Abstract
Introduction
Trigeminal neuralgia (TN) often called as “Tic douloureux” is a syndrome characterized by paroxysmal facial pain, is one of the most painful and debilitating craniofacial pain disorders. The controversy regarding the etiology and treatment of TN still exists.
Objective
To evaluate the effectiveness of percutaneous radiofrequency rhizotomy (PRR) for TN, after failure of pharmacological management.
Method
A nonrandomized, non comparative, descriptive, in vivo study of 15 patients with TN of maxillary and mandibular divisions of trigeminal nerve and patients with pain refractory to pharmacological management were done. It was performed as an O.P.D procedure. A routine follow up was done in all cases for 1 year.
Results
In a total of 15 patients, 8 female and 7 male patients were enrolled for the study. Early pain relief (immediately, postoperatively to 6 month) classified as excellent or good (successful), occurred in 12 of 15 patients (80 %). Fair or poor pain relief (unsuccessful) occurred in three patients (20 %).There was no mortalities and no major morbidity.
Summary
It was found that surgical treatment with PRR is a safe and effective way to manage patients with TN in whom pharmacologic therapy is either ineffective or not tolerated, with low side effects which are well tolerated.
Keywords: Percutaneous, Rhizotomy, Trigeminal neuralgia
Introduction
Trigeminal neuralgia (TN) often called as “Tic douloureux” is a syndrome characterized by paroxysmal facial pain, is one of the most painful and debilitating craniofacial pain disorders. It usually begins as a relapsing disease with a pain free intervals that may last months or years, characterized by paroxysms of severe, lancinating, electric shock like bouts of pain. These pain free intervals however grow shorter and eventually disappear. The incidence is reported to be four per 1,000,000 population and with a predominance in women, and in unilateral involvement, has tactile trigger areas, does not produce a neurosensory or motor deficit, and is restricted to the distribution of the trigeminal nerve [1].
The controversy regarding the etiology and treatment of TN still exists. The first line of treatment is usually pharmacological. Carbamazepine is the usual drug of choice and it provides significant relief of symptoms. Unfortunately, the relief provided by Carbamazepine or other drugs may decrease over time, and side effects may necessitate discontinuation of the medication. About half the patients eventually require alternative procedures for pain relief [3].
The rationale of surgical therapy and injection of gasserian ganglion is to interrupt the peripheral stimuli from reaching the central nervous system [4]. As Onofrio [8] observes “each procedure has its advocates, but the very multiplicity of choices indicates that none is totally satisfactory”. But out of the various surgical procedures percutaneous radiofrequency rhizotomy (PRR) is a well established treatment modality. The present study is to evaluate the effectiveness of PRR for TN, after failure of pharmacological management.
Aim
The present study was carried out to evaluate the effectiveness of PRR for TN, after failure of pharmacological management.
Objectives
To assess the efficacy of PRR as one of the treatment modalities in TN.
The feasibility of PRR as a routine out patient procedure in TN.
Methodology
The study conducted was a nonrandomized, non comparative, descriptive, in vivo study and was conducted on patients with TN who reported to the department of Oral and Maxillofacial Surgery, V. S. Dental College and Hospital, Bangalore. The patients were taken to Department of Neurosurgery, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore for treatment.
The ethical committee clearance was obtained to conduct the present study. The patients were selected based on the following criteria:
Patients with TN of maxillary and mandibular divisions of trigeminal nerve and patients with pain refractory to pharmacological management were included in the study.
Patients who respond to pharmacological management and patients with facial pain other than due to TN were excluded from the study.
Methods
A detailed history was ascertained, Routine blood investigations were done pre operatively in all patients. TC, DC, ESR, RBS, blood urea, serum creatinine, CT, BT. Panoramic radiograph (Fig. 1) and CT/MRI (Figs. 2, 3) were also obtained.
Fig. 1.

OPG
Fig. 2.

CT Scan picture
Fig. 3.
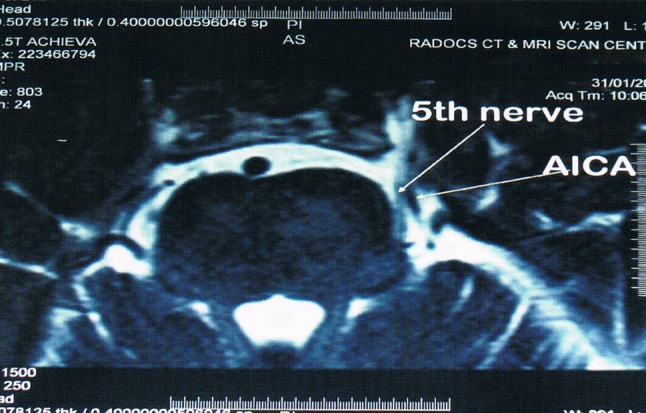
MRI picture
Materials for Rf Lesioning
A 100-mm length, 20-gauge cannula with a stylet (Tew’s kit; Radionics) (Fig. 4) and radionic machine (Fig. 5) used to generate radiofrequency lesions.
Fig. 4.

Tew’s kit
Fig. 5.
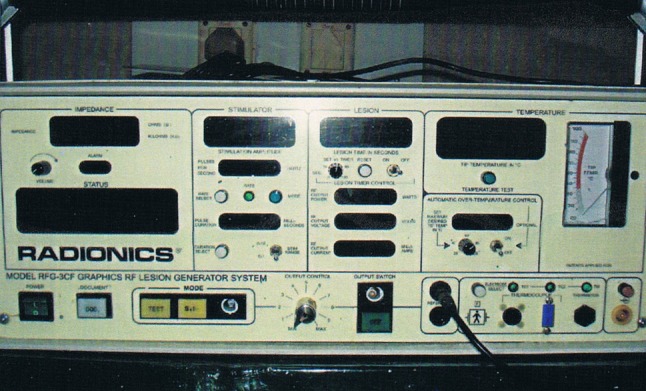
Radionic machine
Surgical Protocol for Radio Frequency Lesion
It was performed as an O.P.D procedure. Patients were advised to come to operation theatre on empty stomach on the day of procedure. The procedure was explained to them before starting it.
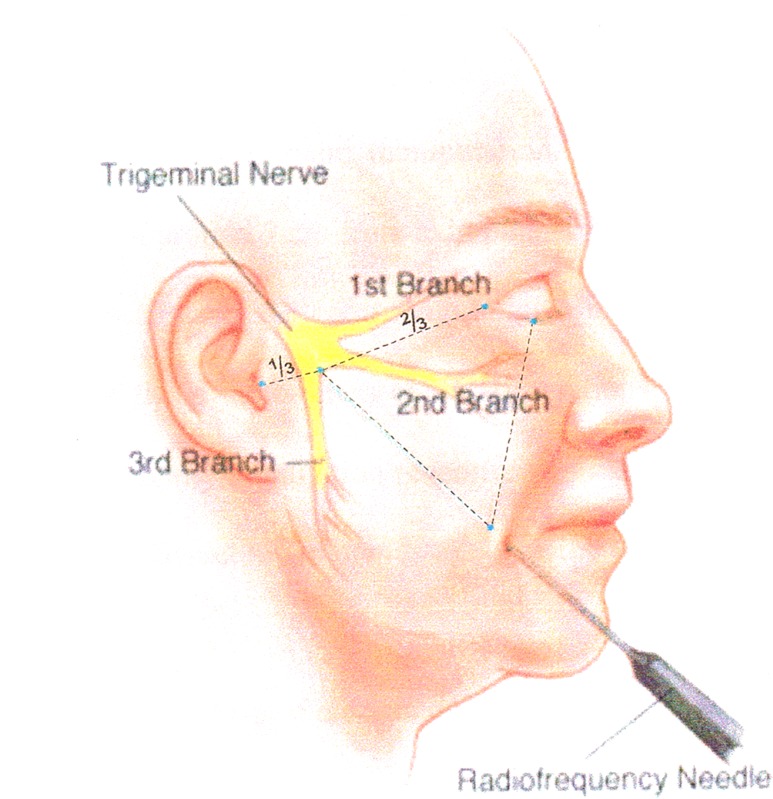
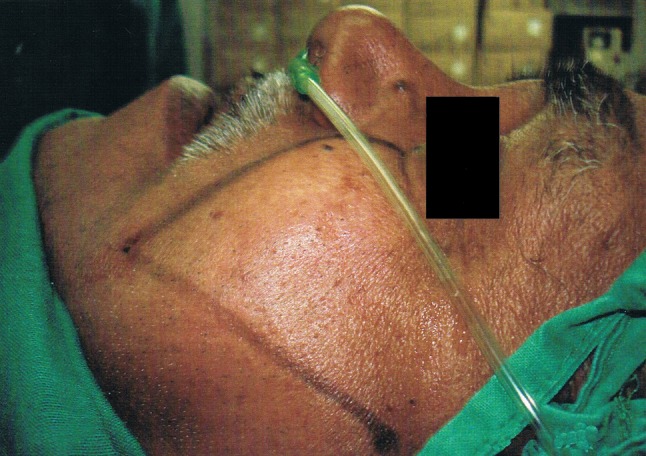
Procedure (Fig. 6)
Fig. 6.
RF technique through foramen ovale
The patient was made to lie in supine position on the table. Hartel’s markings were drawn over the face with marking pencil (Fig. 7). The point of entry of the needle was usually 3 cm lateral to the angle of mouth (Fig. 8). Two other points are (1) medial margin of pupil (2) a point 2.5 cm anterior to tragus on the Zygomatic arch to serve as planes for diverting needle to foramen ovale. Minimal alterations in position of neck such as flexion, extension are needed during the procedure to facilitate the entry of needle into foramen ovale. The patient usually winces or complains of pain referred to ear when the needle is in foramen ovale. In majority of cases entry into foramen ovale is easy in few cases where entry was difficult the attempt was repeated. In all cases the successful entry into foramen ovale was achieved. cerebro spinal fluid (CSF) was obtained in most of the cases and in such cases cannula was withdrawn till the CSF flow stopped.
Fig. 7.
Hartel’s markings
Fig. 8.

Point of entry of the needle
Stimulation at 50 Hz, 0.1–0.3 V was used to identify the nerve division in contact with the electrode tip, while enlisting the patient’s, subjective report of sensation in response to stimulation. A preliminary lesion was made by heating the electrode tip with radiofrequency current to 70 °C and maintaining it for 70 s. After each thermal lesioning, the patient was awakened and sensory stimulation testing was done. Depending on the results of testing, additional thermal lesioning if required was performed. To achieve effective pain relief and preservation of tactile functional sensation, the goal of thermal lesioning was to produce hypoalgesia and not anesthesia. Once that was achieved the procedure was completed.
The lesions were repeated until there was mild hypoalgesia in the involved division and when no pain could be triggered by stimulating the trigger zones.
At the end of procedure the patients were examined for loss of facial sensation, corneal anesthesia and masseter muscle weakness. They were kept in the ward for few hours and then discharged home and were prescribed analgesics for a day to treat the pain due to the procedure and Carbamazepine dose was tapered gradually before stopping the medication.
Follow up (Table 1)
Table 1.
Follow Up
| Results | Description |
|---|---|
| Excellent | No neuralgic pain, dysesthesia, or troublesome paresthesia |
| Good | No neuralgic pain, minor dysesthesia/paresthesia |
| Fair | No neuralgic pain, moderate dysesthesia/paresthesia |
| Poor | No neuralgic pain, major dysesthesia/paresthesia |
| Failure | Immediate |
A routine follow up was done in all cases. All patients were followed up, at 1 day, l week, 1 month, 6 months, 1 year. They were questioned about, and examined for facial hypoalgesia, dysesthesia, side effects, and complications. All patients were asked to give a satisfaction rating for the management of their pain after radiofrequency thermal rhizotomy (RTR) using the criteria: excellent, good, fair, poor and failure. Excellent or good results were considered successful, with no tic pain and no or only minor dysesthesia. Fair and poor results, with some neuralgic pain and moderate to major dysesthesia were considered unsuccessful. Patients with recurrence of pain were considered for reoperation.
Results
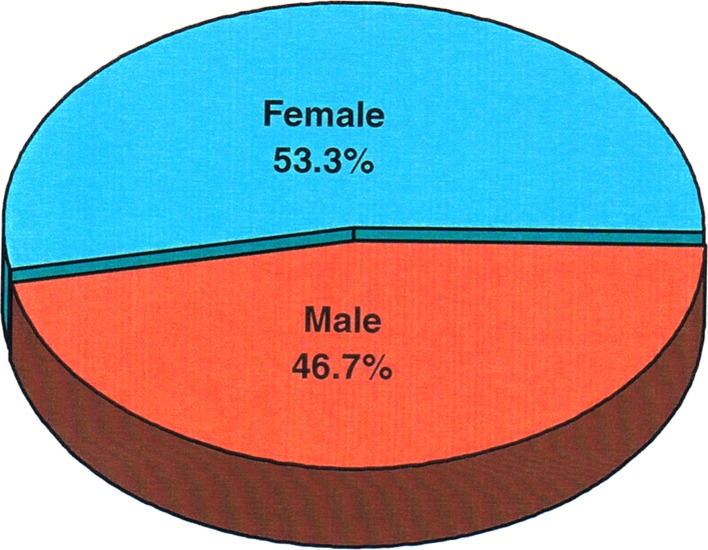
In the present study age distribution of patients studied and age incidence varied from 25 to 70 years. The maximum number of patients belonged to the age group of 51–60 years. In a total of 15 patients, eight female and seven male patients were enrolled for the study (Fig. 9).
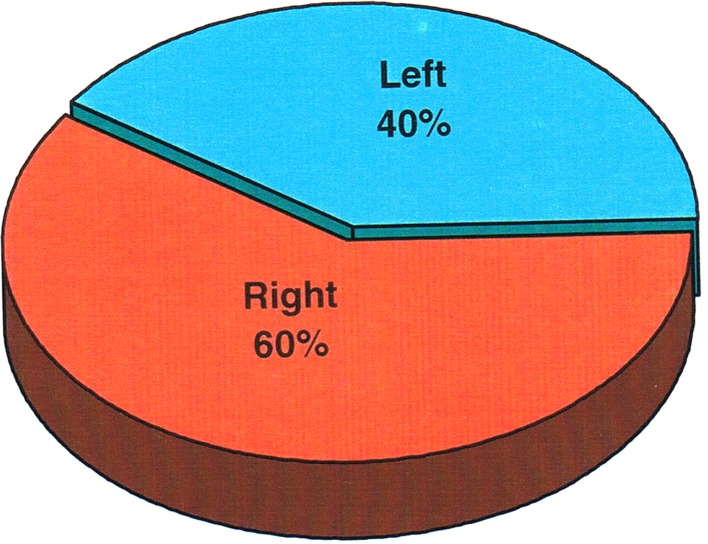
Side of the face involved; nine patients presented with lesion in right side and six patients presented with lesion in left side and lesion in right side found to be affected more frequent (60 %) (Fig. 10).
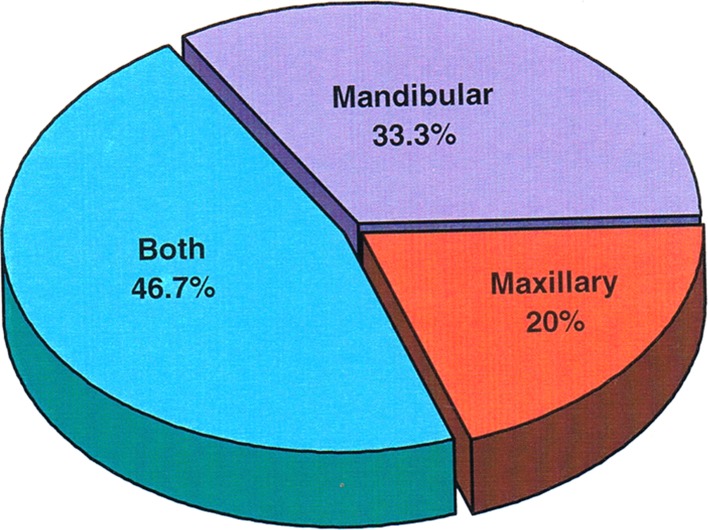
Division of the trigeminal nerve involved: we found that maxillary nerve was involved in three cases and mandibular nerve in five cases and both the maxillary and mandibular nerve together involved in seven cases with a highest incidence (Fig. 11).
Number of radiofrequency lesions made to relieve tic pain: nine patients required three radiofrequency lesions, five patients required to lesions and only one patient required one lesion and found that the maximum number of patients (nine) required only three lesions (60 %) (Fig. 12).
Incidence of complications (Table 2): only two patients developed hematoma and in all other 13 cases there was no complications observed immediate post operatively.
Fig. 9.
Sex distribution
Fig. 10.
Percentage of sides involved
Fig. 11.
Branch of trigeminal nerve involved
Fig. 12.
No. of radiofrequency lesion
Table 2.
Immediate postoperative complications
| Complications | Number | % | 90% CI |
|---|---|---|---|
| Yes | 2 | 13.3 | 0.05–33.36 |
| No | 13 | 86.7 | 66.64–95.48 |
| Total | 15 | 100 |
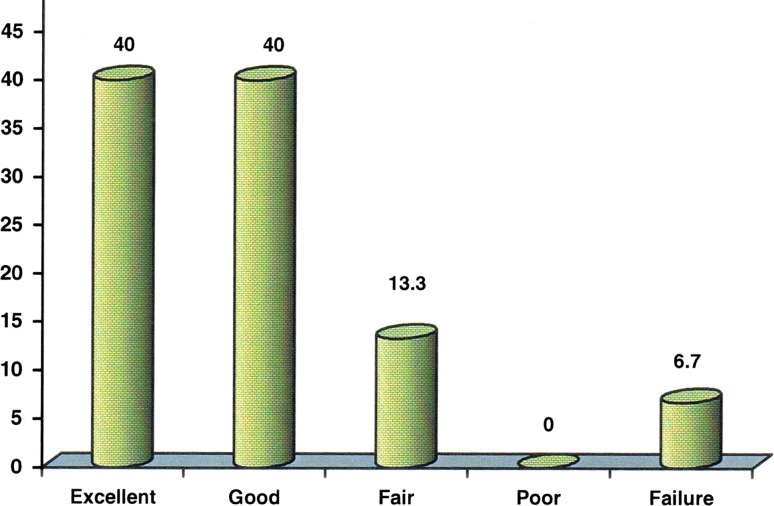
Response of patients of TN treated with RF lesions during follow up period of 1 year (Table 3; Fig. 13).
Table 3.
Comparison of response after the treatment with RF lesion during follow-up
| Response | Follow up | P value | ||||
|---|---|---|---|---|---|---|
| Day 1 | Week 1 | Month 1 | Month 6 | lst Year | ||
| Tic pain | 0 | 0 | I (6.7 %) | 0 | 0 | |
| Minor dysesthesia | 0 | 0 | 0 | 4 (26.7 %) | 4 (26.7 %) | 0.01764* |
| Moderate dysesthesia (%) | 1 (6.7) | 1 (6.7) | 1 (6.7) | 1(6.7) | 1(6.7) | |
| Major dysesthesia | 0 | 0 | 0.0 | 1 (6.7 %) | 0 | – |
| Hypalgesia (%) | 10 (66.7) | 12 (80.0) | 5 (33.3) | 2 (13.3) | 5 (33.3) | 0.0960+ |
Fig. 13.
Response of patients of TN treated with RF lesions
Early pain relief (immediately, postoperatively to 6 month) classified as excellent or good (successful), occurred in 12 of 15 patients (80 %). Fair or poor pain relief (unsuccessful) occurred in three patients (20 %).There was no mortalities and no major morbidity. Excellent and good outcome together was 80 % with 90% CI which is statistically significant (Table 4).
Table 4.
Results
| Results | Number (n = 15) | % | 90% CI |
|---|---|---|---|
| Excellent | 6 | 40.0 | 22.32–60.74 |
| Good | 6 | 40.0 | 22.32–60.74 |
| Fair | 2 | 13.3 | 4.52–33.36 |
| Poor | 0 | 0.0 | – |
| Failure | 1 | 6.7 | 1.50–25.08 |
Inference
Excellent + good outcome in the present study was 80.0 % with 90% CI (59.12–91.71) which is statistically significant.
Discussion
TN has been a condition with no definite etiology established, and also treatment modalities varied from time to time. Dental and medical specialties are both involved with the evaluation and treatment of patients with craniofacial disorders. It has been shown that many patients with these types of problems can go undiagnosed, be misdiagnosed, and have multiple diagnostic and therapeutic interventions before being given the correct diagnosis [7, 8].
Although the results of this study show that RTR is very effective and has limited side effects, avoiding any surgical intervention should be a primary consideration [9–12]. Even the low rate of side effects found in this study can be significantly debilitating in some cases (dysesthesia, analgesia, hypoalgesia), medical therapy before surgical consideration is therefore necessary and can be effective in many patients.
Of the patients in this study who underwent RTR, 94.3 % had early, complete pain relief when compared with other series (Table 5) our data have some similarities and differences.
Table 5.
Comparison with various treatment modalities of TN
| Comparison | Radio frequency thermal rhizotomy | Microvascular decompression | Percutaneous ballon compression | Percutaneous retrogasserion glycerol rhizotomy | Leskell gamma knife treatment |
|---|---|---|---|---|---|
| Sample size | 15 | 24 | 141 | 60 | 12 |
| Results excellent/good (%) | 80 | 71 | 74 | 53 | 73 |
| Failure/recurrence (%) | 20 | 29 | 26 | 47 | 27 |
| Author | Present study | Fergusson et al. [5] | Brown and Gouda [2] | Burchiel et al. [3] | Rand [10] |
Our initial results were slightly less successful 94.3 % versus more than 97 %.The reason for this difference is possibly related to philosophical and clinical consideration of patients for RTR. Although the pain control is the ultimate goal, the relevant issues of the procedure and the decision making procedure were thoroughly discussed with each patient.
RTR is very effective and therefore is often ethically difficult to withhold this treatment from this patient. However many patients with pain are desperate and will say initially that they understand and agree to the potential side effects PRR in exchange for relief of pain. This frequently becomes a difficult challenge, especially when faced with a procedure we believe in, perform regularly and are studying. With RTR being a selective neuroablative procedure it can be performed in a differentially graded fashion. This can give pain relief without the more troublesome pain relief with out the more trouble some side effects. Our technique of performing RTR uses this concept to minimize side effects and provide complete pain relief. The recurrence rate was found to be 20 % in the present study.
Pain recurrence after a successful RTR may not be related to the technique of the procedure but is more likely a property of the disease process. Once a successful thermal lesion is made, the long term anatomic, histologic, and neurophysiologic that occur are not known.
This most likely has some clinical relevance to long term pain relief and recurrence rates, along with possibly altering the pathophysiologic process that is responsible for producing TN.
Anesthesia dolorosa, although an unfortunate complication of RTR as well as other neuroablative procedure, did not occur with a high frequency in the present study.
Dyesthesia is a more common and problematic side effect of RTR. In the present study the rate of mild dyesthesia was 26.7 %, based on this we postulate that our rate of dysesthesia is relatively lower than that of other series because of careful patient evaluation, careful selection of patients for RTR and, most importantly, the production of small, precise lesions producing hypoalgesia and not analgesia or anesthesia.
Other complications like corneal analgesia, masticatory muscle weakness, keratitis did not occur in our patients enrolled in the present study.
Summary and Conclusion
Surgical treatment with PRR is a safe and effective way to manage patients with TN in whom pharmacologic therapy is either ineffective or not tolerated. The side effects are low and are well tolerated. It was found in the present study that it is an effective and safe procedure for initial surgical management of TN.
The major appeal of PRR approach in the treatment of TN is its relative simplicity. Differential coagulation of a delta and C fibers which mediate pain and A beta touch fibers which give touch perception, is the principle of this method.
Though the number of cases (15 patients) and follow up is also short (1 year) the following conclusion can be drawn entirely based on present study.
It is a minimally invasive and effective procedure that is especially indicated in older patients with that is confined to the maxillary and mandibular divisions of trigeminal nerve with a low rate of recurrence.
The procedure can be safely carried out as out-patient procedure.
It provides controlled selective lesions with complications being rare.
In the present study the application of stereotactic principles in the treatment of TN is in no way disappointing. Though the neurophysiological stimulation and response is superior in isolating the division, the application of stereotactic principles will add to efficacy and precision of the technique.
This PRR procedure has stood the test of time at present in relieving the agony of patients suffering from TN.
References
- 1.Allenberg M, Haegerstam G. Invasive dental treatment, pain reports, and disease conviction in chronic facial pain patients: a prospective patients. Acta Odontol Scand. 1995;53:41. doi: 10.3109/00016359509005943. [DOI] [PubMed] [Google Scholar]
- 2.Brown JA, Gouda JJ (1997) Percutaneous balloon compression of the trigeminal nerve. Neurosurg Clin N Am 8(1):53–62 [PubMed]
- 3.Burchiel KJ, Clarke H, Haglund M, et al. Long term efficacy of microvascular decompression in trigeminal neuralgia. J Neurosurg. 1988;68:35–38. doi: 10.3171/jns.1988.69.1.0035. [DOI] [PubMed] [Google Scholar]
- 4.Carney LR. Considerations on the cause and treatment of trigeminal neuralgia. Neurology. 1967;17:1143–1151. doi: 10.1212/WNL.17.12.1143. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson GG, Brett DC, Peerless SJ, Barr HW, Girvin JP (1981) Trigeminal neuralgia: a comparison of the results of percutaneous rhizotomy and microvascular decompression. Can J Neurol Sci 8(3):207–214 [DOI] [PubMed]
- 6.Fromm GH, Sessle BJ. Pathophysiology of trigeminal neuralgia. In: Fromm GH, Sessle BJ, editors. Current concepts regarding pathogenesis and treatment. Boston: Butterworth-Heinmann; 1991. pp. 105–130. [Google Scholar]
- 7.Jannetta PJ. Microvascular decompression of the trigeminal nerve for the is treatment of Tic Douloureux. In: Youmans J, editor. Neurological surgery (ed 4) Philadelphia: Saunders; 1996. pp. 3404–3415. [Google Scholar]
- 8.Onofrio BM. Radiofrequency percutaneous ganglion lesions. J Neurosurg. 1973;42:132–139. doi: 10.3171/jns.1975.42.2.0132. [DOI] [PubMed] [Google Scholar]
- 9.Oppenheim H. Textbook of nervous disease, 5th edn. New York: Stechert and Co.; 1911. [Google Scholar]
- 10.Rand RW (1997) Leksell Gamma Knife treatment of tic douloureux. Neurosurg Clin N Am 8(1):75–78 [PubMed]
- 11.Scrivani SJ, Keith DA, Mathews ES, Kaban LB. Percutaneous sterotactic differential radiofrequency thermal rhizotomy for the treatment of trigeminal neuralgia. J Oral Maxillofac Sur. 1990;57(2):104–112. doi: 10.1016/S0278-2391(99)90218-5. [DOI] [PubMed] [Google Scholar]
- 12.Tensor RB. Trigeminal neuralgia; mechanisms of treatment. Neurology. 1998;51:17–19. doi: 10.1212/WNL.51.1.17. [DOI] [PubMed] [Google Scholar]