Abstract
Prognosis can no longer be relegated behind diagnosis and therapy in high-quality neurologic care. High-stakes decisions that patients (or their surrogates) make often rest upon perceptions and beliefs about prognosis, many of which are poorly informed. The new science of prognostication—the estimating and communication “what to expect”—is in its infancy and the evidence base to support “best practices” is lacking. We propose a framework for formulating a prediction and communicating “what to expect” with patients, families, and surrogates in the context of common neurologic illnesses. Because neurologic disease affects function as much as survival, we specifically address 2 important prognostic questions: “How long?” and “How well?” We provide a summary of prognostic information and highlight key points when tailoring a prognosis for common neurologic diseases. We discuss the challenges of managing prognostic uncertainty, balancing hope and realism, and ways to effectively engage surrogate decision-makers. We also describe what is known about the nocebo effects and the self-fulfilling prophecy when communicating prognoses. There is an urgent need to establish research and educational priorities to build a credible evidence base to support best practices, improve communication skills, and optimize decision-making. Confronting the challenges of prognosis is necessary to fulfill the promise of delivering high-quality, patient-centered care.
To diagnose and to treat have been the pillars of modern neurologic practice. However, prognostication—the process of estimating and communicating “what to expect” for an individual's disease course—is becoming increasingly important in neurologic practice.1 Neurologists frequently avoid prognostication for reasons that include clinician discomfort with uncertainty and “delivering bad news”; lack of training; acculturation to optimism; and fears of destroying hope.2–4 However, growing evidence finds that most patients and families wish to talk about prognosis with their doctor and are not hurt by such conversations. In fact, patients' perceptions of physician dishonesty or avoidance of prognosis hurts more than honest and compassionate conversations about prognoses.5
Prognosis is central to patient-centered care and a key task in successful shared decision-making, but clinicians historically are resistant to discussing prognosis.6,7 Even when it does occur, patient surveys and the wide variations in end-of-life treatment practices suggest that the process of shared decision-making—and possibly the ability to formulate and communicate a prediction—is inadequate.8 Guidelines exist for prognosis in general medical practice and palliative care, but none yet exist that are specific to neurology.9,10 Herein, we review the available evidence as it applies to prognostication in neurologic disease, recommend an approach to formulate a prediction and communicate “what to expect” for many common neurologic conditions, and address areas in need of further research and education.
TYPES OF PROGNOSTIC INFORMATION
In advanced illness, patients and families often have 2 types of prognosis questions: “How long?” and “How well?” Clinical priorities vary with life expectancy and these questions are highly interdependent, dynamic, and intensely personal. Patients and families differ in their preferences for the timing and amount of information; the relative focus on survival and quality-of-life prognoses; and on their personal approaches for dealing with uncertainty. Physicians also differ in their prognostication skills and bring clinical experiences that can bias both their estimation and communication or prognoses.11
“How long?”
Many neurologic diseases affect survival. Despite the challenges and barriers, patients or surrogates should be offered information on the potential survival impact of their disease. To allow for both well-informed life and medical choices, some have argued that patients 85 years or older or with a life expectancy of fewer than 10 years should have this information shared within the clinical encounter.12 Patient-centered care, however, requires awareness that some patients will prefer to defer such information to a later time or to a surrogate decision-maker. Predictions tend to be more accurate the closer one is to death (i.e., the “horizon effect”) and less accurate for physicians who have a longer and more established relationship with a patient. Data from oncology, palliative care, and neuro-intensive care consistently show that physicians tend to be overly optimistic in their survival prediction.13,14 Concerns have been raised in stroke neurology, however, about the possibility of overly pessimistic predictions if mortality/survival estimates are used from populations with mixed treatment intensities (e.g., patients with do-not-resuscitate [DNR] and non-DNR orders), leading to a “self-fulfilling prophecy.”15–17
“How well?”
Most neurologic diseases affect function more than survival. Important considerations are the pattern, type, and severity of impairments, as well as the probability of the outcomes getting worse or better and over what time period.18 Many patients and families seem to weigh prognoses about cognitive deficits to a greater degree than prognoses about other functional deficits when making decisions.19 When predicting long-term function, neurointensivists are more accurate at predicting “poor” outcomes than “good” outcomes.14 Defining “good” and “bad” based on the patient's values can often lead to more accurate and precise estimates and more personalized decision-making. Bringing balance to a conversation will often require attention to both good and bad outcomes so that physicians, patients, and surrogates can avoid the potential bias to overestimate the impact of disease on future quality of life (e.g.,“misimagining the unimaginable”).
SUGGESTED FRAMEWORK FOR PROGNOSTICATION
Formulating the prediction.
In formulating a prediction, we believe a structured and systematic approach using the best available evidence is preferable to relying solely on a physician's heuristic estimate of survival and function. Therefore, we propose the “Anticipating–Anchoring–Tailoring–De-biasing” approach to formulating a prediction.20,21
Anticipating.
Consider the types of prognostic information most likely needed during the encounter (i.e., “How long?,” “How well?,” or both). For patients closer to death, think through the potential and precise ways a patient may die, because many patients want to explore these paths and ways to address symptoms that may occur.
Anchoring.
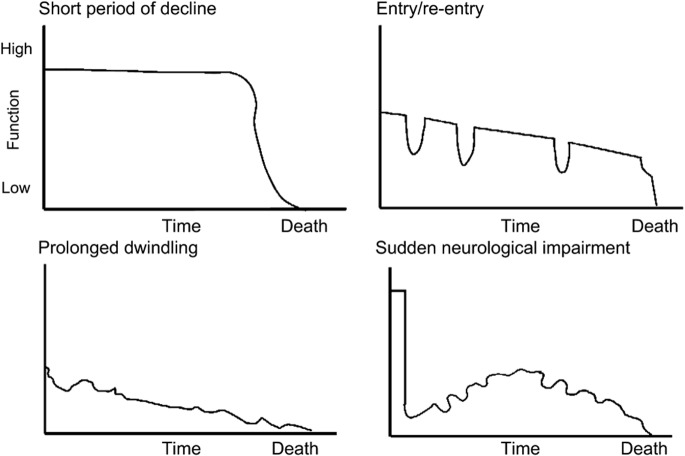
One approach to anchoring is to use age- and race-specific median and interquartile ranges using survival data from standard life tables (see appendix e-1 on the Neurology® Web site at www.neurology.org).22 Another approach is to anchor patients by considering their overall trajectory of illness.23 The 4 trajectories are 1) short period of decline, 2) entry/reentry, 3) prolonged dwindling, and 4) sudden neurologic impairment. Most neurologic diseases can be mapped to these 4 trajectories (figure 1), which provide a framework to assist providers and health care systems in anticipating the needs of patients and families with advancing illness.
Figure 1. Trajectories to death and disability by neurologic disease.
The period of evident, predictable decline before death trajectory is typical of cancer and amyotrophic lateral sclerosis. The chronic illness with entry/reentry is associated with organ failure and relapses as in multiple sclerosis and epilepsy. The prolonged dwindling trajectory is associated with dementia, frailty, and other neurodegenerative conditions (e.g., Parkinson disease). The sudden neurologic impairment trajectory represents a distinct group of neurologic emergencies, the majority of which are the subset of patients with stroke, hypoxic ischemic encephalopathy, and traumatic brain injury who present with severe neurologic symptoms. This figure was published in Andreoli and Carpenter's Cecil Essentials of Medicine.23 Copyright Elsevier 2010.
Tailoring.
Tailoring involves using the best available evidence from literature and the particulars of the patient, including signs, symptoms, comorbidities, protective factors (e.g., social support, community engagement), and the willingness of the patient to live. For each information source, assess the quality of the evidence and the applicability to the patient (e.g., similar in age, disease stage) and setting (e.g., outpatient, hospital-based, hospice enrollee). Seek out consultation from others with more or differing experiences if needed.
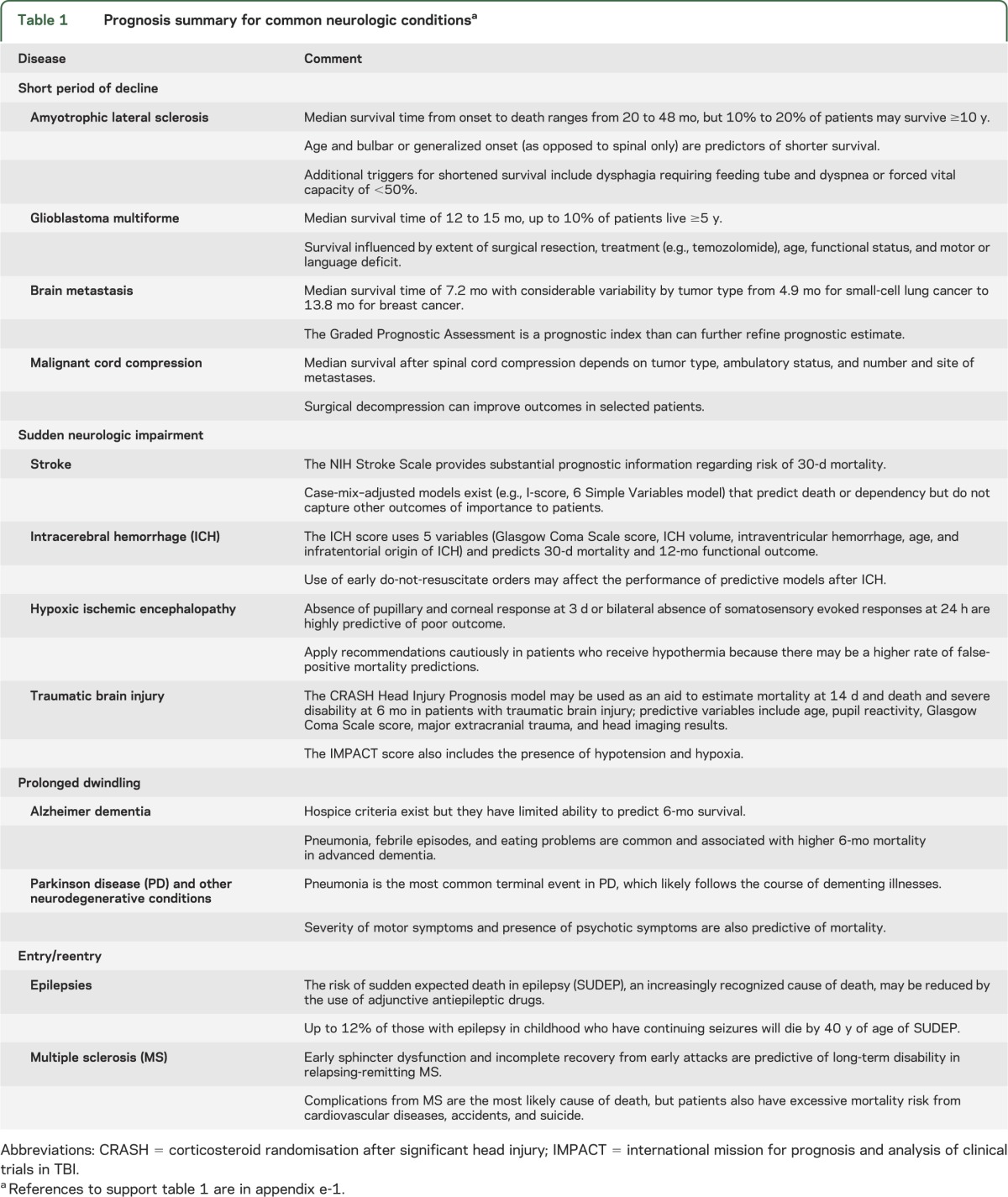
Table 1 shows a summary of the prognostic evidence for common neurologic diseases, and the references to support this table are found in appendix e-1. It is not meant to be a systematic review or all-inclusive. Here, we highlight several observations for tailoring a neurologic prognosis.
a. Build a case for the particular patient about the length of survival and the impairments that may affect physical and cognitive function. Think explicitly about the range of potential outcomes and the realistic exceptions. We suggest using median survival estimates and interquartile ranges, if available, considering patient-specific factors that may make survival longer or shorter (or outcomes better or worse) than the median.
b. Although many individual signs and symptoms correlate with survival, the strength of these correlations is rarely strong enough to rely on when prognosticating. The one possible exception is in patients with severe hypoxic ischemic encephalopathy after a cardiac arrest. In these patients, the absence of pupillary light or corneal reflexes on day 3 or absent cortical (N20) responses on somatosensory evoked potentials by day 1 to 3 uniformly predicts a poor prognosis defined as death or severe disability.24
c. Prognostic indices and Web-based prognostic tools are most developed in stroke, cancer, intensive care unit, traumatic brain injury, and palliative care/hospice populations.25–29 Even though these prognostic indices and rules can help tailor prognostic estimates, they were not designed for individualized decision-making. Therefore, they should be used with extreme caution. A recent systematic review of non–disease-based prognostic indices for older adults concluded significant limitations in the current evidence and ability to apply them to patients.30
d. Patients who are terminally ill regardless of the diagnosis have a convergence of symptoms as death becomes closer. Common factors known to be predictive of short-term survival (i.e., less than 3–6 months) include ambulatory status, performance status, nutritional intake, and mental status. Palliative care performance scales can be used to assist with prognosis in these populations.31 Eligibility criteria for hospice exist for noncancer diagnoses, including cerebrovascular disease and coma, amyotrophic lateral sclerosis, and dementia (see appendix e-2).32 Although not uniformly reliable, they can be useful in formulating estimates where prognosis is likely to be 6 months or less if the disease is allowed to run its natural course.
Table 1.
Prognosis summary for common neurologic conditionsa
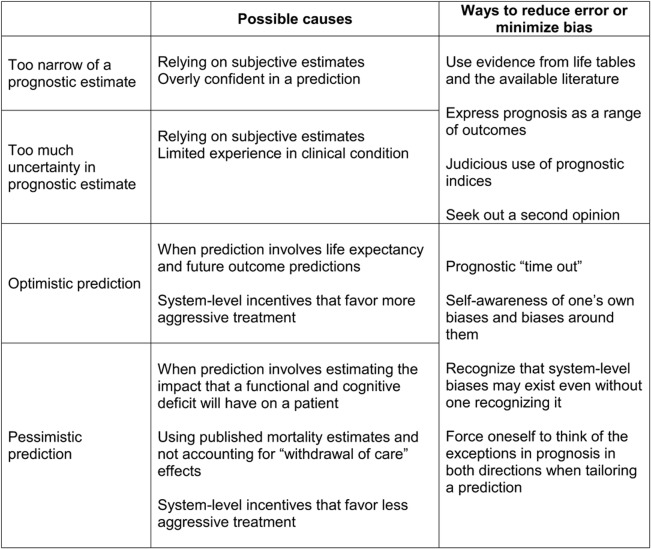
De-biasing.
De-biasing entails an explicit exercise to acknowledge one's own potential to be overly optimistic or pessimistic in one's prediction. This prognostic “time out” is to force a self-awareness of the personal, system-level, and emotional factors that may bias one's prediction, and the potential strategies to overcome these influences when communicating the information (figure 2).
Figure 2. Reducing error and de-biasing strategies when formulating and communicating prognosis.
Communicating “what to expect.”
Communicating what to expect occurs in the context of broader communication tasks of building rapport, discussing treatment options, eliciting patient preferences, dealing with conflict, and running family meetings.33 General principles of effective interpersonal communication between providers and patients/families (e.g., maintenance of eye contact, minimization of interruptions) are of key importance.34 To deliver the prognostic message, we apply the Ecological Model of Prognostic Conversations, which contributes to effective information-seeking, comprehension, and deliberation.35 The 4 elements of the communication strategy include engaging, informing, responding, and framing.
Engaging.
The key prognostic message should be coordinated across the care team to avoid confusion and providing the patient and family with mixed messages. Most patients and families want to know prognosis, but a sizeable minority (up to 25%) do not.6 For those patients who do want to know prognosis, most want some control over timing, amount of information, manner, or presentation, and whom they wish to be present during the discussion. For those patients who do not want to know or are ambivalent about knowing prognosis, assess and acknowledge the reasons underlying their concerns. If important decisions need to be made, explore creative solutions such as supplying limited information or designation of a health care proxy.
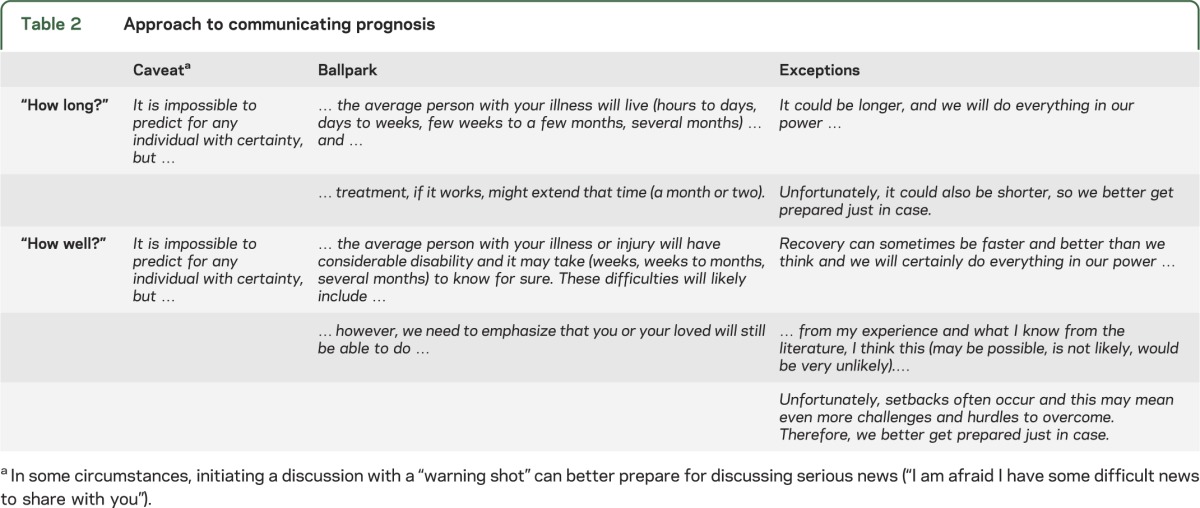
Informing.
Most patients want their physician to be direct but not too blunt, empathic, and willing to spend time on the topic. An example of how to inform patients and families of the prognostic message is the “caveat–ballpark–exceptions” format, which can be adapted for both the “How long?” and “How well?” frames (table 2). A “warning shot” (“I am afraid I have some difficult news to share with you”) may prepare patients and families if prognosis is unexpectedly serious. One approach is to bracket the prognostic estimate with ranges to convey realistic uncertainty, being sure to allow for exceptions in both optimistic and pessimistic directions. For survival-predominant prognoses (e.g., “How long?”), be mindful of overly optimistic prognoses, remembering to think of and convey the lower bound (e.g., “some may live longer, but others may unfortunately live shorter”). For outcome-predominant prognoses (e.g., “How well?”), be mindful of overly pessimistic predictions, remembering the power of adaptation (buffering) and the tendency to focus on impairment rather than remaining abilities (focalism). Presentation formats (qualitative, graphical displays, positive frame, negative frame, frequency, proportions, absolute, relative) strongly determine medical decisions as was recently shown for asymptomatic carotid stenosis.36 Little is known, however, about the optimal approach to information framing, although a recent review highlights 10 methods that have been empirically shown to improve patients' understanding of risk and benefit information.37
Table 2.
Approach to communicating prognosis
Responding.
Dealing with emotions can improve satisfaction, reduce anxiety, and lower risk for depression. Physicians often safeguard themselves from painful emotions while informing patients about prognosis. These emotional blocking behaviors (interrupting, monopolizing, bad news/good news spirals, softening, euphemistic vocabulary) result in the transfer of sparse factual prognostic information to patients.38 Some patients will provide an emotional warning for physicians to be careful in providing information or to pay particular attention to the patient's emotional state. Standard communication strategies to handle emotional cues include acknowledging the emotions being expressed, legitimizing the appropriateness and normalcy of reaction, empathizing (if you genuinely feel it), using silence effectively, pacing information, and periodically “checking in” to make sure the patient and family are still with you.
Framing.
Framing the prognostic discussion requires a higher-level appreciation of both the verbal and nonverbal stimuli that have meaning in delivering the prognostic message. The systematic and structured approach to this prognostic dialog with the patient and family requires a high degree of not only self-awareness of one's own bias and emotional state, but ongoing monitoring of the prognostic “tone” of the discussion. The self-correcting strategies of rebalancing that tone include knowing in real-time when it is best to manage emotions rather than continue to share prognostic information.39
SPECIAL CONSIDERATIONS
Managing uncertainty.
Uncertainty is the rule in neurologic prognosis, and most patients want physicians to acknowledge that prognosis is uncertain.6 This moves beyond how to manage one's own discomfort about being wrong, and into how to incorporate and communicate that angst into effective decision-making with patients. Dealing with uncertainty takes confidence, emotional energy, and time. Knowing when to confidently say “I don't know” takes humility but saying, “I don't know, but I will be there no matter what happens” takes humility and a commitment to a meaningful engagement—that commitment is what patients often want most.40
One approach to managing uncertainty is the effective use of time-limited trials: an agreement between clinicians and a patient/family to use certain medical therapies over a defined period to determine whether the patient improves or deteriorates according to agreed-on clinical outcomes.41 Decisions regarding future therapy (e.g., disease-directed vs shifting to palliation/comfort) are determined by the patient's clinical course. A time-limited trial allows opportunity for evaluation of trends in prognosis, as well as other aspects of goal setting, including patient reflection, family input, adaptation to a “new normal,” palliation of symptoms, recruiting community resources, and rehabilitation and functional improvement.
Balancing hope and realism.
Patients not only want their providers to be optimistic, but studies have shown that patients who are more optimistic have better long-term function and survive longer.42 The mechanisms for this beneficial effect are yet unknown but there may be evolutionary advantages for this disposition.43 As a result, each prognostic disclosure requires a balance of promoting optimistic outlooks (“let's focus on the positives,” “you can beat the odds”), but knowing when too much optimism may do harm (wasting resources, unnecessary suffering, unpreparedness). Setting the prognostic tone of the conversation to deliver information in a nondeceptive, reassuring way requires self-awareness of one's own biases and the emotional readiness of patients and families—no easy task.
A recommended approach to simultaneously manage and affirm both emotions is to use the phrase, “Hope for the best, prepare for the worst.”44 Using “I wish” statements can also simultaneously express empathy and the limits of available treatment options, as one steers the conversation away from cures or improbable improvements in outcomes, to the kind of hope that helps people adapt and find new meaning.
Nocebo effects and the self-fulfilling prophecy.
The opposite of optimism's positive effect is pessimism's potential negative effect or the nocebo (“I will harm”) effect.45 There is increasing evidence that a patient's pessimistic beliefs and expectations can result in worse outcomes. Such concerns may result in a tendency to not divulge prognostic information, for fear of demoralizing the patient and family. Although not studied extensively in neurology, there is evidence from oncology that patients receiving more prognostic information have higher rates of satisfaction, lower rates of depression, and no change in anxiety.46
There has been concern in neurologic disease, particularly in stroke, that physicians may be contributing to nocebo effects, and possibly self-fulfilling prophecies, given studies showing an association between DNR orders and a higher probability of a short-term mortality.15–17 As a result, the American Stroke Association guidelines for intracerebral hemorrhage advise that the “postponement of new DNR orders until at least the second full day of hospitalization is probably recommended.”47
Providers need to be aware that short-term mortality estimates from the literature (e.g., inpatient or 30-day stroke mortality) represent a heterogeneous mix of patients with varying levels of treatment intensities. As a result, an aggressive approach to stroke management would result in a mortality prediction lower than what is published. Therefore, one needs to tailor an individualized mortality prediction from the literature taking into account the treatment plan preferred by the patient (e.g., aggressive care, withdrawal of care). Given the importance of the physician's prediction of poor prognosis in decisions to withdraw care, a self-fulfilling prophecy may occur if the patient or surrogate is provided with a published mortality estimate without an adjustment or reductions in mortality from earlier deaths due to withdrawal or less-intense forms of treatment. Little information is yet known about the magnitude of this “withdrawal of treatment care” bias, but early estimates show it may be as high as 40% for short-term stroke mortality.48
Surrogate decision-makers.
Prognosticating in neurologic illness often involves discussions with surrogate decision-makers. As a result, skills are needed in the conduct of family meetings and conflict resolution.49 Relying on surrogate decision-makers increases uncertainty, because they accurately predict patient treatment preferences only two-thirds of the time, with the lowest accuracy in patients with stroke and dementia.50 However, surrogates understand that prognostic uncertainty is unavoidable, want prognostic estimates disclosed nonetheless, and believe that withholding prognostic information is an unacceptable way of maintaining hope.51 Physicians need to be aware that surrogates often register optimism when prognosis is poor, and use various sources of knowledge when estimating their loved one's prognosis, rarely (2% of the time) relying solely on the physician's estimate.52,53 Providers also need to be aware of the intense emotional burden felt by many surrogates and the negative effects this may have on decision-making, as well as strategies to mitigate them.54
RESEARCH PRIORITIES
There is an urgent need for more research on prognosis in advanced neurologic disease. More conceptual, qualitative, and quantitative work is needed on predictors of mortality and other outcomes of importance to patients. This will include a new language and approach to families on how best to communicate and discuss evidence of willful brain activation in patients with prolonged disorders of consciousness.55
Additional research is needed on best approaches for and the effects of novel interventions (e.g., decision aids, time-limited trials) on medical choices, patient outcomes, and congruence of treatment with patient preferences.56 Research in this area, although challenging and somewhat outside of the mold of classic biomedical research, is feasible and informative.7 More research is needed on measuring and optimizing the prognostic “tone” of conversations and ways to modulate the balance between hope and reality, optimism and pessimism, truth and harmless falsehoods, and placebos and nocebos. This should include ways to approach provider self-awareness and ways to de-bias prognostic estimates.
EDUCATION PRIORITIES
Despite its growing importance, there is little instruction in prognosis and more broadly in developing and improving effective patient-centered communication skills.57 Training opportunities, such as standardized patients, immediate feedback, and coaching, can be further incorporated into residency training programs and become part of continuing medical education offerings. A novel training program for oncologists called “Oncotalk” can be easily adapted to create neurology vignettes (e.g., “Neurotalk”).58 Various self-reflection activities such as mindfulness training may help providers become and stay more empathic as well as become more self-aware of the conscious and unconscious biases that may influence their approach to prognosis and communication with families.59
CONCLUSION
Just like growth charts early in life, we need more recognition and use of survival curves at the end of life. The new norm of medicine demands us to confront and discuss the limits of our profession with each other and with our patients and families. Addressing prognosis fully embodies the ultimate purpose of goal setting and achieving truly patient-centered care.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Michelle Washington for assistance in preparing the manuscript.
GLOSSARY
- DNR
do not resuscitate
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
R. Holloway: study concept and design, acquisition of data, analysis and interpretation, critical revision of the manuscript for important intellectual content, study supervision. R. Gramling and A. Kelly: study concept and design, acquisition of data, analysis and interpretation, critical revision of the manuscript for important intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
R. Holloway is a consultant for Milliman Guideline, Inc., and Associate Editor, Neurology Today®. R. Gramling and A. Kelly report no disclosures. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Gill TM. The central role of prognosis in clinical decision making. JAMA 2012;307:199–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christakis NA. Death Foretold: Prophecy and Prognosis in Medical Care. Chicago: University of Chicago Press; 1999 [Google Scholar]
- 3.Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med 2001;134:1096–1105 [DOI] [PubMed] [Google Scholar]
- 4.Christakis NA, Iwashyna TJ. Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med 1998;158:2389–2395 [DOI] [PubMed] [Google Scholar]
- 5.Hancock K, Clayton JM, Parker SM, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med 2007;21:507–517 [DOI] [PubMed] [Google Scholar]
- 6.Ahalt C, Walter LC, Yourman L, Eng C, Perez-Stable EJ, Smith AK. "Knowing is better": preferences of diverse older adults for discussing prognosis. J Gen Intern Med 2012;27:568–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.SUPPORT Prinicipal Investigators A controlled trial to improve care for seriously ill hospitalized patients. JAMA 1995;274:1591–1598 [PubMed] [Google Scholar]
- 8.Schenker Y, Fernandez A, Sudore R, Schillinger D. Interventions to improve patient comprehension in informed consent for medical and surgical procedures: a systematic review. Med Decis Making 2011;31:151–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glare PA, Sinclair CT. Palliative medicine review: prognostication. J Palliat Med 2008;11:84–103 [DOI] [PubMed] [Google Scholar]
- 10.Clayton JM, Hancock KM, Butow PN, et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust 2007;186(12 suppl):S77, S79, S83–108 [DOI] [PubMed] [Google Scholar]
- 11.Vickrey BG, Samuels MA, Ropper AH. How neurologists think: a cognitive psychology perspective on missed diagnoses. Ann Neurol 2010;67:425–433 [DOI] [PubMed] [Google Scholar]
- 12.Smith AK, Williams BA, Lo B. Discussing overall prognosis with the very elderly. N Engl J Med 2011;365:2149–2151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ 2003;327:195–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finley Caulfield A, Gabler L, Lansberg MG, et al. Outcome prediction in mechanically ventilated neurologic patients by junior neurointensivists. Neurology 2010;74:1096–1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hemphill JC, III, Newman J, Zhao S, Johnston SC. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. Stroke 2004;35:1130–1134 [DOI] [PubMed] [Google Scholar]
- 16.Creutzfeldt CJ, Becker KJ, Weinstein JR, et al. Do-not-attempt-resuscitation orders and prognostic models for intraparenchymal hemorrhage. Crit Care Med 2011;39:158–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zahuranec DB, Morgenstern LB, Sanchez BN, Resnicow K, White DB, Hemphill JC., III Do-not-resuscitate orders and predictive models after intracerebral hemorrhage. Neurology 2010;75:626–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coppola KM, Bookwala J, Ditto PH, Lockhart LK, Danks JH, Smucker WD. Elderly adults' preferences for life-sustaining treatments: the role of impairment, prognosis, and pain. Death Stud 1999;23:617–634 [DOI] [PubMed] [Google Scholar]
- 19.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002;346:1061–1066 [DOI] [PubMed] [Google Scholar]
- 20.Carroll T, Epstein RM, Gramling R. What is a useful strategy for estimating survival in palliative care settings for persons with advanced cancer?. In: Goldstein NE, Morrison RS, editors. Evidence-Based Practice of Palliative Medicine. Philadelphia: Elsevier; 2013:235–240 [Google Scholar]
- 21.Carroll T, Epstein RM, Gramling R. What is a useful strategy for estimating survival for persons with advanced non–cancer-related illness in palliative care settings?. In: Goldstein NE, Morrison RS, editors. Evidence-Based Practice of Palliative Medicine. Philadelphia: Elsevier; 2013:241–243 [Google Scholar]
- 22.Arias E. United States life tables, 2007. Natl Vital Stat Rep 2011;59:1–60 [PubMed] [Google Scholar]
- 23.Holloway RG, Quill TE. Palliative care. In: Andreoli TE, editor. Andreoli and Carpenter's Cecil Essentials of Medicine. Philadelphia: Elsevier; 2010:1210–1217 [Google Scholar]
- 24.Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S; Quality Standards Subcommittee of the American Academy of Neurology Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review). Neurology 2006;67:203–210 [DOI] [PubMed] [Google Scholar]
- 25.Teale EA, Forster A, Munyombwe T, Young JB. A systematic review of case-mix adjustment models for stroke. Clin Rehabil 2012;26:771–786 [DOI] [PubMed] [Google Scholar]
- 26.The MRC CRASH Trial Collaborators Head injury prognosis: crash. Available at: http://www.crash2.lshtm.ac.uk/Risk%20calculator/index.html. Accessed January 29, 2012
- 27.University of Victoria Prognostat. Available at: http://htg.his.uvic.ca/tools/PrognosticTools/PalliativePerformanceScale/Prognostat/index.php. Accessed January 29, 2012
- 28.Washington University in Saint Louis Prognostigram. Available at: http://oto2.wustl.edu/clinepi/prog.html. Accessed January 29, 2012
- 29.Lee S, Smith A, Widera E, Yourman L, Schonberg M, Ahalt C. ePrognosis: estimating prognosis in elders. Available at: http://www.eprognosis.org/. Accessed January 29, 2012
- 30.Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA 2012;307:182–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lau F, Maida V, Downing M, Lesperance M, Karlson N, Kuziemsky C. Use of the Palliative Performance Scale (PPS) for end-of-life prognostication in a palliative medicine consultation service. J Pain Symptom Manage 2009;37:965–972 [DOI] [PubMed] [Google Scholar]
- 32.National Hospice Organization; Medical Guidelines Task Force, et al Medical Guidelines for Determining Prognosis in Selected Non-Cancer Diseases. Arlington: The National Hospice Organization; 1996 [DOI] [PubMed] [Google Scholar]
- 33.Barclay JS, Blackhall LJ, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliat Med 2007;10:958–977 [DOI] [PubMed] [Google Scholar]
- 34.Back A, Arnold R, Tulsky J. Mastering Communication with Seriously Ill Patients: Balancing Honesty with Empathy and Hope. New York: Cambridge University Press; 2009 [Google Scholar]
- 35.Gramling R, Carroll T, Epstein R. What is known about prognostication in advanced illness? In: Goldstein NE, Morrison RS, editors. Evidence-Based Practice of Palliative Medicine. Philadelphia: Elsevier; 2012:228–234. [Google Scholar]
- 36.Silver B, Zaman IF, Ashraf K, et al. A randomized trial of decision-making in asymptomatic carotid stenosis. Neurology 2012;78:315–321 [DOI] [PubMed] [Google Scholar]
- 37.Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst 2011;103:1436–1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graugaard PK, Rogg L, Eide H, Uhlig T, Loge JH. Ways of providing the patient with a prognosis: a terminology of employed strategies based on qualitative data. Patient Educ Couns 2011;83:80–86 [DOI] [PubMed] [Google Scholar]
- 39.Smith A, Juraskova I, Butow P, et al. Sharing vs. caring—the relative impact of sharing decisions versus managing emotions on patient outcomes. Patient Educ Couns 2011;82:233–239 [DOI] [PubMed] [Google Scholar]
- 40.Srivastava R. Dealing with uncertainty in a time of plenty. N Engl J Med 2011;365:2252–2253 [DOI] [PubMed] [Google Scholar]
- 41.Quill TE, Holloway R. Time-limited trials near the end of life. JAMA 2011;306:1483–1484 [DOI] [PubMed] [Google Scholar]
- 42.Barefoot JC, Brummett BH, Williams RB, et al. Recovery expectations and long-term prognosis of patients with coronary heart disease. Arch Intern Med 2011;171:929–935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson DD, Fowler JH. The evolution of overconfidence. Nature 2011;477:317–320 [DOI] [PubMed] [Google Scholar]
- 44.Back AL, Arnold RM, Quill TE. Hope for the best, and prepare for the worst. Ann Intern Med 2003;138:439–443 [DOI] [PubMed] [Google Scholar]
- 45.Colloca L, Finniss D. Nocebo effects, patient-clinician communication, and therapeutic outcomes. JAMA 2012;307:567–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hagerty RG, Butow PN, Ellis PM, Dimitry S, Tattersall MH. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol 2005;16:1005–1053 [DOI] [PubMed] [Google Scholar]
- 47.Morgenstern LB, Hemphill JC, III, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2010;41:2108–2129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kelly AG, Hoskins KD, Holloway RG. Early stroke mortality, patient preferences and the withdrawal of care bias. Neurology 2012;79:941–944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hudson P, Quinn K, O'Hanlon B, Aranda S. Family meetings in palliative care: multidisciplinary clinical practice guidelines. BMC Palliat Care 2008;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med 2006;166:493–497 [DOI] [PubMed] [Google Scholar]
- 51.Evans LR, Boyd EA, Malvar G, et al. Surrogate decision-makers' perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med 2009;179:48–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boyd EA, Lo B, Evans LR, et al. "It's not just what the doctor tells me": factors that influence surrogate decision-makers' perceptions of prognosis. Crit Care Med 2010;38:1270–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers' interpretation of prognostic information: a mixed-methods study. Ann Intern Med 2012;156:360–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med 2011;154:336–346 [DOI] [PubMed] [Google Scholar]
- 55.Cruse D, Chennu S, Chatelle C, et al. Bedside detection of awareness in the vegetative state: a cohort study. Lancet 2011;378:2088–2094 [DOI] [PubMed] [Google Scholar]
- 56.Fowler FJ, Jr, Levin CA, Sepucha KR. Informing and involving patients to improve the quality of medical decisions. Health Aff (Millwood) 2011;30:699–706 [DOI] [PubMed] [Google Scholar]
- 57.Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood) 2010;29:1310–1318 [DOI] [PubMed] [Google Scholar]
- 58.University of Washington Oncotalk. Available at: http://depts.washington.edu/oncotalk/. Accessed January 6, 2013
- 59.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302:1284–1293 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.