Abstract
Objective
Preterm children are at greater risk for psychiatric disorders than their term-born peers including anxiety disorders and ADHD. Prior research has focused primarily on children born at early gestational ages. Less is known about the rate of psychiatric disorders among late preterm or early term children. Additionally, whether a history of maternal depression, also associated with prematurity, impacts the risk for psychiatric disorders remains underexplored.
Method
Preschoolers between ages 3 and 6 years (N=306) were recruited for a study examining preschool depression that included healthy and disruptive preschoolers. Preschoolers were placed in the following groups: Late preterm (34–36 weeks, n=39), early term (37–39 weeks, n=78) and full term (40–41 weeks, n=154). DSM-IV psychiatric disorders were assessed via the Preschool Age Psychiatric Assessment. Maternal history of psychiatric disorders was assessed using the Family Interview for Genetic Studies.
Results
Late preterm children had higher rates of any Axis I psychiatric diagnosis (odds ratio [OR] 3.18, CI 1.09–4.76) and of any anxiety disorder (OR 3.74, CI 1.59–8.78) than full term children after adjusting for gender, ethnicity, family income, and IQ. There were no differences in rates of psychiatric diagnoses between early term and full term children. A history of maternal depression mediated the relationship between late preterm birth and anxiety disorders in preschoolers.
Conclusions
Late preterm children were at increased risk for anxiety disorders at preschool age. A history of maternal depression mediated this association. Findings confirm the extension of the risk of psychiatric disorders associated with prematurity to the late preterm group, and suggest that maternal depression may play a key role in this risk trajectory.
Keywords: preterm, anxiety disorders, maternal depression, preschool, psychiatric disorders
INTRODUCTION
Preterm birth is a major public health problem, principally due to the high risk for adverse medical and developmental outcomes in survivors. Additionally, there is a growing literature reporting increased rates of psychiatric disorders in preterm children, specifically anxiety, depression, attention/deficit-hyperactivity disorder (ADHD), particularly inattentive type, and autism.1–5 The majority of research, however, has focused on those born prior to 30 weeks. Yet, late preterm births, typically between 34 to 36 weeks gestation, are the largest cohort of premature children comprising 70 percent of preterm births in 2009.6 Recent evidence supports an increased rate of psychiatric symptoms in late preterm children as well, particularly ADHD,7 “emotional”, and anxiety symptoms.8 Other investigations, however, have failed to detect a difference in the rates of psychiatric symptoms between late preterm and full term children.9 The small body of research evaluating the psychiatric outcomes of late preterm children has been limited by the reliance on symptom checklists, retrospective review of records or by investigation of child outcomes at a broad range of developmental stages.
There has been recent interest in the “early term” group (born between 37 and 39 weeks gestation) as new evidence suggests this group may have poorer outcomes than previously recognized. Indeed, there is increased perinatal mortality and morbidity for infants born early term.10,11 Similarly, a large population-based study found that early term infants are at increased risk for special education needs well into school-age.12 While this may have included children with psychiatric disorders, whether early term children also have higher risk for psychiatric disorders remains unclear.
Another important factor is the potential impact of maternal history of depression on the risk for psychiatric disorders among late preterm and early term children. Postpartum depressive symptoms are increased among mothers of preterm infants.13,14 Maternal depression is strongly related to increased risk for psychiatric symptoms and disorders in child offspring. This risk is conferred not only by independent but also interactive genetic and environmental mechanisms.15 For instance, maternal hostility and warmth has been found to mediate the relationship between maternal depressive symptoms and child psychopathology in the setting of genetic risk.16 Moreover, preterm infants may be particularly vulnerable to the reduced maternal emotional responsivity associated with poor maternal mental health17,18 as preterm infants have been noted to have poorer state, attention, and greater self-regulatory disorganization and reactivity19 likely secondary to the underdevelopment of their central nervous system (CNS) at birth. Thus, preterm infants with mothers with a history depression may be at increased risk of childhood psychopathology because of the interaction of their genetic and biologic risk (poor self-regulation secondary to altered neurodevelopment) with their exposure to maladaptive parenting behaviors associated with depression. Similarly, mothers of preterm infants have elevated anxiety20,21 also known to increase the risk of psychopathology in child offspring.22,23 Thus, maternal depression or anxiety may play an important role in the risk for mental disorders in preterm infants, a mechanism not previously well-investigated.
Thus, this study aimed to compare those born late preterm, early term, and full term for risk of psychiatric disorders at preschool age. This investigation used a prospectively studied sample of preschoolers utilizing a comprehensive preschool psychiatric interview. Prior research investigating psychiatric disorders and prematurity has recruited cohorts of preterm infants and controls and compared rates of later childhood psychiatric disorders. In contrast, this study assessed the role of preterm birth in the development of preschool psychiatric disorders among preschoolers ascertained for psychiatric symptoms and healthy controls. A secondary aim was to investigate the relationship of maternal history of major depressive disorder and anxiety disorders on preschool psychopathology.
METHOD
Participants
Preschoolers between ages 3 and 6 years (N=306) were recruited from community sites for a study examining the nosology of preschool depression.24,25 Methods of sample recruitment have been described previously.26 A validated screening checklist, The Preschool Feelings Checklist (PFC)27 was completed by caregivers to identify children with high depression or disruptive symptoms. Preschoolers with depressive or disruptive symptoms were oversampled to address key aims of interest of the larger longitudinal study. Those with low or no symptoms were also included to provide a healthy comparison group.
Diagnostic Assessment
The Preschool Age Psychiatric Assessment (PAPA)28 was used to establish DSM-IV Axis I diagnoses. The PAPA is an interviewer-based diagnostic assessment with empirically established test re-test reliability designed for use with caregivers of children aged 2.0–6.0.29 The PAPA covers a broad range of psychiatric symptoms and impairment/disability from symptoms. It was administered by bachelor or masters-level clinicians and final diagnoses were derived using computerized algorithms. All interviews were audiotaped for quality control and group calibration. As recommended by the authors of the measure, in lieu of calculation of interrater reliability, 20% of each interviewer’s tapes were reviewed by a master coder, and when discrepancies arose, they were recoded in consultation with a senior child psychiatrist (J.L.L.). Additionally, weekly coding meetings with interviewers and a master rater were conducted to maintain calibration and avoid rater drift.
Full-scale IQ was obtained utilizing the Vocabulary and Matrix reasoning subscales of the Wechsler Abbreviated Scale of Intelligence (WASI)30 during subsequent follow-up assessments (between ages of 6 and 9).
Maternal Psychiatric History
Maternal history of psychiatric disorders was determined using the Family Interview for Genetic Studies (FIGS), a widely used measure of family history of psychiatric disorders administered by trained interviewers.31 Primary caregivers (92% biological mothers) provide psychiatric histories for all first- and second-degree biological relatives. Any history of major depressive disorder or an anxiety disorder (separation anxiety disorder, generalized anxiety disorder, and posttraumatic stress disorder [PTSD]) was recorded using a dichotomous (yes or no) variable. The age of onset of the first depressive episode and the number of episodes were also recorded. Using mothers’ age at birth of the index child, the timing of the initial episode of depression in relation to the child’s birth (prenatal vs. postnatal) was derived.
Preterm Birth
Gestational age at birth (completed weeks) was reported by the child’s primary caregiver. Gestational age (GA) groups were categorized as follows: Late preterm (LP; 34–36 weeks), early term (ET; 37–39 weeks) and full term (FT; 40–41 weeks). Children born prior to 34 weeks (n=9) or after 41 weeks (n=19) were excluded to minimize confounds due to potentially extensive neurodevelopmental deficits (among those born prior to 34 weeks) and any neurodevelopmental effects of postmaturity. Preschoolers with chronic medical or neurological problems, mental retardation, or autistic spectrum disorders were also excluded.
Data Analysis
Differences in sociodemographic variables between the three GA groups were tested via analysis of variance (ANOVA) and chi-square analyses. The relationship between gestational age and developing any psychiatric disorder was analyzed using univariate logistic regressions with gestational age entered first as a continuous variable. Subsequently, in order to investigate whether those children born late preterm or early term were at particular risk compared to term children, GA group was also entered as a categorical variable. Similar regressions were run for specific disorders (present/absent) as follows: separation anxiety disorder (SAD), generalized anxiety disorder (GAD), major depressive disorder (MDD), ADHD, Oppositional Defiant Disorder, Conduct Disorder, and PTSD. Gender, family income, and IQ are widely associated with increased risk for psychiatric disorders and therefore included as covariates.1,32,33 Rates of preterm birth vary by ethnicity, thus ethnicity was also included as a covariate.34 Maternal MDD was tested as a possible mediator for any significant relationship between gestational age and psychiatric outcomes via a bootstrapping method which estimates standard errors of the direct and indirect effects for significance testing.35 Current analyses utilized 5,000 bootstrap resamples to generate 95% confidence intervals with Mplus 7.0 statistical software. Maternal MDD was tested as a moderator by adding the interaction of maternal MDD and GA group to the logistic regression model including covariates described above.
RESULTS
Characteristics of the sample are presented in Table 1. Seven children were excluded due to missing PAPA data, leaving n=271 available for analysis. FT infants were less likely to be White than either LP (chi-square=7.09, p =.03) or ET infants (chi-square=8.72, p=.013). LPs were more likely to have a maternal MDD history than either ET (chi-square=5.63, p=0.018) or FT infants (chi-square=8.33, p=0.004).
Table 1.
Cohort Characteristics by Gestational Age (GA) Group
| Characteristic | Late Preterm (GA 34–36 weeks) (n=39) | Early Term (GA 37–39 weeks) (n=78) | Full Term (GA 40–41 weeks) (n=154) |
|---|---|---|---|
|
| |||
| Male, % | 53.8 | 50.0 | 50.6 |
|
| |||
| Ethnicity, % | |||
| White | 66.7 | 66.7 | 46.8* |
| Black | 30.8 | 20.5 | 37.0 |
| Other | 2.6 | 12.8 | 16.2 |
|
| |||
| Age in months, mean (SD) | 52.72 (7.9) | 53.12 (9.9) | 52.90 (10.10) |
|
| |||
| GA at birth, weeks, mean (SD) | 35.31 (0.8) | 38.17 (0.8) | 40.37 (.7) |
|
| |||
| Income | |||
| ≤20,000 | 22.2 | 16.9 | 23.8 |
| 20,001–40,000 | 25.0 | 16.9 | 16.8 |
| 40,001–60,000 | 19.4 | 12.7 | 20.3 |
| ≥60,001 | 33.3 | 53.5 | 39.2 |
| IQ, M (SD) | 104.1 (14.1) | 106.6 (15.5) | 103.5 (17.9) |
|
| |||
| History of Maternal MDD, % | 44.7* | 23.0 | 21.6 |
| Age of onset, mean (SD) | 22.2 (9.2) | 20.0 (11.2) | 23.2 (7.5) |
| Median number of episodes | 3 | 2 | 2 |
Note: MDD = major depressive disorder; NICU= Neonatal Intensive Care Unit.
p<.05
Analyses evaluating gestational age as a continuous variable noted decreased GA was associated with increased risk for developing any psychiatric disorder (unadjusted: OR 0.89, 95% CI 0.78–1.02, p=.086 ; adjusted OR 0.84, 95% CI 0.72–0.97 p=.019) and for any anxiety disorder (unadjusted: OR 0.86, 95% CI 0.74–0.99, p=.041 ; adjusted OR 0.81, 95% CI 0.69–0.96, p=.014). Risks for other disorders were not significantly related to gestational age (data not shown). We then evaluated this risk based on whether children were born late preterm or early term. Figure 1 displays frequencies for preschool psychiatric diagnoses for the 3 GA groups. Table 2 displays unadjusted and adjusted ORs for the risk of psychiatric disorders in LP compared to FT. LP infants were more likely to have any psychiatric diagnosis (OR =2.28, 95% CI 1.09–4.76, p=.03) compared to the FT group. These relationships were strengthened after adjusting for gender, ethnicity, family income, and IQ (OR =3.74, 95% CI 1.59–8.78, p=.002).
Figure 1.
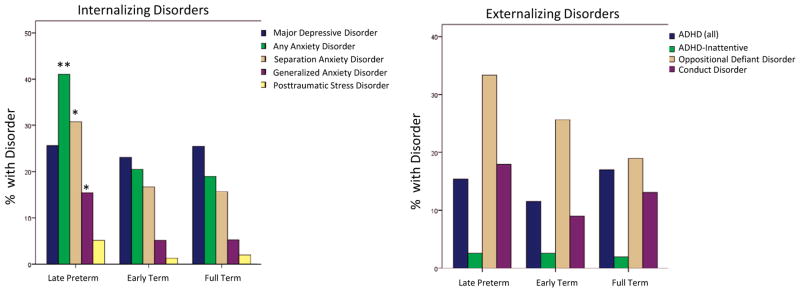
Comparison of the frequencies of internalizing (LEFT) and externalizing disorders (RIGHT) for the late preterm, and early term children compared to full term children. Note: ADHD = attention-deficit/hyperactivity disorder. *p<.05, **p<.01.
Table 2.
Odds Ratios (OR) for Preschool Psychiatric Diagnoses by Gestational Age Group
| Late Preterm | EaEarly Term | Full Term | Unadjusted ORa (95% CI) | Adjusted ORa (95% CI) | |
|---|---|---|---|---|---|
| Any Psychiatric Diagnosis, n (%) | |||||
| Including childhood MDD | 26 (66.7) | 39(50.0) | 72 (46.8) | 2.28 (1.09–4.76)* | 3.18 (1.40–7.27)** |
| Excluding childhood MDD | 22 (56.4) | 34 (43.6) | 63 (40.9) | 3.15 (1.36–7.29)** | 4.22 (1.64–10.8.4)** |
| MDD | 10 (25.6) | 18 (23.1) | 39 (25.5) | 1.01 (0.45–2.26) | 1.16 (0.49–2.74) |
| ADHD | 6 (15.4) | 9 (11.5) | 26 (17.0) | 0.89 (0.34–2.34) | 0.81 (0.29–2.29) |
| ADHD-inattent | 1(2.6) | 2 (2.6) | 3 (1.9) | 1.33 (0.134–13.09) | 1.21 (0.11–13.22) |
| ODD | 13(33.3) | 20 (25.6) | 29 (19.0) | 2.14 (0.98–4.66) | 2.30 (0.98–5.40) |
| CD | 7 (17.9) | 7 (9.0) | 20 (13.1) | 1.45 (0.57–3.74) | 1.60 (0.55–4.66) |
| Any Anxiety Diagnosis | 16 (41.0) | 16 (20.5) | 30 (19.5) | 2.88 (1.36–6.10)** | 3.74 (1.59–8.78)** |
| GAD | 6 (15.4) | 4 (5.1) | 8 (5.2) | 3.30 (1.07–10.14)* | 3.50 (1.03–11.94)* |
| SAD | 12 (30.8) | 13 (16.7) | 24 (15.7) | 2.39 (1.07–5.36)* | 3.04 (1.21–7.63)* |
| PTSD | 2 (5.1) | 1 (1.3) | 3 (2.0) | 2.73 (0.44–16.76) | 6.15 (0.57–66.23) |
Note: Adjusted for gender, ethnicity, family income, and IQ. ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; GAD = generalized anxiety disorder; inattent = inattentive type; MDD = major depressive disorder; ODD = oppositional defiant disorder; PTSD = posttraumatic stress disorder; SAD = separation anxiety disorder.
= Odds Ratio calculated for Late preterm compared to full term.
p=≤.05,
p=<.01
LP children had significantly greater odds of any anxiety disorder compared to FT (41.0% and 19.5% respectively; unadjusted OR 2.88, CI 1.36–6.10; adjusted OR 3.85, CI 1.52–9.52). LP children had increased odds of both GAD (OR 3.30, CI 1.07–10.14) and SAD (OR 2.39, CI 1.07–5.36). After adjustment for covariates both SAD (OR 3.04, CI 1.21–7.63) and GAD (OR 3.50, CI 1.03–11.94) remained significant. There were no significant differences between ET and FT children for any psychiatric disorder.
History of Maternal Depression and Childhood Anxiety Disorders
As LP children were more likely to have a maternal MDD history (Table 1) compared to FT (chi-square=8.33, p=.004) and ET infants (chi-square=5.63, p=.018), a logistic regression tested whether maternal depression history altered the strength of the relationship between LP birth and preschool anxiety disorders (Table 3). IQ, the only significant covariate, was also retained in the model and entered simultaneously with the other predictors. With the addition of maternal MDD, the relationship between LP birth and preschool anxiety disorders was no longer significant, supporting full mediation.
Table 3.
Impact of Maternal Major Depressive Disorder (MDD) History on the relationship of Late Preterm Birth and Preschool Anxiety Disorders.
| Factor | Adjusted OR | 95% CI | p |
|---|---|---|---|
| Late preterm | 1.94 | 0.79–4.73 | .15 |
| IQ | 0.96 | 0.94–0.98 | <.001 |
| History of Maternal MDD | 4.86 | 2.25–10.48 | <.001 |
Note: All factors were entered simultaneously in the model; OR = odds ratio.
We then formally tested for potential mediation or moderation of the relationship between gestational age as a continuous variable and presence of preschool anxiety disorders. Table 4 displays the mediation analysis. Eight mothers reported a single episode of MDD prior to the pregnancy or birth of the index child, and were excluded from the mediation analysis. Nineteen mothers reported age of onset occurring between the index child’s birth and the study assessments. The remaining 29 mothers reported first onset of MDD prior to the index child’s birth with recurrent episodes (median number of episodes = 3). Therefore, we included these subjects in the mediation analysis as they were highly likely to have had an episode occurring between the index child’s birth and participation in the study (however specific onset and timing of episodes after the first episode of MDD was not collected). Results yielded a significant indirect effect of GA on preschool anxiety disorders through maternal MDD (estimate=−0.038; 95% CI −0.079, −0.011). The direct effect of GA on preschool anxiety disorders was no longer significant (p=.26) indicating maternal MDD fully mediated the relationship. Maternal MDD was then evaluated as a moderator by adding the interaction of GA and maternal depression to the logistic regression model. The interaction was not significant, indicating maternal depression served as a mediator but not a moderator between gestational age and preschool anxiety disorders.
Table 4.
Maternal major depressive disorder (MDD) as a Mediator between Gestational Age and Preschool Anxiety Disorders
| Estimate (95% CI) | |
|---|---|
|
| |
| Gestational Age on Maternal MDD | −0.104 (−0.179, −0.028)* |
|
| |
| Maternal MDD on Preschool Anxiety Disorders | 0.362 (0.181, 0.521)*** |
| Gestational Age on Preschool Anxiety Disorders | −0.052 (−0.131, 0.020) (p=.261) |
|
| |
| Indirect Effect of Gestational Age via Maternal MDD on Preschool Anxiety Disorders | −0.038 (−0.079, −0.011)* |
Note:
p< .05,
p<.001
Given common comorbidity between MDD and anxiety disorders, two post hoc analyses were conducted. First, we examined whether the relationship between maternal MDD and preschool anxiety disorders was only due to children with both MDD and anxiety disorders. Comorbid MDD and anxiety disorders were diagnosed in 15%, 9% and 10% of the LP, ET, and FT children, respectively. After restricting the models to those children without comorbid MDD (LP n=29, ET n=60, FT n=114), compared to the data for the entire sample (Table 2), we found the relationship between late preterm birth and preschool anxiety disorders among children without comorbid MDD was stronger in univariate (OR 3.76, CI 1.46–9.70, p=.006) and multivariate analyses adjusting for maternal MDD and IQ (OR 3.34, CI 1.19–9.33, p=.02). Second, maternal anxiety history was not a significant predictor of preschool anxiety disorders in multivariate analysis (OR 1.71 CI 0.63–4.61, p=.29).
DISCUSSION
This investigation of preschool-age children ascertained on the basis of psychiatric symptoms (including those with and without psychiatric disorders) found those born late preterm were three times more likely than term born children to have an Axis I psychiatric diagnosis by preschool age. This study took a unique approach by utilizing a semi-structured diagnostic interview within a sample of preschoolers with a range of gestational ages to assess for DSM-IV psychiatric disorders. Prior studies have either reported on disorders at later ages or used checklists to assess symptoms at earlier ages. Additionally, we examined the role of maternal depression on the relationship between late preterm birth and preschool psychiatric disorders. Notably, the association between late preterm birth and anxiety disorders was significantly mediated by maternal MDD history, a finding that may suggest a mechanism for this increased risk and has implications for preventive interventions.
We found a particularly strong association with SAD and GAD even after adjustment for multiple covariates. These results are consistent with prior research that found higher rates of total difficulties and anxiety symptoms8 and findings from studies of older children born very preterm that have found higher rates of total psychiatric disorders and anxiety disorders.1 Among older school-age and adolescent children born either very preterm or very low birth weight, the odds of anxiety disorders have ranged from 3 to 6 times that in control children,1,2,36 with SAD and GAD being particularly prominent.1,2 These findings are important given that preschool onset SAD and GAD may significantly increase the risk for later psychiatric disorders. Previous research in similar high risk samples have found SAD in early childhood is associated with increased risk of agoraphobia, GAD, panic disorder, and MDD 5 years later.37,38 Less data is available on longitudinal outcomes for GAD during preschool age. The current findings support that the increased risk of anxiety disorders associated with preterm birth in the context of maternal MDD can be detected as early as the preschool period opening the door to application of early interventions in this targeted group to decrease long-term morbidity.
While studies in children born at earlier gestational ages have found increased rates of ADHD,5,7 this was not detected in this sample. The literature among late preterm children has been mixed with one study noting an increased rate of ADHD7 while another reported no increase in ADHD symptoms.8 One possible explanation is that ADHD among preterm children has been predominantly inattentive type. Inattentive symptoms are often under-recognized in early childhood perhaps because children are not in an educational setting where inattention is more readily detected. Alternatively, Grunau and colleagues found the relationship between preterm birth and externalizing disorders was dependent upon cognitive status, a factor that was not significantly different between groups in our sample.39
This study also investigated whether children born early term had an elevated risk of psychiatric disorders. While there was a linear relationship between GA and risk of any psychiatric disorders and anxiety disorders, early term children did not appear to be at greater risk than those born full term. While a recent, large, population-based study indicated this group has a higher incidence of learning disorders, the findings from our sample did not detect an increased risk of psychiatric disorders in early term born children. Research with larger samples is needed to clarify whether early term birth is uniquely associated with an increased risk of learning disorders and not psychiatric disorders.
Another aim of this research was to investigate the role of maternal MDD, a known risk factor for increased rates of psychopathology in offspring. The rates of lifetime depression for our term (21.6%) and early term (23.0%) mothers are similar to those noted in the National Comorbidity Survey-Replication of ~25%.40 The late preterm children, however, had significantly more mothers with lifetime histories of MDD, about 45%, similar to previously reported rates of maternal depression in mothers of preterm infants (40%).41 Mothers with depression histories transfer genetic susceptibility for psychopathology to offspring and in this study, among late preterm children, this was manifest as anxiety disorders. Indeed, depression and anxiety disorders share a common genetic liability, which more commonly manifest as anxiety in prepubertal children.42 Prior MDD among mothers of late preterm infants was noted to be a significant mediator between the relationship between late preterm birth and preschool anxiety disorders while a history of maternal anxiety disorders was not. Future studies directly investigating the effects of maternal anxiety among late preterm infants are warranted.
Maternal depression may mediate the relationship between late preterm birth and anxiety disorders in offspring through the interaction of biological, genetic, and environmental mechanisms. Genetic risk for psychopathology and parenting behaviors can act additively or interact to increase risk of psychopathology.43 There is also substantial evidence suggesting transmission is due at least partly to environmental mechanisms as well as shared genetic liability or passive gene–environment (GxE) interactions.44,45 The quality of mother-infant interaction has been theorized to influence social-emotional development throughout the life span46 with two recent longitudinal investigations supporting the importance of mother-infant interactions for the development of psychopathology in childhood throughout young adulthood.47,48 Mothers already vulnerable to the effects of stress due to depression history face additional challenges in providing optimal interactions with a premature infant who may require greater support. Studies have found interactions between depressed mothers and premature infants tend to be intrusive and less coordinated or responsive to infant behaviors, likely because of the difficulties of reading and responding to dysregulated behavior.46 These asynchronous interactions may have long-term effects associated with developing psychopathology in childhood.
Alternatively, depressed mothers may perceive their preterm children as more vulnerable resulting in “vulnerable child syndrome”49 and associated increased over-protective parenting. This pattern has been shown to increase anxiety and internalizing symptoms in the child.50 Similarly, mothers of preterm infants with depression histories rate themselves higher on perceived child vulnerability51 and view their children as less independent52 which could result in parenting styles that promote anxiety in their children. This possibility warrants further study among late preterm infants who are often less medically fragile and potentially less likely to be perceived as vulnerable. Further, maternal depression is associated with increased exposure to stressful life events and other adverse psychosocial factors which are also associated with risk of childhood psychopathology.53
These findings highlight the importance of assessing the effect of maternal depression on the psychiatric outcomes in preterm children. While prior investigations of psychiatric symptoms in preterm children have evaluated the role of maternal or parental psychiatric history or symptoms to some degree,4,7,8,54–56 recent studies assessing DSM-IV psychiatric disorders in preterm children at school age have not.1,5 Thus, future studies should assess maternal psychiatric history to clarify the relative effect of factors specifically related to premature birth, such as brain injuries associated with preterm birth (e.g., white matter injury or cerebellar hemorrhage) versus genetic and parenting factors on preschool psychiatric disorders as our findings indicate that it is those preterm children with a history of maternal psychiatric disorders who are at particular risk.
Strengths of this study include the relatively large sample size, use of a semi-structured age-appropriate diagnostic interview, and measurement of maternal psychiatric history. One limitation of the study is maternal report of gestational age. While confirmation of gestational age with medical records is preferable, research comparing maternal report to hospital records has demonstrated good agreement with high sensitivity and specificity for maternal report of preterm birth.57 Similar studies were conducted 8 to 11 years after delivery noting 93–94% preterm and 81–83 % term accurately reported,58,59 suggesting maternal report has sufficient accuracy. Nevertheless, there is potential for misclassification, particularly of term children, though the pattern of misclassification noted in these studies would typically lead to the term group containing children with typically higher rates of psychiatric symptoms (both postterm and preterm children) and the preterm group with children with a lower likelihood of psychiatric symptoms (term children). Thus, this would make it more likely for our results to be biased toward underestimation of the effect of late preterm birth on psychiatric outcomes.
Another limitation is that the FIGS does not collect exact onset and offset dates of depressive episodes. Therefore, the timing of maternal depression was estimated using maternal age at child’s birth, maternal reported age at first MDD episode, and maternal reported total number of MDD episodes. Given the chronic and highly recurrent nature of depression and the high risk in the peripartum, we assumed at least one of the reported recurrent episodes of maternal depression in 29 women with an initial prenatal MDD episode occurred after the index child’s birth. Even if this is an overestimate, however, maladaptive parenting behaviors have been associated with depression regardless of remission status. 60,61 Residual depressive symptoms are common even after remission, 62 which is particularly important for young children when residual depressive symptoms may most impair a mother’s ability to have adequate parent-child synchrony.61 Although maternal depression is also a risk factor for preterm birth,63 it is beyond the scope of this investigation to elucidate independent effects of prenatal depression on risk for offspring psychopathology. However, common genetic factors underlying maternal prenatal depression and preterm birth could also support a meditational model even in the absence of subsequent maternal depressive episodes after the child’s birth. Future research will need to clarify this issue by measuring maternal MDD during pregnancy and throughout early childhood and evaluating subsequent development of preschool psychiatric disorders.
Other limitations include the oversampling of children with depressive symptoms and disruptive behaviors. Study findings, cannot inform true prevalence rates of those disorders in the community. While these children were recruited for depressive and disruptive symptoms, notably there were no differences in the rates of MDD or disruptive disorders between the three gestational age groups. This finding, coupled with the results of the sensitivity analysis restricted to late preterm children without comorbid MDD support that the findings are not explained by comorbidity between MDD and anxiety disorders. Further, while the preschool cohort was oversampled for psychiatric symptoms, gestational age remained a random variable (consistent with rates in epidemiological samples). An additional limitation was that the primary caregiver (almost always the mother) was the sole reporter; therefore, symptoms may have been over-reported by depressed mothers. This is unlikely, however, given the specificity for anxiety disorders and the absence of differences in other psychiatric disorders.
Future research should utilize larger cohorts of late preterm children with a comprehensive psychiatric assessment to verify these findings and to better understand the relationship between late preterm birth, maternal psychiatric symptoms and risk for early childhood psychiatric disorders. As late preterm children comprise the largest proportion of preterm births, their increased risk of anxiety disorders represents a public health issue that should be addressed via targeted surveillance and early intervention. This is further underscored by previous findings suggesting that environmental factors (i.e. maternal mental health, family conflict, and poverty) are equally or interactionally determinant of post-NICU developmental outcomes as prematurity.64 Our findings highlight the need to assess the role of maternal depression in research investigating the link between preterm birth and psychiatric outcomes in offspring. Moreover, the results point to the importance of screening and treating mothers of preterm children, even late preterm children, for perinatal depression. Identifying these mothers could both potentially lessen the impact of having a mother with depression and determine which preterm children are at greater risk for psychiatric disorders to best target prevention efforts.
Acknowledgments
Funding for this study was provided by grants MH64769-01 (J.L.L.) and K23MH090245 (S.N.L.) from the National Institute of Mental Health (NIMH), 5T32AA007580 (C.E.R.) from the National Institute on Alcohol Abuse and Alcoholism, and UL1 RR024992 (C.E.R.) from the National Center for Research Resources/National Center for Advancing Translational Sciences.
Rebecca Tillman, M.S., of Washington University School of Medicine served as the statistical expert for this research.
The authors wish to thank the entire Early Emotional Development Program team for assistance in manuscript preparation and the families that participated in this research.
Footnotes
Disclosure: Dr. Luby has received grant or research support from NIMH, the National Alliance for Research on Schizophrenia and Depression, the Communities Healing Adolescent Depression and Suicide Coalition, and the Sidney R. Baer Foundation. She has served as a consultant to the Food and Drug Administration Advisory Board. Drs. Rogers and Lenze report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Johnson S, Hollis C, Kochhar P, et al. Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J Am Acad Child Adolesc Psychiatry. 2010;49(5):453–463.e1. [PubMed] [Google Scholar]
- 2.Botting N, Powls A, Cooke RW, Marlow N. Attention deficit hyperactivity disorders and other psychiatric outcomes in very low birthweight children at 12 years. J Child Psychol Psychiatry. 1997;38(8):931–941. doi: 10.1111/j.1469-7610.1997.tb01612.x. [DOI] [PubMed] [Google Scholar]
- 3.Limperopoulos C. Autism spectrum disorders in survivors of extreme prematurity. Clin Perinatol. 2009;36(4):791–805. vi. doi: 10.1016/j.clp.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Indredavik MS, Vik T, Evensen KAI, et al. Perinatal risk and psychiatric outcome in adolescents born preterm with very low birth weight or term small for gestational age. J Dev Behav Pediatr. 2010;31(4):286–294. doi: 10.1097/DBP.0b013e3181d7b1d3. [DOI] [PubMed] [Google Scholar]
- 5.Scott MN, Taylor HG, Fristad MA, et al. Behavior Disorders in Extremely Preterm/Extremely Low Birth Weight Children in Kindergarten. J Dev Behav Pediatr. 2012;33(3):202–13. doi: 10.1097/DBP.0b013e3182475287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin J, Hamilton B, Ventura S, et al. National vital statistics reports. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2011. Births: Final data for 2009. [PubMed] [Google Scholar]
- 7.Linnet KM, Wisborg K, Agerbo E, et al. Gestational age, birth weight, and the risk of hyperkinetic disorder. Arch Dis Child. 2006;91(8):655–660. doi: 10.1136/adc.2005.088872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westrupp EM, Mensah FK, Giallo R, Cooklin A, Nicholson JM. Mental health in low-to-moderate risk preterm, low birth weight, and small for gestational age children at 4 to 5 years: the role of early maternal parenting. J Am Acad Child Adolesc Psychiatry. 2012;51(3):313–323. doi: 10.1016/j.jaac.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Gurka MJ, LoCasale-Crouch J, Blackman JA. Long-term cognition, achievement, socioemotional, and behavioral development of healthy late-preterm infants. Arch Pediatr Adolesc Med. 2010;164(6):525–532. doi: 10.1001/archpediatrics.2010.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark SL, Miller DD, Belfort MA, et al. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200(2):156.e1–4. doi: 10.1016/j.ajog.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 11.Zhang X, Kramer MS. Variations in mortality and morbidity by gestational age among infants born at term. J Pediatr. 2009;154(3):358–362. 362.e1. doi: 10.1016/j.jpeds.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 12.MacKay DF, Smith GCS, Dobbie R, Pell JP. Gestational age at delivery and special educational need: retrospective cohort study of 407,503 school children. PLoS Med. 2010;7(6):e1000289. doi: 10.1371/journal.pmed.1000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anonymous. Prevalence of self-reported postpartum depressive symptoms--17 states, 2004–2005. MMWR Morb Mortal Wkly Rep. 2008;57(14):361–366. [PubMed] [Google Scholar]
- 14.Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- 15.Goodman SH. Depression in mothers. Annu Rev Clin Psychol. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- 16.Harold GT, Rice F, Hay DF, et al. Familial transmission of depression and antisocial behavior symptoms: disentangling the contribution of inherited and environmental factors and testing the mediating role of parenting. Psychological Medicine. 2010;41(06):1175–1185. doi: 10.1017/S0033291710001753. [DOI] [PubMed] [Google Scholar]
- 17.Bugental DB, Beaulieu D, Schwartz A. Hormonal sensitivity of preterm versus full-term infants to the effects of maternal depression. Infant Behav Dev. 2008;31(1):51–61. doi: 10.1016/j.infbeh.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poehlmann J, Fiese BH. The interaction of maternal and infant vulnerabilities on developing attachment relationships. Dev Psychopathol. 2001;13(1):1–11. doi: 10.1017/s0954579401001018. [DOI] [PubMed] [Google Scholar]
- 19.Als H, Duffy FH, McAnulty GB. Behavioral differences between preterm and full-term newborns as measured with the APIB system scores: I. Infant Behavior and Development. 1988;11(3):305–318. [Google Scholar]
- 20.Brandon DH, Tully KP, Silva SG, et al. Emotional responses of mothers of late-preterm and term infants. J Obstet Gynecol Neonatal Nurs. 2011;40(6):719–731. doi: 10.1111/j.1552-6909.2011.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDonald SW, Benzies KM, Gallant JE, et al. A Comparison Between Late Preterm and Term Infants on Breastfeeding and Maternal Mental Health [published online October 17, 2012] Matern Child Health J. 2012 doi: 10.1007/s10995-012-1153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zelkowitz P, Na S, Wang T, Bardin C, Papageorgiou A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatr. 2011;100(5):700–704. doi: 10.1111/j.1651-2227.2010.02128.x. [DOI] [PubMed] [Google Scholar]
- 23.Schreier A, Wittchen H-U, Hofler M, Lieb R. Anxiety disorders in mothers and their children: prospective longitudinal community study. The British Journal of Psychiatry. 2008;192(4):308–309. doi: 10.1192/bjp.bp.106.033589. [DOI] [PubMed] [Google Scholar]
- 24.Gaffrey MS, Belden AC, Luby JL. The 2-week duration criterion and severity and course of early childhood depression: implications for nosology. J Affect Disord. 2011;133(3):537–545. doi: 10.1016/j.jad.2011.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: homotypic continuity and course over 24 months. Arch Gen Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luby JL, Belden AC, Pautsch J, Si X, Spitznagel E. The clinical significance of preschool depression: impairment in functioning and clinical markers of the disorder. J Affect Disord. 2009;112(1–3):111–119. doi: 10.1016/j.jad.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luby JL, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E. The Preschool Feelings Checklist: a brief and sensitive screening measure for depression in young children. J Am Acad Child Adolesc Psychiatry. 2004;43(6):708–717. doi: 10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- 28.Egger H, Asher B, Angold A. The Preschool Age Psychiatric Assessment: Version 1.4. Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences. Durham, NC: Duke University Medical Center; 2003. [Google Scholar]
- 29.Egger HL, Erkanli A, Keeler G, et al. Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA) J Am Acad Child Adolesc Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 30.Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) London: Psychological Corporation; 1999. [Google Scholar]
- 31.Maxwell E. The Family Interview for Genetic Studies: Manual. National Institute of Mental Health, Intramural Research Program–Clinical Neurogenetics Branch The National Institute of Mental Health; 1992. [Google Scholar]
- 32.Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1036–1045. doi: 10.1097/00004583-199708000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry. 2000;39(12):1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Gavin AR, Chae DH, Mustillo S, Kiefe CI. Prepregnancy depressive mood and preterm birth in black and white women: findings from the CARDIA Study. J Womens Health (Larchmt) 2009;18(6):803–811. doi: 10.1089/jwh.2008.0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breitborde NJK, Srihari VH, Pollard JM, Addington DN, Woods SW. Mediators and moderators in early intervention research. Early Intervention in Psychiatry. 2010;4(2):143–152. doi: 10.1111/j.1751-7893.2010.00177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Indredavik MS, Vik T, Heyerdahl S, et al. Psychiatric symptoms and disorders in adolescents with low birth weight. Arch Dis Child Fetal Neonatal Ed. 2004;89(5):F445–450. doi: 10.1136/adc.2003.038943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biederman J, Petty CR, Hirshfeld-Becker DR, et al. Developmental trajectories of anxiety disorders in offspring at high risk for panic disorder and major depression. Psychiatry Res. 2007;153(3):245–252. doi: 10.1016/j.psychres.2007.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hirshfeld-Becker DR, Biederman J, Henin A, et al. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: a five-year follow-up. J Dev Behav Pediatr. 2007;28(3):225–233. doi: 10.1097/01.DBP.0000268559.34463.d0. [DOI] [PubMed] [Google Scholar]
- 39.Grunau RE, Whitfield MF, Fay TB. Psychosocial and academic characteristics of extremely low birth weight (< or =800 g) adolescents who are free of major impairment compared with term-born control subjects. Pediatrics. 2004;114(6):e725–732. doi: 10.1542/peds.2004-0932. [DOI] [PubMed] [Google Scholar]
- 40.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 41.Vigod SN, Villegas L, Dennis C-L, Ross LE. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- 42.Kendler KS, Gardner CO, Lichtenstein P. A developmental twin study of symptoms of anxiety and depression: evidence for genetic innovation and attenuation. Psychol Med. 2008;38(11):1567–1575. doi: 10.1017/S003329170800384X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tarantino LM, Sullivan PF, Meltzer-Brody S. Using animal models to disentangle the role of genetic, epigenetic, and environmental influences on behavioral outcomes associated with maternal anxiety and depression. Front Psychiatry. 2011;2:44. doi: 10.3389/fpsyt.2011.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lewis G, Rice F, Harold GT, Collishaw S, Thapar A. Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. J Am Acad Child Adolesc Psychiatry. 2011;50(5):451–459.e1. doi: 10.1016/j.jaac.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rice F, Harold GT, Boivin J, et al. The links between prenatal stress and offspring development and psychopathology: disentangling environmental and inherited influences. Psychol Med. 2010;40(2):335–345. doi: 10.1017/S0033291709005911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Feldman R. Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J Child Psychol Psychiatry. 2007;48(3–4):329–354. doi: 10.1111/j.1469-7610.2006.01701.x. [DOI] [PubMed] [Google Scholar]
- 47.Feldman R. The relational basis of adolescent adjustment: trajectories of mother-child interactive behaviors from infancy to adolescence shape adolescents’ adaptation. Attach Hum Dev. 2010;12(1–2):173–192. doi: 10.1080/14616730903282472. [DOI] [PubMed] [Google Scholar]
- 48.Schmid B, Blomeyer D, Buchmann AF, et al. Quality of early mother-child interaction associated with depressive psychopathology in the offspring: a prospective study from infancy to adulthood. J Psychiatr Res. 2011;45(10):1387–1394. doi: 10.1016/j.jpsychires.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 49.GREEN M, SOLNIT AJ. REACTIONS TO THE THREATENED LOSS OF A CHILD: A VULNERABLE CHILD SYNDROME. PEDIATRIC MANAGEMENT OF THE DYING CHILD, PART III. Pediatrics. 1964;34:58–66. [PubMed] [Google Scholar]
- 50.Culley BS, Perrin EC, Chaberski MJ. Parental perceptions of vulnerability of formerly premature infants. J Pediatr Health Care. 1989;3(5):237–245. doi: 10.1016/0891-5245(89)90003-5. [DOI] [PubMed] [Google Scholar]
- 51.Allen EC, Manuel JC, Legault C, et al. Perception of child vulnerability among mothers of former premature infants. Pediatrics. 2004;113(2):267–273. doi: 10.1542/peds.113.2.267. [DOI] [PubMed] [Google Scholar]
- 52.Silverstein M, Feinberg E, Young R, Sauder S. Maternal depression, perceptions of children’s social aptitude and reported activity restriction among former very low birthweight infants. Arch Dis Child. 2010;95(7):521–525. doi: 10.1136/adc.2009.181735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rapee RM. Potential role of childrearing practices in the development of anxiety and depression. Clin Psychol Rev. 1997;17(1):47–67. doi: 10.1016/s0272-7358(96)00040-2. [DOI] [PubMed] [Google Scholar]
- 54.Treyvaud K, Anderson VA, Lee KJ, et al. Parental mental health and early social-emotional development of children born very preterm. J Pediatr Psychol. 2010;35(7):768–777. doi: 10.1093/jpepsy/jsp109. [DOI] [PubMed] [Google Scholar]
- 55.Delobel-Ayoub M, Arnaud C, White-Koning M, et al. Behavioral problems and cognitive performance at 5 years of age after very preterm birth: the EPIPAGE Study. Pediatrics. 2009;123(6):1485–1492. doi: 10.1542/peds.2008-1216. [DOI] [PubMed] [Google Scholar]
- 56.Gray RF, Indurkhya A, McCormick MC. Prevalence, stability, and predictors of clinically significant behavior problems in low birth weight children at 3, 5, and 8 years of age. Pediatrics. 2004;114(3):736–743. doi: 10.1542/peds.2003-1150-L. [DOI] [PubMed] [Google Scholar]
- 57.Poulsen G, Kurinczuk JJ, Wolke D, et al. Accurate reporting of expected delivery date by mothers 9 months after birth. J Clin Epidemiol. 2011;64(12):1444–1450. doi: 10.1016/j.jclinepi.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 58.McCormick MC, Brooks-Gunn J. Concurrent child health status and maternal recall of events in infancy. Pediatrics. 1999;104(5 Pt 2):1176–1181. [PubMed] [Google Scholar]
- 59.Adegboye A, Heitmann B. Accuracy and correlates of maternal recall of birthweight and gestational age. BJOG: An International Journal of Obstetrics and Gynaecology. 2008;115(7):886–893. doi: 10.1111/j.1471-0528.2008.01717.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Donatelli J-AL, Bybee JA, Buka SL. What Do Mothers Make Adolescents Feel Guilty About? Incidents, Reactions, and Relation to Depression. Journal of Child and Family Studies. 2007;16(6):859–875. [Google Scholar]
- 61.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 62.Judd LL, Schettler PJ, Akiskal HS. The prevalence, clinical relevance, and public health significance of subthreshold depressions. Psychiatr Clin North Am. 2002;25(4):685–698. doi: 10.1016/s0193-953x(02)00026-6. [DOI] [PubMed] [Google Scholar]
- 63.Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Müller JM, Achtergarde S, Furniss T. The influence of maternal psychopathology on ratings of child psychiatric symptoms: an SEM analysis on cross-informant agreement. Eur Child Adolesc Psychiatry. 2011;20(5):241–252. doi: 10.1007/s00787-011-0168-2. [DOI] [PubMed] [Google Scholar]


