Abstract
Objective
The present study investigates how consistently DSM-IV major depression (MDD) with psychosis was diagnosed by research consensus across 10 years and the association of clinical characteristics with diagnostic consistency.
Method
The sample included 146 participants, part of a larger first admission cohort (N=628) presenting with psychosis, who were diagnosed with psychotic depression at least once across 4 assessments spanning 10 years (after first admission, at 6-month, 24-month, and 10-year follow-ups). Diagnoses at each assessment were determined from semi-structured interviews, medical records, and informant reports.
Results
Fifty-five (37.7%) of the 146 were diagnosed with psychotic depression at each available assessment, 13(8.9%) switched from MDD to bipolar disorder, 24 (16.4%) switched from MDD to schizophrenia or schizoaffective disorder, and the remaining 54 (37.0%) had other patterns of diagnostic change. Only 47 (58.8%) of 80 participants diagnosed with MDD at baseline retained a mood disorder diagnosis 10 years later (36 or 45.0% had MDD and 11 or 13.8% had bipolar disorder), while 16 (30.8%) of 52 participants who ended the study with MDD were initially misdiagnosed. Those switching from MDD to bipolar disorder had better premorbid adjustment, more first degree relatives with MDD, better functioning, and fewer negative symptoms at baseline, whereas those shifting to the schizophrenia spectrum had a more insidious onset, longer initial hospital stays, worse functioning, and more negative symptoms.
Conclusions
The diagnosis of MDD with psychosis among inpatients showed poor long-term consistency. For clinicians, results indicate that the diagnosis of MDD with psychosis based on a single assessment should be considered provisional.
Major depressive disorder (MDD) with psychotic features is common. Between 15% and 19% of MDD cases in the community report psychotic symptoms.1, 2 MDD with psychosis is associated with worse symptoms, impairment and outcomes than MDD without psychosis.3, 4 There has been a longstanding debate over whether MDD with psychosis simply represents a severity dimension of MDD or constitutes a separate syndrome.5,6
A key piece of evidence in this discussion involves long-term follow-up.7 Many studies have considered long-term outcomes or treatment response,8-27 but few have performed follow-up diagnostic interviews to determine changes, if any, to the original diagnosis. With regard to symptomatology, the National Institute of Mental Health Collaborative Program on the Psychobiology of Depression reported that 10.2% of patients with depression developed mania or hypomania during a 10-year follow-up.28,29 Psychosis among the patients with MDD was highly recurrent across time.30 Two short-term follow-ups, however, raise questions about the stability of the diagnosis itself. The first was the one-year follow-up of the Epidemiologic Catchment Area (ECA) cohort which found that 10.1% of the cohort originally diagnosed with psychotic depression met criteria for schizophrenia one year later, and 3.3% met criteria for bipolar disorder.1 The second was the earlier follow-up of the Suffolk County cohort31 which found that among 103 participants diagnosed with MDD with psychosis at 6-month follow-up, 20 (19.4%) were rediagnosed at two-year follow-up with a non-affective psychosis and 7 (7.8%) with bipolar disorder.
Assessment of diagnostic consistency is important for at least three reasons. First, it speaks to the reliability and validity of the diagnostic criteria.7 Second, it affects interpretation of existing literature. Low diagnostic consistency would mean that previous outcome studies may have included individuals who did not retain the MDD diagnosis, thereby biasing results. Third, frequent shifts in diagnosis have implications for case management and treatment.
The primary goal of the present research therefore was to determine how often the diagnosis of MDD with psychosis was revised and changed to and from another psychotic disorder across 10 years. We considered shifts from MDD to bipolar disorder, from MDD to a schizophrenia spectrum disorder, as well as other patterns of diagnostic change. A final goal was to explore clinical factors associated with different diagnostic shifts.
Data for the study were obtained as part of the Suffolk County Mental Health Project,32 a prospective, epidemiologic study of first admission patients with psychosis. Diagnoses were evaluated at four time points over the 10-year follow-up based on research-based diagnostic reassessments. Reports from the 10-year wave of the project have already considered the long-term consistency of the diagnosis of bipolar disorder33 and schizophrenia34 and the stability of the baseline diagnoses.35 This is the first study to focus on the frequency with which MDD with psychosis was diagnosed and the factors associated with its consistency.
METHOD
Sample and Procedures
The sample was derived from the Suffolk County Mental Health Project cohort, described in detail elsewhere.32, 36-38 Briefly, participants were recruited from 1989-1995 from the 12 psychiatric inpatient facilities of Suffolk County, New York, which included community hospitals, a Veterans Administration hospital, a university hospital and state hospitals. Inclusion criteria were first admission to a psychiatric hospital within six months of enrollment into the study, age 15-60, residency in Suffolk County, capacity to provide written informed consent, and clinical evidence of psychosis. Exclusion criteria included moderate to severe retardation or inability to speak English. Potentially eligible patients were referred to the study by the head nurse or social worker, and 72% of those referred agreed to participate.
A total of 628 participants met eligibility criteria and were enrolled. Among them, 146 participants had at least one follow-up and received a research diagnosis of MDD with psychotic features at one or more assessment points. These 146 participants constitute the sample for the present report.
Participants were interviewed by masters-level mental health professionals (primarily psychiatric social workers) between 1 and 3 weeks after admission. Face-to-face follow-up interviews were conducted 6 months, 2 years and 10 years after enrollment. The first three assessments included the Structured Clinical Interview for DSM-III-R (SCID),39 whereas the 10-year follow-up included the psychosis and mood disorder modules of the SCID for DSM-IV.40 Systematic efforts were made to collect collateral information from medical records and key informants, who were interviewed in person or by phone about the participant's symptoms.
Interviewers received extensive training,32 and inter-rater reliability was maintained by having the project director randomly observe and rate 5-10% of the interviews. Kappa for psychotic symptoms ranged from .81-1.0, while kappa for negative symptoms ranged from .57-1.0. Mood symptom ratings had an average kappa of 0.73.32, 41
Diagnoses were made using best-estimate procedures. Specifically, project psychiatrists formulated a consensus diagnosis on a case-by-case basis after review of all available information, including interviewer ratings and narrative summaries, medical records, information from key informants, and school records. Best-estimate consensus DSM-III-R diagnoses were assigned after the baseline interview, and DSM-IV diagnoses were assigned after the 6-month, 2-year and 10-year assessments.38, 42 At each wave, the SCID interviewer and the consensus diagnosis team were blind to the previous research diagnoses, but they were informed about prior ratings by the interviewer.
Measures
In addition to the SCID, demographic, clinical, and psychosocial functioning data were collected. Basic demographic variables were assessed at baseline. Clinical information included: the Cannon-Spoor Premorbid Adjustment Scale, based on semi-structured items designed to facilitate its completion;43 number of suicide attempts prior to first hospitalization; age of onset of first major depressive episode; age of onset of first psychotic symptoms; DSM-III-R drug and alcohol abuse determined from the baseline SCID; and the Mini-Mental Status Examination (MMSE) administered at baseline.44 Finally, the mode of onset was coded using the 4-level World Health Organization rating scale which ranged from acute without prodromes to insidious onset over a period exceeding one month.45 Medical records were used to determine length of stay of first hospitalization, coded as at/above versus below the median length of stay for the type of hospital (public, community, university) and year when hospitalized. Family history of bipolar disorder, MDD, substance use disorder, and schizophrenia spectrum disorder was obtained from medical records and interviews with respondents and relatives at 6 months and 2 years modeled on Family History-Research Diagnostic Criteria.46
The interviewer-based clinical ratings at baseline and at each subsequent assessment across the 10 years included the Hamilton Rating Scale for Depression (HRSD),47 the Scale for the Assessment of Negative Symptoms (SANS),48 and the Scale for the Assessment of Positive Symptoms (SAPS).49 Two SAPS subscales were analyzed: a positive psychotic symptoms subscale consisting of 16 items on delusions and hallucinations (SAPS-P), and a disorganized symptoms subscale consisting of 13 items on bizarre behavior and formal thought disorders (SAPS–D).41, 49 For each scale, the total score was calculated. In addition, the Global Assessment of Functioning (GAF) was rated by consensus for the best month of the year before baseline and year 10 and for the intervals preceding the earlier follow-ups.
Analysis Plan
We first calculated the percent of participants given the MDD with psychosis diagnosis across the 4 assessment points versus those with other diagnostic patterns. We then looked at the percent of baseline MDD cases who prospectively retained the diagnosis at the last follow-up, as well as the percent of cases who did not receive the diagnosis until after baseline. Alternative diagnoses associated with different diagnostic trajectories were surveyed and described.
Finally, factors associated with diagnostic patterns were explored by stratifying the sample into those consistently diagnosed with MDD (column 1 in Table 1), those who switched from MDD to bipolar disorder (column 2 in Table 1), those who shifted to the schizophrenia spectrum (column 3 in Table 1), and those who followed other patterns of diagnostic change (column 4 in Table 1). Analyses were carried out to determine whether group differences existed for those who had missing assessments or dropped out. Since no differences were detected, descriptions of diagnostic patterns were based on all completed assessments.
Table 1.
Baseline Characteristics of a First Admission Major Depressive Disorder with Psychosis Cohort by 10-year Consistency of Diagnosis (N = 146)
| (1) Consistent MDD (n = 55) | (2) Switch to Bipolar (n = 13) | (3) Switch to Schizophrenia Spectrum (n = 24) | (4) Other Inconsistent Patterns (n = 54) | Significant Differences from Group 1 (t or χ2 p < .05) | |
|---|---|---|---|---|---|
| Demographic Characteristics | |||||
| Age at baseline, M (SD) | 31.7 (12.1) | 28.9 (10.0) | 34.6 (8.4) | 30.2 (9.0) | |
| Female, % (n) | 52.7% (29) | 53.8% (7) | 29.2% (7) | 55.6% (30) | |
| High school graduate, % (n) | 78.2% (43) | 84.6% (11) | 75.0% (18) | 75.9% (41) | |
| African American, % (n) | 7.3% (4) | 0% (0) | 8.3% (2) | 13.0% (7) | |
| Never married, % (n) | 54.5% (30) | 53.8% (7) | 54.2% (13) | 68.5% (37) | |
| Full-time employed or student, % (n) | 43.6% (24) | 61.5% (8) | 37.5% (9) | 42.6% (23) | |
| Baseline Clinical Variables | |||||
| Poor premorbid adjustment, % (n) | 36.4% (20) | 7.7% (1) | 45.8% (11) | 44.4% (24) | 1 > 2 |
| Suicide attempt history, % (n) | 69.1% (38) | 84.6% (11) | 75.0% (18) | 61.1% (33) | |
| Age of onset of MDD, M (SD) | 27.75 (13.25) | 25.85 (11.35) | 30.70 (10.16) | 25.73 (9.01) | |
| Age of onset of psychosis, M (SD) | 30.77 (12.19) | 28.69 (9.99) | 33.38 (8.93) | 29.44 (8.71) | |
| Lifetime drug use disorder,c % (n) | 20.0% (11) | 15.4% (2) | 16.7% (4) | 24.5% (13) | |
| Lifetime alcohol use disorder, % (n) | 43.6% (24) | 50.0% (6) | 50.0% (12) | 43.4% (23) | |
| MMSE, M (SD) | 27.25 (2.74) | 27.61 (1.80) | 27.71 (2.58) | 27.56 (2.48) | |
| Insidious onset, %(n) | 36.4% (20) | 23.1% (3) | 66.7% (16) | 35.2% (19) | 1 < 3 |
| Length of hospitalization (≥median), % (n) | 25.9% (14) | 46.2% (6) | 54.2% (13) | 53.8% (28) | 1 < 3, 4 |
| Family Psychiatric History | |||||
| Bipolar disorder, %(n) | 14.9% (7) | 16.7% (2) | 9.1% (2) | 9.6% (5) | |
| MDD, % (n) | 40.4% (19) | 75.0% (9) | 31.8% (7) | 42.3% (22) | 1 < 2 |
| Substance use disorder, % (n) | 35.2% (19) | 53.8% (7) | 45.8% (11) | 50.0% (27) | |
| Schizophrenia spectrum disorder, % (n) | 11.1% (6) | 7.7% (1) | 12.5% (3) | 9.3% (5) |
Note. Percentage denominators exclude missing data.
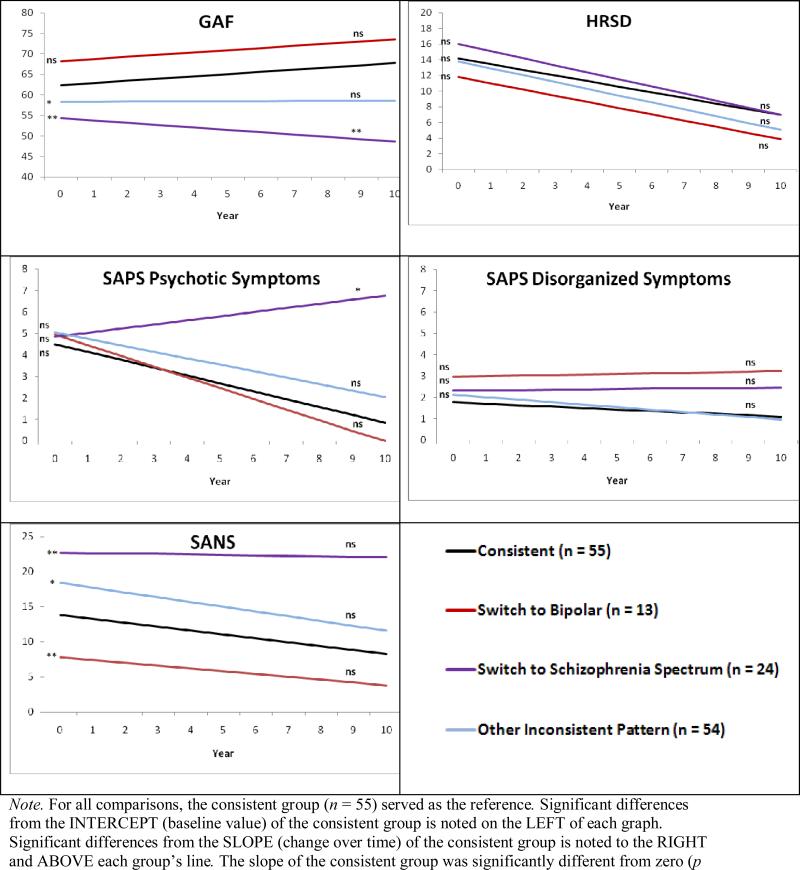
Comparisons of the groups were conducted using chi-squared or independent samples t-tests. Group differences among variables with repeated measurements (GAF, HRSD, SANS, SAPS) were tested using hierarchical linear modeling (HLM).50 For each HLM model, we determined whether the four groups described above had significantly different intercepts (i.e., baseline levels of each variable) or slopes (i.e., the linear change in each variable across the 10 years).
RESULTS
Across the 10-year study, 104 (71.2%) of the 146 participants completed all four assessments, 35 (24.0%) completed three assessments, and 7 (4.8%) completed only two assessments. Most (n=110, 75.3%) were reassessed at year 10. Baseline clinical and demographic characteristics were not significantly associated with retention in this sample. The average age of the study sample was 31.4 (SD=10.3) at baseline. Fifty percent were male, 8.9% were African American, 54.8% had never been married, and 43.8% were employed or in school full time.
Diagnostic Agreement Across 10 Years
Among the 146 participants who ever received an MDD diagnosis, 55 (37.7%) were diagnosed with psychotic depression at each available assessment, 13 (8.9%) switched to bipolar disorder, 24 (16.4%) started with MDD but were rediagnosed later with schizophrenia (n=9) or schizoaffective disorder (n=15), and the remaining 54 (37.0%) had other patterns of diagnostic change. Restricting the sample to participants who completed all four assessment waves (n = 104) reduced the overall consistency from 37.7% to 31.7% (33/104).
Looking at changes prospectively, 80 participants with baseline psychotic depression were reassessed at year 10. Only 36 (45.0%) retained the original MDD diagnosis, 11 (13.8%) ended the study with bipolar disorder, and the remaining 33 (41.3%) had a non-mood disorder diagnosis at year 10. Conversely, of the 52 participants diagnosed with MDD with psychosis at year 10, 36 (69.2%) received this diagnosis at baseline.
Among the 36 baseline MDD respondents who maintained the diagnosis at year 10, 11 had no further mood or psychosis episodes after baseline (and therefore no revision to the baseline diagnosis), 12 had recurrent depressive episodes with psychosis, and 13 had recurrent depressive episodes without psychosis.
Other Diagnostic Trajectories
The diagnostic trajectories of the 54 participants with other inconsistent patterns varied. Twenty-five participants began with a non-MDD diagnosis at baseline, but ended the study with a primary diagnosis of MDD. Their baseline diagnoses included psychosis NOS (n=6), schizophrenia spectrum diagnoses (n=6), other psychotic or substance-related diagnoses (n=6) and cases for which a diagnosis could not be established because of unclear symptoms (n=7). Most of these cases (n=21) were stably diagnosed with MDD within the first two years (i.e., 9 were stably diagnosed with MDD by the 6 month follow-up, 12 by the year 2 follow-up).
Another 12 of these 54 participants had the opposite pattern: they began the study with MDD but then had a shift in primary diagnosis to a non-MDD disorder by their final assessment (i.e., 5 ended with a substance-induced psychosis disorder, 7 ended with another non-MDD disorder). Finally, the remaining 17 participants had a more random pattern of diagnosis, with no clear pattern of switching to or away from psychotic depression.
Predictors of Changes in Diagnosis
Table 1 compares participants diagnosed with psychotic depression across the 10 year study (column 1, n=55) to those whose diagnosis shifted to bipolar disorder (column 2, n=13), those who shifted to a schizophrenia spectrum disorder (column 3, n=24), and those with some other diagnostic patterns (column 4, n=54). As seen in Table 1, the consistent MDD (column 1) and the other groups (columns 2-4) were similar across a range of demographic and clinical characteristics, particularly at baseline when the ability to identify cases who may switch to a different diagnosis is most critical since treatment is being initiated.
A few variables, however, distinguished the groups. Participants who eventually switched into the schizophrenia spectrum (column 3) were more likely to have an insidious onset of symptoms and longer initial hospital stays than those consistently diagnosed with MDD. Participants who switched into a bipolar diagnosis (columns 2) had better premorbid adjustment at baseline relative to those who retained the MDD diagnosis (column 1). They were also more likely to have a family history of MDD.
Comparisons of the 10-year trajectories of the consistent group to other patterns were examined using HLM as shown in Figure 1. As seen there, participants who switched into the schizophrenia spectrum had worse functioning (GAF) at baseline relative to those with a consistent MDD diagnosis. Over time, their functioning declined even further relative to the other groups as reflected in the negative GAF slope. Negative symptoms (SANS) were elevated in this group initially and remained high and stable over time. Meanwhile, this group showed an increase over time in severity of psychotic symptoms (SAPS). In contrast, those with a consistent psychotic depression diagnosis or who switched to a bipolar diagnosis had better functioning over time, including fewer positive and negative symptoms across the 10 years.
Figure 1.
Hierarchical linear models predicting functioning and symptoms by group (with the consistent group in black serving as the reference for all comparisons) (N = 146)
DISCUSSION
The diagnosis of MDD with psychosis had low consistency in this first-admission sample. Fewer than half of those with the disorder at baseline received an MDD diagnosis 10 years later. In addition, about 1 in 3 respondents (30.8%) who ended the study with an MDD diagnosis did not receive it until months or years after their baseline assessment.
The finding of low consistency is seemingly at odds with several previous reports. One large study found psychotic depression to be highly recurrent, with a risk of new depressive episodes with psychosis being common in patients with this MDD subtype.30 Two smaller studies with shorter follow-up periods found similar high rates of recurrence, one showing that over 80% of patients with delusional depression relapsed into delusional depression,51 and another showing that 92% of cases admitted for psychotic depression had a recurrent admission for the same subtype.52 Such discrepancies from previous reports likely reflect differences in methods as well as sample characteristics. Specifically, recruitment into the present study was meant to broadly reflect first psychosis admissions, whereas previous studies more selectively screened for cases of depression. Moreover, the present sample was diagnosed early in the course of their disorder and followed for longer than in previous reports. Hence, an earlier diagnosis, when symptoms are first emerging and are more ambiguous, as well as longer follow-ups involving full re-evaluation of initial diagnoses may have provided more opportunity for shifts in diagnosis and lower rates of diagnostic consistency than seen previously.
With respect to specific types of diagnostic change, a large number of participants classified as having MDD with psychosis at baseline were later rediagnosed with a schizophrenia spectrum disorder as their primary study diagnosis. In fact, this happened twice as often as shifts from MDD to bipolar disorder. There have been major efforts to increase recognition of bipolar disorder among patients presenting with depression,53 yet results from the present work make clear that, at least among inpatients with psychosis, there is an equal and perhaps greater need to better screen for schizophrenia spectrum disorders. To this end, a few factors distinguished the two trajectories at baseline. Those later rediagnosed with a schizophrenia spectrum disorder had worse functioning, more negative symptoms, longer initial hospital stays and more insidious onset of symptoms, whereas those later diagnosed with bipolar disorder had fewer negative symptoms, greater family history of MDD, and better premorbid functioning. Such differences early in the course of patients with psychosis may help alert clinicians to the possibility of a diagnostic change.
Finally, a further common trajectory was for a participant to have a delay in receiving the MDD diagnosis, consistent with previous reports showing that MDD with psychosis is a commonly missed diagnosis. For example, Rothschild and colleagues found that psychotic depression in inpatient and emergency academic centers was missed almost 1 out of 3 times,54 a rate similar to what was seen in the present study.
Findings must be viewed in the context of study limitations. The sample consisted of patients with illness severe enough to warrant hospitalization. The results thus cannot be generalized to outpatient samples or to depression samples without psychosis. With respect to inpatient settings, however, the findings are likely to be generalizable since recruitment occurred from a broad spectrum of inpatient programs as opposed to specialty clinics or academic centers. Moreover, given that respondents were recruited primarily at first admission, the sampling design avoided the problem of mixing recent onset and chronic cases that are common in cohorts of consecutively hospitalized patients. A second limitation was that the SCID interviewers and project psychiatrists were not blind to previous information other than prior research diagnoses. The latter methodological issue, however, should have led to more rather than less consistency of diagnoses across assessments. Moreover, the present results were based on a best estimate consensus procedure. Each assessment included a semi-structured diagnostic interview, often considered the gold standard for assessing psychiatric disorders, but the psychiatrists also considered information from medical records as well as reports of significant others. This manner of classification increases confidence in the validity and reliability of the diagnosis, at least more than what would be the case had the diagnosis been based on a single clinical interview. A third potential limitation was that DSM-III-R and DSM-IV criteria differed somewhat, which may have contributed to observed inconsistency. Changes in the criteria, however, were minor and would not account for the observed level of instability.
Despite these limitations, this report provides previously unavailable information about the long-term consistency of MDD with psychotic features. The findings have theoretical implications regarding the MDD with psychosis diagnosis, as well as practical implications for clinicians treating patients with the disorder.
On a theoretical level, the findings raise questions about the validity of the diagnosis. A key component in establishing the validity of a diagnosis is follow-up.7 The present results were striking in the degree to which diagnoses shifted across time, indicating that cross-sectional assessment using MDD criteria will not by itself identify a homogenous group. Even among those consistently diagnosed with MDD, there was variability in the degree to which psychosis was present or not. Refinement of MDD with psychosis criteria to consider the nature of onset, the level of functioning, or the severity of negative symptoms, all significant predictors of diagnostic change in the present report, may be warranted for patients with psychotic symptoms. Until such criteria refinement occurs, future revisions of the DSM may wish to emphasize the provisional nature of an MDD with psychosis diagnosis.
On a practical level, the present results should serve as a caution for physicians treating patients diagnosed with MDD with psychosis. Even when using state-of-the-art assessments, including integration of information from diverse sources, it is likely that the diagnosis will need to be revised as the illness evolves.
Acknowledgments
Support for this study was provided by a grant from the National Institute of Mental Health (44801). We gratefully acknowledge the support of the participants and mental health community of Suffolk County for graciously contributing their time and energy to this project. We are also indebted to the interviewers for their diligent and caring assessments, and to the following psychiatrists who contributed to the consensus diagnoses: Alan Brown, Eduardo Constantino, Thomas Craig, Frank Dowling, Shmuel Fennig, Silvana Fennig, Laura Fochtmann, Beatrice Kovasznay, Alan Miller, Ramin Mojtabai, Bushra Naz, Joan Rubinstein, Carlos Pato, Michele Pato, Ranganathan Ram, Charles Rich, and Ezra Susser. Special thanks to Janet Lavelle and Al Hamdy for coordinating the study.
REFERENCES
- 1.Johnson J, Horwath E, Weissman MM. The validity of major depression with psychotic features based on a community study. Arch Gen Psychiatry. 1991;48(12):1075–1081. doi: 10.1001/archpsyc.1991.01810360039006. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM, Schatzberg AF. Prevalence of depressive episodes with psychotic features in the general population. Am J Psychiatry. 2002;159(11):1855–1861. doi: 10.1176/appi.ajp.159.11.1855. [DOI] [PubMed] [Google Scholar]
- 3.Schatzberg AF. New approaches to managing psychotic depression. J Clin Psychiatry. 2003;64(Suppl 1):19–23. [PubMed] [Google Scholar]
- 4.Gaudiano BA, Young D, Chelminski I, et al. Depressive symptom profiles and severity patterns in outpatients with psychotic vs nonpsychotic major depression. Compr Psychiatry. 2008;49(5):421–429. doi: 10.1016/j.comppsych.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schatzberg AF, Rothschild AJ. Psychotic (delusional) major depression: should it be included as a distinct syndrome in DSM-IV? Am J Psychiatry. 1992;149(6):733–745. doi: 10.1176/ajp.149.6.733. [DOI] [PubMed] [Google Scholar]
- 6.Winokur G, Monahan P, Coryell W, et al. Schizophrenia and affective disorder--distinct entities or continuum?: an analysis based on a prospective 6-year follow-up. Compr Psychiatry. 1996;37(2):77–87. doi: 10.1016/s0010-440x(96)90566-0. [DOI] [PubMed] [Google Scholar]
- 7.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 8.Coryell W, Endicott J, Keller M. The importance of psychotic features to major depression: course and outcome during a 2-year follow-up. Acta Psychiatr Scand. 1987;75(1):78–85. doi: 10.1111/j.1600-0447.1987.tb02755.x. [DOI] [PubMed] [Google Scholar]
- 9.Coryell W, Keller M, Lavori P, et al. Affective syndromes, psychotic features, and prognosis. II. Mania. Arch Gen Psychiatry. 1990;47(7):658–662. doi: 10.1001/archpsyc.1990.01810190058008. [DOI] [PubMed] [Google Scholar]
- 10.Coryell W, Tsuang MT. Primary unipolar depression and the prognostic importance of delusions. Arch Gen Psychiatry. 1982;39(10):1181–1184. doi: 10.1001/archpsyc.1982.04290100051008. [DOI] [PubMed] [Google Scholar]
- 11.Coryell W, Tsuang MT. Major depression with mood-congruent or mood-incongruent psychotic features: outcome after 40 years. Am J Psychiatry. 1985;142(4):479–482. doi: 10.1176/ajp.142.4.479. [DOI] [PubMed] [Google Scholar]
- 12.Coryell W, Zimmerman M, Pfohl B. Outcome at discharge and six months in major depression. The significance of psychotic features. J Nerv Ment Dis. 1986;174(2):92–96. doi: 10.1097/00005053-198602000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Coryell W, Leon A, Winokur G, et al. Importance of psychotic features to long-term course in major depressive disorder. Am J Psychiatry. 1996;153(4):483–489. doi: 10.1176/ajp.153.4.483. [DOI] [PubMed] [Google Scholar]
- 14.Duggan CF, Lee AS, Murray RM. Do different subtypes of hospitalized depressives have different long-term outcomes? Arch Gen Psychiatry. 1991;48(4):308–312. doi: 10.1001/archpsyc.1991.01810280024003. [DOI] [PubMed] [Google Scholar]
- 15.Flint AJ, Rifat SL. Two-year outcome of psychotic depression in late life. Am J Psychiatry. 1998;155(2):178–183. doi: 10.1176/ajp.155.2.178. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg JF, Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J Affect Disord. 2004;81(2):123–131. doi: 10.1016/S0165-0327(03)00161-7. [DOI] [PubMed] [Google Scholar]
- 17.Gaudiano BA, Beevers CG, Miller IW. Differential response to combined treatment in patients with psychotic versus nonpsychotic major depression. J Nerv Ment Dis. 2005;193(9):625–628. doi: 10.1097/01.nmd.0000177791.33649.69. [DOI] [PubMed] [Google Scholar]
- 18.Kettering RL, Harrow M, Grossman L, et al. The prognostic relevance of delusions in depression: a follow-up study. Am J Psychiatry. 1987;144(9):1154–1160. doi: 10.1176/ajp.144.9.1154. [DOI] [PubMed] [Google Scholar]
- 19.Lykouras L, Christodoulou GN, Malliaras D, et al. The prognostic importance of delusions in depression: a 6-year prospective follow-up study. J Affect Disord. 1994;32(4):233–238. doi: 10.1016/0165-0327(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 20.Lykouras E, Malliaras D, Christodoulou GN, et al. Delusional depression: phenomenology and response to treatment. A prospective study. Acta Psychiatr Scand. 1986;73(3):324–329. doi: 10.1111/j.1600-0447.1986.tb02692.x. [DOI] [PubMed] [Google Scholar]
- 21.Maj M, Pirozzi R, Di Caprio EL. Major depression with mood-congruent psychotic features: a distinct diagnostic entity or a more severe subtype of depression? Acta Psychiatr Scand. 1990;82(6):439–444. doi: 10.1111/j.1600-0447.1990.tb03075.x. [DOI] [PubMed] [Google Scholar]
- 22.Maj M, Pirozzi R, Magliano L, et al. Phenomenology and prognostic significance of delusions in major depressive disorder: a 10-year prospective follow-up study. J Clin Psychiatry. 2007;68(9):1411–1417. doi: 10.4088/jcp.v68n0913. [DOI] [PubMed] [Google Scholar]
- 23.Murphy E. The prognosis of major depression in old age. The Br J Psychiatry. 1983;142:111–119. doi: 10.1192/bjp.142.2.111. [DOI] [PubMed] [Google Scholar]
- 24.Parker G, Hadzi-Pavlovic D, Hickie I, et al. Distinguishing psychotic and non-psychotic melancholia. J Affect Disord. 1991;22(3):135–148. doi: 10.1016/0165-0327(91)90047-v. [DOI] [PubMed] [Google Scholar]
- 25.Robinson DG, Spiker DG. Delusional depression. A one year follow-up. J Affect Disord. 1985;9(1):79–83. doi: 10.1016/0165-0327(85)90013-8. [DOI] [PubMed] [Google Scholar]
- 26.Rothschild AJ, Bates KS, Boehringer KL, et al. Olanzapine response in psychotic depression. J Clin Psychiatry. 1999;60(2):116–118. doi: 10.4088/jcp.v60n0208. [DOI] [PubMed] [Google Scholar]
- 27.Rothschild AJ, Samson JA, Bessette MP, et al. Efficacy of the combination of fluoxetine and perphenazine in the treatment of psychotic depression. J Clin Psychiatry. 1993;54(9):338–342. [PubMed] [Google Scholar]
- 28.Coryell W, Endicott J, Maser JD, et al. Long-term stability of polarity distinctions in the affective disorders. Am J Psychiatry. 1995;152(3):385–390. doi: 10.1176/ajp.152.3.385. [DOI] [PubMed] [Google Scholar]
- 29.Coryell W, Leon A, Winokur G, et al. Importance of psychotic features to long-term course in major depressive disorder. Am J Psychiatry. 1996;153(4):483–489. doi: 10.1176/ajp.153.4.483. [DOI] [PubMed] [Google Scholar]
- 30.Coryell W, Winokur G, Shea T, et al. The long-term stability of depressive subtypes. Am J Psychiatry. 1994;151(2):199–204. doi: 10.1176/ajp.151.2.199. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz JE, Fennig S, Tanenberg-Karant M, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57(6):593–600. doi: 10.1001/archpsyc.57.6.593. [DOI] [PubMed] [Google Scholar]
- 32.Bromet EJ, Schwartz JE, Fennig S, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18(2):243–255. doi: 10.1093/schbul/18.2.243. [DOI] [PubMed] [Google Scholar]
- 33.Ruggero CJ, Carlson GA, Kotov R, et al. Ten-year diagnostic consistency of bipolar disorder in a first-admission sample. Bipolar Disord. 2010;12(1):21–31. doi: 10.1111/j.1399-5618.2009.00777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bromet EJ, Naz B, Fochtmann LJ, et al. Long-term diagnostic stability and outcome in recent first-episode cohort studies of schizophrenia. Schizophr Bull. 2005;31(3):639–649. doi: 10.1093/schbul/sbi030. [DOI] [PubMed] [Google Scholar]
- 35.Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic stability revisited: shifts during the decade following first-admission for psychosis. Am J Psychiatry. doi: 10.1176/appi.ajp.2011.11010048. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bromet EJ, Fennig S. Epidemiology and natural history of schizophrenia. Biol Psychiatry. 1999;46(7):871–881. doi: 10.1016/s0006-3223(99)00153-5. [DOI] [PubMed] [Google Scholar]
- 37.Mojtabai R, Susser ES, Bromet EJ. Clinical characteristics, 4-year course, and DSM-IV classification of patients with nonaffective acute remitting psychosis. Am J Psychiatry. 2003;160(12):2108–2115. doi: 10.1176/appi.ajp.160.12.2108. [DOI] [PubMed] [Google Scholar]
- 38.Schwartz JE, Fennig S, Tanenberg-Karant M, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57(6):593–600. doi: 10.1001/archpsyc.57.6.593. [DOI] [PubMed] [Google Scholar]
- 39.Spitzer RL, Williams JB, Gibbon M, et al. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 40.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient edition (SCID-I/P, version 2.0) 1995.
- 41.Kotov R, Guey LT, Bromet EJ, et al. Smoking in schizophrenia: diagnostic specificity, symptom correlates, and illness severity. Schizophr Bull. 2010;36(1):173–181. doi: 10.1093/schbul/sbn066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fennig S, Kovasznay B, Rich C, et al. Six-month stability of psychiatric diagnoses in first-admission patients with psychosis. Am J Psychiatry. 1994;151(8):1200–1208. doi: 10.1176/ajp.151.8.1200. [DOI] [PubMed] [Google Scholar]
- 43.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8(3):470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 44.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 45.Hoopper K, Harrison C, Wanderlin JA. An overview of course and outcome in the ISoS. In: Hopper K, Harrison G, Janca A, et al., editors. Recovery from Schizophrenia: an international perspective. Oxford univ press; Oxford: 2007. pp. 23–38. [Google Scholar]
- 46.Endicott J, Andreasen NC, Spitzer RL. Family History-Research Diagnostic Criteria. 1985.
- 47.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br J Psychiatry Suppl. 1989;(7):49–58. (7) [PubMed] [Google Scholar]
- 49.Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS) The University of Iowa; Iowa City: 1984. [Google Scholar]
- 50.Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods. 2nd ed. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- 51.Aronson TA, Shukla S, Gujavarty K, et al. Relapse in delusional depression: a retrospective study of the course of treatment. Compr Psychiatry. 1988;29(1):12–21. doi: 10.1016/0010-440x(88)90032-6. [DOI] [PubMed] [Google Scholar]
- 52.Helms PM, Smith RE. Recurrent psychotic depression. Evidence of diagnostic stability. J Affect Disord. 1983;5(1):51–54. doi: 10.1016/0165-0327(83)90036-8. [DOI] [PubMed] [Google Scholar]
- 53.Hirschfeld RM, Vornik LA. Recognition and diagnosis of bipolar disorder. J Clin Psychiatry. 2004;65(Suppl 15):5–9. [PubMed] [Google Scholar]
- 54.Rothschild AJ, Winer J, Flint AJ, et al. Missed diagnosis of psychotic depression at 4 academic medical centers. J Clin Psychiatry. 2008;69(8):1293–1296. doi: 10.4088/jcp.v69n0813. [DOI] [PubMed] [Google Scholar]