Abstract
The Hospital Elder Life Program (HELP), an effective intervention to prevent delirium among hospitalized elders, has been successfully replicated in a community teaching hospital as a quality improvement project. Now, we report on successfully sustaining the program over 7 years and expanding its scale from 1 to 6 inpatient units at the same hospital. The program currently serves over 7000 older patients annually and is accepted as the standard of care throughout the hospital. Innovations which enhanced scalability and widespread implementation included ensuring dedicated staffing for the program, local adaptations to streamline protocols, continuous recruitment of volunteers, and more efficient data collection. Outcomes include reduced rate of incident delirium, reduced length of stay, increased satisfaction by patients, families, and nursing staff, and significantly reduced costs for the hospital. The financial return of the program, estimated at over $7.3 million per year during 2008, is comprised of cost savings from delirium prevention as well as revenue generated from freeing up hospitals beds (reduced length of stay in delirious and non-delirious HELP patients). Delirium poses a major challenge for hospital quality of care, patient safety, Medicare no-pay conditions, and costs of hospital care for older persons. Faced with rising numbers of elderly patients, hospitals can utilize HELP to improve both the quality and cost-effectiveness of care.
Keywords: delirium, Hospital Elder Life Program (HELP) , intervention, prevention, hospital care, sustainability
INTRODUCTION
Delirium is a frequent and costly complication of hospitalization for older persons. Since it is often iatrogenic, delirium serves as an important health care quality indicator for older hospitalized persons, and it is included as a quality of care measure in the Agency for Healthcare Research and Quality (AHRQ) National Quality Measures Clearinghouse (NQMC) <http://www.qualitymeasures.ahrq.gov>. Previous studies indicate that for each hospitalization in older patients with delirium, on average $2,500 of hospital costs are attributable to delirium (1). This amounts to over $6.5 billion (2004 USD) of Medicare hospital expenditures related to delirium. Substantial additional costs estimated at over $100 billion per year (2) accrue after hospital discharge because of the increased need for nursing home care, rehabilitation services, formal home health care, and informal caregiving costs. Moreover, with the aging of the U.S. population, delirium is a problem that is likely to increase in the future. Finding ways to prevent delirium, such as the Hospital Elder Life Program (HELP) program, will allow us to improve quality of life and efficiency of healthcare for these vulnerable patients.
The Hospital Elder Life Program (HELP) <www.hospitalelderlifeprogram.org> is an innovative model of care, designed to prevent delirium and functional decline in hospitalized older persons (3,4). The program provides skilled interdisciplinary staff and trained volunteers to carry out intervention protocols targeted toward six delirium risk factors: orientation, therapeutic activities, early mobilization, vision and hearing protocols, oral volume repletion, and sleep enhancement. The program is designed to be superimposed on existing hospital units, and does not require a separate, dedicated geriatric unit. HELP has been demonstrated to be effective for prevention of delirium, as well as for prevention of cognitive and functional decline (3–5). Cost-effectiveness has been demonstrated previously for both acute hospital costs (6) and for long-term nursing home placement costs (7). In addition, cost savings have been demonstrated previously at our site (8), and in Australia in a capitated system (9). Finally, the HELP model is effective for prevention of falls, pressure sores, and other iatrogenic complications of hospitalization (10–11). The unique strengths of the HELP model, which contribute to its effectiveness, include the targeted nature of the interventions, early intervention focusing on prevention, well-trained staff dedicated to the program, standardized intervention protocols, tracking of adherence to all protocols, and built-in quality assurance procedures (4). Currently, the program has been disseminated to over 60 hospitals in the U.S., Canada, United Kingdom, Australia, and Taiwan.
The purpose of the current study is to describe the evolution of the HELP program at Shadyside over the 7 year period from 2002–2008 (inclusive), including the adaptations, patient outcomes, cost savings, challenges and successes.
METHODS
Evolution of the HELP model of care at Shadyside
University of Pittsburgh Medical Center (UPMC) Presbyterian Shadyside, Shadyside campus, is a 500 bed community teaching hospital in Pittsburgh, PA created by the merger of Presbyterian University Hospital and Shadyside Hospital, which retains the culture of community-based clinical practice. A full description of the HELP program is provided in previous studies (4–5). Overall, the HELP model at Shadyside retains a high degree of fidelity with the original HELP model, in terms of staffing, operational structure, interventions, and quality assurance procedures. While the intent at Shadyside was to conduct all of the HELP interventions, Shadyside made pragmatic adaptations at the outset to some of the original HELP processes and procedures. All of our volunteers received the complete training program developed at Yale; however, because of a shortage of volunteers, we omitted the mobility and volume repletion protocols during the initial months. After we had successfully recruited and trained sufficient volunteers, these protocols were implemented. The sleep protocol was modified to include hand rather than back massage. Unit-wide noise reduction strategies were already being implemented throughout the hospital prior to HELP. Some of our volunteers were trained by speech therapists in an enhanced feeding protocol. Additionally, some were trained by physical therapists in an enhanced mobilization protocol. The role of our Elder Life Nurse Specialist was modified to omit discharge planning, linkages with community agencies, and post-discharge follow-up with patients, because these functions were already being performed by other hospital personnel. Finally, our HELP program provides some services to all patients over age 70 whether or not they meet HELP criteria. However, we prioritize patients meeting the HELP criteria, especially those at intermediate risk for delirium (1–2 risk factors by a previously developed predictive model (12)).
Dissemination process
HELP at Shadyside began in 2002 on one 40-bed medical unit. We enrolled all patients age 70 and older on this unit who met the HELP criteria. By 2008 it was active on 6 units, involving 184 hospital beds. The hospital dissemination proceeded in a methodical fashion. Initially, we worked with hospital leadership to determine the metrics for measuring success. These included: reduced rate of delirium; no increased burden on nursing staff; favorable satisfaction ratings by patients, families, nurses, and nursing assistants; and net costs either unchanged or reduced. We obtained private foundation support for our first year of operation. The hospital granted us access to an analyst in the fiscal department who used the hospital administrative database to conduct analyses comparing patients enrolled in HELP with controls, and comparing patients with delirium to similar patients without delirium. We utilized a proxy measure, as described previously (8) to identify delirious patients at baseline prior to implementation of HELP, and subsequently to track the effectiveness of HELP on the incidence of delirium over time. After 2004, the proxy measure was no longer used; we used direct bedside assessment by the Elder Life nurse specialist, described below.
Because we demonstrated initial success based on the proposed metrics, our hospital leadership agreed to continue funding for HELP and allowed us to expand to additional units. Before beginning HELP on a new unit, we met with each nursing unit director and solicited their input. Since we extensively publicized the program throughout the hospital, the unit director was already aware of HELP prior to this meeting. The publicity included presentations at multiple committee meetings, such as the Board of Directors, wall posters, brochures, and presentations at Grand Rounds, house staff conferences, nursing in-service conferences, and regional continuing medical education (CME) meetings. With the concurrence of the Chief Nursing Officer (CNO), we conducted surveys of the nurses and nursing assistants on each new unit to assess their baseline knowledge about care of the frail elderly in general and about delirium in particular, and whether they enjoyed providing such care. After 6 months of HELP on the unit, we repeated the surveys. We worked closely with our CNO to identify the subsequent units to target for implementation, based upon patient characteristics and logistical considerations. As our volume of patients increased, we added paid HELP staff and volunteers to match the demand. We also designated one Elder Life Specialist as the “lead volunteer coordinator” to provide front-line supervision and coordination of the large pool of volunteers. To allow our nurse specialist to extend her scope, we supplemented her role with a new position filled with a bachelors-prepared nurse.
Maintaining quality
We held weekly meetings of the Hospital Elder Life Program staff, and monthly meetings with the Program Director and a process improvement specialist. We periodically clarified definitions of terms and reviewed our daily processes for uniformity and consistency over time. We documented the modifications made to the original HELP protocols. Volunteer training remained fully standardized and well-documented. In order to work with patients, volunteers were required to demonstrate competence in performing all intervention protocols, and review sessions were conducted three times per year. The staff reviewed the worksheets completed daily by the volunteers to assure adherence, and conducted regular quality checks of each other’s patient assessments.
Program outcomes
Beginning in 2004, rates of delirium were determined by the Elder Life Nurse Specialist during a direct bedside assessment using the Confusion Assessment Method (13) rather than the proxy assessment used at baseline (8). Data on length of stay and hospital costs were derived from the hospital administrative database. We developed a brief satisfaction questionnaire with a Likert-type scale which was administered anonymously to all nurses and nurse’s aides on the HELP units before HELP and repeated 6 months later. A separate Likert-type questionnaire was administered to all patients (or their families) who were in the program for at least 2 days. Patients and families had the option to return these anonymously.
RESULTS
The evolution of the HELP model at Shadyside during the inclusive period from 2002 through 2008 is summarized in Table 1. During this time, the program grew from enrolling 940 patients per year on one unit to over 7,000 patients per year on 6 units. Paid HELP staff increased from 1.8 full-time equivalents to 7.5 during this time period. Volunteers similarly increased from 24 volunteers conducting 5,381 volunteer interventions during start-up in 2002 to over 100 volunteers conducting over 41,000 volunteer interventions in 2008. The program expanded from a single medical unit to include 4 medical, 1 orthopedic, and 1 neurosurgical units. The multiplicative expansion of the program during this timeframe attests to the scalability and generalizability of the HELP interventions.
Table 1.
HELP Model Characteristics at Shadyside
| Year | 2002 | 2005 | 2008 |
|---|---|---|---|
| Total Patients Served to Date, No. | 940 | 4,044 | 27,196 |
| Paid Staff, full-time equivalents | 1.8 | 5.5 | 7.5 |
| Volunteers, No. | 24 | 52 | 107 |
| Volunteer Interventions, No. | 5,381 | 24,000* | 41,880 |
For 2005, exact volunteer hours were not permanently recorded. This estimate based on number of patients served.
Delirium outcome
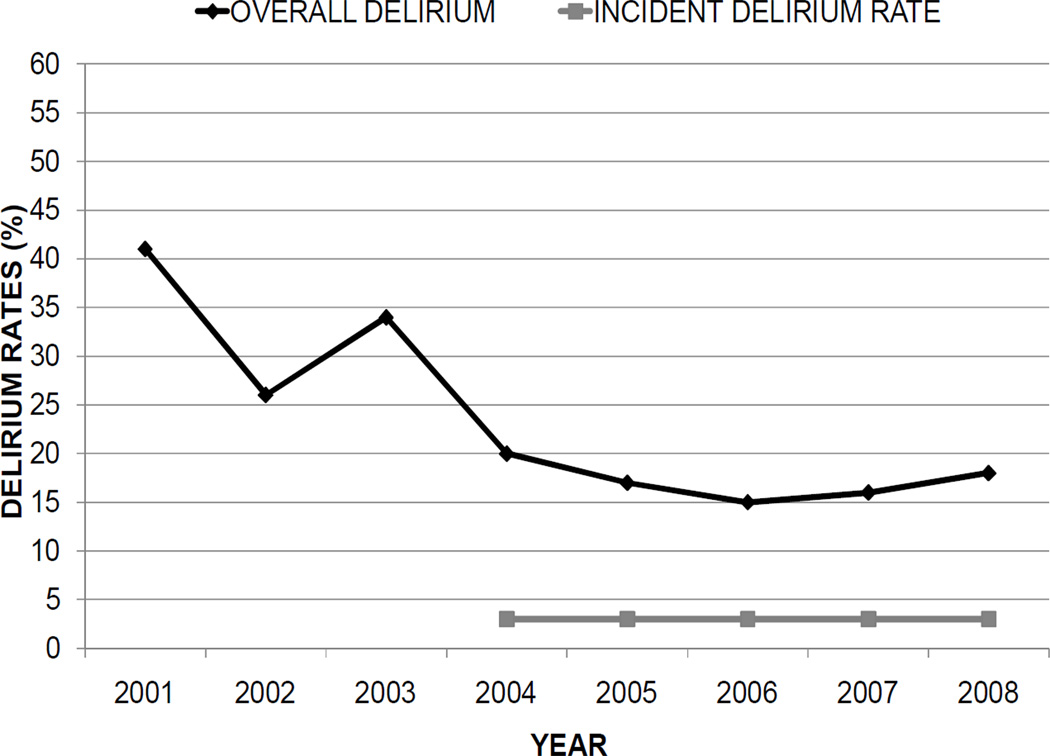
The rates of delirium, including both incident and overall delirium rates, are presented in Table 2 and Figure 1. The overall rate is the sum of incident and prevalent delirium. Since implementation in 2002, delirium rates have declined. The baseline delirium rate was 41% prior to HELP in 2001, based on a proxy measure using methods described previously (8). In brief, the proxy measure was developed using hospital administrative data in all patients age 70 years and older admitted to the HELP units. After excluding patients with a diagnosis of schizophrenia or who were using major tranquilizers at hospital admission, any patient who was newly started on a major tranquilizer (haloperidol, risperidone, or quetiapine) or who was physically restrained during hospitalization was counted as having a delirium marker. The rate obtained was multiplied by a factor of 3, based on correlation with clinical ratings in a pilot study. The proxy measure was subsequently validated against formal delirium assessments by geriatricians and nurse practitioners, and found to be a good approximation of total delirium rate (8). In 2002, the rate was 26%, a decrease of 15% compared to baseline. In 2008, the rate was 18% based on direct observation, a decrease of 23% compared to baseline. Notably, incident delirium—that is, delirium of new onset during hospitalization, remained at 3% or less from 2004–2008, demonstrating the efficacy of the HELP model for primary prevention of delirium in the hospital setting. Although we observed clinically that patients who did become delirious after enrollment in HELP were less severely affected, we did not formally assess severity.
Table 2.
HELP Program Outcomes Over Time
| Year | 2002 | 2005 | 2008 | |
|---|---|---|---|---|
| Outcome | ||||
| Delirium | ||||
| • Delirium rate | 26% | 16% | 18% | |
| • Reduction in delirium* | −15% | −25% | −23% | |
| Patient Satisfaction§ | 2.8/3.0 | 2.8/3.0 | 2.9/3.0 | |
| Nurse Satisfaction∥ | 4.8/5.0 | 4.5/5.0 | ¶ | |
| Length of stay, days: | ||||
| • Delirious patients (reduction from baseline) | 8.8 (1.0) | ¶ | 7.0 (2.8) | |
| • Non-delirious patients (reduction from baseline) | 6.0 (0.1) | ¶ | 5.3 (0.8) | |
| Cost savings, per year‡ | $1.23 million | ¶ | $7.37 million |
Absolute reduction compared with baseline rate pre-HELP (2001) based on proxy data.
Reduction compared with baseline length of stay pre-HELP (2001).
See text and Figure 2 for further details.
Based on 496 responses
Based on 134 responses
Data not collected or not available for this time period
Figure 1. Rates of Delirium over Time at Shadyside Hospital.
Initial delirium rates were based on a proxy measure, described previously, which has been validated against direct observation. Beginning in 2004, rates were based on direct observation by a nurse practitioner, including both incident and overall delirium rates. Low levels of incident delirium have been maintained since 2004, supporting the efficacy of the program for delirium prevention. See text for details.
Other outcomes
Overall patient and nurse satisfaction remained high throughout the study period. Patients reported being highly satisfied with their care on the HELP program. In addition, nurses and nurse’s aides reported benefit and satisfaction with the HELP program, and agreed with the questionnaire item that their job was “more satisfying due to HELP”.
Length of hospital stay decreased in all patients relative to baseline. In delirious patients on the HELP program, length of stay was reduced by 1.0 days in 2002, and by 2.8 days in 2008, relative to delirious patients not receiving HELP at baseline. For patients enrolled in HELP who did not become delirious, length of stay was reduced by 0.1 days in 2002 and 0.8 days in 2008, compared to non-delirious patients not receiving HELP at baseline.
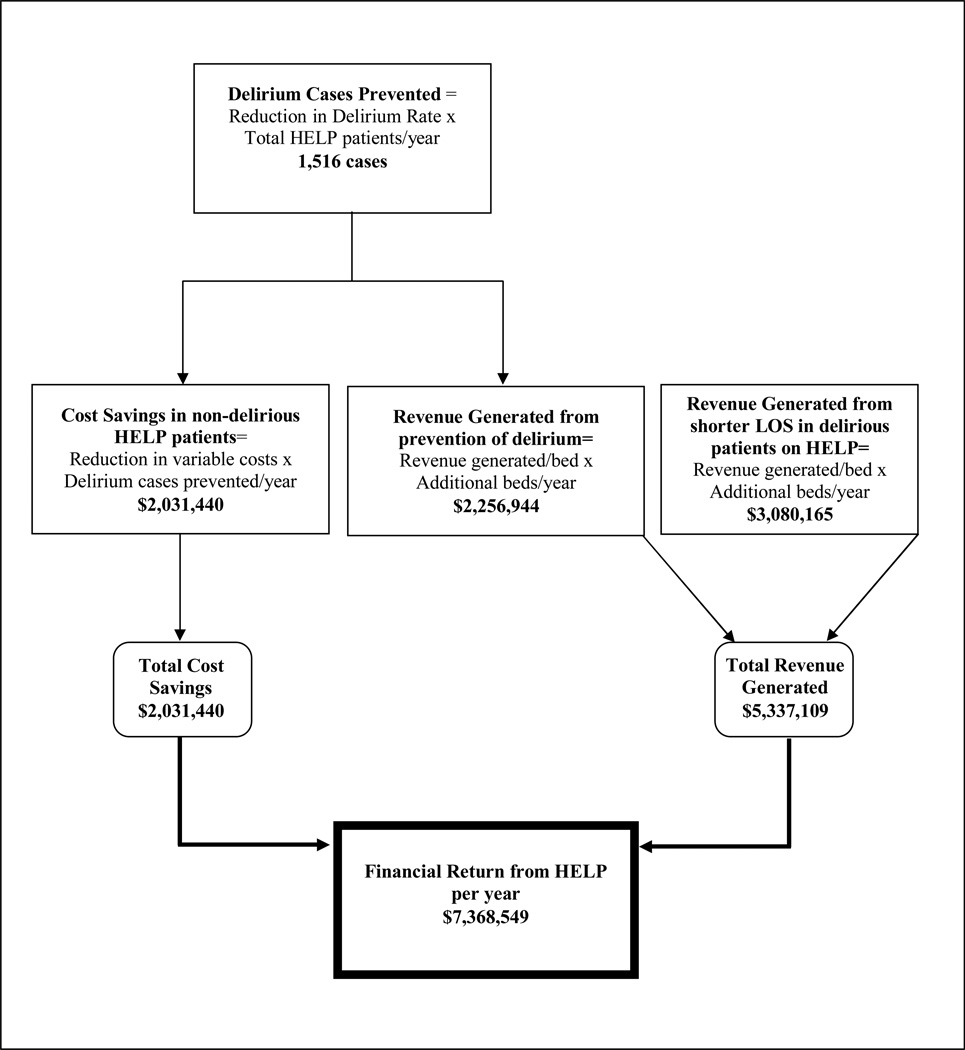
Financial return
The current financial benefits of the HELP program at Shadyside are estimated in Figure 2. These benefits are comprised of both cost-avoidance through delirium prevention and revenue generation through decreasing hospital length of stay, thus increasing the availability of hospital beds. The rate of prevented cases of delirium (23%) was calculated as the difference between the delirium rate at baseline prior to HELP (41%) and the current delirium rate measured in HELP patients (18%). Multiplying the rate of prevented delirium cases by the total number of HELP patients served yields 1,516 cases of delirium prevented. At baseline, the variable costs per delirious patient were $5,785, compared with $4,696 per nondelirious patient. Adjusting for inflation, the variable cost savings are $1,340 (2008 dollars) for each case of delirium prevented. Thus, for the 1,516 cases prevented, the cost savings amount to $2,031,440 per year. For sites that are unable to measure the delirium rates directly, these rates can be estimated either by creation of a proxy delirium rate based on administrative data (8), or a 35% relative delirium rate reduction can be used as the rate of prevented cases of delirium (4,8).
Figure 2. Annual Financial Return from HELP Program at Shadyside.
See text for details on financial calculations. The financial return is based on both cost savings from reduction in variable costs from delirium cases prevented, as well as revenue generated from back-filling of beds now available due to delirium prevention and shortening length of stay in delirious patients on HELP. Further cost savings (not included in figure) accrue from volunteer time contribution.
Revenue generation occurs from the decreased length of hospital stay in non-delirious patients, which in turn, frees up hospital beds to be filled by other patients. The reduced length of stay (LOS) resulting from delirium prevention can be calculated as the difference between LOS in delirious and non-delirious patients. The revenue generated is calculated as the reduced LOS (adjusted) in days X (number of delirium cases prevented/365 days) X annual revenue per hospital bed. For the present study, these values are: 1.3 days X (1516 cases/365 days) X $417,995 = $2,256,944 per year. Notably, the calculations for 2008 are based on actual measurements in HELP patients. Note that the LOS values in these calculations are reduced by 0.5 days to account for global shortening in LOS in Medicare patients between 2001 and 2008.
Another source of revenue generation by the Shadyside HELP program was reduced length of stay in delirious patients. The delirious patients demonstrated benefits from the HELP program, and were discharged from the hospital sooner than delirious patients not receiving HELP. Following the approach outlined above, the revenue generated can be calculated as follows: reduced LOS (adjusted) in delirious patients on HELP of 2.15 days X (1251 HELP delirium cases/365 days) X $417,995 per bed = $3,080,165 per year. The HELP program also decreased variable costs in the delirious patients, but since LOS also influences these costs, they were not evaluated separately to avoid overlap; however given this omission, the present cost savings estimate likely represents an underestimate of the true cost savings of the program.
Based on these 3 sources of financial benefit, the overall financial return of the Shadyside HELP program in 2008 was estimated at $7,368,549 (Figure 2). Hospital administrative leadership has consistently endorsed our findings that HELP both reduces expenses and creates additional bed capacity for new patients.
An additional source of cost savings not included in these estimates is the volunteer time contribution. Volunteers currently contribute over 300 hours per week to the program. The Independent Sector coalition <http://www.independentsector.org/programs/research/volunteer_time.html> currently values volunteer time at $20.25 per hour, yielding a volunteer contribution of $6075 per week to the hospital. This would amount to over $243,000 per year as an additional economic contribution of HELP, compared with paid staff providing these services.
On the expense side of the ledger, the costs to Shadyside of operating the HELP program for the first year were $127,000, of which $58,000 was provided by a private foundation. In 2008, the costs of the expanded program, including personnel and supplies, were $439,440. The personnel costs, totaling $375,724, were for salary support of 4 full time equivalent (FTE) Elder Life Specialists, 2 FTE Elder Life Nurse Specialists, 0.1 FTE geriatrician, and 0.6 administrative assistant. Program supplies, totaling $63,716, were for supplies needed to conduct the HELP interventions, including therapeutic activities equipment, hearing and vision adaptation equipment, large-print magazines, office supplies, and recruitment costs for volunteers. These costs will need to be taken into account at sites wishing to replicate the HELP program.
Challenges and successes encountered
Challenges and successes during the dissemination process are outlined in Table 3. The program encountered many challenges during large-scale expansion. As the program expanded, with the need for more staffing, inevitable problems arose with staff turnover and personnel conflicts. In particular, we experienced significant turnover in the nurse practitioner role. We found that many individuals in this role wanted to provide direct care, rather than the more supportive, educational, and supervisory role played by the Elder Life Nurse Specialist. Thus, clear definition of the role before recruitment efforts is critical. Team building efforts and regular staff meetings were essential to address interpersonal conflicts. Volunteer turnover is an ongoing issue that was recognized early on. Many volunteers are college students, who will move on; thus, recruitment efforts must be continuous. We have developed a variety of techniques to enhance both recruitment and retention. We work directly with local college campuses to facilitate recruitment, and with specific program directors to grant academic credit for volunteer time. The HELP program serves as an official field placement site for Masters in Social Work (MSW) students from the University of Pittsburgh. As we expanded to new units, the distance our staff had to cover became considerable. With support from hospital management, we were able to identify spaces that we transformed into satellite offices, equipped with computer workstations and storage space for the materials used for patient support, such as hearing amplification devices and equipment for therapeutic activities. At present, we have 3 satellite offices in different wings of the hospital. Finally, the time necessary to process the patient worksheets and to collect data on each patient, such as the names of their medications, limited our ability to serve large numbers of patients. To address this, we developed specialized software for volunteer assignments and data collection that is linked to our electronic health record (EHR).
Table 3.
Challenges and Successes of the Shadyside HELP Model
| Challenge | Solution |
|---|---|
Staff expansion:
|
|
| Volunteer turnover |
|
| Broad geographical coverage across units |
|
| Paperwork reduction and tracking |
|
| Success | Outcome |
| Met success metrics defined by hospital leadership | Hospital-wide dissemination to 6 units |
| Successful prevention of delirium and reduced length of hospital stay | Awarded Grand Prize in hospital’s annual Quality Improvement Fair in 2003, 2007 |
| Volunteer recognition | Volunteers receive widespread commendation, including top volunteer award at hospital and Community Champion awards from local newspaper |
We have been able to overcome these challenges, and our program has experienced tremendous success. First and most importantly, we were able to meet the success metrics defined by our hospital leadership, and thus, to gradually expand hospital-wide to 6 units. The program has been successful for prevention of delirium, improved patient and nursing satisfaction with care, reduced length of stay, and reduced costs. As a result, HELP was awarded the Grand Prize in the hospital’s annual Quality Improvement Fair in 2003 and 2007, both of the years the program was nominated. Our volunteers have also received widespread recognition and commendation. In 2006, one of our volunteers received the top award among all volunteers in the hospital. In 2008, two of our volunteers received Community Champion Awards from the local newspaper.
DISCUSSION
This paper summarizes an example of the successful implementation, adaptation, and evolution into a mature dissemination site for an effective clinical program. The processes outlined in this study provide a real-world demonstration of the factors which enhance the adoption of healthcare innovations documented previously (14–16) including: 1) strong clinical leadership; 2) gaining support of senior management; 3) providing credible supportive data; 4) developing an infrastructure supportive to the innovation; 5) ability to change organizational culture to support the innovation; 6) developing effective interdepartmental and interdisciplinary collaboration; and 7) being responsive to immediate pressures and threats, including economic pressures and Medicare no-pay conditions. In fact, the HELP dissemination at Shadyside fulfilled all of these identified factors for successful adoption. Notably, this site demonstrated important positive outcomes in terms of improving clinical care (reduction of delirium), enhancing staff and patient satisfaction with care, decreasing length of hospital stay and reducing costs of care. Thus, this program fulfilled key clinical effectiveness and quality improvement goals while enhancing efficiency on a large scale within the hospital. The low rate of incident delirium (3%) among enrolled patients might represent a benchmark for delirium reduction programs.
The strengths of this study include its size and scale, documenting that system-wide changes can be implemented within a community hospital. In addition, the program maintained high fidelity to the original model, while making local adaptations necessary to program survival, which enhanced both its feasibility and sustainability. Finally, the data collection and documentation of key metrics of success were noteworthy strengths of this study. The steps taken during the process of establishing the HELP program at Shadyside demonstrate the importance of institutional commitment and administrative buy-in to assure successful implementation and survival of any new program over time. The HELP program leader worked closely with hospital administration to identify key success metrics, to collect and present outcomes to make a convincing case for the program based on their own data, and to keep administration informed of the program’s success over time. Keeping the program visible through awards and commendations, as well as ongoing demonstrations of the clinical and financial benefits of the program have made this site one of the largest and most successful HELP programs nationally.
Several important caveats regarding the study must be noted. First, this study was conducted in the context of a quality improvement program and not a research study; there were no dedicated staff for data collection. Thus, some important data elements were not tracked or not available across all years. Administrative data were utilized for the major study outcomes and financial analysis. Delirium rates—and thus, the cost savings calculated—may have been underestimated by our approach. While acknowledging the limitations of this approach, the use of administrative data is a realistic option which can be utilized by many hospitals. Moreover, the proxy measure for delirium utilized at baseline and described in detail previously, has been validated for accuracy against direct clinical observations (8). The follow-up delirium rates in 2005 and 2008 were based on direct observation by the Elder Life Nurse Specialist using gold standard ratings for delirium. The low rates of observed delirium (3% or less) from 2004–2008, which are relatively lower than observed rates in previous studies utilizing HELP, may have been a reflection of the inclusion of lower risk patients in our sample and also the once a day clinical delirium assessments [as opposed to daily research assessments augmented by nursing interviews and medical record reviews in previous studies (3)]. Unfortunately, we were unable to stratify the costs of care for our patients by their delirium risk at baseline, and to provide separate estimates for cost savings across these strata. Another limitation is the temporal separation of the follow-up delirium ratings and the baseline (historical) controls. Since the HELP program is implemented hospital-wide, we were unable to examine a comparable concurrent control group without HELP for this study. Thus, changes in healthcare over time may have influenced these observations. However, the maintenance of low levels of delirium overall (and particularly incident delirium) despite increases in patient acuity over time at our site, as well as repeated and reproducible rates of delirium reduction on launching of other HELP programs in the U.S. and elsewhere lend strong support for the continued effectiveness of the program. During our study period, overall length of stay in the Medicare population has decreased somewhat, declining from 6.0 days in 2001 to 5.5 days in 2008 <http://www.cdc.gov/nchs/nchs_for_you/older_americans.htm> which may account for some of the shortening observed in this study. However, it is important to emphasize that these shifts in length of stay do not offset the much greater observed reduction in length of stay observed for delirious patients vs. non-delirious patients. Finally, not all hospitals will have the resources to enroll all patients age 70 years and older into HELP, as we did in our study. Targeting moderate to high risk patients for delirium has previously been demonstrated to be an efficient and cost-effective approach (3–7).
Delirium poses a major challenge for hospital quality of care, patient safety, and costs of hospital care. As hospitals struggle to address the current economic realities, cost reductions in the care of vulnerable older persons are often necessary. The HELP model provides a proven method for reducing hospital costs while simultaneously improving quality and safety. The HELP program has been extensively evaluated in multiple studies, and has consistently demonstrated both effectiveness and cost-effectiveness. The present study now makes the dissemination and financial case for HELP, which should clearly be a priority area for hospitals. In addition to preventing delirium, the program is effective for other key quality indicators, including falls, pressure ulcers, and length of stay. The rising numbers of elderly inpatients compel all hospitals to carefully address their approaches to this population, and to seriously consider HELP. Moreover, HELP is synergistic with other innovations designed to improve quality of health care for the elderly, such as acute care for the elderly units (ACE), Nurses Improving Care for Healthsystem Elders (NICHE), and the Transitions programs (17). This study can serve as a useful model for the successful implementation and dissemination of HELP.
ACKNOWLEDGMENTS
The authors wish to acknowledge the following individuals for their contributions to the HELP program at Shadyside: Eileen Mozolak, F.D. Fields, Phyllis Glass, Monica J. Giulioli, Lisa S. Panzarello, Jennifer T. Williams, and Richard Grimes. The authors also thank Nina O’Brien for assistance with manuscript preparation. This work is dedicated with admiration to the Hospital Elder Life Program Dissemination teams at Yale and Hebrew SeniorLife, and the committed staffs at over 60 dissemination sites worldwide.
Funding sources: Funded in part by grants no. K24AG00949 from the National Institute on Aging (SKI), no. 2007-225 from the Retirement Research Foundation (SKI), no. IIRG-08-88737 from the Alzheimer’s Association (SKI), and the Aging Brain Center, Institute for Aging Research, Hebrew Senior Life. Dr. Inouye holds the Milton and Shirley F. Levy Family Chair.
Sponsor’s Role: The sponsors had no role in the design, methods, subject recruitment, data collection, analysis and preparation of the paper.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Study concept and design: F Rubin
Acquisition of data: F. Rubin, K Neal, S Hassan
Analysis and interpretation of data: F Rubin, K Fenlon, SK Inouye
Drafting of the manuscript: F Rubin, SK Inouye
Critical revision of the manuscript for important intellectual content: F Rubin, K Neal, K Fenlon, S Hassan, SK Inouye
Statistical expertise: F Rubin, K Fenlon, SK Inouye
Obtained funding: SK Inouye
Administrative, technical, or material support: F Rubin, SK Inouye
References
- 1.Inouye SK. Current concepts: Delirium in older persons. N Engl J Med. 2006;354:1157–1165. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 2.Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly. Arch Intern Med. 2008;168:27–32. doi: 10.1001/archinternmed.2007.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK, Bogardus ST, Baker DI, et al. The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in hospitalized older patients. J Am Geriatr Soc. 2000;48:1697–1706. doi: 10.1111/j.1532-5415.2000.tb03885.x. [DOI] [PubMed] [Google Scholar]
- 5.Inouye SK, Baker DI, Fugal P, et al. Dissemination of the Hospital Elder Life Program: Implementation, adaptation, and successes. J Am Geriatr Soc. 2006;54:1492–1499. doi: 10.1111/j.1532-5415.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 6.Rizzo JA, Bogardus ST, Leo-Summers L, et al. Multicomponent targeted intervention to prevent delirium in hospitalized older patients: What is the economic value? Med Care. 2001;39:740–752. doi: 10.1097/00005650-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Leslie DL, Zhang Y, Bogardus ST, et al. Consequences of preventing delirium in hospitalized older adults on nursing home costs. J Am Geriatr Soc. 2005;53:405–409. doi: 10.1111/j.1532-5415.2005.53156.x. [DOI] [PubMed] [Google Scholar]
- 8.Rubin FH, Williams JT, Lescisin DA, et al. Replicating the Hospital Elder Life Program (HELP) in a community hospital and demonstrating effectiveness using administrative data. J Am Geriatr Soc. 2006;54:969–974. doi: 10.1111/j.1532-5415.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- 9.Caplan GA, Harper EL. Recruitment of volunteers to improve vitality in the elderly: the REVIVE study. Intern Med J. 2007;37:95–100. doi: 10.1111/j.1445-5994.2007.01265.x. [DOI] [PubMed] [Google Scholar]
- 10.Inouye SK, Brown CJ, Tinetti ME. Perspective: Medicare Nonpayment, Hospital Falls, and Unintended Consequences. N Engl J Med. 2009;360:2390–2393. doi: 10.1056/NEJMp0900963. [DOI] [PubMed] [Google Scholar]
- 11.Bradley EH, Webster TR, Schlesinger M, et al. The roles of senior management in improving hospital experiences for frail older adults. J Healthcare Management. 2006;51:323–337. [PubMed] [Google Scholar]
- 12.Inouye SK, Viscoli CM, Horwitz RI, et al. A predictive model for delirium in hospitalized elderly medical persons based on admission characteristics. Ann Intern Med. 1993;119:474–481. doi: 10.7326/0003-4819-119-6-199309150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Inouye SK, Van Dyck CH, Alessi CA, et al. Clarifying confusion: The Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 14.Bradley EH, Webster TR, Baker D, et al. Translating research into practice: Speeding the adoption of innovative health care programs. The Commonwealth Fund; Issue Brief. 2004;No 724 (April 2004) [PubMed] [Google Scholar]
- 15.Bradley EH, Schlesinger MJ, Webster TR, et al. Translating research into clinical practice: Making change happen. J Am Geriatr Soc. 2004;52:1875–1882. doi: 10.1111/j.1532-5415.2004.52510.x. [DOI] [PubMed] [Google Scholar]
- 16.Bradley EH, Webster TR, Baker D, et al. After adoption: Sustaining the innovation. A case study of disseminating the Hospital Elder Life Program. J Am Geriatr Soc. 2005;53:1455–1461. doi: 10.1111/j.1532-5415.2005.53451.x. [DOI] [PubMed] [Google Scholar]
- 17.Siu AL, Spragens LH, Inouye SK, et al. Can chronic care be improved using an acute care platform? The ironic business case for chronic care. Health Affairs. 2009;28:113–125. doi: 10.1377/hlthaff.28.1.113. [DOI] [PubMed] [Google Scholar]