing communities on and around Lake Chilwa. A total of 1,171 cholera cases and 21 deaths were reported in the three districts around the lake during this period (attack rate: 74.6 per 100,000; case fatality rate: 1.1%), with cases also being reported on the Mozambican side of the lake.
The Cholera Surveillance Unit in the Ministry of Health (MOH) divides the year into wet and dry seasons, and uses 1 November as the start of the annual reporting period. The wet season runs from the beginning of November until the end of May, and the dry season runs from the beginning of June until the end of October. In the Southern Region, several districts, including Blantyre, Thyolo and Chikhwawa, experience cholera outbreaks during the wet season. The Machinga, Zomba and Phalombe Districts, which border on Lake Chilwa (Figure 1), experience cholera outbreaks more commonly during the wet season, but also experience outbreaks during the dry season. Lake Chilwa is the second largest lake in Malawi and straddles the Malawi-Mozambique border. People living on and around the lake use the lake as a source of drinking water and for their ablutions. Levels of faecal contamination are high, particularly in parts of the lake with stagnant water.
Health surveillance assistants (HSAs) employed by the MOH distribute 1% stock solution to people living in communities around Lake Chilwa every few months. In addition, several nongovernmental organisations (NGOs) provide water treatment products at a subsidised price. These include WaterGuard, a 0.6% solution of sodium hypochlorite distributed by Population Services International (PSI); and PUR®, a powdered chemical sedimentation disinfectant licensed to Proctor and Gamble.3 Water disinfection measures have been shown to reduce diarrhoeal disease and death.4–6
Approximately 6,000 fishermen fish on the lake, many living in floating homes (vimbowela) on the lake, in clusters of 10 to 16 people. It generally takes at least an hour to reach land by boat and about 3 hours to reach land by canoe. Fishermen in these communities may remain on the lake for up to three months at a time without coming ashore. Due to their remoteness from land, fishermen living on the lake have very limited access to water disinfectants and health facilities.
Description of the outbreak
The 2009–2010 cholera outbreak began in Machinga District in May 2009. Cases were diagnosed using the MOH clinical case definition of acute profuse watery diarrhoea, with or without vomiting, in the absence of fever or abdominal pain, in persons aged 5 years or older. The three districts adjacent to Lake Chilwa (Zomba, Machinga, and Phalombe) were the worst affected.7
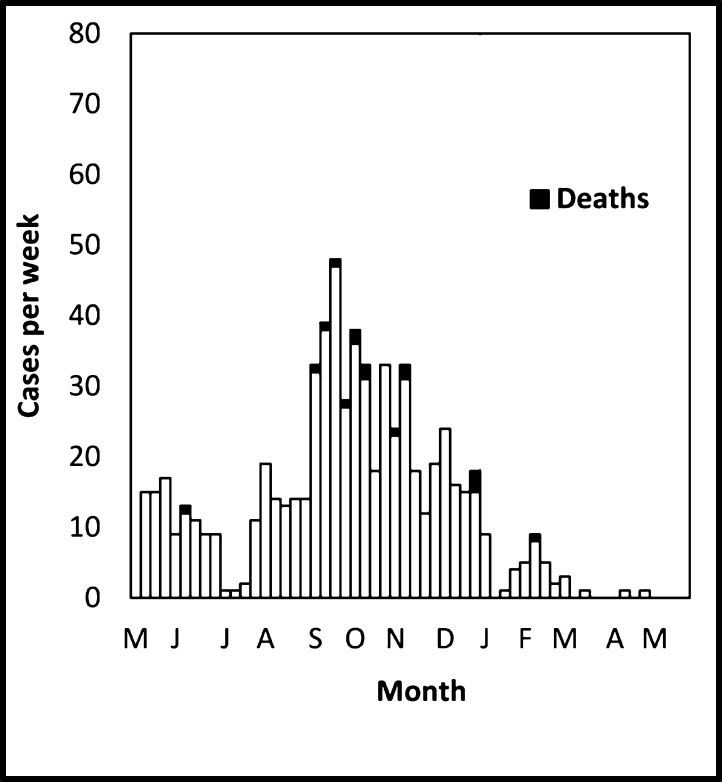
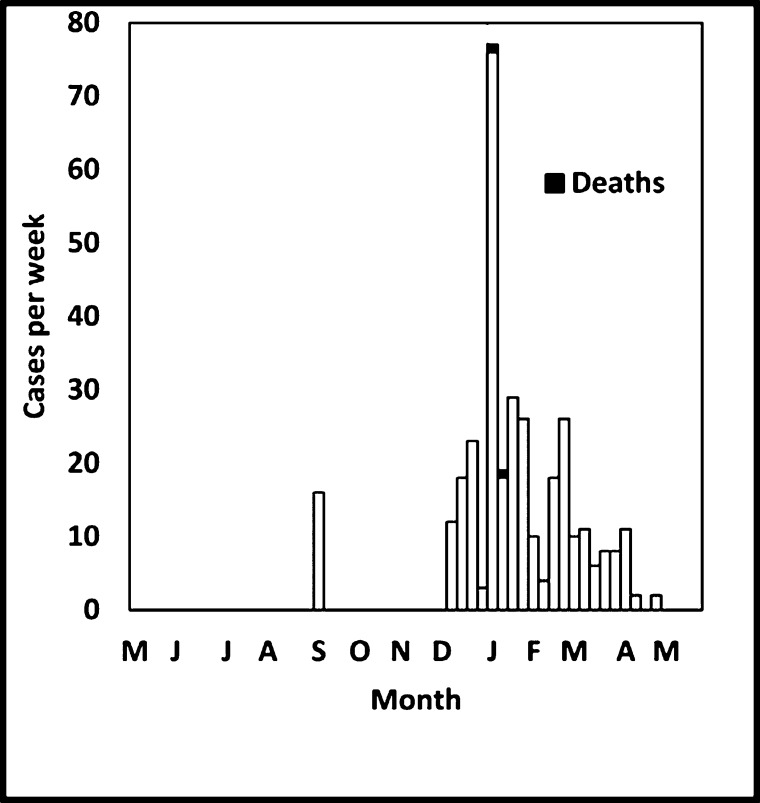
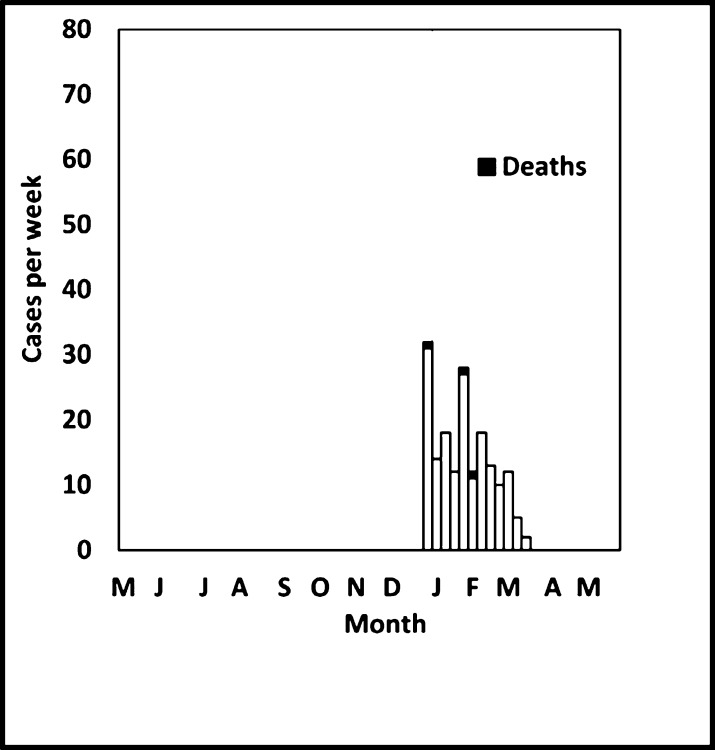
In Machinga District, the outbreak started in May 2009 and lasted until the end of April 2010 with the number of cases peaking in September 2009 (Figure 2a). During this period, 220 cases were reported, with 4 deaths (case fatality rate [CFR]: 2%). In Zomba District, the outbreak started in December 2009 and lasted until the end of April 2010, with the number of cases peaking in early January 2010 (Figure 2b). During this period, 324 cases were reported, with one death (CFR 0.3%). In Phalombe District, the outbreak started towards the end of December 2009 and lasted until the middle of March 2010, with the number of cases peaking during the first week (Figure 2c). During this period, 176 cases were reported, with three deaths (CFR 1.7%).
Fig 2a.
Machinga District
Fig 2b.
Zomba District
Fig 2c.
Phalombe District
The attack rate was highest among people living on or around the lake, with the number of cholera cases decreasing with increasing distance from the lake. Health staff reported that the outbreak predominantly affected fishermen and fish traders, but this could not be confirmed because occupation is not reported on the standard case notification form. Several other districts remote from Lake Chilwa reported cases of cholera during the wet season towards the end of 2009 and in early 2010. In November 2009, MSF staff received reports of cases of cholera in Blantyre and Thyolo, linked to a businessman who had bought fish at Lake Chilwa, and subsequently received reports of the outbreak in Machinga District. The laboratory at Queen Elizabeth Hospital in Blantyre isolated Vibrio cholerae in stool samples of the early cases in Blantyre.
In January 2010, staff from MSF conducted a rapid assessment to assess how MSF could contribute to outbreak management and response. This assessment met the MSF Ethics Review Board-approved criteria for analysis of routinely-collected programme data, and did not therefore require formal ethics review.
A record review of cholera cases admitted to a health facility in Machinga District in November 2009 showed that 70 of 74 cases (95%) were male. Patients' age ranged from 7 to 70 years with a median of 27 years. Only five cases (7%) were in children under 15 years of age. This demographic profile supports health worker reports that the majority of cases were fishermen and fish traders. Three of the 74 cases were fatal (CFR: 4%).
Although water samples were not tested to confirm the presence of Vibrio cholerae, circumstantial evidence suggests that untreated lake water is likely to have been the primary source of infection. Of the 23 cholera patients admitted to health facilities in Machinga District in November 2009 with information recorded on possible sources of exposure, all reported drinking untreated lake water. All three samples of lake water taken on 5 January 2010, that were tested using a turbidity tube and a conductivity meter, found a high turbidity and a high mineral content: A high mineral content and a high algae concentration are conducive to the propagation of V. cholerae.8
Outbreak response
Staff working at MSF in Thyolo District, located about 80 kilometres from Lake Chilwa, did not become aware of the outbreak until relatively late in the course of the outbreak. During the first week of January 2010.
District to conduct a rapid assessment of the outbreak, and to assess whether MSF could assist district health authorities with control measures and case management. The MSF team had meetings with District Health Management Teams (DHMTs), visited affected sites, reviewed case registers, and interviewed health workers and fishermen.
From January to March 2010, MSF supported the outbreak response and case management in Machinga, Zomba and Phalombe Districts, under the oversight of the MOH, working in partnership with local NGOs, including Emmanuel International, Clinton HIV/AIDS Initiative (CHAI) and Population Services International (PSI).
Control Measures
From 26 January to 1 February 2010, two six-person teams, consisting of a supervisory HSA and two additional HSAs employed by MOH, two boat riders, and a person from MSF. The teams distributed water storage containers, supplies of water disinfectant and soap, and health education materials to 1,793 households (Table 1). The health education materials were adapted to the setting and provided basic information about cholera, hand-washing, creating designated water collection points, and water disinfection.
Table 1.
Materials and Supplies Donated by MSF to People living in Fishing Communities, by District
| District | Fisherman targeted |
Jerry cans |
Water buckets |
Water disinfectant sachets |
Posters | Soap |
| Zomba | 4,000 | 4,000 | 2,000 | 120,000 | 1,000 | 4,000 |
| Machinga | 3,000 | 3,000 | 1,200 | 120,000 | 2,000 | 0 |
| Total | 7,000 | 7,000 | 3,200 | 240,000 | 3,000 | 4,000 |
The teams targeted communities without ready access to clean water in the areas most affected by the outbreak, particularly fishermen living on the lake. Likhonyowa, Lumala and Nayuchi were covered first, and control measures were later extended to Phonde, Chipakwe, Namanja, Ntila and Tholowa.
Case Management
MSF also provided support with case management in MOH-run district health centres. Cases were managed either in tents or in purpose-built cholera shelters attached to health centres. Many health centres had limited supplies and no separate facilities for cholera case management. MSF donated tents, cholera beds and supplies of calcium hypochlorite (HTH) tabs, Ringer's lactate, ORS and gloves (Table 2).
Table 2.
Medical Equipment and Supplies Donated by MSF to District Health Management Teams, by District
| Supplies | Equipment | |||||
| District | HTH tabs |
Ringer's lactate |
Gloves | ORS | Cholera beds |
Tents |
| Zomba | 0 | 820 | 23,600 | 9,286 | 20 | 3 |
| Machinga | 100,000 | 365 | 5,000 | 10,600 | 8 | 2 |
| Phalombe | 112,000 | 800 | 1,500 | 500 | 10 | 2 |
| Total | 212,000 | 1,985 | 30,100 | 20,386 | 38 | 7 |
Donations of equipment and supplies differed in each district, according to the needs identified by district health authorities.
An MSF nurse became directly involved with case management and provided mentorship and guidance to staff without experience in cholera case management. Many patients arrived with severe dehydration and required rehydration with intravenous fluids and ORS. As case management did not address the source of infection, additional cases sometimes occurred in the households of patients who had been discharged. Among some female patients, case registers recorded “taken care of sick husband” as the source of infection.
Discussion and Recommendations
Communities that use untreated lake or river water as a source of drinking water are particularly vulnerable to cholera outbreaks. Similar lake-water associated outbreaks have been reported in other lakes along the Rift Valley of Africa, including Lake Victoria in Kenya,9 Lake Kivu in the Democratic Republic of Congo,10 and Lake Tanganyika in Burundi.11
Cases that were not seen at a health facility were not reported. In addition, cases among children under five years of age were not included in case counts because this age group is excluded from the clinical case definition used by the MOH for case reporting. Although cholera affects people of all ages, children under five are at greatest risk in settings where cholera is endemic.12 Fisherman living on the lake did not have ready access to health centres, and cases among fishermen are likely to have been under-reported. Deaths are also likely to have been under-reported due to some people having limited access to health facilities. Although there was no systematic attempt to count the number of cholera deaths in the community, the outbreak response teams received anecdotal reports of fishermen dying before reaching a health centre.
The Lake Chilwa cholera outbreak revealed several deficiencies in control measures and outbreak preparedness, and provides an opportunity to reflect on practical steps that could be taken to avert and respond more effectively to future outbreaks. The WHO Global Task Force on Cholera Control recommends the following approaches to control and manage epidemics more effectively: improved surveillance; improved environmental management; improved preparedness; improved case management; research into drug resistance; use of available vaccines; partnerships; and health education.13
Improving surveillance
Currently, cholera case notifications are submitted to the MOH Cholera Surveillance Unit. This unit conveys this information to the National Epidemiology Unit, which produces and distributes weekly cholera reports. The cholera surveillance system could be strengthened by improving the dissemination of cholera reports. MSF, which has considerable experience in responding rapidly to cholera outbreaks, having recently assisted with the management of major outbreaks in Zimbabwe, Mozambique, Pakistan, Haiti and the Democratic Republic of Congo, could have volunteered assistance sooner, had the organisation become aware of the outbreak sooner. Surveillance could also be improved by training HSAs to carry out active case-finding during community work. The National Epidemiology Unit uses 1 November each year as the start of the cholera reporting season. Although it is necessary to have clearly defined reporting periods, in an outbreak setting it is important to keep count of the cumulative number of cases since the start of the outbreak. Starting cumulative case counts on 1 November 2009, and ignoring earlier cases in Machinga District, may have led health authorities to underestimate the magnitude of the outbreak, and this may have delayed the response.
Improving environmental management
Improving water and sanitation measures should be the mainstay of cholera prevention efforts.14 A review published in 2002, ranked Malawi's Water Poverty Index 143rd out of the 147 countries reviewed.15 Since then, progress has been made towards improving water and sanitation.16 In 2006, 76 percent of the population had access to an improved water source, and 60 percent had access to proper sanitation facilities.1 The 2006 Malawi Growth and Development Strategy Paper identified development of a water and sanitation infrastructure as one of six key priorities; and in 2008, cabinet adopted a National Sanitation Policy.16 Despite these initiatives, water and sanitation remains inadequate in many districts. The WHO Global Task Force on Cholera Control13 advocates that arrangements be made for the protection of water sources to reduce the risk of water contamination. It is not feasible to protect Lake Chilwa from contamination at source, given the large bodies of stagnant water. In places where it is not possible to protect water sources, point-of-use measures have been shown to be effective at reducing the incidence of diarrhoea.4–6,17 Sodium hypochlorite, the active ingredient in the 1% stock solution distributed by MOH, is less effective than sedimentation disinfectants for treating highly turbid water such as that found in Lake Chilwa.4,18 Since the outbreak, the supply and distribution of chemical sedimentation disinfectants has become sporadic. Funding needs to be secured, and a means established to resume the distribution of chemical sedimentation disinfectants, and water disinfectants should be stockpiled for use in future outbreaks.
Improving outbreak preparedness
Outbreak preparedness could be improved by developing district cholera emergency plans and stockpiling equipment and supplies needed for outbreak management. Outbreak preparedness plans should cover the essential elements of an outbreak response including coordination and logistics; human resources; training and staff responsibilities; availability of financial support; plans for the implementation of control measures, including provision of safe water; plans for education campaigns; support for laboratory confirmation of outbreaks; and monitoring and evaluation of control activities.
Improving case management
WHO recommends stockpiling supplies and holding cholera preparedness sessions for involved parties.14 In Malawi, where cholera outbreaks follow seasonal patterns, training health workers at the start of each wet season would help to increase awareness; ensure accurate diagnosis; and ensure good case management. During the outbreak, many health facilities were not adequately equipped to manage large numbers of cholera cases. This could be addressed by establishing cholera stations at health centres, and by maintaining stocks of tents, drip stands, cholera beds, and supplies, so that cholera stations can be set up rapidly in the event of an outbreak.
Antibiotics were generally not used to treat cholera cases during the outbreak. The WHO cholera treatment protocol recommends that antibiotics be used to treat severe cases (>10% dehydration),19 and some authorities recommend that antibiotics also be used moderate cases (5–10% dehydration), with the choice of antibiotic determined by the resistance pattern of the outbreak strain.20 In future outbreaks, laboratories should carry out culture for Vibrio cholerae during the early stages of the outbreak to confirm that it is a cholera outbreak, and perfom sensitivity testing of isolates to guide the choice of antibiotics, as was done in a previous outbreak.21
Use of vaccines
In 2010, WHO issued an updated recommendation that vaccination should be considered in areas where cholera is endemic, and for use in controlling outbreaks.14 Injectable cholera vaccines are not recommended for use by WHO due to low efficacy; limited duration of protection; and an unfavourable safety profile.22 Recently, safer and more effective oral cholera vaccines have been developed. The WHO position paper14 stresses that vaccines should only be considered for use in conjunction with other cholera prevention and control measures, and that vaccination should not disrupt the implementation of such measures. Mass vaccination of the general population is not recommended.
There are two types of oral cholera vaccines currently available: (1) killed monovalent whole cell (Dukoral); and (2) killed bivalent whole cell without toxin B subunit (Shanchol and mORCVAX). Dukoral is used primarily by travellers from non-endemic settings, but has been used effectively in some outbreak settings, including an urban outbreak in Beira, Mozambique.22–24 There are several promising live attenuated oral cholera vaccines in development which have the potential advantage of stimulating an immune response similar to natural cholera. The first of these is likely to receive WHO pre-qualification in 2013. Currently available vaccines have several practical disadvantages, including the need to administer two doses, so they are currently not a feasible option in settings such as Lake Chilwa. Vaccination could be considered for use in future outbreaks if obstacles to their use can be overcome.
Partnerships
WHO recommends that mechanisms should be established for ensuring good collaboration between volunteers from NGOs and MOH health care workers in the field.13 During the Lake Chilwa outbreak, different players worked well together, but because of the lack of cholera control committees, valuable time was lost in implementing control measures. Coordination between district health management teams (DHMTs) and organisations providing water and sanitation services, health promotion, and emergency medical services could be improved by establishing a cholera control committee in each district.
Health education
During the Lake Chilwa outbreak there was a shortage of suitable educational materials, and minimal health promotion activities were in place to inform fisherman about cholera prevention and management, thus people in the affected areas continued to use untreated water. This could be addressed by increasing the availability of appropriate education materials, and using HSAs to provide cholera health education and to distribute disinfectants, soap, and water storage containers. Health education materials should include information about symptoms of cholera; where to get treatment in the event of symptoms; water disinfection and safe water storage; washing hands with soap and clean water after performing ablutions and before and after handling fish; and cooking food thoroughly.
Aftermath of the 2009/2010 cholera outbreak
During the year following the outbreak, there were no subsequent cholera outbreaks in the area. However, as problems with water quality persist and prevention and preparedness measures remain inadequate, further cholera outbreaks are likely to occur in the future. Surveillance mechanisms need to be maintained; water and sanitation problems addressed; prevention measures and outbreak response improved; and a state of outbreak preparedness maintained in order to prevent, and respond more effectively, to future outbreaks.
Acknowledgements
We thank Marc Biot and Michel van Herp of Médecins Sans Frontières in Brussels for their critical review of the manuscript and their helpful comments and suggestions.
References
- 1.WHO, author. Cholera Country Profile 2010: Malawi. [5 July 2011]. Available at: http://www.who.int/cholera/countries/MalawiCountryProfile2010.pdf.
- 2.Swerdlow DL, Malenga G, Begkoyian G, Nyangulu D, Toole M, Waldman RJ, Puhr DN, Tauxe RV. Epidemic cholera among refugees in Malawi, Africa: treatment and transmission. Epidemiol Infect. 1997;118(3):207–214. doi: 10.1017/s0950268896007352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.News Release: USAID and P&G Highlight Partnership for Safe Drinking Water in Africa. Washington, DC: 2007. Mar 6, [5 July 2011]. Available at: http://www.pginvestor.com/phoenix.zhtml?c=104574&p=irolnewsArticle&ID=970936&highlight= [Google Scholar]
- 4.Crump JA, Otieno PO, Slutsker L, Keswick BH, Rosen DH, Hoekstra RM, Vulule JM, Luby SP. Household based treatment of drinking water with flocculant-disinfectant for preventing diarrhoea in areas with turbid source water in rural western Kenya: cluster randomised controlled trial. BMJ. 2005;331:478. doi: 10.1136/bmj.38512.618681.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chiller TM, Mendoza CE, Lopez MB, Alvarez M, Hoekstra RM, Keswick BH, Luby SP. Reducing diarrhoea in Guatemalan children: randomized controlled trial of flocculantdisinfectant for drinking-water. Bull World Health Organ. 2006;84:28–35. doi: 10.2471/blt.04.016980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clasen T, Schmidt WP, Rabie T, Roberts I, Cairncross S. Interventions to improve water quality for preventing diarrhoea: systematic review and meta-analysis. BMJ. 2007;334:782. doi: 10.1136/bmj.39118.489931.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malawi Ministry of Health, author. Weekly Cholera Reports. Lilongwe: MOH; 2009 – 2011. [Google Scholar]
- 8.Constantin de Magny G, Murtugudde R, Sapiano MR, Nizam A, Brown CW, Busalacchi AJ, Yunus M, Nair GB, Gil AI, Lanata CF, Calkins J, Manna B, Rajendran K, Bhattacharya MK, Hug A, Sack RB, Colwell RR. Environmental signatures associated with cholera epidemics. Proc Natl Acad Sci USA. 2008;105:17676–17681. doi: 10.1073/pnas.0809654105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro RL, Otieno MR, Adcock PM, Phillips-Howard PA, Hawley WA, Kumar L, Waiyaki P, Nahlen BL, Slutsker L. Transmission of epidemic Vibrio cholerae O1 in rural western Kenya associated with drinking water from Lake Victoria: an environmental reservoir for cholera? Am J Trop Med Hyg. 1999;60(2):271–276. doi: 10.4269/ajtmh.1999.60.271. [DOI] [PubMed] [Google Scholar]
- 10.Bompangue D, Giraudoux P, Piarroux M, Mutombo G, Shamavu R, Sudre B, Mutombo A, Mondonge V, Piarroux R. Cholera epidemics, war and disasters around Goma and Lake Kivu: an eight-year survey. PLoS Negl Trop Dis. 2009;3(5):e436. doi: 10.1371/journal.pntd.0000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birmingham ME, Lee LA, Ndayimirije N, Nkurikiye S, Hersh BS, Wells JG, Deming MS. Epidemic cholera in Burundi: patterns of transmission in the Great Rift Valley Lake region. Lancet. 1997;349(9057):981–985. doi: 10.1016/S0140-6736(96)08478-4. [DOI] [PubMed] [Google Scholar]
- 12.Deen JL, von Seidlein L, Sur D, Agtini M, Lucas ME, Lopez AL, Kim DR, Ali M, Clemens JD. The high burden of cholera in children: comparison of incidence from endemic areas in Asia and Africa. PLoS Negl Trop Dis. 2008;2:e173. doi: 10.1371/journal.pntd.0000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO, author. Global Task Force on Cholera Control. Cholera Unveiled. Geneva: WHO; 2003. [5 July 2011]. Available at: http://whqlibdoc.who.int/hq/2003/WHO_CDS_CPE_ZFK_2003.3.pdf. [Google Scholar]
- 14.WHO, author. Cholera vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85:117–128. [PubMed] [Google Scholar]
- 15.Lawrence p, Meigh J, Sullivan C. The Water Poverty Index: an international comparison. Natural Resources Forum. 2003;3:189–199. [Google Scholar]
- 16.DeGabrielle J. Water Supply and Sanitation Collaborative Council. Sanitation Sector Status and Gap Analysis: Malawi. September, 2009. Lilongwe: Global Sanitation Fund; 2009. [Google Scholar]
- 17.Colindres RE, Jain S, Bowen A, Mintz E, Domond P. After the flood: an evaluation of inhome drinking water treatment with combined flocculent-disinfectant following Tropical Storm Jeanne — Gonaives, Haiti, 2004. J Water Health. 2007;5(3):367–374. doi: 10.2166/wh.2007.032. [DOI] [PubMed] [Google Scholar]
- 18.Crump JA, Okoth GO, Slutsker L, Ogaja DO, Keswick BH, Luby SP. Effect of point-of-use disinfection, flocculation and combined flocculation-disinfection on drinking water quality in western Kenya. J Appl Microbiol. 2004;97:225–231. doi: 10.1111/j.1365-2672.2004.02309.x. [DOI] [PubMed] [Google Scholar]
- 19.WHO Global Task Force on Cholera Control, author. Prevention and control of cholera outbreaks: WHO policy and recommendations. [5 July 2011]. Available at: http://www.who.int/cholera/technical/prevention/control/en/index.html.
- 20.Nelson EJ, Nelson DS, Salam MA, Sack DA. Antibiotics for both moderate and severe cholera. N Engl J Med. 2011;364:5–7. doi: 10.1056/NEJMp1013771. [DOI] [PubMed] [Google Scholar]
- 21.Zachariah R, Harries AD, Arendt V, Nchingula D, Chimtulo F, Courteille O, Kirpach P. Characteristics of a cholera outbreak, patterns of Vibrio cholerae, and antibiotic susceptibility testing in rural Malawi. Trans Royal Soc Trop Med Hyg. 2002;96:39–40. doi: 10.1016/s0035-9203(02)90233-6. [DOI] [PubMed] [Google Scholar]
- 22.Shin S, Desai SN, Sah BK, Clemens JD. Oral vaccines against cholera. Clin Infect Dis. 2011;52:1343–1349. doi: 10.1093/cid/cir141. [DOI] [PubMed] [Google Scholar]
- 23.Cavailler P, Lucas M, Perroud V, McChesney M, Ampuero S, Guérin PJ, Legros D, Nierle T, et al. Feasibility of a mass vaccination campaign using a two-dose oral cholera vaccine in an urban cholera-endemic setting in Mozambique. Vaccine. 2006;24:4890–4895. doi: 10.1016/j.vaccine.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Lucas ME, Deen JL, von Seidlein L, Wang XY, Ampuero J, Puri M, Ali M, Ansaruzzaman M, Amos J, Macuamule A, Cavailler P, Guerin PJ, Mahoudeau C, Kahozi-Sangwa P, Chaignat CL, Barreto A, Songane FF, Clemens JD. Effectiveness of mass oral cholera vaccination in Beira, Mozambique. N Engl J Med. 2005;352:757–767. doi: 10.1056/NEJMoa043323. [DOI] [PubMed] [Google Scholar]