Abstract
More than three decades of health disparities research in the United States has consistently found lower adult mortality risks among Hispanics than their non-Hispanic white counterparts, despite lower socioeconomic status among Hispanics. Explanations for the “Hispanic Paradox” include selective migration and cultural factors, though neither has received convincing support. This paper uses a large nationally representative survey of health and smoking behavior to examine whether smoking can explain life expectancy advantage of Hispanics over US-born non-Hispanics whites, with special attention to individuals of Mexican origin. It tests the selective migration hypothesis using data on smoking among Mexico-to-US migrants in Mexico and the United States. Both US-born and foreign-born Mexican-Americans exhibit a life expectancy advantage vis-à-vis whites. All other Hispanics only show a longevity advantage among the foreign-born, while those born in the United States are disadvantaged relative to whites. Smoking-attributable mortality explains the majority of the advantage for Mexican-Americans, with more than 60% of the gap deriving from lower rates of smoking among Mexican-Americans. There is no evidence of selective migration with respect to smoking; Mexicans who migrate to the US smoke at similar rates to Mexicans who remain in Mexico, with both groups smoking substantially less than non-Hispanic whites in the US. The results suggest that more research is needed to effectively explain the low burden of smoking among Mexican-Americans in the United States.
Keywords: U.S.A, Hispanic paradox, cigarette smoking, life expectancy, migration, Mexican, selection
INTRODUCTION
More than three decades of health disparities research in the United States has consistently found lower adult mortality risks among Hispanics than among their non-Hispanic white counterparts (Elo et al., 2004; Hummer et al., 2000; Markides & Coreil, 1986). This occurs despite lower average education and income and higher rates of poverty among Hispanics, which gives rise to the term “Hispanic Paradox” (Markides & Eschbach, 2005; Palloni & Arias, 2004). The phenomenon has been identified and thoroughly described using nationally representative surveys, small-sample cohort studies, and vital statistics. The Hispanic advantage in life expectancy is non-trivial, amounting to 2.5 years at birth according to recently-released life tables by Hispanic origin produced by the National Center for Health Statistics (Arias, 2010). Corresponding advantages are observed for many chronic health conditions including cardiovascular disease, cancers, and chronic respiratory diseases. The topic has received a large amount of attention in the literature, has been investigated extensively, and a number of possible hypotheses have been offered. However, despite its ubiquity, the Hispanic paradox has previously eluded a convincing explanation.
Examining Hispanics as a homogeneous group with a singular mortality experience is problematic. The US Hispanic population has origins in many different countries with varied social and economic circumstances and health profiles. The heterogeneity of mortality experiences among subgroups within the Hispanic population is as large as that between Hispanics and other race/ethnic groups in the US (Hummer et al., 2000), and recent research contends that the Hispanic paradox is not a feature of all Hispanics, only of certain subgroups. In addition to being the largest Hispanic subgroup, the Mexican population also shows perhaps the most consistent mortality advantage relative to non-Hispanic whites (Abraido-Lanza et al.,1999; Hummer et al., 2000; Sorlie et al.,1993). According to the 2010 Census, there were more than 30 million individuals of Mexican descent in the US, making up more than 10% of the total population and nearly two-thirds of all Hispanics (US Census Bureau, 2011). Indeed, the “Hispanic paradox” is largely a “Mexican paradox”, as Palloni and Arias (2004) contend that the advantage exists primarily among Mexicans. Evidence for the advantage among the next largest subgroups, Puerto Ricans and Cubans, is more mixed (Abraido-Lanza et al., 1999; Sorlie et al., 1993). Puerto Ricans, especially those born in the 50 states, differ from other Hispanic subgroups in that they are often disadvantaged relative to whites with respect to mortality (Hummer et al., 2000; Markides & Eschbach, 2005). Related to the Hispanic paradox is the immigrant paradox, the tendency for foreign-born populations to outlive the native-born despite lower socioeconomic status. A similar pattern is observed within Hispanic populations, and some research asserts that the Hispanic paradox exists only for the foreign-born (Palloni & Morenoff, 2001). Although other studies find an advantage for US-born Hispanics, it is at best greatly diminished compared with that of foreign-born Hispanics (Singh & Siahpush, 2002). Since nearly 60% of adult Hispanics are foreign-born, it is inappropriate to consider Hispanic immigrants and US-born Hispanics in combination, and explaining the Hispanic paradox necessarily requires attention to the role of nativity.
This paper uses data from a nationally representative survey to examine the contribution of cigarette smoking to the adult life expectancy advantage of Hispanics relative to US-born non-Hispanic whites. The focus of the paper is the experience of foreign- and US-born Mexican-Americans. In addition, the paper combines data from national surveys in Mexico and the United States to test whether the findings with respect to smoking might reflect a prominent explanation for the paradox: the selective migration hypothesis. Individuals who move from their origin country to the United States are likely to be in better health than those who remain in the origin country on a number of dimensions that are relevant to the Hispanic paradox (Abraido-Lanza et al., 1999).
EVIDENCE FOR THE HISPANIC MORTALITY ADVANTAGE
The major sources of data on Hispanic mortality are US vital statistics and nationally representative surveys. Studies using vital statistics suffer from issues related to differences in the identification of Hispanic origin on death certificates and the census, and have the potential to underestimate Hispanic mortality (Arias et al., 2008). Representative surveys with prospective mortality follow-up partially solve this issue, since origin is self-reported and respondents are matched to records in the National Death Index. Surveys also allow the researcher to examine the Hispanic advantage across a variety of other covariates and to examine the mortality of multiple Hispanic subgroups (Palloni & Arias, 2004). Although evidence for the Hispanic paradox is abundant, empirical evidence for the most prominent explanations is somewhat unconvincing. The two broad hypotheses for explaining the paradox are selective migration and culture.
Selective migration hypothesis
Since most adult Hispanics in the United States are foreign born, any examination of the Hispanic mortality experience must consider to what extent immigrants are a select group of their origin country populations. If migrants differ significantly from non-migrants, our estimates of the mortality of the foreign-born in the US may be biased. Selective migration can refer to both in-migration of healthy individuals (healthy migrant effect) and out-migration of unhealthy individuals (salmon bias). The former concerns the greater human capital and health resources that may be necessary to undertake an international move, such that we observe a highly select group of individuals from sending countries, potentially offsetting the negative effects of their poor socioeconomic profile (Abraido-Lanza et al., 1999). The latter suggests that foreign-born individuals in the United States may return to their countries of origin when they become ill, leaving a healthier subset in the US (Palloni & Ewbank, 2004).
The specific mechanisms through which selection operates are kept relatively vague in conceptual formulations of the hypothesis (Palloni & Ewbank, 2004). Migrants may be selected on aspects of underlying health or robustness, which are generally difficult to measure, or on social characteristics that impact health, such as educational attainment or wealth. Migrant selection may also operate through health-related behaviors if characteristics such as poor diet, low physical activity, or cigarette smoking present greater barriers to migration owing in part to the negative health effects of the behaviors (Buttenheim et al., 2010). In general, direct investigation of health selection with respect to immigration from Mexico to the US is lacking. The most comprehensive recent study was by Rubalcava et al. (2008) who examined differences between Mexican immigrants to the United States and Mexicans who remained in Mexico on several measures of health, and found overall weak evidence for health-selective migration. No studies have considered migrant selection on health behaviors.
Cultural hypothesis
As with their mortality experience, it may be inappropriate to classify Hispanics as having a singular consistent culture or assume that attitudes and practices are similar between or within all Hispanic subgroups. Heterogeneity in the cultural practices and attitudes among Hispanic subgroups is certainly large and attributing health outcomes of the Hispanic population to cultural characteristics may ignore important variation (Rodriguez, 1995). Still, certain aspects of shared culture may promote better health and prevent mortality among specific Hispanic subgroups (Marin & Marin, 1991). Indeed, Mexican-Americans living in enclaves with a high proportion of Mexican immigrants appear to retain Mexican cultural traditions more effectively (Eschbach et al., 2004). These populations may benefit from strong familial and friendship networks that provide a needed source of social support. The positive effects of social support may be manifested in a number of ways including the tendency to engage in healthier behaviors.
CIGARETTE SMOKING AND THE HISPANIC PARADOX
Cigarette smoking may play a key role in the Hispanic mortality advantage for two reasons. First, cigarette smoking has a strong negative impact on individual mortality and is the single greatest cause of premature death in the United States (Mokdad et al., 2004). Smoking is responsible for more than 20% of adult deaths among Americans (Preston et al., 2010). Second, survey data indicate that Hispanics in the US have a relatively low prevalence of the behavior. Hispanics who do smoke are also less likely to do so every day, smoke fewer cigarettes per day, and have smoked for fewer years on average than non-Hispanic whites (Siahpush et al., 2010). Non-Hispanic whites are more likely than Hispanics to smoke and are likely to have higher amounts of accumulated physiological damage from a history of heavy smoking (Bethel & Schenker, 2005). As this evidence has grown in recent years, several studies have considered the relevance of smoking to the Hispanic paradox (Perez-Stable et al., 2001). The Hispanic advantage is largest for causes of death that are strongly associated with smoking including lung cancers, respiratory diseases, and ischemic heart disease (Singh & Siahpush, 2002). Blue and Fenelon (2011) were the first to directly examine the contribution of smoking to the Hispanic paradox. They used an indirect method to estimate smoking-attributable mortality for all Hispanics and non-Hispanics whites using vital statistics data from the year 2000. They found that smoking-related mortality was responsible for 75% of the Hispanic advantage in life expectancy at age 50 for men and for women (both slightly more than 2 years).
Their study did not account for differences by nativity and country of origin in mortality or smoking experience among Hispanics. Much of the reason we observe such low prevalence and intensity of smoking among Hispanics is the particularly light smoking of the Hispanic immigrant population (Singh & Siahpush, 2002). Consistent with the immigrant health advantage, evidence suggests that foreign-born Hispanics smoke less than their US-born counterparts and significantly less than non-Hispanic whites. Mexican-Americans are the largest subgroup of both foreign- and US-born Hispanics, and have substantial leverage in determining the predominant smoking patterns of the Hispanic population as a whole. Surveys indicate that Mexican-Americans smoke less than many other Hispanic subgroups including Cubans and Puerto Ricans (Singh & Siahpush, 2002). Mexican-Americans also appear to have exceptionally low cigarette consumption, with a large fraction of smokers in this group identifying as “intermittent” or “occasional” rather than “daily” smokers (Caraballo et al., 1998).
DATA
This paper uses data from the National Health Interview Survey Linked-Mortality Files (NHIS-LMF), which are obtained through the Integrated Health Interview Series (IHIS, 2010). NHIS collects detailed demographic, behavioral, and health information in annual cross-sectional samples. Respondents are linked to US death records in the National Death Index through the end of 2006. Annual surveys are pooled for the years 1990 – 2004, including only individuals aged 35 or older and for whom smoking status was identified. Age 35 is chosen as a cutoff because few smoking-related deaths occur prior to age 35 and because the Hispanic advantage is concentrated in the adult age range (Markides & Eschbach, 2005). The final sample includes a total of 155,173 women and 119,138 men and 35,224 deaths. Observations are weighted using supplement-specific annual person weights for survey years 1990 – 1995 and mortality sample adult weights for 1997 – 2004. The study was exempt from human subjects review since all data are publicly available and do not contain individual identifiers.
Smoking status is measured through a series of questions and respondents are classified into six groups according to current and past smoking behavior and current daily cigarette consumption. Respondents who have smoked fewer than 100 cigarettes in their entire lives are classified as “never smokers”. Respondents who report having smoked at least 100 cigarettes but who answer “no” to the question “Do you currently smoke cigarettes every day or some days?” are coded as “former smokers”. The definition of “every day or some days” is left up to the respondent. To account for increased mortality risk associated with greater cigarette consumption, current smokers are also classified by number of cigarettes smoked per day: current very light smoker (fewer than 10 cigarettes per day), light smoker (10–19 per day), medium smoker (20–29 per day), and heavy smoker (30+ per day).
Individuals are categorized into 5 race/ethnic groups based on nativity and Hispanic origin: 1) US-born non-Hispanic whites, who serve as the majority comparison group for each Hispanic subgroup, 2) US-born Mexican-Americans, individuals specifically identifying as being of Mexican origin born in the United States, 3) US-born other Hispanics, individuals who are of Hispanic but not Mexican origin and born in the United States, 4) foreign-born Mexican-Americans, Mexican origin individuals born outside the United States, and 5) foreign-born other Hispanics. Small sample sizes precluded the analysis of smoking with respect to more detailed countries of origin among Hispanics.
METHODS
Statistical model
Loglinear hazard regression models are used to estimate all-cause death rates and the impact of smoking by race/ethnic group (Rogers et al. 2005). The models predict the all-cause mortality hazard as a function of 5-year age groups (35–39, 40–44,…,85+), race/ethnic group, and smoking status. Models are stratified by sex and include an interaction between the “former smoker” category and race/ethnic group in order to account for race/ethnic differences in daily cigarette consumption among former smokers. If white former smokers smoked more heavily before quitting, they may experience a higher relative mortality risk of former smoking than lighter-smoking Hispanic subgroups. Individuals contribute risk exposure each year between interview (or age 35 for those younger at baseline) and death or censoring. Censoring occurs for individuals who are alive as of the end of 2006.
Life expectancy in the presence and absence of smoking
Mortality attributable to cigarette smoking in each race/ethnic group is calculated using a conventional attributable-risk approach. This method estimates the proportion of deaths in each group that would not occur if smokers experienced no excess mortality relative to never-smokers. The method takes into account both the proportion of individuals in each smoking status category as well as the estimated relative mortality risk of each smoking status compared with never smokers based on the hazard model described above. Smoking-attributable mortality is calculated for men and women by 5-year age group and race/ethnic group. These values allow us to examine life expectancy in the presence and absence of smoking. Life expectancy at age 35 is estimated using standard life table methods (Preston et al., 2001). Life expectancies for each race/ethnic group in the presence of smoking (e35) are calculated using predicted death rates from observed covariate values, while corresponding life expectancies in the absence of smoking ( ) are calculated using death rates with smoking-related mortality removed. The change in the life expectancy gap after the removal of smoking represents the portion of the advantage that is attributable to smoking. The contribution is calculated as
where He35 and We35 are life expectancies at age 35 for the Hispanic subgroup and US-born non-Hispanic whites, respectively. and are the same values calculated in the absence of smoking. The first term in the equation refers to the life expectancy advantage (in years) for the Hispanic subgroup in the presence of smoking and the second term is the advantage in the absence of smoking.
Standard errors for attributable-risk fractions and the contribution of smoking are estimated by simulated resampling based on regression parameter uncertainty. 1,000 sets of age-specific death rates are simulated by allowing these death rates to vary within the regression-predicted parameter variance determined by the variance-covariance matrix of the hazard regression model. These sets of death rates produce a simulated sample of attributable-fractions and contributions of smoking from which it is possible to calculate standard errors. 95% confidence intervals are reported in the results below.
Testing the selective migration hypothesis
In order to test the selective migration hypothesis with respect to smoking, it is necessary to compare smoking prevalence of migrants and non-migrants in Mexico prior to migration. NHIS data are combined with data from the Mexican Family-Life Survey (MxFLS), a panel survey in Mexico that completes follow-up interviews for all respondents irrespective of changes in residential location, which includes more than 800 individuals who migrated to the United States between 2002 and 2005 (Rubalcava & Teruel, 2008). Information on cigarette smoking comes from respondent self-reports of current and past behavior, and is comparable to that in the NHIS. Among individuals ages 18–39, logistic regression is used to predict the probability of being a current smoker for five groups based on place of birth and migrant status. Two groups come from MxFLS: 1) Mexican non-migrants who remain in Mexico between 2002 and 2005, and 2) Mexico-to-US migrants who enter the United States during this period. Three groups come from the NHIS: 3) Mexican immigrants who arrived in the US within the past 5 years, 4) US-born Mexican-Americans, and 5) US-born non-Hispanic whites. If selective migration is operating, Mexico-to-US migrants and Mexican immigrants in the US should be less likely to smoke than non-migrants in Mexico.
RESULTS
Consistent with previous research, this study found that Hispanics significantly outlived US-born non-Hispanic whites at age 35, though there were differences by nativity and country of origin (Table 1). Among US-born Hispanics, only Mexican-Americans experienced an advantage over whites (1.9 years among women, 1 year among men). US-born other Hispanics were at a substantial disadvantage, trailing whites by 1.5 years among women. Foreign-born Mexican-Americans had a large life expectancy advantage, outliving whites by 3 years among women and 2.1 years among men. The advantage was fairly similar for Foreign-born other Hispanics.
Table 1.
Estimated remaining life expectancy in years at age 35 by race/ethnic group and sex
| Women
|
Men
|
|||
|---|---|---|---|---|
| Life Expectancy | Advantage1 | Life Expectancy | Advantage | |
|
|
||||
| US-born non-Hispanic white | 47.60 (47.3 – 47.9) | -- | 41.67 (41.5 – 41.9) | -- |
| US-born Mexican-American | 49.52 (48.9 – 50.1) | 1.92 (1.8 – 2.1) | 42.48 (42.5 – 43.6) | 0.81 (0.5 – 1.2) |
| US-born other Hispanic | 46.03 (45.0 – 45.9) | −1.57 (−1.2 – −1.9) | 41.27 (40.8 – 41.7) | −0.40 (−0.8 – 0.0) |
| Foreign-born Mexican-American | 50.71 (50.4 – 51.0) | 3.11 (3.0 – 3.3) | 43.81 (43.2 – 44.4) | 2.14 (1.8 – 2.5) |
| Foreign-born other Hispanic | 50.58 (49.8 – 50.4) | 2.98 (2.8 – 3.3) | 44.39 (44.0 – 44.8) | 2.72 (2.3 – 3.1) |
Notes: Estimated with hazard regression using NHIS pooled samples 1990 – 2004. 95% confidence intervals in parentheses. Mexican-Americans respond as being of Mexican origin. Other Hispanics are all Hispanics not of Mexican origin
In years at age 35 compared with US-born non-Hispanic whites
Data on smoking status (Table 2) suggested that Mexican-Americans have a lower burden of smoking than whites. Among men, the major difference between whites and Mexican-Americans in the impact of smoking was in the prevalence of medium or heavy current smoking. While more than 70% of white men smokers consumed at least one pack (20 cigarettes) per day, only 33% of US-born and 20% of foreign-born Mexican-Americans men did. Among women, whites also smoked more heavily than Mexican-Americans. Nearly one-fifth of white women were current smokers compared with 13% of US-born and only 8% of foreign-born Mexican-American women. Nearly 60% of white women smokers smoked a pack or more per day, compared to only 23% of US-born Mexican-American women and 11% of foreign-born Mexican-American women. While US-born other Hispanic men and women were slightly more likely to smoke than whites, foreign-born other Hispanics showed a substantially lower prevalence and daily cigarette consumption.
Table 2.
Baseline smoking status by race/ethnic group ages 35 and above
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| N | Never Smoker | Former Smoker | Current Smoker | Current Very Light Smoker | Current Light | Current Medium | Current Heavy | |
|
|
||||||||
| Women | ||||||||
| Non-Hispanic white | 131,949 | 54.7% | 26.5 | 18.8 | 2.6 | 5.2 | 7.6 | 3.3 |
| US-born Mexican-American | 6,196 | 67.6% | 19.2 | 13.2 | 6.0 | 4.2 | 2.4 | 0.7 |
| US-born other Hispanic | 3,478 | 56.8% | 21.2 | 22.0 | 8.8 | 6.2 | 5.3 | 1.7 |
| Foreign-born Mexican-American | 6,318 | 81.2% | 11.1 | 7.7 | 5.6 | 1.2 | 0.8 | 0.1 |
| Foreign-born other Hispanic | 7,232 | 74.9% | 13.7 | 11.4 | 5.8 | 3.0 | 2.2 | 0.4 |
| Men | ||||||||
| Non-Hispanic white | 101,861 | 37.0% | 41.9 | 21.1 | 2.0 | 3.8 | 8.4 | 6.9 |
| US-born Mexican-American | 4,491 | 43.0% | 35.8 | 21.2 | 8.3 | 5.8 | 5.2 | 1.9 |
| US-born other Hispanic | 2,419 | 44.2% | 31.5 | 24.3 | 7.1 | 6.7 | 7.4 | 3.1 |
| Foreign-born Mexican-American | 5,545 | 48.8% | 31.9 | 19.3 | 10.8 | 4.9 | 3.2 | 0.6 |
| Foreign-born other Hispanic | 4,822 | 51.3% | 28.9 | 19.8 | 7.7 | 5.2 | 5.2 | 1.7 |
Notes: Cigarette consumption categories: very light = 0–9 cigarettes per day; light = 10–19 per day; medium = 20–29; heavy = 30+. All values are age-standardized for comparison across race/ethnic groups.
Source: National Health Interview Survey pooled smoking supplements 1990 – 2004.
Estimated regression results (hazard ratios) are presented in Table 3 by sex. Model 1 includes only age and race/ethnic group, and Model 2 adds smoking status variables. Model 1 indicated that Mexican-Americans and foreign-born other Hispanics experienced lower mortality risks than non-Hispanic whites. The inclusion of smoking status in Model 2 attenuated these differences. Each smoking status experienced higher mortality than never smokers, and the risk increased with greater consumption. Light smokers had 80%–100% higher risk of death while heavy smokers had a risk three times that of never smokers. Interactions between the former smoker category and race/ethnic group were significant for foreign-born Mexican-Americans and other Hispanics. The coefficients indicated that the mortality risk associated with being a former smoker was lower for foreign-born Hispanic subgroups than for whites, presumably reflecting higher former cigarette consumption among whites.
Table 3.
Estimated impact of smoking on mortality: Hazard regression
|
|
Women | Men | ||
|---|---|---|---|---|
| Age | Model 1 | Model 2 | Model 1 | Model 2 |
| 35–39 (ref.) | -- | -- | -- | -- |
| 40–44 | 1.8 (1.4 – 2.2) | 1.8 (1.2 – 2.3) | 1.8 (1.5 – 2.2) | 1.7 (1.3 – 2.2) |
| 45–49 | 2.7 (2.2 – 3.3) | 2.7 (1.9 – 3.5) | 2.8 (2.3 – 3.5) | 2.6 (2.0 – 3.3) |
| 50–54 | 4.1 (3.4 – 5.0) | 4.1 (3.0 – 5.2) | 4.3 (3.5 – 5.2) | 3.9 (3.0 – 5.0) |
| 55–59 | 6.6 (5.5 – 7.9) | 6.5 (4.6 – 8.3) | 6.7 (5.5 – 8.1) | 6.1 (4.8 – 7.8) |
| 60–64 | 10.7 (9.0 – 12.8) | 10.7 (7.9 – 13.8) | 10.8 (9.0 – 13.1) | 9.8 (7.7 – 12.5) |
| 65–69 | 16.7 (14.0 – 19.8) | 17.3 (13.3 – 22.8) | 17.2 (14.3 – 20.6) | 15.1 (11.8 – 19.2) |
| 70–74 | 25.7 (21.6 – 30.3) | 27.6 (20.5 – 35.6) | 26.3 (22.0 – 31.4) | 23.5 (18.5 – 29.9) |
| 75–79 | 40.9 (34.4 – 48.1) | 45.8 (34.8 – 60.1) | 42.2 (35.4 – 50.4) | 39.2 (30.8 – 49.8) |
| 80–84 | 67.1 (57 – 79) | 78.9 (59 – 103) | 68.6 (58 – 82) | 66.7 (53 – 85) |
| 85+ | 138.6 (117 – 163) | 172.4 (130 – 229) | 142.2 (119 – 169) | 146.9 (116 – 187) |
| race/ethnic group
|
||||
| US-born white (ref.) | -- | -- | -- | -- |
| US-born Mexican | 0.94 (0.88 – 1.00) | 0.99 (0.91 – 1.09) | 0.95 (0.88 – 1.03) | 1.01 (0.92 – 1.10) |
| US-born other | 1.16 (1.02 – 1.31) | 1.12 (0.97 – 1.30) | 1.07 (0.98 – 1.17) | 1.15 (1.01 – 1.29) |
| Foreign-born Mexican | 0.80 (0.74 – 0.86) | 0.96 (0.89 – 1.02) | 0.85 (0.77 – 0.91) | 0.99 (0.89 – 1.10) |
| Foreign-born other | 0.77 (0.70 – 0.84) | 0.88 (0.80 – 0.98) | 0.81 (0.71 – 0.93) | 0.85 (0.73 – 0.96) |
| Smoking
|
||||
| Never smoker (ref.) | -- | -- | ||
| Former smoker | 1.36 (1.31 – 1.40) | 1.34 (1.30 – 1.38) | ||
| Current (0–9 cigs per day) | 1.80 (1.66 – 1.95) | 2.00 (1.82 – 2.20) | ||
| Current (10–19) | 2.10 (1.95 – 2.26) | 2.11 (1.98 – 2.25) | ||
| Current (20–29) | 2.51 (2.36 – 2.66) | 2.51 (2.38 – 2.63) | ||
| Current (30+) | 3.13 (2.88 – 3.40) | 3.13 (2.88 – 3.39) | ||
| Smoking Interactions
|
||||
| Former x US-born Mex. | 1.05 (0.96 – 1.13) | 0.86 (0.70 – 1.08) | ||
| Former x US-born other | 0.93 (0.85 – 1.00) | 1.07 (0.87 – 1.30) | ||
| Former x For.-born Mex. | 1.15 (0.87 – 1.52) | 1.11 (0.97 – 1.24) | ||
| Former x For.-born other. | 0.78 (0.60 – 0.97) | 0.83 (0.73 – 0.97) | ||
|
| ||||
| Constant | 0.000857 | 0.000621 | 0.00172 | 0.00116 |
| N | 155,173 | 155,173 | 119,138 | 119,138 |
Notes: Estimated using hazard regression on data from NHIS smoking supplements 1990 – 2004. Hazard ratios shown. 95% confidence intervals in parentheses. Interactions reflect differences in the mortality risk of former smoking by race/ethnic group. Model 1 includes age and race/ethnic group. Model 2 adds coefficients for smoking status.
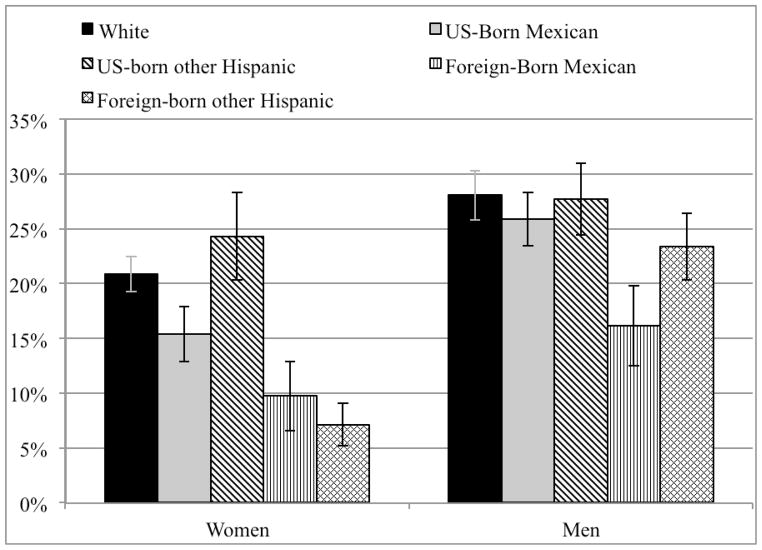
The smoking data in Table 2 along with the regression coefficients in Table 3 were used to predict the fraction of deaths attributable to smoking by sex for each race/ethnic group, shown in Figure 1. There was substantial variation among race/ethnic groups in the mortality burden of smoking. 28% (95% CI: 26%–30%) of deaths among white men and 21% (19%–22%) among white women were due to smoking. Comparatively, attributable-fractions for US-born Mexican-American men and women were 26% and 15%, respectively. Attributable risk for foreign-born Mexican-Americans was lower still, just 16% (12%–19%) for men and 10% (9%–12%) for women. US-born other Hispanic women had substantially higher smoking-attributable mortality (24%) than whites, and other Hispanic men had levels similar to those of whites. Foreign-born other Hispanics had relatively low smoking-attributable mortality, 7% among women and 23% among men.
Figure 1.
Percent of deaths attributable to smoking by race/ethnic group ages 35 and above. Estimated using hazard regression by comparing the predicted mortality for each race/ethnic using observed smoking status distribution to the predicted mortality for never smokers. Error bars indicate 95% confidence intervals of attributable-risk.
Source: Author’s calculations from National Health Interview Survey pooled smoking supplements 1990 – 2004.
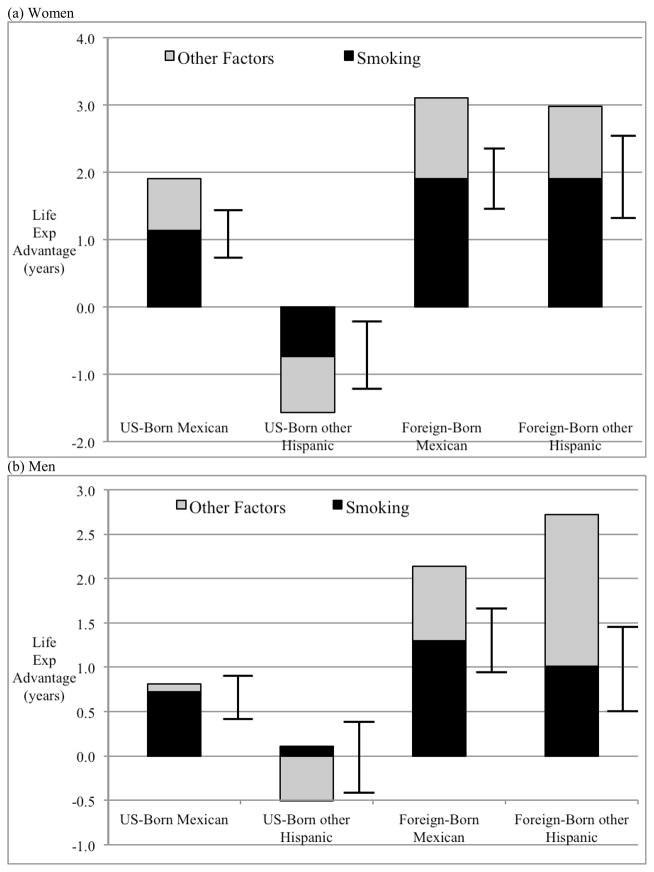
Removing smoking-attributable mortality produced estimates of the contribution of smoking to the life expectancy advantage of each Hispanic subgroup. These are shown in Figure 2a for women and 2b for men. Smoking was a major factor explaining the advantage, though the absolute contribution differed significantly by subgroup. Smoking explained 1.1 years (60%) of the advantage of US-born Mexican-American women and 1.9 years (61%) among the foreign-born. Among Mexican-American men, it explained 0.7 years (89%) for the US-born and 1.3 years (61%) for the foreign-born. Smoking also explained a substantial fraction of the advantage of foreign-born other Hispanics, 1.9 years among men and 1 year among women. Among US-born other Hispanic women, smoking appeared to be partially responsible for their life expectancy disadvantage, which would decrease by 0.7 years (46%) in the absence of smoking. Differences in smoking also contributed to the life expectancy advantage of foreign-born Mexican-Americans over the US-born. Among women, smoking explained 64% of this difference and among men 44%.
Figure 2.
Contribution of smoking to the life expectancy advantage of each Hispanic subgroup over US-born non-Hispanic whites at age 35. The black bar refers to the contribution of smoking to the advantage of each subgroup. The grey bar refers to the contribution of other factors and represents the size of the advantage in the absence of smoking. Error bars indicate 95% confidence intervals for the contribution of smoking.
Source: Author’s calculation using National Health Interview Survey pooled smoking supplements 1990 – 2004.
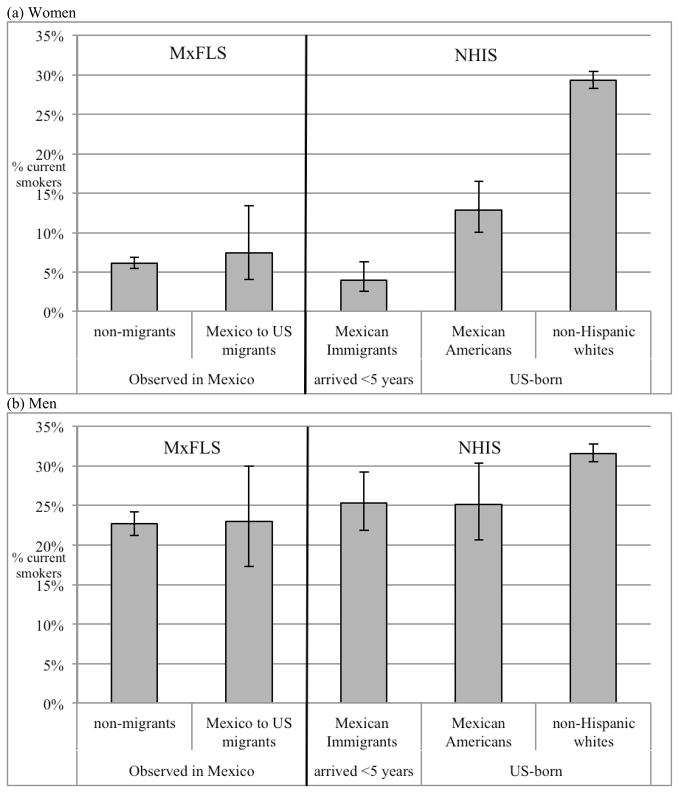
Testing the selective migration hypothesis
Data from MxFLS provide smoking status information on 315 Mexico-to-US migrants collected in 2002 prior to migration. Figure 3 compares smoking behavior of this group to non-migrants in order to test the selective migration hypothesis. Panel (a) shows the prevalence of current smoking for women by migrant status. Overall, there was no evidence of selective migration with respect to smoking status. Mexico-to-US migrants and non-migrants showed very similar prevalence of smoking among individuals aged 18–39 (23% among men, 6–7% among women). The prevalence of smoking among recent Mexican immigrants in the US was also very similar to the figures in Mexico, 25% among men and 4% among women, suggesting that low rates of smoking in Mexico were maintained among Mexicans in the United States. US-born Mexican-Americans showed higher prevalence than Mexican-born groups among women but not among men. US-born whites showed the highest prevalence among both men and women, consistent with the finding that smoking contributes to the life expectancy advantage for Mexican-born individuals in the US.
Figure 3.
Current smoking prevalence by migrant status among individuals ages 18 – 39 Two groups on the left of the black line come from the Mexican Family Life Survey. Mexico to US migrants enter to the United States between 2002 and 2005, while non-migrants remain in Mexico. The three groups on the right of the black line come from the National Health Interview Survey 2002 – 2005.
Source: Authors calculations using logistic regression on pooled NHIS-MxFLS sample.
Social gradients in health and the Hispanic advantage
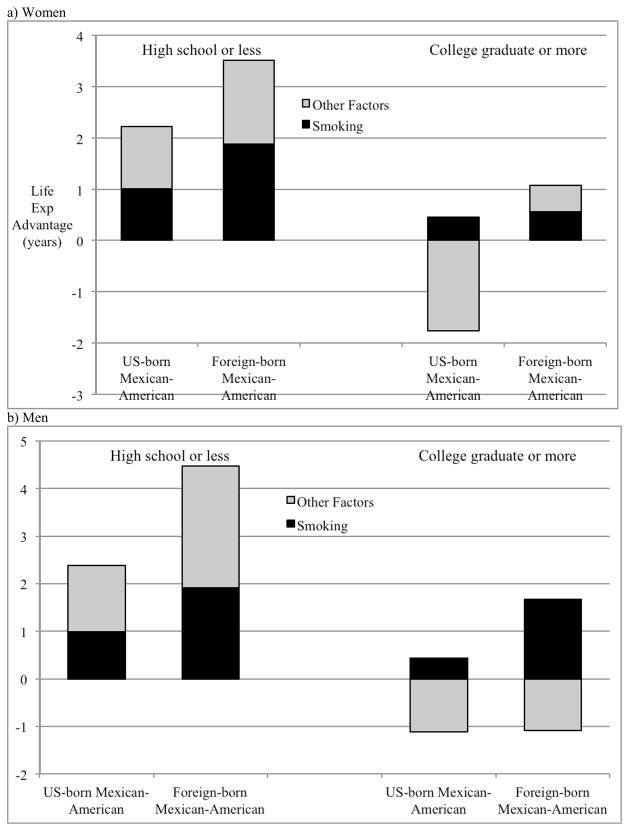
An important aspect of the Hispanic advantage is the differential relationship between socioeconomic status (SES) and mortality among Hispanics as compared to whites. Among whites, the socioeconomic gradient is strong, while the corresponding gradient for Hispanic populations is considerably less steep, with smaller differences in mortality risk by SES. As a result, the Hispanic mortality advantage is concentrated in the lower end of the socioeconomic spectrum (Turra & Goldman, 2007). This section examines the contribution of smoking to the advantage of US-born and foreign-born Mexican-Americans in two education categories: high school education or less (low), and college graduate or more (high). Individuals with some college were excluded. Both Mexican-American subgroups exhibited weaker education gradients than whites, and their life expectancy advantages were substantially larger in the low education group (Figure 4). Foreign-born Mexican-American women outlived whites by 3.5 years in the low education group and only 1.1 years in the high education group. Corresponding advantages for men were 4.5 years and 0.6 years. The life expectancy advantage of US-born Mexican-Americans was driven by the experience of those with low education; whites had a 0.7-year life expectancy advantage among men and a 1.3-year advantage among women among the highly educated. Likewise, the contribution of smoking was greater in the low education group compared to the high education group, 1.9 years compared to 0.6 years for foreign-born Mexican-American women, and 1 year compared to 0.5 years for the US-born. The pattern was similar for men. Overall, smoking explained 54% of the difference in the education gradient (size of the high-low education gap in life expectancy) between whites and foreign-born Mexican-American among women and 6% among men.
Figure 4.
Contribution of smoking to the life expectancy advantage of Mexican-American subgroups over US-born non-Hispanic whites at age 35 for women by level of education. The black bar refers to the contribution of smoking to the advantage of each subgroup. The grey bar refers to the contribution of other factors and represents the size of the advantage in the absence of smoking.
Source: Author’s calculation using National Health Interview Survey pooled smoking supplements 1990 – 2004.
The results were also similar when the hazard model included a simple control for education. Table 4 presents the contribution of smoking based on estimates from a model including a dummy variable for educational category. The similarity of these results to those of the original model suggested that education did not significantly confound the relationship between smoking and mortality. Although education was correlated with both the likelihood of smoking and with mortality risk, the inclusion of education in the models had little effect on the estimated coefficients for smoking, consistent with evidence on confounding in the smoking-mortality relationship (Thun et al., 2000). Adjusting for education did not impact the conclusion that smoking explains a majority of the Hispanic advantage.
Table 4.
Contribution of Smoking to life expectancy advantage at age 35 based on coefficients adjusted for education
| Life Expectancy Advantage | Advantage in the Absence of Smoking | % of advantage attributable to smoking | |
|---|---|---|---|
| Women
|
|||
| US-born Mexican-American | 1.92 | 1.33 | 68.20% |
| US-born other Hispanic | −1.57 | −0.78 | 49.68%1 |
| Foreign-born Mexican-American | 3.11 | 1.67 | 53.71% |
| Foreign-born other Hispanic | 2.98 | 1.47 | 49.33% |
| Men
|
|||
| US-born Mexican-American | 0.81 | 0.57 | 70.10% |
| US-born other Hispanic | −0.4 | −0.11 | 27.51%1 |
| Foreign-born Mexican-American | 2.14 | 1.29 | 60.28% |
| Foreign-born other Hispanic | 2.72 | 1.89 | 69.49% |
Notes: Life expectancy advantages are in years at age 35. Smoking-attributable mortality and contribution of smoking estimated using a standard attributable-risk method. Coefficients for smoking status are adjusted for education: high school or less, and college graduate or more.
For US-born other Hispanics, higher smoking attributable mortality partially explains their mortality disadvantage relative to whites.
Discussion
This study examines the impact of cigarette smoking on the mortality advantage of Hispanics over non-Hispanic whites in the United States. The results confirm that the Hispanic advantage is not consistent across all Hispanic subgroups. Mexican-Americans, both foreign- and US-born, enjoy a significant life expectancy advantage over whites. On the other hand, other US-born Hispanics (primarily Puerto Ricans) are disadvantaged. The differences observed and between US-born non-Hispanic whites and foreign-born Mexican-Americans are similar to those in official US life tables (Arias, 2010). The principal contribution of this study is establishing that low smoking-related mortality among Hispanics is the primary reason for their favorable mortality experience vis-à-vis non-Hispanic whites. Although this finding mainly refers to Mexican-Americans, it is also true of foreign-born other Hispanics. The first direct treatment of the issue indicated that low rates of lung cancer among Hispanics suggests that smoking explains the majority of their life expectancy advantage over non-Hispanic whites (Blue & Fenelon, 2011). The current study improves on this analysis in two ways. First, it establishes a better connection of the findings to real data on cigarette smoking, showing indeed that smoking is less common among Hispanics than non-Hispanic whites, and that this translates into a substantially lower mortality burden of smoking. Second, examining the process by nativity and specifically among Mexican-Americans reveals meaningful variation within the Hispanic population both in mortality and in the impact of smoking. The current study also demonstrates that the smoking explanation is consistent with the educational pattern of the Hispanic advantage. A relatively high burden of smoking among less educated whites partially helps to explain why the life expectancy advantage for Mexican-Americans is concentrated among those with low SES. This finding is consistent with evidence that social gradients in health in rural Mexico are quite flat and that Mexican immigrants import social patterns of health and health behaviors (Buttenheim et al., 2010; Smith & Goldman, 2007).
Another important contribution is a direct test of the selective migration hypothesis in explaining the low smoking prevalence among Mexican immigrants in the United States. This is the first examination of selective migration with respect to cigarette smoking. The results reveal no evidence of the selective migration of non-smokers from Mexico. On the contrary, Mexican individuals who migrate to the United States are about as likely to smoke as their counterparts who remain in Mexico, and smoke at comparable rates after arriving in the US. Cigarette smoking itself does not appear to present a barrier to migration, which is consistent with previous research documenting that health selection among Mexican immigrants is relatively weak, perhaps due to geographic proximity (Akresh & Frank, 2008; Rubalcava et al., 2008).
The finding that Mexican-born individuals in both Mexico and the United States smoke at very similar rates may support the cultural hypothesis, although NHIS data are insufficient to test the particular pathways through which Mexican culture might discourage smoking. Cultural norms in Mexico tend to stress the role of the group in health and social considerations (Gallo et al., 2009). The “allocentric” perspective places the needs of the group above those of the individual, which may eliminate some individual health behavior decision-making (Almeida et al., 2009). Alternatively, comparatively low smoking among Mexicans may not reflect cultural considerations at all. Although rarely considered in studies on the Hispanic paradox, an additional explanation concerns the relatively high cost of cigarettes relative to income in Mexico. Efforts by the tobacco industry in Mexico have been particularly potent, including attempts by cigarette companies to limit regulations to less strict versions of the World Health Organization recommendations (Samet et al., 2006). Despite widespread salience of the tobacco industry, smoking may be kept low partially due to economic considerations of cigarette pricing. In Mexico, individuals in disadvantaged communities often exchange single cigarettes. The “Sachet economy”, buying less more often, has widespread effects on the consumption of non-necessities (Singh et al., 2009). This model is highly prevalent as a cost containment method in Mexico, and smokers who purchase single cigarettes often smoke less than they would if cigarettes were available only in packs (Thrasher et al., 2009). If we assume that low smoking among Mexicans reflects an exclusively behavioral-cultural orientation rather than economic considerations, we may incorrectly conclude that smoking will remain low as incomes rise in Mexico.
The principal limitation of this study is the inability to account for return migration. Even if return migrants are no less healthy than those who remain in the US, Hispanic mortality will still be biased because deaths that occur abroad are unobserved in US vital registration. As Palloni and Arias (2004) indicate, this will lead to an increase in the size of the advantage at older ages as return migration increases. Despite findings that salmon bias explains only very little of the Hispanic advantage (Abraido-Lanza et al., 1999; Turra & Elo, 2008), it remains an issue that the present data cannot completely address and is the toughest challenge to the Hispanic paradox (Markides & Eschbach, 2005). To fully address the challenge of salmon bias would require multinational data capturing the mortality experience of foreign-born individuals outside the United States. Such data are currently unavailable for most purposes.
Conclusion
The Hispanic paradox represents an important situation in social science research in which a group with lower socioeconomic status outperforms the high-status majority group with respect to health outcomes. Explaining the Hispanic paradox thus improves our knowledge of the factors that mediate the relationship between socioeconomic status and health, in addition to providing a fruitful description of the mortality experience of Hispanics. This study also provides strong evidence that the favorable health and mortality experience of Mexican immigrants in the United States is not a consequence of selective migration. This finding is important in itself, but it should also inform a future research agenda on the factors that mediate the relationship between socioeconomic status and health for other immigrant groups in the United States. Studies examining better-than-expected health outcomes among immigrant populations should not assume that these findings are being driven by health-selective migration, and should look deeper into social, economic, and behavioral characteristics of the migrant populations, both in their origin countries and in the United States. As the results of the current study show, testing for selective migration requires measuring health (behaviors) among those who migrate as well as those who do not.
Recognizing that smoking is the primary proximate reason for the life expectancy advantage of Mexican-Americans is important but is less policy relevant before we understand the underlying reasons for extant disparities in smoking. The results of this study confirm that migrant selection effects are not responsible for low smoking among Mexicans. Whatever does keep smoking low in Mexico, it appears to be retained more effectively in the United States by the immigrants themselves than by their children. Foreign-born Mexican-Americans live one and a half years longer at age 35 than Mexican-Americans born in the United States. The gap among other Hispanic subgroups is even larger, 3–4 years. Among Hispanics, there is evidence that linguistic and cultural assimilation is accompanied by behavioral assimilation (Acevedo-Garcia et al., 2005); health behaviors converge to the mainstream norm with greater exposure to US cultural and social norms, and this includes heavier smoking among US-born Hispanics than their parents’ generation (Gordon-Larsen et al., 2003). This realization presents an opportunity for policymakers to improve the health of U.S. populations. Policy interventions designed to reduce the impact of smoking should prioritize research aimed at understanding the smoking behavior of Mexican immigrants in the United States. The specific factors that keep smoking low among Mexican-born populations might also be generalized to benefit other immigrant and non-immigrant populations in the United States that suffer a high burden of smoking. As knowledge of the role of smoking in population health grows, it will become increasingly important for policymakers to identify paths to reducing its impact, particularly in high-risk populations.
Smoking contributes 1.9 years to the advantage of foreign-born Mexican-American women and 1.3 to the advantage of men compared with non-Hispanic whites, 60% of the total advantage
The contribution of smoking is larger for foreign-born Hispanics than for US-born Hispanics
Smoking explains 50% of the difference between non-Hispanic whites and Mexican-Americans in the size of the educational gap in life expectancy
Selective migration does not explain favorable smoking behavior among Mexicans in the US
Appendix: Sensitivity and Robustness
In order to examine the sensitivity of the results to the attributable-risk method and model selection, I perform several robustness checks. To investigate the sensitivity of the results to this choice of attributable-risk method, I also estimate attributable-risk using an indirect method developed by Preston et al. (2010) and refined by the analysis in Fenelon and Preston (2012). This method uses the lung cancer death rate as an indicator of the cumulative damage from smoking in a population. The approach is supported by evidence that smoking is responsible for the vast majority of lung cancer deaths and that differences in lung cancer mortality across populations and over time largely reflect differences in smoking (Peto et al., 1992). I estimate age-specific lung cancer death rates by race/ethnic group using hazard regression. The regression predicts the hazard of lung cancer death, treating deaths for all other causes of death as censoring. These rates are used to calculate attributable-risk based on coefficients estimated in Fenelon and Preston (2012). Results using this attributable-risk method are presented in Table A1. The results indicate that the main findings are robust to alternative attributable risk methods. Although this produced a slight difference in the estimated contribution of smoking, the substantive conclusion remained unchanged.
Table A1.
Contribution of Smoking using alternative attributable risk method: Life expectancy at age 50
| Life Expectancy Advantage | Advantage Explained by Smoking | % of advantage attributable to smoking | |
|---|---|---|---|
| Women
|
|||
| US-born Mexican-American | 1.89 (1.8 – 2.1) | 1.70 (1.4 – 2.0) | 90.10% |
| US-born other Hispanic | −1.90 (−2.2 – −1.6) | −0.89 (−1.2 – −0.6) | 46.84% |
| Foreign-born Mexican-American | 2.73 (2.6 – 2.9) | 1.60 (1.3 – 1.9) | 58.60% |
| Foreign-born other Hispanic | 2.84 (2.6 – 3.1) | 1.74 (1.5 – 2.0) | 61.10% |
| Men
|
|||
| US-born Mexican-American | 0.82 (0.5 – 1.2) | 0.87 (0.6 – 2.1) | 106.10%1 |
| US-born other Hispanic | −0.16 (−0.5 – 0.2) | 0.23 (−0.2 – 0.5) | −143.8%2 |
| Foreign-born Mexican-American | 1.99 (1.7 – 2.3) | 1.54 (1.3 – 1.8) | 77.40% |
| Foreign-born other Hispanic | 2.70 (2.4 – 3.0) | 1.68 (1.4 – 2.0) | 62.20% |
Notes: Life expectancy advantages are in years at age 50. Smoking-attributable mortality and contribution of smoking estimated using indirect method developed in Preston et al. (2010) and refined in Fenelon and Preston (2012). 95% confidence intervals in parentheses.
Contribution greater than 100% indicates that, in the absence of smoking, US-born Mexican-American men would be disadvantaged relative to non-Hispanic white men.
This percentage contribution is not statistically distinguishable from zero.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Pan J, Jun HJ, Osypuk TL, Emmons KM. The effect of immigrant generation on smoking. Social Science & Medicine. 2005;61(6):1223–1242. doi: 10.1016/j.socscimed.2005.01.027. [DOI] [PubMed] [Google Scholar]
- Akresh IR, Frank R. Health Selection Among New Immigrants. American Journal of Public Health. 2008;98(11):2058–2064. doi: 10.2105/AJPH.2006.100974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J, Kawachi I, Molnar BE, Subramanian SV. A Multilevel Analysis of Social Ties and Social Cohesion among Latinos and Their Neighborhoods: Results from Chicago. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2009;86(5):745–759. doi: 10.1007/s11524-009-9375-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias E. United States Life Tables by Hispanic Origin. Vital Health Statistics. 2010;152(2) [PubMed] [Google Scholar]
- Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Statistics. 2008;(148):1–23. [PubMed] [Google Scholar]
- Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: A review. American Journal of Preventive Medicine. 2005;29(2):143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Blue L, Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: the role of smoking. International Journal of Epidemiology. 2011;40(3):786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttenheim AM, Goldman N, Pebley AR, Wong R, Chung C. Do Mexican immigrants “import” social gradients in health to the US? Social Science & Medicine. 2010;71(7):1268–1276. doi: 10.1016/j.socscimed.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, Mowery PD, Richter PA, Strauss WJ, Sharp DJ, et al. Racial and ethnic differences in serum cotinine levels of cigarette smokers - Third National Health and Nutrition Examination Survey, 1988–1991. Journal of the American Medical Association. 1998;280(2):135–139. doi: 10.1001/jama.280.2.135. [DOI] [PubMed] [Google Scholar]
- Elo IT, Turra CM, Kestenbaum B, Ferguson BR. Mortality among elderly Hispanics in the United States: Past evidence and new results. Demography. 2004;41(1):109–128. doi: 10.1353/dem.2004.0001. [DOI] [PubMed] [Google Scholar]
- Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: Is there a barrio advantage? American Journal of Public Health. 2004;94(10):1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A, Preston SH. Estimating Smoking-Attributable Mortality in the United States. Demography. 2012;49(3):797–818. doi: 10.1007/s13524-012-0108-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Penedo FJ, de los Monteros KE, Arguelles W. Resiliency in the Face of Disadvantage: Do Hispanic Cultural Characteristics Protect Health Outcomes? Journal of Personality. 2009;77(6):1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the national longitudinal study of adolescent health. Social Science & Medicine. 2003;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Hummer RA, Rogers RG, Amir SH, Forbes D, Frisbie WP. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Social Science Quarterly. 2000;81(1):459–476. [PubMed] [Google Scholar]
- IHIS. Minnesota Population Center and State Health Access Data Assistance Center. Minneapolis: University of Minnesota; 2010. Jul, Integrated Health Interview Series: Version 2.0. [Google Scholar]
- Marin G, Marin BV. Research with Hispanic Populations. 1. Sage Publications, Inc; 1991. [Google Scholar]
- Markides KS, Coreil J. The Health of Hispanics in the Southwestern United-States - An Epidemiologic Paradox. Public Health Reports. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic paradox. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2005;60:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Palloni A, Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Palloni A, Ewbank DC. Selection processes in the study of racial and ethnic differentials in adult health and mortality. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox - Demographic and epidemiologic approaches. In: Weinstein M, Hermalin AI, Stoto MA, editors. Population Health and Aging - Strengthening the Dialogue between Epidemiology and Demography. Annals of the New York Academy of Sciences; 2001. pp. 140–174. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, Marti J, et al. Cigarette smoking behavior among US Latino men and women from different countries of Origin. American Journal of Public Health. 2001;91(9):1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peto R, Lopez AD, Boreham J, Thun MJ, Heath C. Mortality From Smoking in Developed Countries - Indirect Estimation From National Vital-Statistics. Lancet. 1992;339(8804):1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- Preston SH, Glei DA, Wilmoth JR. A new method for estimating smoking-attributable mortality in high-income countries. International Journal of Epidemiology. 2010;39(2):430–438. doi: 10.1093/ije/dyp360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston SH, Heuveline P, Guillot M. Demography: measuring and modeling population processes. Wiley-Blackwell; 2001. [Google Scholar]
- Rodriguez S. Hispanics in the United States: An insight into group characteristics. Washington DC: Department of Health and Human Services; 1995. [Google Scholar]
- Rogers RG, Hummer RA, Krueger PM, Pampel FC. Mortality attributable to cigarette smoking in the United States. Population and Development Review. 2005;31(2):259–292. doi: 10.1111/j.1728-4457.2005.00065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubalcava LN, Teruel GM. User’s Guide for the Mexican Family Life Survey Second Wave. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: New findings from the Mexican family life survey. American Journal of Public Health. 2008;98(1):78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet J, Wipfli H, Perez-Padilla R, Yach D. Mexico and the tobacco industry: doing the wrong thing for the right reason? BMJ. 2006;332(7537):353. doi: 10.1136/bmj.332.7537.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, Singh GK, Jones PR, Timsina LR. Racial/ethnic and socioeconomic variations in duration of smoking: results from 2003, 2006 and 2007 Tobacco Use Supplement of the Current Population Survey. Journal of Public Health. 2010;32(2):210–218. doi: 10.1093/pubmed/fdp104. [DOI] [PubMed] [Google Scholar]
- Singh, Ang RP, Sy-Changco JA. Buying less, more often: an evaluation of sachet marketing strategy in an emerging market. The Marketing Review. 2009;9:3–17. [Google Scholar]
- Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Smith &, Goldman N. Socioeconomic differences in health among older adults in Mexico. Social Science & Medicine. 2007;65:1372–1385. doi: 10.1016/j.socscimed.2007.05.023. [DOI] [PubMed] [Google Scholar]
- Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic Status in the United States. Journal of the American Medical Association. 1993;270(20):2464–2468. [PubMed] [Google Scholar]
- Thrasher JF, Villalobos V, Dorantes-Alonso A, Arillo-Santillán E, Cummings KM, O’Connor R, Fong GT. Does the availability of single cigarettes promote or inhibit cigarette consumption? Perceptions, prevalence and correlates of single cigarette use among adult Mexican smokers. Tobacco Control. 2009;18(6):431–437. doi: 10.1136/tc.2008.029132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thun MJ, Apicella LF, Henley SJ. Smoking vs other risk factors as the cause of smoking-attributable deaths - Confounding in the courtroom. Journal of the American Medical Association. 2000;284(6):706–712. doi: 10.1001/jama.284.6.706. [DOI] [PubMed] [Google Scholar]
- Turra CM, Elo IT. The impact of salmon bias on the Hispanic mortality advantage: New evidence from social security data. Population Research and Policy Review. 2008;27(5):515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turra CM, Goldman N. Socioeconomic differences in mortality among US adults: Insights into the Hispanic paradox. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2007;62(3):S184–S192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. 2010 Census Summary File 1—United States. Vol. 2011 prepared by the U.S. Census Bureau; 2011. [Google Scholar]