Abstract
Objectives
This study was undertaken to compare the anesthetic properties of 4 % Articaine hydrochloride and 2 % Lidocaine both with 1:100,000 epinephrine for mandibular inferior alveolar nerve anesthesia.
Materials and Methods
Thirty healthy patients were included in this randomized double-blind clinical cross over study. Each subject received each test solution at different times. Inferior alveolar nerve block anesthesia was used for extraction of bilateral impacted mandibular third molar on different occassions. The time of onset of action, duration of anesthesia, efficacy of anesthesia, hemodynamic parameters and oxygen saturation were monitored during the procedure. A visual analog scale was used to assess pain during surgery, and thus subjectively evaluate the anesthetic efficacy of the two solutions.
Results
No statistically significant differences were seen in the onset and duration of anesthesia between the Articaine and Lidocaine solutions.
Conclusions
4 % Articaine offers better clinical performance than 2 % Lidocaine, particularly in terms of latency and duration of the anesthetic effect. However, no statistically significant differences in anesthetic efficacy were recorded between the two solutions.
Keywords: Efficacy, Articaine, Lidocaine, Impacted mandibular third molar, Randomized, Clinical study
Introduction
Dentistry enjoys the first credit of introducing general anesthesia by Horace Wells in 1844, a dentist who inhaled nitrous oxide and got his tooth extracted [1]. The era of local anesthetics started with discovery of Cocaine in 1860 [2]. Later, the developments of Novocain 1904 and then Lignocaine by Lofgren and Lundquist in 1942 revolutionized dental practice. This soon became a gold standard drug against which all other new local anesthetics were compared and later several newer drugs such as Bupivacaine, Etidocaine, Articaine, Mepivacaine etc. were discovered [2, 3].
Articaine hydrochloride (HCl) in 1969 with the name of Carticaine, was first marketed in Germany in 1976. The pharmacological characteristics of this anesthetic are responsible for its main advantages. Substitution of the aromatic ring with a thiophenic ring increased the liposolubility of the drug along with its potency (1.5 times greater than that of lidocaine) [3]. Moreover, Articaine is the only amide local anesthetic containing an ester group in its molecular structure—thus allowing metabolization of the drug both by plasma esterases and by liver microsomal enzymes. The clinical advantages of Articaine include the duration of its anesthetic effect—only surpassed by ultra-long acting anesthetics such as Bupivacaine, Etidocaine and Ropivacaine—and its superior diffusion through bony tissue [4–7]. Since its discovery various studies [8–59] have been carried out which compared Articaine with various anesthetic agents.
Lidocaine being the safest, most commonly used anesthetic agent, with encouraging results referring to greater efficacy of Articaine [8, 9], only few studies [24–26, 35, 36, 44, 45, 50, 51, 53, 55, 59] reported about the comparison of Lidocaine and Articaine and in India only few studies on third molar surgery are conducted, we decided to compare the solution of 2 % Lidocaine in 1:100,000 with 4 % Articaine in 1:100,000 in surgical removal of impacted third molars.
Thus the aims and objectives of the study were planned as:
To assess the efficacy of Articaine and Lidocaine for surgical removal of impacted lower third molar.
To study time of onset and duration of anesthesia after injection of Articaine and to compare with Lidocaine.
To monitor cardiovascular responses after administration of Lidocaine 2 % and Articaine 4 % with adrenaline 1:100,000.
To observe any signs of systemic toxicity clinically.
Materials and Methods
All patients provided written informed consent during the pretreatment screening period before any study procedures were performed. The protocol of this study was approved by the Ethics Committee of Modern Dental College and Research Centre, India.
The study population comprised 30 patients [13 males and 17 females, mean age 25.8 years (standard deviation (SD) = 0.86), range from 18–48 years]; with symmetrically positioned partial impacted lower third molars. Eligibility criteria included absence of systemic illness and no signs of inflammation or infection at the extraction sites. Exclusion criteria included medical history of cardiovascular and kidney diseases, gastrointestinal bleeding or ulceration, allergic reaction to local anesthetic, allergy to aspirin, ibuprofen, or any similar drugs, and pregnancy or current lactation. Patients were also given instructions not to take any other pain medication prior to the removal of the third molars. This was a double-blind study; neither the surgeon nor the patients were aware of the local anesthetic being tested at the two different appointments. Each patient required similar surgical treatment on opposite sides of the mandible, which was performed in two visits, 1 to 2 months apart. For local anesthesia, in the first appointment the patients were randomly selected to receive either 2 % lidocaine (Lignospan®, Indore, India) or 4 % Articaine (Articaine 4 % Septanest®, Indore, India) both with 1:100,000 epinephrine. In the second appointment, the local anesthetic not used previously was then administered in a crossed manner. All surgeries were performed by the same surgeon.
Effect was defined as follows:
Successful—the patient felt no pain during surgery, patient who only had a short duration of pain sensation when their tooth was sectioned during surgery were also included in this group.
Partial successful—the patient experienced some pain, but additional small amount of the same coded local anesthetic solution was sufficient to produce analgesia.
Failure—local anesthetic solution had to be given in excess in order to complete surgery.
The data obtained in the study was tabulated under two groups assigned to each of the local anesthetic agent used in the study. Group A was Articaine and group B was Lidocaine.
The data obtained in the study included:
Onset of anesthesia—recorded from time of injection to the onset of anesthesia of the lip as subjective and objective symptoms.
Duration of surgery—measured from time of placing the incision to the last suture placed.
Duration of anesthesia—The duration of anesthesia was in turn recorded as the time from initial patient perception of the anesthetic effect to the moment in which the effect began to fade.
Blood pressure, oxygen saturation and heart rate were recorded before the administration of local anesthetic and after 5, 15, 30, 45 and 60 min.
Any signs of systemic toxicity like talkativeness, slurred speech, apprehension, localized muscular twitching and tremor of the hand and feet, rise in blood pressure, heart rate and respiratory rate were noted.
Intra operatively pain was scored on visual analog scale (0–10) (e.g. none, slight, mild, moderate, severe) [60].
The statistical analysis of the results was carried out with the Student t- and Chi-square tests.
Results
Of the 38 patients, eight were excluded from the study: one due to the development of transient inferior alveolar nerve paresthesia, another because of transient paresthesia of the lingual nerve, and six as a result of voluntary dropout from the study. A total of 60 interventions were included in the study: 30 performed with 2 % lidocaine, and 30 with 4 % articaine (with epinephrine 1:100,000 in both cases). The mean duration of surgery was 28.95 min (SD: 12.49) for Articaine, 28.75 min (SD: 14.49) for lidocaine, without significant differences between the two groups. The mean time of onset anesthetic action subjective symptoms for Articaine was 1.35 min (SD: 0.49) and Lidocaine was 1.40 min (SD: 0.60), the objective symptoms were at 2.12 min (SD: 0.81) for Articaine and 2.15 min (SD: 0.86) for lidocaine; no statistically significant differences being observed between the two anesthetic solutions. In turn, the mean duration of the anesthetic effect was 196.8 min (SD: 57.3) for Articaine and 175.9 min (SD: 51.7) for Lidocaine the difference in this case being statistically not significant (p = 0.092) (Table 1).
Table 1.
Onset of anesthesia, duration of surgery and anesthesia
| Variables | Group A (n = 30) | Group B (n = 30) | p value | Result |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Time of onset | ||||
| Subjective symptoms | 1.35 ± 0.49 | 1.40 ± 0.60 | 0.773 | NS |
| Objective symptoms | 2.12 ± 0.81 | 2.15 ± 0.86 | 0.914 | NS |
| Duration of anesthesia (min) | 196.8 ± 57.3 | 175.9 ± 51.7 | 0.092 | NS |
| Duration of surgery (min) | 28.95 ± 12.49 | 28.75 ± 14.49 | 0.974 | NS |
| Amount of LA (ml) | 1.73 ± 0.11 | 1.86 ± 0.41 | 0.159 | NS |
| VAS | 1.88 ± 1.18 | 2.45 ± 1.68 | 0.218 | NS |
In one intervention (3.33 % of cases) re-anesthesia of the surgical zone proved necessary for Articaine and four interventions (13.33 % of cases) for Lidoacine (Table 2). However, in terms of the amount of anesthetic solution used (including the cases of re-anesthesia) during the operation to achieve the desired anesthetic effect, larger volumes of 2 % lidocaine with epinephrine 1:100,000 were required, administering an average of 1.86 ml (SD = 0.41) per operation, versus 1.73 ml (SD = 0.11) in the case of 4 % Articaine with epinephrine 1:100,000. This differences did not quite reach statistical significance, however (p = 0.159). Lastly, subjective intraoperative pain scoring by the patients showed no differences between the two anesthetic solutions, with mean VAS scores of 1.88 (SD: 1.18) and 2.45(SD: 1.68) for articaine and lidocaine, respectively (Table 1).
Table 2.
Local anesthetic effect of group A and group B (%)
| Anesthetic effect | Group A | Group B |
|---|---|---|
| Successful | 96.67 % | 86.67 % |
| Partial successful | 3.33 % | 13.33 % |
| Failure | 0 | 0 |
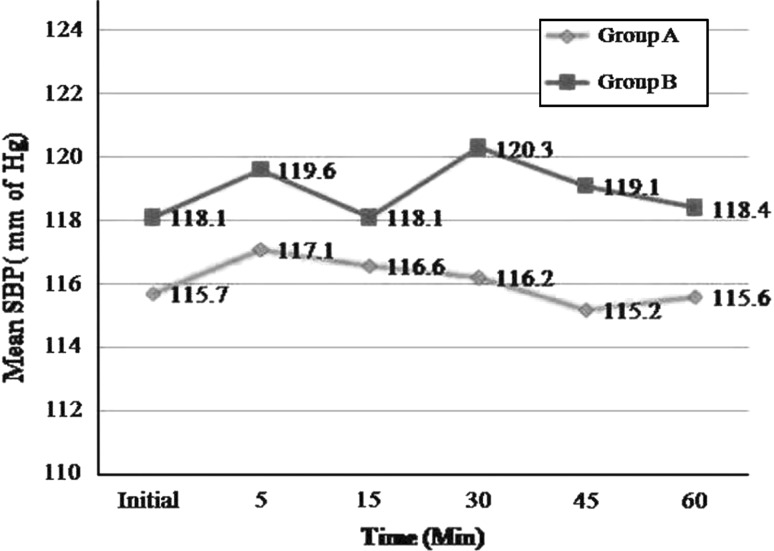
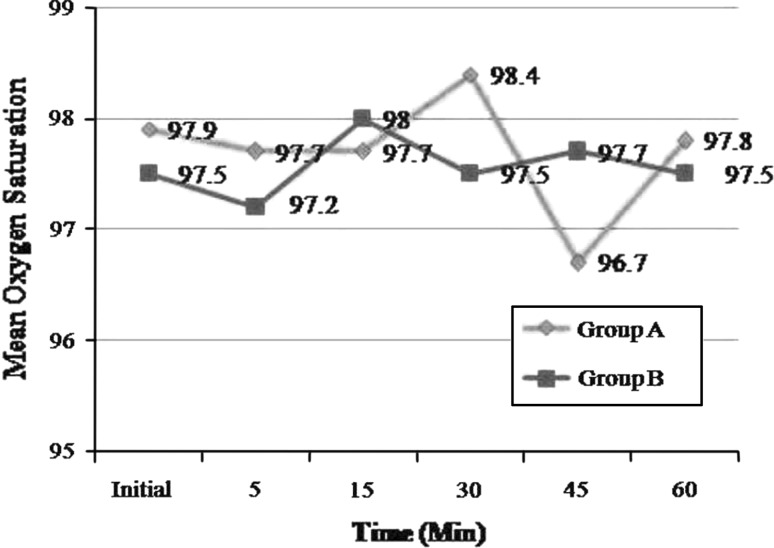
With respect to the hemodynamics parameters, there was no statistically significant difference in blood pressure, heart rate, or oxygen saturation before and during the surgery (p > 0.05) (Figs. 1, 2, 3, 4).
Fig. 1.
Mean values of pulse rate
Fig. 2.
Mean values of Systolic blood pressure
Fig. 3.
Mean values of Diastolic blood pressure
Fig. 4.
Mean values of Oxygen saturation
Discussion
The discovery of Lidocaine in 1942 [5] has been landmark in the history of local anesthetic. Today it is considered as a reference standard against which other local anesthetic agents are compared. Various studies have been done in dentistry evaluating the safety and efficacy of Articaine [10, 11, 21–37]. Since its introduction in 1969, Articaine has gradually become implanted in Europe. Its chemical structure, different to that of other local anesthetics due to substitution of the aromatic ring with a thiophenic ring, and the presence of an additional ester ring, provides Articaine with increased liposolubility and intrinsic potency, as well as greater plasma protein binding versus other commonly used local anesthetic such as Prilocaine or Mepivacaine. These differential characteristics are in turn clinically reflected by a shorter latency and increased duration of anesthesia, as well as superior bony tissue diffusion [50].
Onset of action
Depends on a number of factors, such as the intrinsic properties of the drug substance used, and the anesthetic technique employed. On the other hand, latency is directly influenced by the corresponding pKa value—smaller pKa values being associated to shorter latency. Accordingly, 4 % Articaine (pKa = 7.8) would at least in theory present a shorter latency than 2 % Lidocaine (pKa = 7.9). Our results coincide with this assumption, since the latency was shorter for Articaine versus Lidocaine.
The mean time taken by 4 % Articaine was 2–3 min as compared to 3 min for 2 % Lidocaine [5]. Dugal et al. [23] concluded onset of action of Lidocaine was 1.15 min. Moore et al. [40] reported 4 % Articaine HCl with 1:100,000(A100) as 4.2 ± 2.8 min and for 4 % Articaine HCl with 1:200,000(A200) as 4.7 ± 2.6 min. Colombini et al. [43] stated 149.50 ± 14.29 s for Articaine. Rebolledo et al. [50] reported 53.03 s (0.93 min) for Articaine versus 75.04 s (1.25 min) for Lidocaine. The long period of analgesia for Articaine explained by Gregorio et al. [54] stated that onset of action of Articaine was 1.66 ± 0.13 min. Statistically significant difference was not present in action of onset of the two drugs. The average time of onset for subjective symptoms for Articaine in our study was 1.35 min (1–2 min) and objective symptoms 2.12 min (1.08–4 min). On comparison to Lidocaine it was subjective symptoms 1.40 min (1–3 min) and objective symptoms 2.15 min (1–4 min). The results of the present study are in accordance with the above reported studies.
Duration of anesthesia
Duration of anesthesia is proportional to its degree of protein binding. However, the duration of the effect of the local anesthetic is also dependent on the injection site or concentration of vasoconstrictor present in the anesthetic solution, among other factors. Articaine presents one of the greatest protein binding percentages of all amide local anesthetics, comparable only to ultra-long action substances such as Bupivacaine, Ropivacaine and Etidocaine. This in turn implies a longer duration of the anesthetic effect [50]. The duration of anesthesia required to complete the procedure will be major consideration in the selection of a local anesthetic solution. In the present study, average duration of anesthesia for Articaine was 196.8 ± 57.3 min (range 85–317) in comparison to Lidocaine which was 175.9 ± 51.7 min (range 60–241). There was no significant difference in duration of anesthesia between two drugs. Articaine stands better in this respect though statistically it is not significant. Haas et al. [25], Vahatalo et al. [26] and Costa et al. [36] stated that 4 % Articaine with 1:100,000 epinephrine clinically presented the shortest onset and the longest duration periods and both Articaine solutions produced shorter onset and longer duration of pulpal anesthesia by maxillary infiltration than the Lidocaine solution but statistically did not confirm better clinical results. Moore et al. [40] reported mean duration of pulpal anesthesia was (A100)61.8 ± 59 min and (A200)51.2 ± 55.9 min. Colombini et al. [43] concluded that 273.80 ± 15.94 min for Articaine and 216.85 ± 20.15 min for Mepivacaine. Rebolledo et al. [50] reported 220.8 min for Articaine while 168.2 min for Lidocaine anesthesia. The long period of analgesia for Articaine explained by Gregorio et al. [54] in their study stated that the concentration of Articaine in the alveolus of a tooth after extraction is about 100 times higher than in systemic circulation. This saturable local Articaine mechanism has been considered as possibly contributing to the observed duration of the local anesthetic effect. The findings of the present study are confirmatory of the previous studies.
Profoundness/Depth of anesthesia
Profoundness of anesthesia was made by means of a visual analog scale (VAS) in which the patient was instructed to score intraoperative pain intensity. In our study intra-operative VAS of 1–10 for Articaine was 1.88 ± 1.18 while for Lidocaine it was 2.45 ± 1.68 but these results are statistically not significant. This is in accordance with Malamed et al. [8, 9], Rebolledo et al. [50]. Gregorio et al. [54] reported the intra operative analgesia evoked by Articaine may be explained by its ability to readily diffuse through tissues due to the presence of thiophene group in the molecule which increases liposolubility. Sumer et al. [57] reported that painfulness of local anesthetic injections may be related to the pH of the injected solutions. Local anesthetic solutions with low pH have been thought to cause a burning sensation and thus more pain than anesthetics with more neutral pH. The pH of Lidocaine is 5–5.5 while that of Articaine is 4.4–5.2 and Prilocaine was 3.5–5.2 and concluded that there was no significant differences among the anesthetic solutions for injection pain. Nusstein et al. [35] reported that the intra-ligamentary injection pain of 4 % Articaine with 1:100,000 epinephrine was similar to 2 % Lidocaine when administered with a computer-controlled local anesthetic local anesthetic delivery system. Haase et al. [53] stated that there was no significant difference with the injection pain of both the solutions.
With regards to surgical analgesia, no significant difference exists between the two solutions. Successful analgesia was noted in 96.67 % of patients in Articaine group and 86.67 % of patients in Lidocaine group (Table 2).
Efficacy of Articaine
In this study a clinical evaluation of the efficacy of the two anesthetic solutions was made by comparing the need for re-anesthesia during surgery. In one intervention (3.33 %) another dose of Articaine had to be administered via local infiltration technique. The number of repeat anesthetic procedures was greater when using 2 % Lidocaine (13.33 %). On the other hand, this difference in the total amount of anesthetic solution used for Articaine is 1.73 ± 0.11 ml and that for Lidocaine is 1.86 ± 0.41 ml and the value is similar to the value reported by Malamed et al. [8] in their multi-centric study of 1,325 adult patients. However, the difference in both the mean frequency and amount of solution used for re-anesthesia of the surgical zone failed to reach statistical significance. This was in accordance to Rebolledo et al. [50]. Potonick et al. [45] reported that 2 % Articaine more effectively depresses the compound action potential of the A fibers in the isolated rat sural nerve than either 2 % or 4 % Lidocaine or 3 % Mepivacaine. Paessler et al. [46] concluded that the 4 % Articaine solution did not prove superior in local anesthetic effect. Articaine 2 % with epinephrine 1:200,000, therefore, can be considered a suitable local anesthetic for tooth extractions. The most noticeable difference observed between the two injection solutions concerned the duration of anesthesia, which was significantly shortened under the low dose solution. Foster et al. [17], Kanaa et al. [44], Robertson et al. [47] and Haase et al. [53] concluded that buccal infiltration of the mandibular first molar with 4 % Articaine of 1:100,000 epinephrine will result in a higher success rate than 2 % Lidocaine with 1:100,000 epinephrine, but the duration of pulpal anesthesia will decline over 60 min with either formulation. Tofoli et al. [34] and Moore et al. [48] reported that 4 % Articaine anesthetic formulations containing epinephrine provided excellent surgical pain control. For patients who can tolerate higher amounts of epinephrine, the 4 % Articaine 1:100,000 epinephrine formulations had the additional therapeutic advantage of providing better visualization of the surgical field and less bleeding. Santos et al. [49] reported that epinephrine concentration in 4 % Articaine solution does not influence the clinical efficacy of local anesthetic in terms of anesthetic properties (latency, post operative analgesia, post operative anesthesia and quality of anesthesia), intra operative bleeding and hemodynamic parameters in patients undergoing lower third molar removal. Gregorio et al. [54] stated that 4 % Articaine provided shorter time of onset, comparable homeostasis and post operative pain control with a shorter duration of soft tissue anesthesia in lower third molar removal. Uckan et al. [39] and Lacet-Lima et al. [58] reported that Articaine demonstrated relatively good vestibule palatal diffusion with efficacy rates of anesthesia 98 %. Retained maxillary third molar extractions could be performed with only buccal vestibule infiltrative terminal anesthesia in the majority of cases with no need for supplemental palatal anesthesia [58].
Pulse Rate
In our study the values of cardiovascular parameters showed that pulse rate increased with injection of 4 % Articaine and 2 % Lidocaine. The increase in pulse rate was maximum after 5 min of administration of Articaine and Lidocaine. The mean rise in Articaine group was 4 beats/min and the percentage increase from basal value was by 4.39 % and gradually decreased to the basal value after 30 min. The mean rise in Lidocaine group was 6.4 beats/min and the percentage increase from the basal value was by 7.46 % and gradually decreased to the basal value after 30 min. This correlates that the pulse rate increased during the time of incision and osteotomy but gradually decreases to normal base line over time. This was in accordance to Moore et al. [40], Martinez et al. [52], Vasconcellos et al. [56]. Meral et al. [16] reported that increase in pulse rate immediately after injection were likely an expression of endogenous catecholamine because of the injection pain. Nusstein et al. [35] concluded that pulse rate did not significantly increase with intra-ligamentary injection using the computer–controlled local anesthetic system with both anesthetic solutions.
Blood Pressure
The change in the systolic and diastolic blood pressure was recorded after administration of the local anesthetic agent and compared with the base line value in both the groups. There was no significant change noted in the systolic or diastolic blood pressure from the base line values at different time intervals after administration of both the anesthetic solutions (p > 0.05). Hersh et al. [41] reported that there was greater evidence of increase in systolic blood pressure in Articaine with 100,000 epinephrine (A100) after completion of injection when compared to Articaine with 200,000 epinephrine (A200). Santos et al. [49] reported that transient increase or decrease in blood pressure and oxygen saturation were observed but they were neither clinically significant nor statistically significant. Several authors Malamed et al. [8, 9], Brkovic et al. [18], Colombini et al. [43], Martinez et al. [52], Elad et al. [55], Vasconcellos et al. [56] were in accordance with our findings. On the contrary Moore et al. [40] reported that only A100 treatment group showed a statistically significant decrease in systolic blood pressure at the completion of testing A100 decreased 2.6 mmHg, p = 0.0153). Both A100 and A200 treatment groups showed small (2–4 mmHg) but statistically significant decreases in diastolic blood pressure 5 min post injection, both were considered as minimal clinical significance. Hence findings of the present study coincide with the findings of previous authors.
Oxygen Saturation
The change in the oxygen saturation was recorded after administration of the local anesthetic agent and compared with the base line value in both groups. There was no significant change noted in the oxygen saturation from the base line values at different time intervals after administration of 4 % Articaine and 2 % Lidocaine (p > 0.05). Several authors Colombini et al. [43], Santos et al. [49], Martinez et al. [52], Elad et al. [55] reported in accordance to our result. Vasconcellos et al. [56] suggested that all patients submitted to surgery for removal of third molars are at risk for hypoxia. Short episodes of hypoxia may have only minor consequences in healthy patients, but those in unhealth may develop serious complications.
Adverse Effects
According to literature Articaine has potential to cause methemeglobinemia, neuropathies, paresthesia [7, 14, 15, 32, 38, 50], hypersensitivity [28], allergy [29, 31]. Malamed et al. [8, 9] reported overall incidence of adverse events in the combined studies was 22 % for Articaine and 20 % Lidocaine of which paresthesia was 0.9 %, hypoesthesia 0.7 %, headache 0.55 %, infection 0.45 %, rash and pain 0.3 %. Potonick et al. [45] reported that although 4 % Articaine is more effective, they suggested that it may be worth considering replacing the 4 % Articaine with 2 % Articaine solution as the risk of an intravenous injection of the anesthetic solution during the induction of inferior alveolar nerve block and the possibility that the 4 % Articaine solution may increase the incidence of non surgical paresthesia. In our study, two patients experienced inferior alveolar nerve paresthesia who were anesthetized by Articaine. Rebolledo et al. [50] reports there is insufficient evidence to believe the underlying cause to be the type of anesthetic used. We therefore consider that further studies are needed to establish such a possible relationship. Most of the findings between Lidocaine and Articaine are comparable but statistically insignificant. Clinically significant difference exist wherein Articaine is found more comfortable to the patient with less bleeding, more profoundness, less time of onset of action, slightly larger duration of anesthesia and surgeons comfort. Hence the authors have recommended Articaine practically a better anesthetic [49, 50].
Conclusion
Thus it can be concluded that Articaine was as potent as Lidocaine and showed similar properties to Lidocaine (Gold standard) and better cardiac stability. In medically compromised patients where the use of Lidocaine with adrenaline can be recommended with caution, Articaine can be a better acceptable alternative. However, further studies are required in these groups of patients to prove its safety. Clinically significant advantage was found in Articaine. The main advantage of Articaine is its better haemostatic and bone diffusibility but the drawback of Articaine is paresthesia. There is absolutely no scientific evidence available to support the claim that Articaine is associated with a greater incidence of paresthesia [5, 10, 11, 31]. However further studies on a larger group of population are recommended for greater authenticity of this relatively new drug in oral and maxillofacial surgery in India to make as popular and safer to be used as a routine anesthetic agent in dentistry. Study in other surgical procedures, particularly larger surgical procedures as well as medically compromised patients are also recommended to give clinically significant rating to either of these drugs.
Acknowledgments
Conflict of interests
None.
Funding
None.
References
- 1.Bennett CR (ed) (1990) Phero JC: Postoperative pain control. In: Monheim’s local anesthesia and pain control in dental practice, 7th edn. CV Mosby, St. Louis, pp 125–159
- 2.Catterall W, Mackie K (2001) Local anesthetics. In: Hardman JG, Limbird LE (eds) Goodman & Gilman’s the pharmacological basis of therapeutics, 10th edn. McGraw-Hill, New York, NY, pp 367–384
- 3.Strichartz GR, Berde CB (2005) Local anesthetics. In: Miller RD (ed) Miller’s anesthesia. Churchill Livingstone, New York, pp 573–603
- 4.Satoskar RS, Bhandarkar SD, Ainapure SS (1999) Pharmacology and pharmacotherapeutics. Popular Prakashan, Mumbai, pp 224–229
- 5.Malamed SF (ed) (2007) Clinical action of specific agents. In: Handbook of local anesthesia, 5th edn. Mosby, St Louis, MO, pp 61–65 and 71–73
- 6.Becker DE, Reed KL. Essentials of local anesthetic pharmacology. Anesth Prog. 2006;53:98–109. doi: 10.2344/0003-3006(2006)53[98:EOLAP]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yagiela JA. Local anesthetics: a century of progress. Anesth Prog. 1985;32(2):47–56. [PMC free article] [PubMed] [Google Scholar]
- 8.Malamed SF, Gagnon S, Leblanc Dominique. Efficacy of Articaine: a new amide local anesthetic. J Am Dent Assoc. 2000;131:635–642. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 9.Malamed S, Ganong S, Leblanc D. Articaine hydrochloride: a safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177–185. doi: 10.14219/jada.archive.2001.0152. [DOI] [PubMed] [Google Scholar]
- 10.Rahn R, Ball B (2001) Local anesthesia in dentistry—articaine and epinephrine for dental anesthesia, 1st edn. 3M ESPE AG, Seefeld, Germany
- 11.Hersh EV (2008) Local anesthetics. In: Fonseca RJ (ed) Oral and maxillofacial surgery. WB Saunders, Philadelphia, pp 58–78
- 12.Calatayud J, Gonzalez History of the development and evolution of local anesthesia since the coca leaf. Anesthesiology. 2003;98:1503–1508. doi: 10.1097/00000542-200306000-00031. [DOI] [PubMed] [Google Scholar]
- 13.Tripati KD (2008) Essentials of medical pharmacology, 6th edn. Jaypee Brothers medical publishers, pp 351–361
- 14.Kaufman E, Goharian S, Katz Y. Adverse reactions triggered by dental local anesthetics: a clinical survey. Anesth Prog. 2000;47:134–138. [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell JR, Maestrello CL, Campbell RL. Allergic response to meta-bi-sulfite in Lidocaine anesthetic solution. Anesth Prog. 2001;48:21–26. [PMC free article] [PubMed] [Google Scholar]
- 16.Meral G, Tasar F, Sayin F, Saysel M, Kir S, Karabulut E. Effects of Lidocaine with and without epinephrine on plasma epinephrine and Lidocaine concentrations and hemodynamic values during third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:E25–E30. doi: 10.1016/j.tripleo.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 17.Foster W, Drum M, Reader A, Beck M. Anesthetic efficacy of buccal and lingual infiltrations of Lidocaine following an inferior alveolar nerve block in mandibular posterior teeth. Anesth prog. 2007;54:163–169. doi: 10.2344/0003-3006(2007)54[163:AEOBAL]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brkovic B, Gardasevic M, Roganovic J, Jovic N, Todorovic L, Stojic D. Lidocaine +clonidine for maxillary infiltration anaesthesia: parameters of anesthesia and vascular effects. Int J oral maxillofac surg. 2008;37:149–155. doi: 10.1016/j.ijom.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Brunetto P, Ranali J, Ambrosano MB, Oliveira C, et al. Anesthetic efficacy of 3 volumes of Lidocaine with epinephrine in maxillary infiltration anesthesia. Anesth Prog. 2008;55:29–34. doi: 10.2344/0003-3006(2008)55[29:AEOVOL]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Porto GG, Vasconcelos CD, Gomes AC, Albert D. Evaluation of Lidocaine and Mepivacaine for inferior third molar surgery. Med Oral Patol Oral Cir Bucal. 2007;12:E60–E64. [PubMed] [Google Scholar]
- 21.Rosenquist JB, Rosenquist KI, Lee KM. Comparison between Lidocaine and Bupivacaine as local anesthetics with Difiunisal for postoperative pain control after lower third molar surgery. Anesth Prog. 1988;35:1–4. [PMC free article] [PubMed] [Google Scholar]
- 22.Hinkley SA, Reader Al, Beck M, Meyer WJ. An evaluation of 4% Prilocaine with 1:200000 epinephrine and 2% Mepivacaine with 1:20, 000 levonordefrn compared with 2% Lidocaine with 1: 100000 epinephrine for inferior alveolar nerve block. Anesth Prog. 1991;38:84–89. [PMC free article] [PubMed] [Google Scholar]
- 23.Dugal A, Khanna R, Patankar A. A comparative study between 0.5% Centbucridine HCl and 2% Lignocaine HCl with adrenaline (1:200000) J Maxillofac Oral Surg. 2009;8(3):221–223. doi: 10.1007/s12663-009-0054-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright GZ, Weinberger SJ, Friedman CS, Plotzke OB. The use of Articaine local anesthesia in children under 4 years of age a retrospective report. Anesth Prog. 1989;36:268–271. [PMC free article] [PubMed] [Google Scholar]
- 25.Haas DA, Harper DG, Saso MA, Young ER. Comparison of Articaine and Prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anesth Prog. 1990;37:230–237. [PMC free article] [PubMed] [Google Scholar]
- 26.Vahatalo K, Antila H, Lehtinen R. Articaine & Lidocaine for maxillary infiltration anesthesia. Anesth prog. 1993;40:114–116. [PMC free article] [PubMed] [Google Scholar]
- 27.Jakobs W, Ladwig B, Cichon P, Ortel R, Krich W. Serum levels of Articaine 2% and 4% in children. Anesth Prog. 1995;42:113–115. [PMC free article] [PubMed] [Google Scholar]
- 28.Malanin K, Kalimo K. Hypersensitivite to the local anesthetic Articaine Hydrochloride. Anesth Prog. 1995;42:144–145. [PMC free article] [PubMed] [Google Scholar]
- 29.Daubliinder M, Muller R, Lipp DW. The Incidence of complications associated with Local Anesthesia in dentistry. Anesth Prog. 1997;44:132–141. [PMC free article] [PubMed] [Google Scholar]
- 30.Diago MP, Sanchis-Bielsa JM. Ophthalmologic complications after intraoral local anesthesia with Articaine. Oral Surg Oral Med Oral Pathol oral Radiol Endod. 2000;90:21–24. doi: 10.1067/moe.2000.107506. [DOI] [PubMed] [Google Scholar]
- 31.Baluga JC, Casamayou R, Carozzi E, Lopez N, Anale R, Borges R, et al. Allergy to local anesthetics in dentistry. Myth or reality? Allergol Immunopathol (Madr) 2002;30(1):14–19. doi: 10.1016/s0301-0546(02)79081-2. [DOI] [PubMed] [Google Scholar]
- 32.Finder RL, Moore PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002;46:747–757. doi: 10.1016/S0011-8532(02)00018-6. [DOI] [PubMed] [Google Scholar]
- 33.Dogan N, Ucok C, Korkmaz C, Ozlem Ucok, Karasu HA. The effects of Articaine HCl on wound healing: an experimental study. J Oral Maxillofac Surg. 2003;61:1467–1470. doi: 10.1016/j.joms.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Tofoli RG, Ramacciato JC, de Oliveria PC, Volpato MC, Groppo FC, Ranali J. Comparison of effectiveness of 4% Articaine associated with 1:100000 or 1:200000 epinephrine in inferior alveolar nerve block. Anesth Prog. 2003;50:164–168. [PMC free article] [PubMed] [Google Scholar]
- 35.Nusstein J, Berlin J, Beck M, Weaver JM. Comparison of injection pain, heart rate increase, and post injection pain of Articaine and Lidocaine in a primary intra-ligamentary injection administered with a computer-controlled local anesthetic delivery system. Anesth Prog. 2004;51:126–133. [PMC free article] [PubMed] [Google Scholar]
- 36.Costa CG, Tortamano IP, Rocha RG, Francischone CE, Tortarmano N. Onset and duration periods of Articaine and Lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- 37.Magliocca KR, Kessel NC, Gerald W. Transient diplopia following maxillary local anesthetic injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:730–733. doi: 10.1016/j.tripleo.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Hillerup S, Jensen R. Nerve injury caused by mandibular block analgesia. Int J Oral Maxillofac Surg. 2006;35:433–437. doi: 10.1016/j.ijom.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 39.Uckan S, Dayangac E, Araz K. Is permanent maxillary tooth removal without palatal injection possible? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:733–735. doi: 10.1016/j.tripleo.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 40.Moore PA, Boynes SG, Hersh EV, DeRossi SS, Sollecito TP, Goodson JM, et al. The anesthetic efficacy of 4% Articaine 1:200000 epinephrine. J Am Dent Assoc. 2006;137:1572–1581. doi: 10.14219/jada.archive.2006.0093. [DOI] [PubMed] [Google Scholar]
- 41.Hersh EV, Giannakopoulos H, Levin LM, Secreto S, Moore PA, Peterson C, et al. The pharmacokinetics and cardiovascular effects of high dose Articaine with 1:100000 and 1:200000 epinephrine. J Am Dent Assoc. 2006;137:1562–1571. doi: 10.14219/jada.archive.2006.0092. [DOI] [PubMed] [Google Scholar]
- 42.Pozos AJ, Martinez R, Aguirre P, Perez J. The effect of Tramadol added to Articaine on anesthesia duration. Oral Surg Oral Med Oral Pathol oral Radiol Endod. 2006;102:614–617. doi: 10.1016/j.tripleo.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 43.Colombini BL, Modena KC, Calvo AM, Sakai VT, Gigilo FP, Dionisio TJ, et al. Articaine and Mepivacaine efficacy in post operative analgesia for lower third molar removal: a double-blind, randomized, cross over study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:169–174. doi: 10.1016/j.tripleo.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 44.Kanaa MD, Whitworth JM, Corbet IP, Meechan JG. Articaine and Lidocaine mandibular buccal infiltration anesthesia: A prospective randomized double blind cross over study. J Endod. 2006;32:296–298. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 45.Potonick I, Tomsic M, Sketelj J, Bajrovic FF. Articaine is more effective than Lidocaine or Mepivacaine in rat sensory nerve conduction block in vitro. J Dent Res. 2006;85:162–166. doi: 10.1177/154405910608500209. [DOI] [PubMed] [Google Scholar]
- 46.Hintze A, Paessler L. Comparative investigations on the efficacy of Articaine 4% (epinephrine 1:200000) and Articaine 2% (epinephrine 1:200000) in local infiltration anaesthesia in dentistry—a randomised double-blind study. Clin Oral Investig. 2006;10:145–150. doi: 10.1007/s00784-005-0025-0. [DOI] [PubMed] [Google Scholar]
- 47.Robertson D, Nusstein J, Reader A, Beck M, McCartney M. The anesthetic efficacy of Articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc. 2007;138:1104–1112. doi: 10.14219/jada.archive.2007.0324. [DOI] [PubMed] [Google Scholar]
- 48.Moore P, Doll B, Delie RA, Hersh EV, et al. Hemostatic and anesthetic efficacy of 4% Articaine HCl with 1:200000 epinephrine and 4% Articaine HCl with 1:100000 epinephrine when administered intraorally for peiodontolal surgery. J Periodontol. 2007;78:247–253. doi: 10.1902/jop.2007.060314. [DOI] [PubMed] [Google Scholar]
- 49.Santos CF, Modena K, Giglio F, Sakai, et al. Epinephrine concentration (1:100000 or 1:200000) does not affect the clinical efficacy of 4% Articaine for lower third molar removal: a double-blind, randomized, cross-over study. J Oral Maxillofac Surg. 2007;65:2445–2452. doi: 10.1016/j.joms.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 50.Rebolledo AS, Molina ED, Aytes LB, Escoda CA. Comparative study of the anesthetic efficacy of 4% Articaine versus 2% Lidocaine in inferior alveolar nerve block during surgical extraction of impacted lower third molars. Med Oral Patol Oral Cir Bucal. 2007;12:E139–E144. [PubMed] [Google Scholar]
- 51.Wahl MJ, Flanagan T, Schmitt MM, Wahl JA, et al. Articaine versus Lidocaine: A prospective, double-blind, randomized study of anesthetic efficacy. J Maxillofac Oral Surg. 2007;6(4):7–10. [Google Scholar]
- 52.Martinez AA, Castellon EV, Aytes LB, Escoda CG. Haemodynamic changes during the surgical removal of lower third molars. J Oral Maxillofac Surg. 2008;66:453–461. doi: 10.1016/j.joms.2007.06.634. [DOI] [PubMed] [Google Scholar]
- 53.Haase A, Reader A, Nusstein J, Beck M, Drum M. Comparing anesthetic efficacy of Articaine versus Lidocaine as a supplement buccal infiltration of the mandibular first molar after an inferior alveolar nerve block. J Am Dent Assoc. 2008;139(9):1228–1235. doi: 10.14219/jada.archive.2008.0338. [DOI] [PubMed] [Google Scholar]
- 54.Gregorio L, Giglio F, Sakai V, Modena KC, et al. A comparison of the clinical anesthetic efficacy of 4% Articaine and 0.5% Bupivaciane (both with 1:200000 epinephrine) for lower third molar removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:19–28. doi: 10.1016/j.tripleo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 55.Elad S, Admon D, Kedmi M, Naveh E, et al. The cardiovascular effect of local anesthesia with Articaine plus 1:2000000 versus Lidocaine plus 1:100000 adrenaline in medically compromised cardiac patients: a prospective, randomized, double blind study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:725–730. doi: 10.1016/j.tripleo.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 56.Vasconcellos RJ, Vasconcelos BC, Genu PR. Influence of local anesthetics with adrenalina 1:1, 00, 000 in basic vital constants during third molar surgery. Med Oral Patol Oral Cir Bucal. 2008;13(7):E431–E437. [PubMed] [Google Scholar]
- 57.Sumer M, Misir F, Celebi N, Muglali A comparison of injection pain with Articaine with adrenaline, Prilocaine with pheylpressin and Lidocaine with adrenaline. Med Oral Patol Oral Cir Bucal. 2008;13(7):E427–E430. [PubMed] [Google Scholar]
- 58.Lacet-Lima, Riberio E, Araujo T, Rocha J et al (2009) Evaluation of the buccal vestibule-palatal diffusion of 4% Articaine HCl in impacted maxillary third molar extractions. Med Oral Patol Oral Cir Bucal 14(3):E 129–E 132 [PubMed]
- 59.Bradt RG, Anderson PF, McDonald NJ, Sohn W, et al. The pulpal anesthetic efficacy of Articaine versus lidocaine in dentistry. J Am Dent Assoc. 2011;142(5):493–504. doi: 10.14219/jada.archive.2011.0219. [DOI] [PubMed] [Google Scholar]
- 60.Gracely Richard H. Measuring Pain in the Clinic. Anesth Prog. 1990;34:88–92. [PMC free article] [PubMed] [Google Scholar]