Abstract
Prevalent hypertension in National Health and Nutrition Examination Surveys (NHANES) is traditionally defined as blood pressure (BP) ≥140 mm Hg systolic and/or ≥90 diastolic and/or currently taking antihypertensive medications. When estimating prevalent hypertension, American Heart Association (AHA) statistical updates include the traditional definition of hypertension (tHTN) and untreated individuals with nonhypertensive BP told twice that they were hypertensive (nontraditional [ntHTN]). The characteristics of ntHTN and their impact on the clinical epidemiology of hypertension and Healthy People prevention and control goals are undefined. NHANES 1999–2002, 2003–2006, and 2007–2010 were analyzed. The ntHTN group was younger and had less diabetes and lower BP than the tHTN group but higher BP than the normotensive group. When classifying ntHTN as hypertensive, prevalent hypertension increased approximately 3% and control 5% to 6% across NHANES periods. In 2007–2010, the Healthy People 2010 goal of controlling BP in 50% of all hypertensive patientss was attained when ntHTN was classified as hypertension (56.5% [95% confidence interval (CI), 54.2–58.7]) and nonhypertension (51.8% [95% CI, 49.6–53.9]). When including ntHTN in prevalent hypertension estimates, the Healthy People 2020 goal of controlling BP in 60% of hypertensive patients becomes more attainable, whereas reducing prevalent hypertension to 26.9% (31.8% [95% CI, 30.5–33.1]) vs 28.7% [95% CI, 27.5–30.0]) becomes more challenging.
Hypertension is a prevalent risk factor for cardiovascular and chronic kidney disease as well as premature disability and death.1 US Healthy People goals for hypertension prevention and control further attest to the public health importance of this diagnosis.2, 3 Temporal trends in the prevalence, awareness, treatment, and control of hypertension are of major public health importance and an indirect measure of the effectiveness of healthcare policy and delivery in attaining key public health objectives.
National Health and Nutrition Examination Survey (NHANES) data for 1988–1994 and 1999–2008 demonstrated that hypertension awareness, treatment, and control all increased significantly over time.4 Hypertension control to blood pressure (BP) <140/<90 mm Hg rose from an estimated 23.7% of all hypertensive patients in 1988 to 1994 to 50.1% in 2007 to 2008,4 which met the Healthy People 2010 goal of controlling BP in 50% of all hypertensive patients.2 In contrast, prevalent hypertension rose from 25.4% in 1988 to 1994 to 29.0% in 2007 to 2008, which rendered the goal of reducing prevalent hypertension to 16.0% by 2010 essentially unattainable.
Healthy People 2020 goals include reducing prevalent hypertension to 26.9% or roughly 10% from current levels.3 Moreover, the hypertension control goal for all hypertensive patients, which includes unaware and untreated patients, was raised from 50% in 2010 to 60% in 2020. Definitions of hypertension prevalence and control are of fundamental importance in assessing progress toward Healthy People BP objectives.
Traditionally, prevalent hypertension (tHTN) in NHANES is defined as systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg and/or by patients affirming that they are currently taking prescribed medication to lower BP.4, 5, 6, 7 NHANES reports from the US Department of Health and Human Services, National Institutes of Health, Centers for Disease Control, and the American Heart Association annual statistical update8, 9 also included as hypertension untreated individuals with nonhypertensive BP told twice by a physician that they had hypertension, ie, nontraditional hypertension (ntHTN).
Clinical characteristics of individuals with ntHTN and their impact on the clinical epidemiology of hypertension in the United States and Healthy People goals have not been systematically quantified. Thus, the 3 main objectives of this report are to: (1) describe clinical characteristics of ntHTN and to define their impact on the (2) clinical epidemiology of hypertension and (3) Healthy People goals. The report also assesses the mpact of defining hypertension control as <140/<90 mm Hg for all patients rather than <140/<90 mm Hg in patients without and <130/<80 mm Hg in patients with diabetes and/or chronic kidney disease.
Methods
NHANES 1999–2010 were conducted by the Centers for Disease Control and Prevention National Center for Health Statistics (NCHS).7, 10 NHANES volunteers were selected using stratified, multistage probability sampling of the noninstitutionalized US population. All adults provided written informed consent approved by the NCHS institutional/ethics review board.7
Definitions
Race/ethnicity was determined by self report and separated into non‐Hispanic white (white), non‐Hispanic black (black), Hispanic ethnicity of any race as described.4, 5 The numbers and percentages of individuals of other races including American Indian, Alaskan Native, Asian or Pacific Islander and other race not specified were relatively small and categorized as ‘Other.’
Height and weight were measured without shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
BP was measured with the same methods across NHANES 1999–2010.4, 11 In brief, trained physicians measured BP using a mercury sphygmomanometer and appropriately sized arm cuff on patients after 5 minutes of seated rest. Individuals without recorded BP values were excluded. Mean systolic and diastolic BPs were determined as recommended in NHANES reporting guidelines. The majority of patients had 3 recorded BP values, and the mean of the second and third values was used in analyses. For individuals with two recorded BP values, the second BP alone was used. For individuals with one BP measurement, the single value was used. In all survey periods, >90% of patients had ≥2 BP measurements.
Hypertension was defined as mean systolic BP ≥140 mm Hg and/or mean diastolic BP ≥90 mm Hg and/or a positive response to the question “Are you currently taking medication to lower your BP?”4, 5, 6, 7, 11 Untreated individuals with BP <140/<90 mm Hg who reportedly were told twice by a physician that they were hypertensive (ntHTN) were also designated as hypertensive in some analyses.8, 9
Awareness of hypertension was determined by hypertensive patients answering “yes” to the question, “Have you ever been told by a doctor or other healthcare professional that you had hypertension, also called high BP?”4, 5, 6, 7
Treatment of hypertension was defined by patients responding “yes” to the question, “Because of your hypertension/high BP, are you now taking prescribed medicine?”4, 5, 6, 7, 11
Control of hypertension was defined as BP <140/<90 mm Hg across all survey periods, although the BP goals for high‐risk subgroups including diabetics was lower for 1999 to 2010.1, 12 Recent evidence does not clearly support a goal systolic BP <140 mm Hg for diabetic patients or those with nonproteinuric hypertensive renal disease.13, 14 For these reasons and to facilitate comparisons across the 3 NHANES study periods, this report focuses primarily on goal BP <140/<90 mm Hg for all hypertensive patients. To address the secondary study objective, differences in BP control rates between the goal of <140/<90 mm Hg for all patients and <140/<90 mm Hg for patients without and <130/<80 mm Hg for patients with diabetes and/or chronic kidney disease (CKD) are reported.
CKD was defined as an estimated glomerular filtration rate (eGFR) <60 mL/1.7 m2/min and/or urine albumin:creatinine ≥300 mg/g.15, 16 Serum creatinine values were adjusted to facilitate comparisons of eGFR across surveys.17
Diabetes mellitus was defined by a positive response to “Have you ever been told by a doctor that you have diabetes?” and/or “Are you now taking insulin?” and/or “Are you now taking diabetes pills to lower your blood sugar?” The definition did not include patients with only fasting plasma glucose ≥126 mg/dL, ie, “undiagnosed diabetes.”18, 19
Data Analysis
The NHANES Analytic and Reporting Guidelines were followed. SAS callable SUDAAN version 10.0.1 (SAS Institute, Cary, NC) was used for all analyses to account for the complex NHANES sampling design. Standard errors were estimated using Taylor series linearization. To compare prevalence, awareness, treatment, and control rates across surveys, age‐adjustment to the US 2000 census data was performed on all NHANES periods in SUDAAN DESCRIPT procedure. For Tables 1 and 2, the CROSSTAB procedure was used for categorical variables and the DESCRIPT procedure was used for continuous variables. Pair‐wise comparisons between the 3 NHANES periods were conducted using t tests of weighted means and z tests of weighted proportions with the weight equal to the standard errors estimated from the above‐mentioned SUDAAN procedures. Since multiple statistical comparisons were performed among the 3 NHANES time periods, 2‐sided P values <.01 were accepted as statistically significant. P values <.05 were accepted as significant when two groups were compared.
Table 1.
Selected Characteristics of All Adult Patients Who Had BP Measured in 3 NHANES Time Periods
| NHANES | 1999–2002 | 2003–2006 | 2007–2010 |
|---|---|---|---|
| No. | 10,006 | 9930 | 11,723 |
| Age, y | |||
| Mean | 44.1 (43.5–44.8) | 45.2 (44.2–46.2) | 46.0 (45.4–46.7) a |
| Sex | |||
| Male, % | 48.4 (47.4–49.3) | 48.6 (47.6–49.5) | 48.5 (47.7–49.3) |
| Female, % | 51.6 (50.7–52.6) | 51.4 (50.5–52.4) | 51.5 (50.7–52.3) |
| Race | |||
| White, % | 71.0 (67.2–74.6) | 72.2 (67.6–76.4) | 68.8 (63.5–73.6) |
| Black, % | 10.5 (8.4–13.2) | 11.1 (8.7–14.1) | 11.3 (9.3, 13.7) |
| Hispanic, % | 13.8 (10.2–18.4) | 11.4 (9.0–14.5) | 13.7 (10.4–17.8) |
| Other race, % | 4.6 (3.5–6.1) | 5.2 (4.3–6.2) | 6.2 (5.0–7.7) |
| SBP, mm Hg | |||
| All patients | 122.1 (121.3–123.0) | 121.9 (121.2–122.6) a | 120.4 (119.8–121.0)‡ |
| DBP, mm Hg | |||
| All patients | 72.3 (71.7–72.9) a | 70.5 (70.0–71.0) | 69.9 (69.1–70.7) a |
| ≥160/≥100, % | 5.3 (4.6–6.1) | 4.7 (4.2–5.3) a | 3.2 (2.9–3.5) a |
| 140–159/90–99, % | 12.7 (11.8–13.6) | 12.0 (10.9–13.1) | 11.2 (10.4–12.0) b |
| 120–139/80–89, % | 36.3 (35.0–37.6) | 36.1 (34.8–37.5) | 35.0 (33.5–36.5) |
| <120/<80, % | 45.7 (43.8–47.7) | 47.2 (45.4–49.0)† | 50.7 (48.9–52.4)‡ |
| SBP, mm Hg | |||
| Nonhypertensive | 114.8 (114.2–115.5) | 115.1 (114.6–115.5) | 114.5 (113.9–115.0) |
| DBP, mm Hg | |||
| Nonhypertensive | 70.4 (69.9–70.9) a | 68.6 (68.2–69.0) | 68.6 (67.9–69.4) a |
| 120–139/80–89, % | 41.4 (39.5–43.4) | 39.5 (37.4–41.6) | 36.9 (35.0–38.9) a |
| <120/<80, % | 58.6 (56.6–60.5) | 60.5 (58.4–62.6 | 63.1 (61.1–65.0) a |
| BMI, kg/m2 | |||
| Mean | 27.8 (27.6–28.1) | 28.2 (27.9–28.5) | 28.5 (28.3–28.7) a |
| <25.0 | 36.5 (34.6–38.3) | 34.3 (32.5–36.1) | 32.3 (30.7–33.9) a |
| 25.0–29.9 | 34.0 (32.4–35.7) | 33.3 (31.9–34.8) | 33.4 (32.2–34.7) |
| ≥30, % | 29.5 (27.7–31.4) | 32.4 (30.4–34.4) | 34.3 (32.9–35.8) a |
| Diabetes, % | 6.2 (5.5–6.9) b | 7.3 (6.6–8.1) b | 8.9 (8.1–9.7) a |
| CKD, % | 5.6 (5.1–6.1) | 6.0 (5.3–6.8) | 6.1 (5.5–6.8) |
Abbreviations: BMI, body mass index; CKD, chronic kidney disease (estimated GFR <60 mL/1.7 m2/min); DBP, diastolic blood pressure; NHANES, National Health and Nutrition Examination Surveys; SBP, systolic blood pressure. Symbols in column (a) 1999–2002 indicate P value vs 2003–2006, (b) 2003–2006 vs 2007–2010, and (c) 2007–2010 vs 1999–2002. a P<.001. b P<.01.
Table 2.
Characteristics of Traditional and Untreated Twice‐Told Hypertensives With Nonhypertensive BP in 3 NHANES Time Periods
| NHANES Time Period | 1999–2002 | 2003–2006 | 2007–2010 | |||
|---|---|---|---|---|---|---|
| Group | tHTN | ntHTN | tHTN | ntHTN | tHTN | ntHTN |
| No. (%) | 3150 (26.9) | 262 (2.8) | 3107 (29.0) | 299 (3.1) | 4150 (28.7) | 355 (2.9) |
| Age, y | 58.4 (57.3–59.5) | 41.9 (40.1–43.8) | 58.9 (57.5–60.3) | 43.1 (41.0–45.1) | 59.4 (58.8–60.0) | 43.6 (41.8–45.5) |
| Sex | ||||||
| Male, % | 46.4 (44.3–48.6) | 49.0 (41.3–56.7) | 48.9 (46.9–51) | 49.9 (40.7–59.1) | 48.3 (46.6–49.9) | 46.7 (40.3–53.1) |
| Female, % | 53.6 (51.4–55.7) | 51.0 (43.3–58.7) | 51.1 (49.0–53.1) | 50.1 (40.9–59.3) | 51.7 (50.1–53.4) | 53.3 (46.9–59.7) |
| Race | ||||||
| White, % | 73.1 (68.5–77.2) | 72.4 (65.5–78.4) | 74.9 (69.6–79.6) | 76.4 (70.0–81.8) | 72.3 (66.4–77.6) | 66.3 (58.7–73.1) |
| Black, % | 13.3 (10–17.5) | 10.9 (7.1–16.4) | 13.7 (10.5–17.7) | 8.5 (5.6–12.6) | 14.3 (11.1–18.1) | 14.1 (10.5–18.7) |
| Hispanic, % | 9.7 (6.2–14.9) | 11.5 (8.2–15.9) | 6.8 (4.5–10.0) | 10.1 (7.1–14.0) | 8.8 (6.1–12.6) | 11.8 (8.2–16.8) |
| Other race, % | 3.9 (2.5–5.8) | 5.3 (2.4–11.2) | 4.6 (3.5–6.0) | 5.1 (2.6–9.5) | 4.6 (3.3–6.3) | 7.7 (4.8–12.2) |
| SBP, mm Hg | 141.9 a (140.7–143.2) | 122.3 (120.1–124.4) | 138.6 a (137.6–139.6) | 120.6 (118.8–122.5) | 134.4 a (133.7–135.2) | 120.6 (119.2–121.9) |
| DBP, mm Hg | 77.5 a (76.6–78.4) | 74.1 (72.5–75.6) | 75.0 (74.0–76.1) b | 71.7 (70.0–73.4) | 72.9 (71.9–73.9) a | 71.7 (70.3–73.0) |
| BP category Stage 2 | ||||||
| ≥160/≥100, % | 19.7 (17.3–22.3) b | 16.1 (14.4–18.1) a | 10.6 (9.5–11.8) a | |||
| Stage 1 | ||||||
| 140–159/90–99, % | 47.1 (45.1–49.0) a | 41.1 (38.4–43.9) | 37.4 (35.2–39.6) a | |||
| Pre‐HTN | ||||||
| 120–139/80–89, % | 22.5 (20.3–24.9) a | 69.9 (63.0–76.0) | 27.9 (25.8–30.1) | 61.7 (54.5–68.3) | 30.5 (28.7–32.5) a | 63.0 (57.1–68.6) |
| Normal | ||||||
| <120/<80, % | 10.7 (9.3–12.3) a | 30.1 (24.0–37.0) | 14.8 (13.2–16.6) a | 38.3 (31.7–45.5) | 21.5 (19.8–23.2) a | 37.0 (31.4–42.9) |
| BMI, kg/m2 | ||||||
| Mean | 30.1 (29.7–30.5) | 29.8 (28.8–30.9) | 30.3 (29.9–30.6) b | 29.1 (28.1–30.1) | 30.9 (30.7–31.2) a | 30.3 (29.4–31.3) |
| <25, % | 21.2 (19.4–23.2) | 25.7 (19.9–32.5) | 21.0 (19.2–22.9) | 32.9 (26.8–39.7) | 19.0 (17.3–20.8) | 20.5 (14.7–27.7) |
| ≥30, % | 43.5 (41.2–46.0) | 40.9 (33.4–48.8) | 44.8 (42.4–47.3) b | 38.6 (30.7–47.1) | 48.8 (46.8–50.8) a | 47.2 (40.7–53.8) |
| Diabetes, % | 14.0 (12.8–15.3) b | 8.1 (5.2–12.3) | 16.6 (15.4–17.7) a | 9.1 (5.8–14.2) | 20.5 (18.6–22.5) a | 6.6 (4.6–9.4) |
| CKD, % | 15.1 (13.7–16.6) | 6.1 (2.7–13.3) | 15.1 (13.1–17.3) | 4.8 (2.6–8.5) | 15.0 (13.8–16.4) | 3.6 (1.9–6.7) |
Abbreviations: CKD, chronic kidney disease; BMI, body mass index; DBP, diastolic blood pressure; HTN, hypertension; ntHTN, nontraditional hypertensive; NHANES, National Health and Nutrition Examination Surveys; SBP, systolic blood pressure; tHTN, traditional hypertensive (defined by blood pressure [BP] ≥140/≥90 mm Hg or nonhypertensive BP and self‐report of prescribed medication treatment for hypertension); u2tHT‐NHT, untreated, twice‐told patients with nonhypertensive BP. The symbols in the column 1999–2002 indicate the P value for comparison with 2003–2006 within tHTN or u2tHT‐NHT group. The symbols in the column 2003–2006 indicate the P value for comparison with 2007–2010 within tHTN or u2tHT‐NHT group. The symbols in the column 2007–2010 indicate the P value for comparison with 1999–2002 within tHTN or u2tHT‐NHT group. Bold values in the ntHTN column indicate significant difference vs tHTN in same time period by nonoverlapping 95% confidence limits. a P<.001. b P<.01.
Results
The stepwise process by which the study sample of 31,659 adults was derived from the NHANES 1999–2010 database is depicted in Figure 1. Selected characteristics of all adults included in the NHANES 1999–2002, 2003–2006, and 2007–2010 time periods are provided in Table 1. Mean age increased by nearly 2 years across surveys but remained in the mid‐40s. Systolic and diastolic BP declined over time in all adults combined, whereas only diastolic BP declined in nonhypertensive individuals. The proportion of adults classified with stage 2 hypertension was lower in 2007–2010, whereas the proportion with normal BP was greater than in the two earlier time periods. Mean BMI and the proportion of obese adults increased with time. The percentage of adults with diagnosed diabetes mellitus increased over time and the proportion with CKD did not change.
Figure 1.
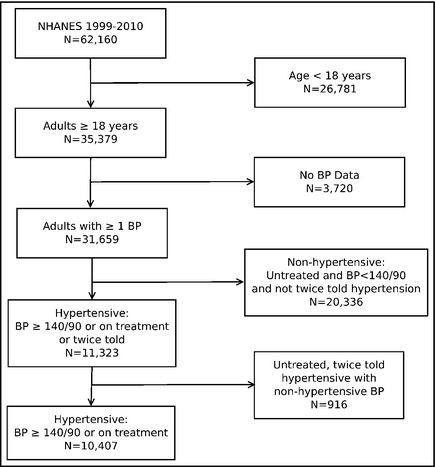
The process by which the various categories of patients for this report were derived from National Health and Nutrition Examination Surveys (NHANES) 1999–2010.
Descriptive characteristics of hypertensive patients defined by BP ≥140/≥90 mm Hg and/or reported treatment and (tHTN) and untreated twice‐told hypertensive patients with nonhypertensive BP (ntHTN) are shown in Table 2. Among the tHTN group, BP declined 7.5/4.6 mm Hg from 1999–2002 to 2007–2010. The proportion of hypertensive patients with stage 2 and stage 1 hypertension each declined 9% to 10% from the first to last survey period, whereas the proportion with BP in the prehypertensive and normal range increased. Mean BMI and the percentage of obese and diabetic patients rose with time. Prevalent CKD did not change.
Among ntHTN group, the only significant difference was a higher proportion of lean individuals in 2003–2006 than 2007–2010. The patients in the ntHTN group were younger than those in the tHTN group. They had a lower proportion of individuals with diabetes and CKD but similar mean BMI values. While ntHTN patients had lower systolic and diastolic BP values than tHTN patients, their BP values were greater than normotensives (Table 1). Moreover, the majority of normotensive individuals had normal BP <120/<80 mm Hg, whereas the majority of ntHTN individuals had BP in the prehypertension range.
Table 3 provides data on hypertension control during 3 NHANES time periods from 1999–2010 to 2 levels including: (1) <140/<90 mm Hg for all patients and (2) <140/<90 for patients without and <130/<80 mm Hg for patients with diabetes and/or CKD. Control rates are shown across the 3 time periods and for the 2 levels of control excluding and including patients with ntHTN. Hypertension control increased significantly with time at both BP goal levels and when designating ntHTN individuals as either hypertensive or nonhypertensive.
Table 3.
BP Control in 3 NHANES Periods Excluding and Including ntHTN Patients
| NHANES Time Period | |||
|---|---|---|---|
| <140/<90 in all HTN patients | 1999–2002 | 2003–2006 | 2007–2010 |
| Excluding uHTN | 33.3 (30.6–36.0) a | 42.7 (39.9–45.5) a | 51.8 (49.6–53.9) a |
| Including uHTN | 39.5 (37.3–41.7) a | 48.5 (45.7–51.4) a | 56.5 (54.2–58.7) a |
| <140/<90 without and <130/<80 with DM and/or CKD | |||
| Excluding uHTN | 28.7 (26.1–31.5) a | 36.9 (34.0–39.9) a | 46.6 (44.2–48.9) a |
| Including uHTN | 34.6 (32.4–37.0) a | 42.8 (39.9–45.7) a | 51.6 (49.2–53.9) a |
Abbreviations: BP, blood pressure; CKD, chronic kidney disease; DM, diabetes mellitus; HTN, hypertension; NHANES, National Health and Nutrition Examination Surveys; ntHTN, nontraditional hypertensive; uHTN, untreated hypertensive. The column 1999–2002 shows the P value for comparison with 2003–2006. The column 2003–2006 shows the P value for comparison with 2007–2010. The column 2007–2010 shows the P value for comparison with 1999–2002. a P<.001.
Table 4 provides data on the clinical epidemiology of hypertension when comparing NHANES 2007–2008 with 2009–2010 using both definitions of prevalent hypertension, ie, designating ntHTN patients as nonhypertensive (Definition A) or hypertensive (Definition B). With both definitions, prevalence and awareness did not change within group between the two survey periods, whereas the proportion of patients treated and controlled (all hypertensives to <140/<90 mm Hg and those with diabetes and/or CKD to <130/<80 mm Hg were marginally higher (P values .05–.07) in 2009–2010. As expected, hypertension control rates were lower when defined by goal values <140/<90 mm Hg in patients without and <130/<80 mm Hg in patients with diabetes mellitus and/or CKD rather than <140/<90 mm Hg for all patients.
Table 4.
Clinical Epidemiology of Hypertension in NHANES 2007–2008 vs 2009–2010: Impact of Untreated Twice‐Told Hypertensive Patients With Nonhypertensive BP
| NHANES | 2007–2008 | 2009–2010 | ||
|---|---|---|---|---|
| Def A | No. | 2057 | 2093 | P Value |
| Prevalence, % | 29.0 (27.6–30.5) | 28.4 (26.3–30.6) | .32 | |
| Awareness, % | 80.7 (78.2–83.0) | 81.1 (78.1–83.8) | .41 | |
| Treated, % | 72.7 (70.3–74.9) | 75.8 (72.0–79.2) | .06 | |
| Controlled, % | 50.1 (46.8–53.5) | 53.3 (50.3–56.3) | .07 | |
| <140/<90, <130/<80 DM/CKDa | 44.7 (41.0–48.4) | 48.4 (45.3–51.4) | .05 |
| Def B | No. | 2221 | 2284 | |
| Prevalence, % | 32.2 (30.8–33.7) | 31.4 (29.3–33.6) | .32 | |
| Awareness, % | 82.6 (80.1–84.9) | 83.0 (80.2–85.5) | .41 | |
| Treated, % | 65.5 (63.4–67.6) | 68.6 (65.2–71.8) | .06 | |
| Controlled, % | 55.0 (51.4–58.6) | 57.8 (54.8–60.8) | .07 | |
| <140/<90, <130/<80 DM/CKDa | 49.8 (45.9–53.7) | 53.2 (50.2–56.2) | .05 |
Abbreviations: Def, Definition; A, excluding and B, including untreated, twice‐told hypertensive with nonhypertensive BP (ntHTN); DM, diabetes mellitus; CKD, chronic kidney disease; NHANES, National Health and Nutrition Examination Surveys. aHypertension control with blood pressure goal <140<90 mm Hg in patients without and <130/<80 mm Hg in patients with DM and/or CKD.
Awareness, treatment, control, and prevalence of hypertension using both definitions of prevalent hypertension are depicted in Figure 2 for the 3 NHANES time periods. Hypertension awareness, treatment, and control increased with time, whereas prevalence did not change. Hypertension prevalence, awareness, and control were higher when designating ntHTN as hypertensive, whereas treatment was lower.
Figure 2.

The impact of excluding (A) or including (B) untreated, twice‐told hypertensive patients with nonhypertensive blood pressure (ntHTN) on hypertension prevalence, awareness, treatment, and control in 3 National Health and Nutrition Examination Surveys (NHANES) time periods from 1999–2010 are provided. The actual mean and 95% confidence intervals for each data point are provided online in Table S1. BP indicates blood pressure; DM, diabetes mellitus; CKD, chronic kidney disease.
Discussion
The principal objectives of this report were to: (1) describe clinical characteristics of untreated twice‐told hypertensive patients with nonhypertensive BP, ie, ntHTN, and assess their impact on the (2) clinical epidemiology of hypertension in the US and (3) Healthy People goals. A related objective was to define the impact of assessing BP control with a goal of <140/<90 mm Hg for all patients vs <140/<90 mm Hg in patients without and <130/80 mm Hg in patients with diabetes and/or CKD on hypertension control goals.
Clinical Characteristics of ntHTN
The patients in the ntHTN group were younger than those in the tHTN group and similar in age to the general adult population (Table 1). BMI in ntHTN and tHTN individuals was similar and higher than all adults combined. The ntHTN patients were less likely to have diabetes mellitus and CKD than tHTN patients, which probably reflected their relative youth. BP values in ntHTN patients were lower than “traditional” hypertensives but higher than normotensives. Of note, BP values in ntHTN patients were similar to BP in treated, controlled hypertensive patients reported previously.20
BP is variable, and there are several errors in measuring BP, which often occur in clinical settings.1, 21, 22, 23 Thus, it is not surprising that roughly 3% of all adults were previously told on 2 occasions that they were hypertensive but had a nonhypertensive NHANES examination. In NHANES, BP is measured according to guidelines including correct positioning of the patient and a period of rest. According to NHANES reporting guidelines, the initial reading was not included in defining mean systolic and diastolic BP values in >90% of participants who had ≥2 BP measurements. In other words, correct positioning and rest prior to BP measurement and discarding the first reading would generally lead to lower BP values when compared with a single, hurried measurement in the usual clinical setting.1, 23 Of note, >60% of individuals with ntHTN have prehypertensive range BP values. Moreover, they are predominantly overweight and obese, both of which increase risk of future hypertension.24
The available data do not clearly resolve whether individuals in NHANES with ntHTN are more appropriately classified as hypertensive or nonhypertensive. NHANES is a critically important dataset for assessing progress toward major national health objectives, eg, Healthy People, and indirectly assessing the effectiveness of healthcare policy and delivery. Thus, inconsistencies in classifying BP status are worth resolving. BP on repeated visits and/or out‐of‐office readings, eg, 24‐ to 48‐hour ambulatory BP monitoring, would enhance accuracy in defining the clinical epidemiology of hypertension.1
Impact of ntHTN on the Clinical Epidemiology of Hypertension
The ntHTN group comprised approximately 3% of the US adult population (Table 2), ie, raised estimates of prevalent hypertension by approximately 3%. Given 234.6 million adults 18 years and older in the US 2010 census,25 the estimated number of hypertensive patients increases by roughly 7 million when ntHTN is included, eg, the AHA Statistical Updates.9, 10 Awareness and control were higher and the percentage of hypertensive patients on treatment lower when ntHTN individuals were classified as hypertensive rather than nonhypertensive (Figure 2).
The impression that hypertension control in the United States remains at <50% designated ntHTN patients as nonhypertensive and included the first BP measurement in calculating mean systolic and diastolic BP.26, 27 The determination of mean systolic and diastolic BP by including the first reading is consistent with hypertension guidelines but not with NHANES reporting guidelines and leads to higher BP values and lower control rates for many hypertensive patients.1, 4, 28
Hypertension control is approximately 5% to 6% higher when ntHTN patients are classified as hypertensive rather than nonhypertensive. Defining BP control as <140/<90 mm Hg in all patients rather than <140/<90 mm Hg in patients without and <130/<80 mm Hg in patients with diabetes and/or CKD also raises hypertension control approximately 5% to 6% across 3 different NHANES periods from 1999–2010. Thus, large absolute differences of approximately 10% to 12% in hypertension control between reports can be explained by these two factors alone and further magnified by including the first BP value (Table 3).4, 20, 26, 27, 28 Of note, Canadian hypertensive patients met the US Healthy People 2020 goal of 60% control in 2007 to 2009, with control at 64.6% (95% confidence interval [CI], 60.0%–69.2%). Their high level of control was achieved without designating ntHTN as hypertensive.22
Irrespective of the hypertension control definition, the time‐dependent improvement in hypertension control was evident across the 3 NHANES time periods (Table 3). Moreover, it appeared that progress was continuing from 2007–2008 to 2009–2010 (Table 4). The observations attest to the effectiveness of primary healthcare for improving population health, despite a growing proportion of uninsured adults in 2009 to 2010.27
Impact of ntHTN on Healthy People Goals
When excluding the group with ntHTN, the Healthy People 2010 goal of controlling 50% of all hypertensive patients to <140/<90 mm Hg was met (51.8%, 95%CI, 49.6%–53.9%) and exceeded when they were included (56.5%, 95%CI, 54.2%–58.7%). Hypertension is a highly prevalent disorder and a major contributor to morbidity and mortality from cardiovascular and CKDs.1 Thus, reducing prevalent hypertension is an important national and international health topic.29 The US Healthy People goals 2000 and 2010 included objectives for reducing prevalent hypertension to 16%.2, 3 Recognizing the lack of progress in hypertension prevention, Healthy People 2020 set a more credible goal of reducing prevalent hypertension by a relative 10% to 26.9%. Designating ntHTN patients as hypertensive raises prevalent hypertension from 28.7% to 31.8% in 2007–2010 thereby reducing the likelihood of achieving the Healthy People 2020 goal for prevalent hypertension.
Conclusions
Individuals with nontraditionally defined hypertension are younger and less likely to have diabetes and CKD than traditionally defined hypertensives but are equally overweight and obese. They comprise approximately 3% of all adults, and thus raised estimates of prevalent hypertension by approimxately 7 million individuals in the United States in 2010. Moreover, inclusion of ntHTN as hypertensive raises hypertension control rates approximately 5% to 6% and assessing BP control for all patients at <140/<90 mm hg vs <140/<90 mm Hg in patietns without and <130/<80 mm Hg for patients with diabetes and/or CKD also raises control approximately 5% to 6%. Together, these two variables can lead to 10% to 12% absolute differences in hypertension control between reports. Given the importance of accurately classifying ntHTN patients in assessing the clinical epidemiology of hypertension within and between populations over time, addition of 24‐ to 48‐hour ambulatory BP and/or home BP monitoring could be useful in correctly assigning BP category and assessing the clinical epidemiology of hypertension.1 Consistent definitions of prevalent hypertension and control are essential in assessing the burden of risk and the effectiveness of healthcare policy and delivery in moving toward important national health objectives.
Disclosures
Brent Egan: In addition to federal and state funding sources listed, Dr Egan has received research support from Daiichi‐Sankyo (>$10,000), Medtronic (>$10,000), Novartis (>$10,000), Takeda (>$10,000) during the past 3 years and has served as a consultant to Astra Zeneca (<$10,000), Novartis (<$10,000), Medtronic (>$10,000), Takeda (<$10,000), and Blue Cross Blue Shield of South Carolina (>$10,000). Yumin Zhao: None. None of the funding agencies had input on the study design, data analysis, interpretation, or the decision to submit this paper for publication.
Supporting information
Table S1. Clinical Epidemiology of Hypertension During 3 NHANES Time Periods When Excluding and Including Untreated, Twice‐Told Hypertensive With Nonhypertensive BP.
Acknowledgments
None.
Funding Sources
This original paper was indirectly supported by grants from the Centers for Disease Control (Community Transformation Grant through the South Carolina Department of Health and Environmental Control [SC DHEC]); State of South Carolina; NIH HL105880; SC DHEC, Tobacco Control and Heart Disease and Stroke Prevention; NIH NS058728, and NIH HL091841.
J Clin Hypertens (Greenwich). 2013;15:154–161. ©2013 Wiley Periodicals, Inc.23458586
References
- 1. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. [DOI] [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services . Healthy People 2010. With Understanding and Improving Health and Objectives for Improving Health, 2 vols, 2nd edn. Washington, D.C.: U.S. Government Printing Office; 2000. [Google Scholar]
- 3. Healthy People 2020 Objective Topic Areas and Page Numbers . Heart Disease and Stroke, pp. 150–159. http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf. Accessed July 11, 2012.
- 4. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 5. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 6. Ong KL, Cheung BMH, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 7. Cutler JA, Sorlie PD, Wolz M, et al. Trends in the hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. [DOI] [PubMed] [Google Scholar]
- 8. Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 to 2000. A rising tide. Hypertension. 2004;44:398–404. [DOI] [PubMed] [Google Scholar]
- 9. Roger VL, Go AS, Lloyd‐Jones DM, et al. Heart disease and stroke statistics–2012 Update. A report from the American Heart Association. Circulation. 2012;125:e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NHANES methods 2009–2010. http://www.cdc.gov/nchs/data/nhanes/survey_content_99_12.pdf. Accessed July 12, 2012.
- 11. Centers for Disease Control and Prevention—National Health and Nutrition Examination Survey: Survey questionnaires, examination components and laboratory components 2009—2010 . http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/questexam09_10.htm. Accessed July 12, 2012.
- 12. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 13. Accord Study Group . Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Appel LJ, Wright JT Jr, Greene T, et al., Intensive blood pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:974–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stevens LA, Coresh J, Feldman HI, et al. Evaluation of the modification of diet in renal disease equation in a large diverse population. J Am Soc Nephrol. 2007;18:2749–2757. [DOI] [PubMed] [Google Scholar]
- 16. Jones CA, Francis ME, Eberhardt MS, et al. Microalbuminura in the US population: third national health and nutrition examination survey. Am J Kid Dis. 2002;39:445–459. [DOI] [PubMed] [Google Scholar]
- 17. Selvin E, Manzi J, Stevens LA, et al. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis. 2007;59:918–926. [DOI] [PubMed] [Google Scholar]
- 18. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–1197. [DOI] [PubMed] [Google Scholar]
- 19. Harris MI, Goldstein DE, Flegal KM, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults; the Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21:518–524. [DOI] [PubMed] [Google Scholar]
- 20. Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the U.S. 1988–2008. Circulation. 2011;124:1046–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McAlister FA, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ. 2011;183:1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rosner B, Polk BF. The implications of blood pressure variability for clinical and screening purposes. J Chron Dis. 1979;32:451–461. [DOI] [PubMed] [Google Scholar]
- 23. Jones DW, Appel LJ, Sheps SG, et al. Measuring blood pressure accurately. New and persistent challenges. JAMA. 2003;289:1027–1030. [DOI] [PubMed] [Google Scholar]
- 24. Selassie A, Wagner CS, Laken ML, et al. Progression is accelerated from pre‐hypertension to hypertension in African Americans. Hypertension. 2011;58:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Howden LM, Meyer JA. Age and sex composition 2010: US Census Briefs. http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. Accessed November 8, 2012.
- 26. Guo F, He D, Zhan W, Walton RG. Trends in the prevalence, awareness, management and control of hypertension among United States adults, 1999 to 2010. JACC. 2012;60:599–605. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention . Vital signs: awareness and treatment of uncontrolled hypertension among adults— United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61(35):703–709. [PubMed] [Google Scholar]
- 28. Handler J, Zhao Y, Egan BM. Impact of the number of blood pressure measurements on blood pressure classification in U.S. adults: NHANES 1999–2008. J Clin Hypertens. 2012;14:751–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Perkovic V, Huxley R, Wu Y, et al. The burden of blood pressure‐related disease: a neglected priority for global health. Hypertension. 2007;50:991–997. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Clinical Epidemiology of Hypertension During 3 NHANES Time Periods When Excluding and Including Untreated, Twice‐Told Hypertensive With Nonhypertensive BP.


