Abstract
One of the most commonly used local anesthetic techniques in dentistry is the Fischer’s technique for the inferior alveolar nerve block. Incidentally this technique also suffers the maximum failure rate of approximately 35–45%. We studied a method of inferior alveolar nerve block by injecting a local anesthetic solution into the pterygomandibular space by arching and changing the approach angle of the conventional technique and estimated its efficacy. The needle after the initial insertion is arched and inserted in a manner that it approaches the medial surface of the ramus at an angle almost perpendicular to it. The technique was applied to 100 patients for mandibular molar extraction and the anesthetic effects were assessed. A success rate of 98% was obtained.
Keywords: Inferior alveolar nerve block, Failure rate, Arched needle
Introduction
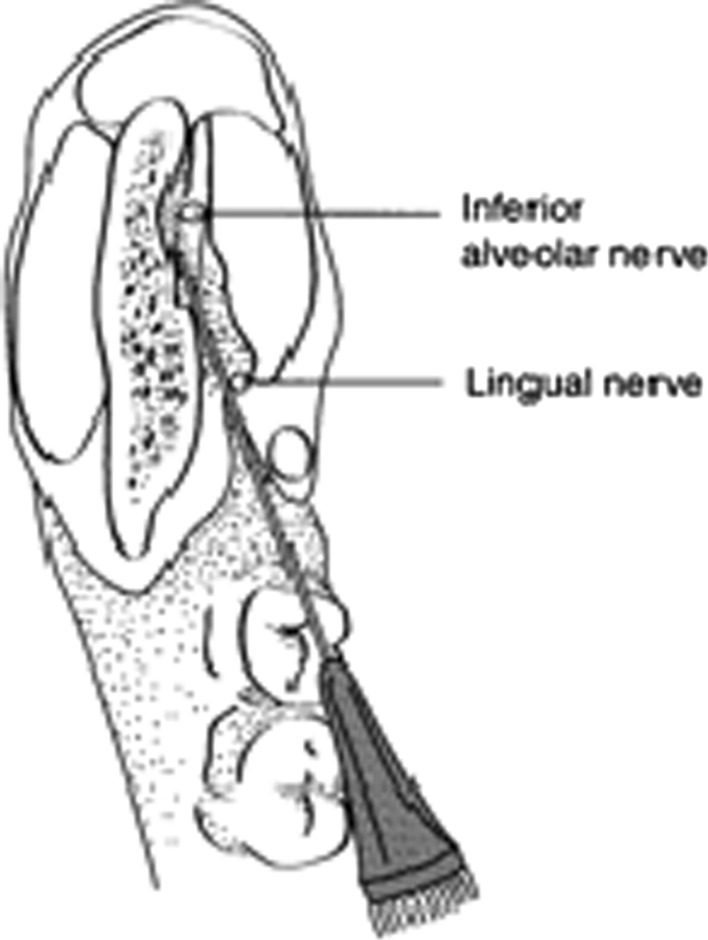
The most commonly practiced inferior alveolar nerve block is the Fischer’s technique [1, 2] (Fig. 1). The success of inferior alveolar nerve block largely depends on deposition of the anesthetic solution in the correct area i.e. in close proximity to the nerve. However, the conventional technique is reported to have been associated with risks and complications such as neural or vascular injury, intravascular injection and failure to achieve adequate anesthesia. Improper technique was deemed to be one of the major factors contributing to the failure of a desired result which has been reported as high as thirty-five to forty-five percent [2–4] In our study, we altered the insertion angle of the needle by arching it to achieve a near perpendicular angle with the ramus, resulting in a more accurate deposition of the anesthetic solution thus lowering the incidence of failure to achieve desired anesthesia.
Fig. 1.
Conventional inferior alveolar nerve block
Aim
The aim of the study was to assess the efficacy of the arched needle technique while administering an inferior alveolar nerve block.
Materials and Methods
The prospective analytical study was carried out at the Division of Oral & Maxillofacial Surgery, Dental Centre, INHS Kalyani, Eastern Naval Command, Vishakhapatnam, (AP) India from Jan 2009 to Jan 2010. Patients were randomly selected from those reporting to the OPD of Division of Oral & Maxillofacial Surgery, Dental Centre, INHS Kalyani, Vishakhapatnam, (AP) India with a complaint of pain in the lower third molar region. The selection criteria included those patients who were clinically and or radiologically diagnosed with symptomatic impacted lower third molar teeth. However patients requiring other procedures i.e. RCTs or extraction of teeth other than impacted teeth were excluded. Also the patients with bleeding disorders and those on anticoagulants and antiplatelet drugs were excluded. The study group includes 63 males and 47 females in an age range of 26 to 61 years (mean 32 years). In 58 patients the left side and in 42 patients the right side was involved.
Thorough preoperative assessment including mouth opening, cheek thickness, periapical pathology, pericoronitis apart from the hematological and radiological assessment for the grade/anticipated difficulty of surgical extraction was made. The patient was asked to rinse with a 0.2% chlorhexidine mouth wash. The dental chair was placed at a comfortable angle of about 30 degrees. The operator (right handed) was seated on the operating stool at 8 o’clock position for the right side and 11 o’clock for the left side nerve block. In all cases a side loading stainless steel aspirating syringe with a 2 cc cartridge containing 2% lignocaine with 1:80,000 adrenaline at room temperature with a 27 gauge 25 mm long (Septojet) needle was used. As per the conventional technique the standard landmarks were palpated and the index finger or the thumb placed to determine the level and approximate location of incretion of the needle. The needle was then inserted from the same side a little posterior to that in conventional technique and parallel to the mandibular occlusal plane to a depth of 4 to 5 mm, following which using the embedded tip as pivot the uninserted portion of the needle was arched posteromedially which changed the angle of approach of the needle tip from acute to almost perpendicular to the medial surface of the ramus. The needle was further inserted maintaining the arch till bone was contacted on the medial surface of the ramus. The needle was then withdrawn a bit, aspirated and when found correct 1.5 cc of anesthetic solution was deposited. No special maneuver was use to anesthetize the lingual nerve. The needle was then withdrawn and the remainder 0.5 cc of solution was used to administer the long buccal nerve block conventionally. The anesthetic effect was found to be exactly mimicking the conventional technique which was subjectively assessed by verifying tingling and numbness on the lower lip and tongue on the injected side and objectively assessed by noting the pain/discomfort during dental procedure. In both the techniques the areas anesthetized and the depth of anesthesia was found to be similar.
Results
In ninety-eight percent cases the desired anesthetic effect was achieved within three to five minutes of the administration of the drug. In two cases, both females, the depth of anesthesia was found to be inadequate and a repeat administration was done (Table 1).
Table 1.
Complications
| S. No | Problem areas | Number of cases | Remedial measures | Result |
|---|---|---|---|---|
| 1. | Incorrect needle position | 05 | Needle withdrawn and reinserted | Desired anesthesia achieved |
| 2. | Aspiration of blood | 04 | Needle withdrawn a little, direction changed, reinserted and same solution injected. | Desired anesthesia achieved |
| 3. | Inadequate depth of anesthesia | 02 | Repeat administration using the same technique | Desired anesthesia achieved |
In five cases the needle had to be withdrawn and reinsert as it was felt that the needle contacted the bone too early and was deemed to be incorrectly placed, however on reinsertion and subsequent injection the desired anesthetic effect was achieved (Table 1).
In four cases there was minor aspiration of blood. The needle was withdrawn aspiration rechecked and same solution was injected (Table 1).
Discussion
Successful painless reversible anesthesia is the single most important factor on which the modern day out patient clinical dental practice relies. Interestingly if learnt correctly based on a clear understanding of anatomy, physiology and pharmacology, the techniques are not very difficult to master. However in difficult cases i.e. restricted mouth opening, inflammation, apprehension etc. the results may be suboptimal even in the best of hands, needless to overemphasize the importance of good training and practice. Many techniques have been advocated for the inferior alveolar nerve block; however the Fischer’s technique seems to be the one which is most widely practiced. Unfortunately this technique is marred with a failure rate of approximately forty-five percent [3]. This may be due to the fact that the needle on insertion in the tissue approaches the medial surface of the ramus at an acute angle. At this angle there is a possibility that either the needle contacts the bone too far posteriorly, or may even miss it completely. This would lead to the anesthetic solution being deposited incorrectly resulting in a suboptimal result and also endangering complications like transient facial paralysis [5].
The arched needle technique for inferior alveolar nerve block as advocated by us is an antithesis to conventional teaching. Contemporary safe practices advocate that the needle should not be prebent or curved once in the tissues to avoid needle breakage and tissue tear [6]. Although needle breakage is a remote possibility, it is likely to happen with very thin bore needles [6]. In our study, fine 27 gauge needles were used. Prior to being used clinically, these needles were in vitro tested for breakage by bending them free hand (Figs. 2, 3) and were found to be safe. Tissue tear secondary to change in direction of the advancing needle tip is probably an over stated phenomenon, again possibly more significant with large bore and barbed needles [7]. Also the fact that needle deflection has been successfully utilized in techniques like bidirectional rotation [8] goes on to prove that midcourse path correction of the advancing needle is safe and inconsequential in terms of tissue damage.
Fig. 2.
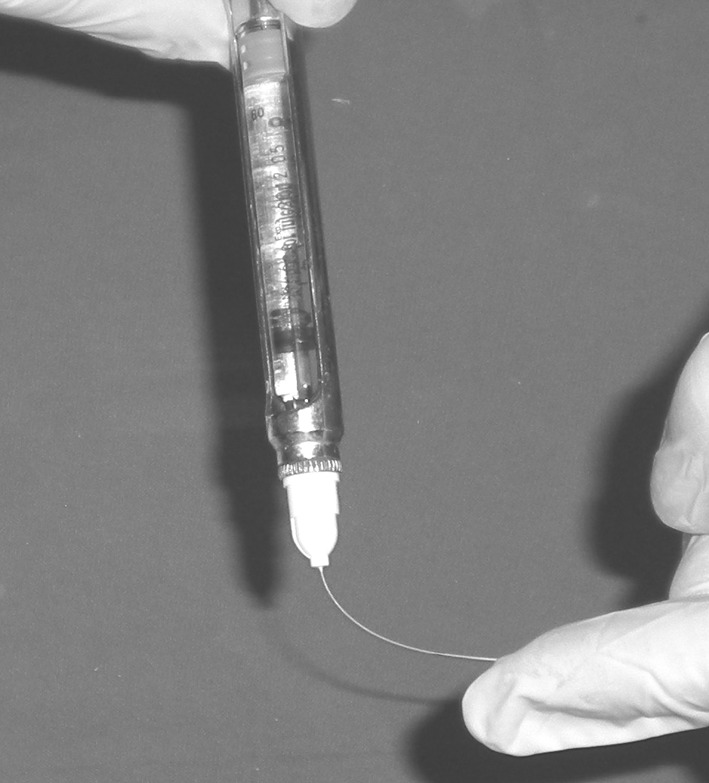
In vitro assessment of arching of the needle fixed on a syringe
Fig. 3.
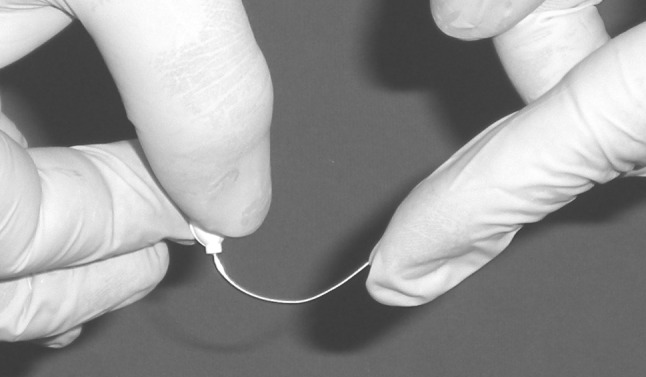
In vitro assessment of arching of the needle
In the arched needle technique the flexibility of the fine bore needle is utilized to change the approach angle of the needle tip (Fig. 4). Inserted at an acute angle the subsequent arching changes the path and the needle approaches the medial surface of the ramus almost perpendicularly, which is otherwise impossible to achieve with an unarched or unbent needle.
Fig. 4.

Administration of inferior alveolar nerve block using the arched needle technique
Conclusion
With a success rate of ninety-eight percent this technique may be utilized effectively in routine clinical practice especially in cases where mouth opening is limited, however it is equipment specific and may not be meant for inexperienced operators.
After completion of this study the authors have successfully used this technique on more than ten thousand patients for all procedures requiring mandibular anesthesia.
References
- 1.Malamed SF (1997) Techniques of mandibular anesthesia. In: Handbook of local anesthesia, 4th edn. Harcourt Brace, Noida, pp 228–234
- 2.Johnson TM, Badovinac R, Shaefer J. Teaching alternatives to the standard inferior alveolar nerve block in dental education: outcomes in clinical practice. J Dent Educ. 2007;71(9):1145–1152. [PubMed] [Google Scholar]
- 3.Potocnik I, Bajrović F. Failure of inferior alveolar nerve block in endodontics. Dent Traumatol. 1999;15(6):247–251. doi: 10.1111/j.1600-9657.1999.tb00782.x. [DOI] [PubMed] [Google Scholar]
- 4.Madan GA, Madan SG, Madan AD. Failure of inferior alveolar nerve block: exploring the alternatives. J Am Dent Assoc. 2002;133(7):843–846. doi: 10.14219/jada.archive.2002.0298. [DOI] [PubMed] [Google Scholar]
- 5.Parsons-Smith G, Roberts JM (1970) Facial paralysis after local dental anaesthesia. Br Med J 4(5737):745–746 [DOI] [PMC free article] [PubMed]
- 6.Rifkind JB. Management of a broken needle in the pterygomandibular space following a vazirani-akinosi block: case report. J Can Dent Assoc. 2011;77:b64. [PubMed] [Google Scholar]
- 7.Stacy GC. Barbed needle and inexplicable paresthesias and trismus after dental regional anesthesia. Oral Surg Oral Med Oral Pathol. 1994;77(6):585–588. doi: 10.1016/0030-4220(94)90315-8. [DOI] [PubMed] [Google Scholar]
- 8.Hochman MN, Friedman MJ. An in vitro study of needle force penetration comparing a standard linear insertion to the new bidirectional rotation insertion technique. Quintessence Int. 2001;32(10):789–796. [PubMed] [Google Scholar]