Abstract
Background
One strategy proposed to alleviate nursing shortages is the promotion of organizational efforts that will improve nurse recruitment and retention. Cross-sectional studies have shown that the quality of the nurse work environment is associated with nurse outcomes related to retention, but there have been very few longitudinal studies undertaken to examine this relationship.
Objectives
To demonstrate how rates of burnout, intention to leave, and job dissatisfaction changed in a panel of hospitals over time, and to explore whether these outcomes were associated with changes in nurse work environments.
Methods
A retrospective, two-stage panel design was chosen for this study. Survey data collected from large random samples of registered nurses employed in Pennsylvania hospitals in 1999 and 2006 were used to derive hospital-level rates of burnout, intentions to leave current positions, and job dissatisfaction, and to classify the quality of nurses’ work environments at both points in time. A two-period difference model was used to estimate the dependence of changes in rates of nurse burnout, intentions to leave, and job dissatisfaction on changes in nurse work environments between 1999 and 2006 in 137 hospitals, accounting for concurrent changes in nurse staffing levels.
Results
In general, nurse outcomes improved between 1999 and 2006, with fewer nurses reporting burnout, intentions to leave, and job dissatisfaction in 2006 as compared to 1999. Our difference models showed that improvements in work environment had a strong negative association with changes in rates of burnout (β =−6.42%, p<0.01) intentions to leave (β =−4.10%, p<0.01), and job dissatisfaction (β =−8.00%, p<0.01).
Conclusions
Improvements in nurse work environments over time are associated with lower rates of nurse burnout, intentions to leave current positions, and job dissatisfaction.
Keywords: burnout, intention to leave, job satisfaction, nurse management, nurse staffing, nurse retention, nurse work environments
1. Introduction
Improving the quality of healthcare is an international priority in which nurses play an essential role; yet many countries are faced with having too few nurses to meet the needs of their citizens (Buerhaus, Auerbach, and Staiger, 2009, Oulton, 2006, Sermeus and Bruyneel, 2010). Nursing shortages can be particularly felt in acute care hospitals, where patient complexity and workload demands are rapidly increasing (Rechel et al., 2009). At the same time, hospital nurses in many countries have been identified as having high levels of dissatisfaction and burnout, while many intend to leave their current job (Aiken et al., 2012, Estryn-Behar et al., 2007). One strategy that has been suggested to alleviate nursing shortages is the promotion of organizational efforts to improve recruitment and retention of staff (Van den Heede et al., 2011).
A number of studies have shown that the environment in which nurses work, a modifiable organizational feature of hospitals, is an important determinant of work-related outcomes, including burnout levels, intentions to leave positions, and job dissatisfaction (Aiken et al., 2011, Hasselhorn et al., 2006, Van Bogaert et al., 2010). Moreover, the link between unfavorable work environments and poor nurse outcomes appears to be a global phenomenon. In a recent study of nurses in 12 countries in Europe (RN4CAST) and the United States, Aiken and colleagues (2012) revealed that the odds of nurses reporting high levels of burnout, intentions to leave, and job dissatisfaction were lower in hospitals with better work environments than in hospitals with poor environments, and that these differences were similar in both European and U.S. hospitals. These relationships have also been confirmed in several Asian countries (Aiken et al., 2011). In another large survey of nurses, the European Nurses’ Early Exit (NEXT) study found that poor working conditions were the most common reason nurses offered for leaving their current position (Estryn-Behar et al., 2010). Moreover, nurses’ job satisfaction and burnout are highly associated with quality of patient care, including mortality (Aiken et al., 2002), patient safety (Aiken, 2012), and the patient experience of hospital care (Aiken et al., 2012, McHugh et al., 2011, Vahey et al., 2004).
One shortcoming of this growing international evidence base is that it consists primarily of evidence from cross-sectional studies. Unfortunately, there is very little evidence that changes in a hospital’s nurse work environment over time are related to changes in a hospital’s rates of nurse burnout, intentions to leave, and job dissatisfaction. Longitudinal data would provide hospital administrators and policymakers with a stronger empirical case to improve nurse work environments. The European NEXT survey was longitudinal in design and prospectively surveyed nurses at two points in time (Hasselhorn et al. 2006). The most recent longitudinal analyses of those data have focused on individual nurse perceptions about work-related factors and intentions to leave (Estryn-Behar et al., 2010, Hasselhorn et al., 2008). In the United States, Spetz (2008) used random samples of nurses at two points in time to document an increase in nurses’ job satisfaction after staffing levels and working conditions improved due to the implementation of California’s mandated staffing ratios. Spetz, however, was unable to link nurses to their employing hospitals. Therefore, it is not clear whether the increase in nurse satisfaction was any more pronounced in hospitals that improved their staffing than in those that witnessed no change in staffing, or a negative one. Our study fills a gap in the literature by exploring how changes in work environments at the hospital-level are associated with rates of unfavorable nurse outcomes.
The current study presents data from 137 hospitals in Pennsylvania, one of the most populous and geographically diverse states in the U.S. In 1999, a survey of Pennsylvania nurses revealed that over 40% of staff nurses were dissatisfied with their jobs and experienced high burnout levels, while nearly a quarter were planning to leave their current positions within the next year (Aiken et al., 2002). We use these same data from 1999, and merge those data with survey data from 2006 to construct a two-wave panel of hospitals. We demonstrate how nurse outcomes changed in a set of Pennsylvania hospitals between 1999 and 2006, and how these outcomes may have been influenced by changing work environments, accounting for concurrent changes in staffing levels.
2. Methods
A retrospective, two-stage panel design was used for this study and involved the use of two types of data from 1999 and 2006: nurse survey and administrative hospital data. There were 137 hospitals for which both sources of data were complete and available at both points in time. This study was reviewed and approved by the University of Pennsylvania Institutional Review Board.
2.1 Data Sources and Study Sample
Nurses
Data from the Pennsylvania Registered Nurse Survey (1999) and Multi-State Nursing Care and Patient Safety Survey (2006), both collected by the University of Pennsylvania, were used for this study (Aiken et al., 2002, Aiken et al., 2011). Mail surveys were used to collect job-related data from large random samples of all licensed Pennsylvania nurses in 1999 (50%) and 2006 (40%). All nurses were asked to identify their work setting. Hospital nurses were additionally requested to name their employer. Identical items regarding workload, the work environment, job outcomes, and demographics were asked in both the 1999 and 2006 surveys. More than 42,000 nurses (52% response rate) returned the survey in 1999, while over 25,000 nurses (39% response rate) responded in 2006. A double sample of 650 non-responders was drawn in 2006 and results from that analysis showed no evidence of response bias on the primary variables of interest (Smith, 2008). The representativeness of the nurses at both time points was confirmed by comparing a set of basic demographic characteristics from the survey with the responses of Pennsylvania nurses in the 2000 and 2008 National Sample Survey of Registered Nurses (Spratley et al., 2001, U.S. Department of Health and Human Services, 2010). About one- third of respondents in both years worked as acute care hospital staff nurses. This set of nurses comprised the analytic sample for this study, and included 9,345 nurses in 1999 and 5,957 nurses in 2006. In 1999, about 70 nurses from each hospital responded, while in 2006, there were 49 nurse respondents on average in each hospital.
Hospitals
Nurse survey data were aggregated to obtain hospital-level measures of nurse work environments and staffing, as well as rates of nurse job outcomes for both years. To reliably estimate measures, only hospitals that had at least 10 nurse respondents were used in the final analysis. The American Hospital Association (AHA) Annual Survey data for corresponding years was used to obtain data on other structural hospital characteristics.
2.2 Study Variables
Our primary outcomes of interest were the changes in rates of nurse burnout, intent to leave, and job dissatisfaction in a set of Pennsylvania hospitals between 1999 and 2006. The emotional exhaustion subscale of the Maslach Burnout Inventory (Maslach and Jackson, 1986) was used to measure nurse burnout. The emotional exhaustion subscale consists of 9 items on which nurses are asked to respond using a scale of 1 through 6. Respondents that scored greater than 27, which is the norm for healthcare workers, on the subscale were classified as having high burnout (Maslach and Jackson, 1986). Intent to leave was measured by asking respondents to report whether or not they intended to be with their current employer in one year. Job satisfaction was measured by a single item on the survey that asked respondents to rate how satisfied they were with their job. Nurses were considered to be “dissatisfied” if they reported being very dissatisfied or moderately dissatisfied, as compared to nurses who reported being very satisfied or somewhat satisfied. At each time point, we calculated an aggregated hospital-level rate for each outcome, adjusting for individual nurse characteristics including age, sex, education, full-time status, and unit type. After obtaining hospital-level adjusted outcome rates, we then calculated the change in each of the three nurse outcome rates in each hospital from 1999 to 2006.
Our primary independent variable of interest was change in the nurse work environment of hospitals between 1999 and 2006. The nurse work environment was measured using the Practice Environment Scale of the Nursing Work Index (PES-NWI), a 31-item scale composed of five subscales: staffing and resource adequacy, nurse manager ability and leadership, nurse-physician relations, nurse participation in hospital affairs, and nursing foundations for quality of care (Lake, 2002). The predictive validity of the PES-NWI as it relates to nurse job outcomes has been established in various international settings (Aiken et al., 2012, Warshawsky and Havens, 2011), and the discriminate validity of the PES-NWI to differentiate hospital nurse work environments has been demonstrated (Lake and Friese, 2006). Nurses were asked to report the degree to which each of 31 characteristics of better work environments was present in their current jobs, using a Likert-type scale ranging from strongly disagree (coded 1) to strongly agree (coded 4). Subscales scores were calculated by averaging individual nurse responses to items on each subscale. Nurse scores were then averaged for each hospital and thus aggregated to the hospital-level. A composite PES-NWI score was calculated for each hospital in both years by taking the average of four of the five PES-NWI subscales. The excluded subscale, staffing and resource adequacy, was omitted due to its substantial correlation with the staffing measure we included in our analyses, described below.
We then categorized hospitals’ nurse work environments as “better”, “mixed”, or “poor” in each year, and used these two categorizations to distinguish hospitals that “improved,” “worsened,” or showed “no change” over time.. In each year, hospitals were classified as “better” if their PES-NWI composite score fell in the highest quartile for all hospitals, “mixed” if they were in the two middle quartiles, and “poor” if they were in the lowest quartile. Hospitals were then classified as “improved” over the time period if they moved from poor to mixed, mixed to better, or poor to better. Hospitals were classified as “worsened” if they moved from better to mixed, mixed to poor, or better to poor. Hospitals that were consistently “good”, “mixed”, or “poor” in both years, or that did not change work environment categories between 1999 and 2006 were classified as “no change”.
We also wanted to account for simultaneous changes in nurse staffing over the time period. To measure nurse staffing, we used a measure on the survey that asked nurses to report the number of patients they cared for on their last shift. Nurses that reported caring for at least one but no more than twenty patients on their last shift were included in calculating the staffing measure. Responses were averaged across all nurses in each hospital yielding a mean number of patients cared for in each hospital. The predictive validity of using nurse reports in this manner to assess staffing levels has been previously demonstrated (Aiken et al., 2002, Aiken et al., 2008). We then calculated the change in aggregate staffing levels from 1999 to 2006, and then categorized the hospitals based on these differences. Hospitals with an average increase of more than 0.5 patients per nurse were coded as “worsened”, hospitals declining more than 0.5 average patients per nurse were coded as “improved”, and hospitals between these two values were defined as having “no change” with respect to staffing. We chose to classify hospitals based on these cut points because it facilitated interpretation of our results and provided a sufficient number of hospitals in each category.
Structural characteristics of hospitals at both points in time were derived from the AHA Annual Survey. Hospital size was measured as number of beds and was classified into three categories of small (≤100 beds), medium (101–250 beds), and large (≥251 beds). Technology status was measured by presence of facilities to perform open heart surgery and/or organ transplants. Teaching status was defined by the number of medical residents and fellows per bed, and was classified as non-teaching, minor (<1:4 trainee to bed ratio), and major (>1:4 trainee to bed ratio).
2.3 Data Analysis
We estimated a two-period difference model in order to analyze the changes in rates of nurse burnout, intentions to leave, and job dissatisfaction from 1999 to 2006 and their associations with changes in nurse staffing and work environment. Our dependent variables were the changes in adjusted rates of burnout, intention to leave, and job dissatisfaction, and our covariates were categorical measures of changes in work environment (i.e. worsened, no change, improved) and staffing (i.e. worsened, no change, improved). We adjusted for baseline staffing and work environment values in 1999, in addition to hospital characteristics that may have differing effects at the two time periods (Allison, 2005). Taking advantage of the LSMEANS statement in PROC GLM, we were able to compare differences in the change in nurse outcome rates between hospitals that had varying levels of work environment changes. As an example, our model allowed us to see if hospitals that improved in work environments had greater declines in burnout rates, or lesser increases in burnout rates, than hospitals that witnessed no change or declines in their work environments. All statistical analyses were conducted using SAS V9.2 (SAS Institute, Cary, NC).
3. Results
We obtained a sample of 137 hospitals in Pennsylvania that had available nurse and hospital data in 1999 and 2006. Table 1 outlines the sample hospitals’ characteristics at both points in time. As compared to 1999, more hospitals in 2006 had the capability to perform high technology procedures, a greater number of beds, and were affiliated with a medical school. The percentage of nurses with high burnout across hospitals decreased by about 5% between 1999 and 2006 (42.2% vs. 37.6%, p=0.01). The percentage of nurses who reported intentions to leave diminished from 22.4% to 14.2% (p<0.01) over the time period. A similar trend was observed in the number of nurses across hospitals that reported job dissatisfaction, which decreased from 40.7% in 1999 to 31.5% in 2006 (p<0.01).
Table 1.
Pennsylvania Hospital Characteristics and Nurse Outcomes in 1999 and 2006 (n=137)
| 1999 | 2006 | P- value | |
|---|---|---|---|
| Hospital Characteristics | |||
| Technology Status (n, %) | 0.05 | ||
| High | 45 (32.8) | 61 (44.5) | |
| Low | 92 (67.2) | 76 (55.5) | |
| Beds Set-Up and Staffed, (mean, SD) | 205 ± 8 | 247 ± 16 | <0.01 |
| Teaching Status (n,%) | 0.04 | ||
| Major | 17 (12.4) | 19 (13.9) | |
| Minor | 37 (27.0) | 54 (39.4) | |
| Non-Teaching | 83 (60.6) | 64 (46.7) | |
| Nurse Outcomes, mean % (SD) | |||
| High Burnout Level | 42.2 (13.2) | 37.6 (14.1) | 0.01 |
| Intention to Leave Present Job Within One Year | 22.4 (8.7) | 14.2 (9.0) | <0.01 |
| Dissatisfied with Present Job | 40.7 (10.7) | 31.5 (13.9) | <0.01 |
3.1 Changes in Work Environment and Staffing
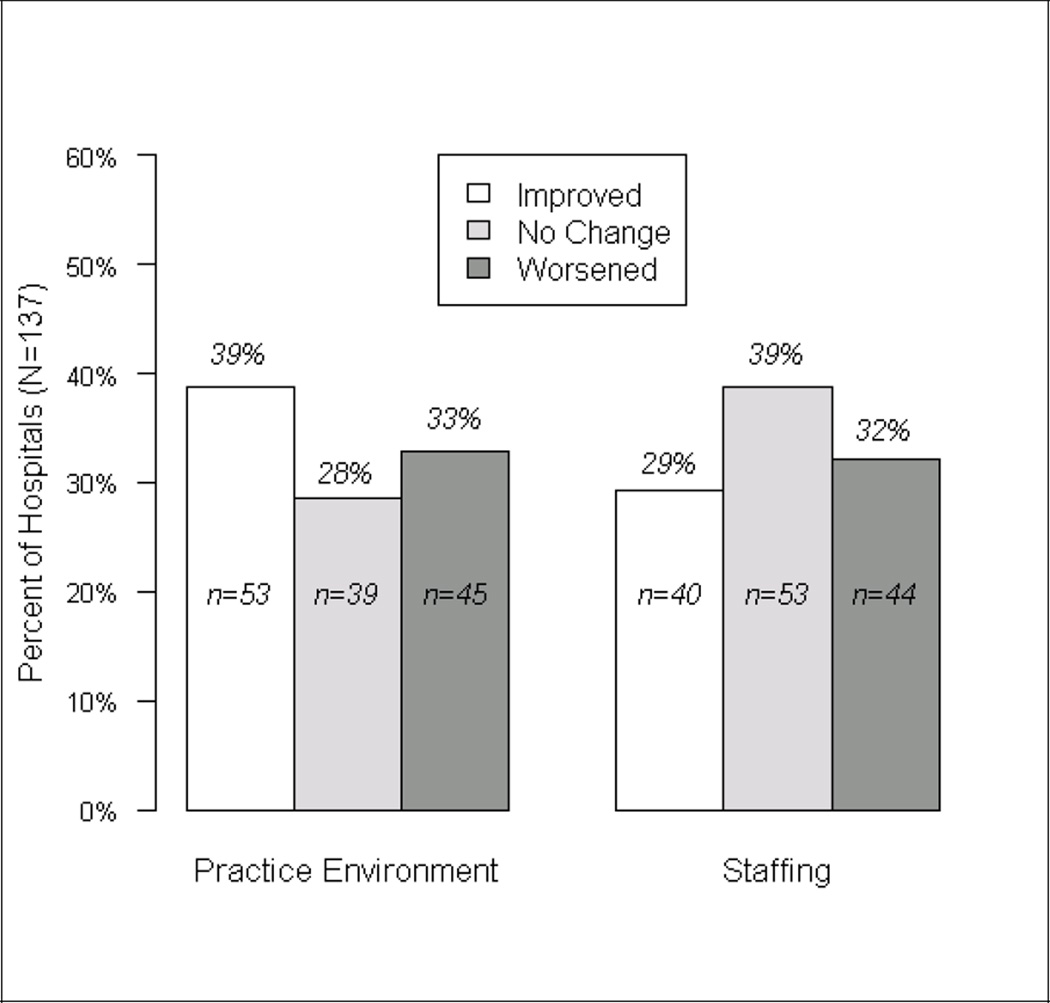
We then examined how individual hospitals changed in terms of the work environments and nurse staffing between 1999 and 2006. Figure 1 shows that roughly four in ten hospitals (53 of the 137, or 39%) improved their nurse work environments over the time period while 45 (33%) worsened and 39 (28%) remained unchanged. We found that nurse staffing levels did not change by more than 0.5 patients per nurse in 39% of the hospitals over the time period, while 29% of the hospitals improved their staffing and 32% worsened in staffing.
Fig. 1.
Change in nursing organization characteristics from 1999 to 2006.
3.2 Regression Results
Table 2 displays the results of our two-period difference model examining the association between the change in nurse outcome rates and change in nurse work environments, accounting for changes in nurse staffing. We found that improvements in work environment had a strong negative association with changes in rates of burnout, intentions to leave, and job dissatisfaction (all p<0.01), suggesting that hospitals that improved their work environment had lowered rates of adverse nurse outcomes over time. For example, the percentage of nurses who reported being dissatisfied with their jobs was 8% lower (β=−8.00, p<0.01) in hospitals that improved their work environments as compared to those that did not change (or in hospitals that did not change as compared to those that declined). Improvements in nurse staffing were significantly associated with lowered burnout rates over time (β=−3.63, p=0.03), but were not found to be significantly associated with changes in intentions to leave or job dissatisfaction.
Table 2.
Two-period Difference Model Regression Results: Association between Changes in Work Environment and Staffing and Changes in Nurse Outcomes (n=137 hospitals) †
| Estimate | SE | P-Value | |
|---|---|---|---|
| Burnout | |||
| Work Environment | −6.42 | 1.77 | <0.01 |
| Staffing | −3.63 | 1.60 | 0.03 |
| Intention to Leave | |||
| Work Environment | −4.10 | 1.24 | <0.01 |
| Staffing | 0.47 | 1.13 | 0.68 |
| Job Dissatisfaction | |||
| Work Environment | −8.00 | 1.46 | <0.01 |
| Staffing | −0.96 | 1.32 | 0.47 |
Regressions control for baseline staffing, work environment, teaching status, bed size, and technology status. Coefficients for work environment/staffing represent the average change in outcome rate associated with a hospital that improved as compared to a hospital that did not change (or a hospital that did not change as compared to one that declined).
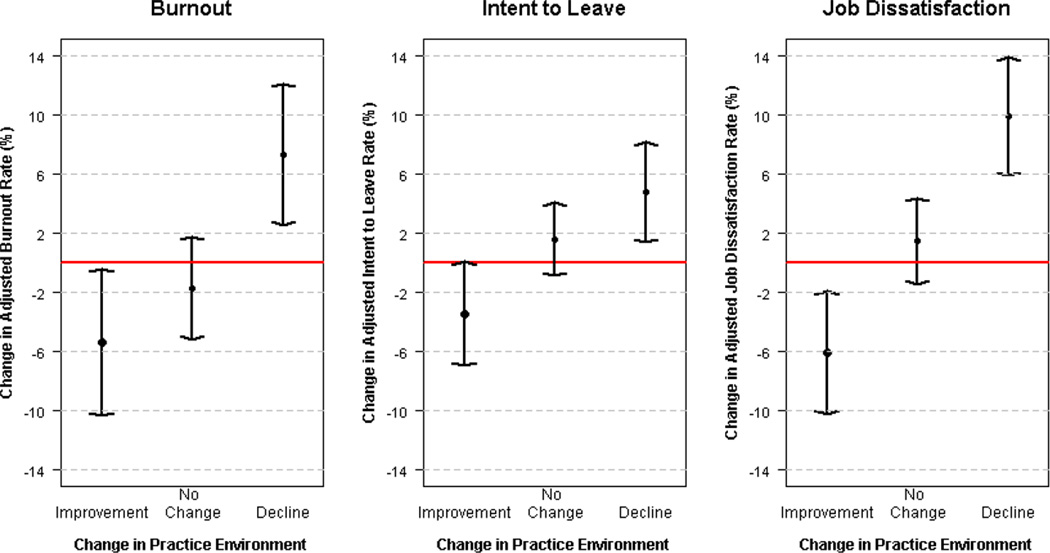
To further quantify the differences in nurse outcome rates based on changes in work environment, we report and compare the least squares average change rate at each work environment level. Table 3 summarizes the average changes in nurse outcomes by work environment level, and Figure 2 graphically displays the results. There were significant and substantial declines in burnout rates among hospitals that improved in work environment, that averaged 5.4% (p= 0.04), while hospitals that that showed declining work environments had increases in burnout averaging 7.4% (p<0.01). We found that nurses working at hospitals with improved work environments experienced a 3.5% decrease (p=0.06), in average rates of intention to leave, as compared to 4.8% increase for declining hospitals (p<0.01). Finally, changes in job dissatisfaction rates followed a similar pattern, with a significant decrease in rates for the hospitals that improved in work environment by about 6% on average (p<0.01). Hospitals declining in work environment showed an increase in average job dissatisfaction rates by about 10% (p<0.01) from 1999 to 2006. Hospitals that did not change their work environment between the two years did not experience a significant change in any of the three outcomes.
Table 3.
Summary of Changes in Nurse Outcomes from 1999 to 2006 by Level of Change in Work Environment (n=137 hospitals)†
| Nurse Outcome | Change in Work Environment from 1999 to 2006 |
Mean Change† in Outcome Rate from 1999 to 2006 (%) |
SE | P-Value |
|---|---|---|---|---|
| Burnout | ||||
| Decline | 7.35 | 2.45 | <0.01 | |
| No Change | −1.70 | 1.78 | 0.34 | |
| Improvement | −5.38 | 2.55 | 0.04 | |
| Intention to Leave | ||||
| Decline | 4.77 | 1.73 | <0.01 | |
| No Change | 1.61 | 1.26 | 0.20 | |
| Improvement | −3.46 | 1.80 | 0.06 | |
| Job Dissatisfaction | ||||
| Decline | 9.93 | 2.04 | <0.01 | |
| No Change | 1.47 | 1.48 | 0.32 | |
| Improvement | −6.06 | 2.12 | <0.01 |
Mean change represents the least-square average changes from a linear regression model, adjusted for staffing and hospital characteristics (teaching status, bed size, and technology status)
Figure 2.
Comparing Mean Changes in Nurse Outcome Rates among Pennsylvania Hospitals from 1999 to 2006, by Change in Work Environment (n=137 hospitals) †
†Mean change represents the least-square average changes from a linear regression model, adjusted for staffing and hospital characteristics (teaching status, bed size, and technology status)
4. Discussion
This study represents one of the first empirical examinations of how hospitals changed in terms of their nurse work environments and the concomitant change in nurse outcomes that are strongly related to nurse retention. Our results suggest that improvements in nurse work environments over time are associated with declines in the rates of nurse burnout, intentions to leave current positions, and job dissatisfaction. Although the percentage of nurses who reported being burned out, intended to leave their position, or who were dissatisfied with their job declined overall between the two years, hospitals that improved their nurse work environments witnessed favorable changes in these outcomes over time, while unfavorable changes were found in hospitals where the work environment declined. Our findings using longitudinal panel data confirm the associations found between work environments and nurse job outcomes in cross-sectional studies and take us a step closer to the conclusion that the connection between the two is causal.
Changes in nurse staffing levels were significantly associated with changes in rates of burnout. Controlling for baseline staffing levels, the percentage of nurses who reported being burned-out in hospitals that improved their staffing levels decreased by nearly 4% as compared to hospitals that did not change. These findings are consistent with those of cross-sectional studies that have linked staffing with nurse burnout (Aiken et al., 2012, Rafferty et al., 2007). We did not observe significant changes in the percentage of nurses who intended to leave or were dissatisfied related to more favorable staffing levels. While nearly a third of the hospitals in our sample witnessed increases in workloads averaging more than half a patient per nurse, these changes may not be sizable enough to produce substantial or significant differences in intentions to leave and dissatisfaction.
Our finding that work environment was a stronger and more consistent predictor of nurse job outcomes than staffing is not particularly surprising when examined in the context of the current literature on the topic. Our findings echo those of the longitudinal European EXIT study that found work-related factors, such as relationships with physicians, nurse managers and colleagues, and overall working climate, to be significantly related to nurse turnover (Estryn-Behar et al., 2010, Hasselhorn et al., 2008). Although staffing was one of the reasons why nurses left their jobs, it was not cited as often as dissatisfaction with autonomy and with working relationships (Estryn-Behar et al., 2010)— two similar concepts measured by the PES-NWI in this study. Other research suggests that favorable staffing levels are not beneficial to patient outcomes unless the work environment is good (Aiken et al., 2011). Future research should examine whether this relationship holds true in the examination of nurse job outcomes.
We acknowledge some limitations to our approach. First, the two-period difference model theoretically accounts for unobserved and unmeasured characteristics that did not change over time; however, there are potential variables that did change over time that we were unable to measure that could influence outcomes, such as internal quality improvement efforts and the hospital’s fiscal health. More than two time points would also provide for a more accurate assessment of the direction of the relationships we observed, as well as identify how soon hospitals might expect to see an improvement in outcomes after changes are made. We also did not have a direct measure of actual nurse turnover. Our measure was based upon nurse’s intentions to leave in the next year; we do not know if nurses with intentions to leave their jobs actually follow through on those intentions. However, evidence suggests that intention to leave is highly correlated with actual turnover (Hayes et al., 2006). Finally, our study was limited to 137 hospitals in one large state in the mid-Atlantic region of the United States. Therefore, researchers should aim to perform similar studies in other contexts.
5. Conclusion
Using longitudinal panel data, we demonstrate that hospitals that improve their nurse work environments may expect to have lower rates of burnout, intentions to leave, and job dissatisfaction among their nurses. The findings of this study are supportive of current initiatives to transform the environment in which nurses practice (Institute of Medicine, 2004, Robert Wood Johnson Foundation and the Institute for Healthcare Improvement, 2007). The international Magnet recognition program, coordinated by the American Nurses Credentialing Center, provides a model for healthcare organizations to promote nurse leadership, empowerment, professional practice, and innovation to improve outcomes (American Nurses Credentialing Center, 2012). Given the current state of the global nursing workforce, investments in nurse work environments may prove to be a critically important, cost-efficient, option to promote the recruitment and retention of nurses, and ultimately improve the quality of patient care.
What is already known about the topic?
Nurse work environments are predictive of nurse job outcomes associated with retention, including burnout, intentions to leave, and job satisfaction.
Most studies of the association between nurse work environments and nurse job outcomes have been cross-sectional.
What this paper adds
This study provides longitudinal evidence that improvements in hospital nurse work environments are associated with reductions in poor nurse job outcomes over time.
The findings of this study provide stronger evidence to support current initiatives to improve hospital nurse work environments.
Acknowledgements
This project was supported by AHRQ K08-HS-018534 (Kutney-Lee, PI), NINR R01-NR-004513 (Aiken, PI), and the Robert Wood Johnson Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the National Institute of Nursing Research, or the Robert Wood Johnson Foundation. The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of the report. The authors would like to thank Tim Cheney and Megan Soisson for their assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff DF. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care. 2011;49:1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. Journal of Nursing Administration. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Bruyneel L, Rafferty AM, Griffiths P, Moreno-Casbas MT, Tishelman C, Scott A, Brzostek T, Kinnunen J, Schwendimann R, Heinen M, Zikos D, Strømseng Sjetne I, Smith HL, Kutney-Lee A. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Clarke S, Poghosyan L, Cho E, You L, Finlayson MM, Kanai-Pak M, Aungsuroch Y. Importance of work environments on hospital outcomes in nine countries. International Journal for Quality in Health Care. 2011;23(4):357–364. doi: 10.1093/intqhc/mzr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison P. Fixed effects regression methods for longitudinal data using SAS. Cary, N.C.: 2005. [Google Scholar]
- American Nurses Credentialing Center. Magnet Recognition Program Model ®. 2012 http://www.nursecredentialing.org/Magnet/ProgramOverview/New-Magnet-Model.aspx. [Google Scholar]
- Buerhaus PI, Auerbach DI, Staiger DO. The recent surge in nurse employment: causes and implications. Health Affairs. 2009;28(4):w657–w668. doi: 10.1377/hlthaff.28.4.w657. [DOI] [PubMed] [Google Scholar]
- Estryn-Behar M, Van Der Heijden JM, Fry C, Hasselhorn HM. Longitudinal analysis of personal and work-related factors associated with turnover among nurses. Nursing Research. 2010;59(3):166–177. doi: 10.1097/NNR.0b013e3181dbb29f. [DOI] [PubMed] [Google Scholar]
- Estryn-Behar M, Van Der Heijen JM, Oginska H, Camerino D, Le Nezet O, Conway PM, Fry C, Hasselhorn HM NEXT Study Group. The impact of social work environment, teamwork characteristics, burnout, and personal factors upon intent to leave among European nurses. Medical Care. 2007;45(10):939–950. doi: 10.1097/MLR.0b013e31806728d8. [DOI] [PubMed] [Google Scholar]
- Hasselhorn HM, Conway PM, Widerszal-Bazyl M, Simon M, Tackenberg P, Schmidt S, Camerino D, Müller BH NEXT Study Group. Contribution of job strain to nurses’ consideration of leaving the profession—results from the longitudinal European Nurses’ Early Exit Study. Scandinavian Journal of Work, Environment and Health. 2008;(Supplement)(6):75–82. [Google Scholar]
- Hasselhorn HM, Tackenberg P, Kuemmerling A, Wittenberg J, Simon M, Conway PM, Bertazzi PA, Beermann B, Buscher A, Camerino D, Caillard JF, D’Hoore W, Estryn-Behar M, Fontenla M, Gould D, Van Der Heijden B, Josephson M, Kiss P, Kovarova M, Kuhn K, Laine M, Le Nezet O, Lindberg P, Oginska H, Pokorski J, Radkiewicz P, Rimarcik M, Van Der Schoot E, Stelzig S, Stordeur S, Wickstroem G, Widerszal-Bazyl M, Mueller BH. Nurses’ health, age and the wish to leave the profession—findings from the European NEXT-Study. La Medicina del Lavoro. 2006;97(2):207–214. [PubMed] [Google Scholar]
- Hayes LJ, O’Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, Spence Laschinger HK, North N, Stone PW. Nurse turnover: a literature review. International Journal of Nursing Studies. 2006;43(2):237–263. doi: 10.1016/j.ijnurstu.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Keeping patients safe: transforming the work environment of nurses. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Research in Nursing and Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lake ET, Friese CR. Variations in nursing practice environments. Nursing Research. 2006;55(1):1–9. doi: 10.1097/00006199-200601000-00001. [DOI] [PubMed] [Google Scholar]
- Maslach C, Jackson SE. Maslach Burnout Inventory Manual. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs. 2011;30(2):202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oulton JA. The global nursing shortage: an overview of issues and actions. Policy, Politics, and Nursing Practice. 2006;7(3):34S–39S. doi: 10.1177/1527154406293968. [DOI] [PubMed] [Google Scholar]
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, Aiken LH. Outcomes of variation in hospital nurse staffing in English hospitals: Cross-sectional analysis of survey data and discharge records. International Journal of Nursing Studies. 2007;44:175–182. doi: 10.1016/j.ijnurstu.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rechel B, Wright S, Edwards N, Dowdeswell B, McKee M. Introduction: hospitals within a changing context. In: Rechel B, Wright S, Edwards N, Dowdeswell B, McKee M, editors. Investing in Hospitals of the Future. European Observatory on Health Systems and Policies; 2009. pp. 3–25. [Google Scholar]
- Robert Wood Johnson Foundation and the Institute for Healthcare Improvement. Publications and research. A new era in nursing: Transforming Care at the Bedside. 2007 http://www.rwjf.org/pr/product.jsp?id=18662&topicid=1046&catid=24. [Google Scholar]
- Sermeus W, Bruyneel L. Brussels, Belgium: European Observatory on Health Systems and Policies; 2010. Investing in Europe’s health workforce of tomorrow: scope for innovation and collaboration: summary report of the three policy dialogues. http://www.healthworkforce4europe.ed/downloads/report_pd_leuven_final.pdf. [Google Scholar]
- Smith HL. A double sample to minimize bias due to non-response in a mail survey. In: Ruiz-Gazen A, Guilbert P, Haziza D, Tillé Y, editors. Survey Methods: Applications to Longitudinal Studies, to Health, to Electoral Studies and to Studies in Developing Countries. Dunod, Paris: 2008. pp. 334–339. [Google Scholar]
- Spetz J. Nurse satisfaction and the implementation of minimum nurse staffing regulations. Policy, Politics and Nursing Practice. 2008;9(1):15–21. doi: 10.1177/1527154408316950. [DOI] [PubMed] [Google Scholar]
- Spratley E, Johnson A, Sochalski J, Fritz M, Spencer W. Rockville, MD: U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions, Division of Nursing; 2000. The registered nurse population: findings from the National Sample Survey of Registered Nurses, March 2000. http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurvey2000.pdf. [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration. The registered nurse population: findings from the 2008 National Sample Survey of Registered Nurses, September 2010. 2010 http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf.
- Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Medical Care. 2004;42(2):57–66. doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bogaert P, Clarke S, Roelant E, Meulemans H, Van de Heyning P. Impacts of unit-level nurse practice environment and burnout on nurse-reported outcomes: a multilevel modelling approach. Journal of Clinical Nursing. 2010;19(11–12):1664–1674. doi: 10.1111/j.1365-2702.2009.03128.x. [DOI] [PubMed] [Google Scholar]
- Van den Heede K, Florquin M, Bruyneel L, Aiken L, Diya L, Lesaffre E, Sermeus W. Effective strategies for nurse retention in acute hospitals. International Journal of Nursing Studies. 2011 doi: 10.1016/j.ijnurstu.2011.12.001. Online early: http://dx.doi.org/10.1016/j.ijnurstu.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Warshawsky NE, Havens DS. Global use of the practice environment scale of the Nursing Work Index. Nursing Research. 2011;60(1):17–31. doi: 10.1097/NNR.0b013e3181ffa79c. [DOI] [PMC free article] [PubMed] [Google Scholar]