Abstract
Background:
Cranioplasty is a surgical intervention aimed at reestablishing the integrity of skull defects, and should be considered the conclusion of a surgical act that began with bone flap removal. Autologous bone is still considered the treatment of choice for cranioplasty. An alternative choice is bioceramic porous hydroxyapatite (HA) as it is one of the materials that meets and comes closest to the biomimetic characteristics of bone.
Methods:
The authors analyzed the clinical charts, compiled by the neurosurgeon, of all patients treated with custom-made porous HA devices (Custom Bone Service Fin-Ceramica, Faenza) from which epidemiological and pathological data as well as material-related complications were extrapolated.
Results:
From November 1997 to December 2010, 1549 patients underwent cranioplasty with the implantation of 1608 custom-made porous HA devices. HA was used in 53.8% of patients for decompressive craniectomy after trauma or intracranial hemorrhage, while the remaining cases were for treated for comminuted fracture, cutaneous or osseous resection, cranial malformation, autologous bone reabsorption or infection or rejection of previously implanted material. The incidence of adverse events in patients treated for cranioplasty, as first line treatment was 4.78% (56 events/1171 patients), and 5.02%, (19 events/378 patients) at second line.
Conclusion:
This study demonstrates that HA is a safe and effective material, is well tolerated in both adult and pediatric patients, and meets the requirements necessary to repair craniolacunia.
Keywords: Cranioplasty, customized cranioplasty, porous hydroxyapatite prosthesis
INTRODUCTION
Cranioplasty is a surgical intervention aimed at reestablishing the integrity of skull defects, usually because of previous craniotomy, and should be considered as the conclusion of a surgical act that began with bone flap removal. In the past 10 years, there has been an increase in the number of cranioplasties performed, reaching 20-25 per million inhabitants per year (Europe, Middle East and Africa, area), mainly due to an increase in the use of decompressive craniectomies.[33]
Autologous bone is still considered the treatment of choice for cranioplasty,[9,16] although it is not always available as it is sometimes abnormal. Moreover, cranioplasty is encumbered by increasingly restrictive and costly storage regulations, and finally, may be associated with a high incidence of resorption.[21] As a result, the use of heterologous or synthetic materials is required in an increasing number of cases. Such materials must have many characteristics such as biocompatibility, sterilizable, easy to design and manipulate shape, usable with stereolithography, compatible with diagnostic imaging, high impact strength and adequately heavy.
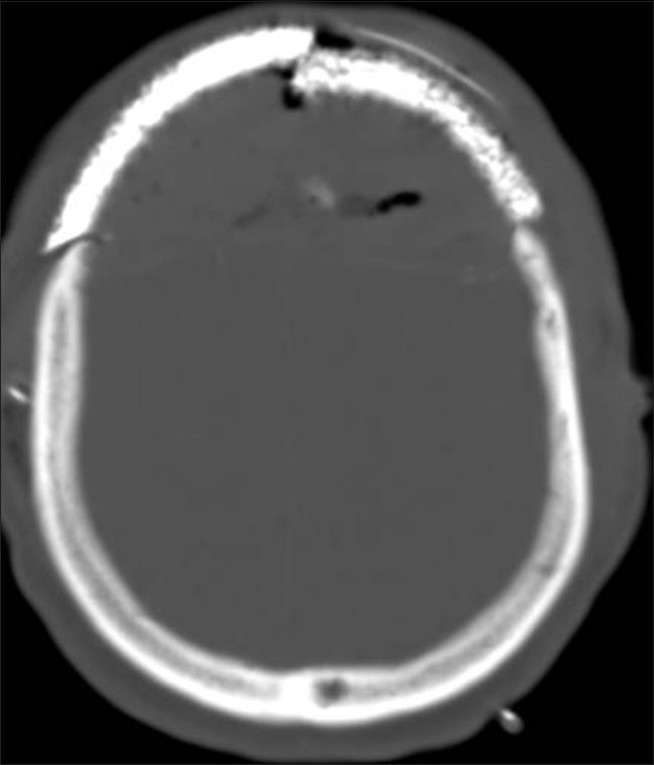
Bioceramic porous hydroxyapatite (HA) is one of the materials that meets these features and comes closest to the biomimetic characteristics of bone. Furthermore, due to its osteo-integrability it can interact with bone tissues without producing scar tissue [Figure 1].
Figure 1.
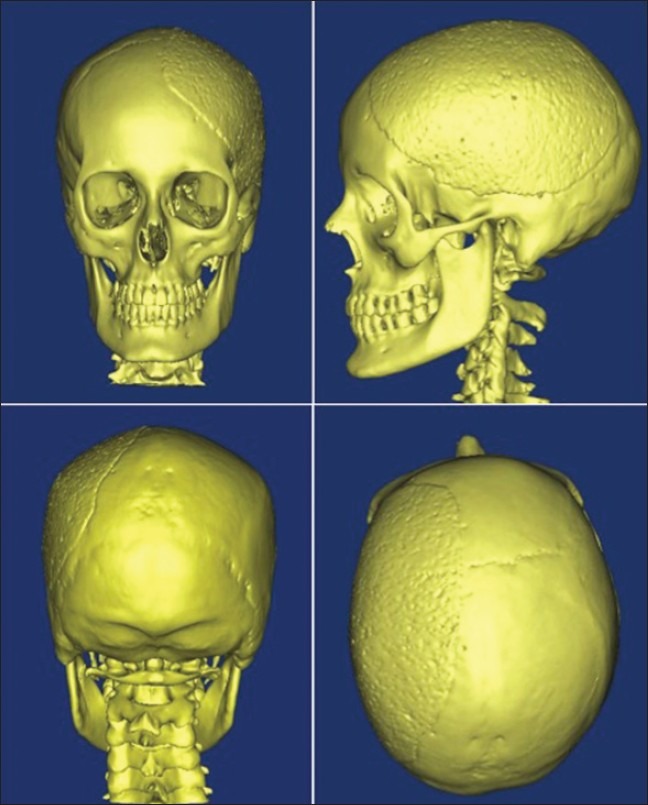
Fronto-temporo-parietal hydroxyapatite device with apparently good osteointegration
The present study reviews the worldwide case reports of cranioplasty using custom-made bioceramic porous HA, analyzing the number and type of complications directly or indirectly related to the material. This permits evaluation of the safety characteristics and identification of possible corrective suggestions in terms of design, validation, and surgical technique.
MATERIALS AND METHODS
Within the context of a research study, the University of Brescia entered into an agreement with Finceramica Company to gain access to data collection forms and patient data for the purposes of the investigation. The company provided the authors with all clinical charts of patients treated with custom-made porous HA devices (Custom Bone Service Fin-Ceramica, Faenza) compiled by the requesting neurosurgeon, from which epidemiological and pathological data as well as material-related complications were extrapolated.
All data collection forms, reporting immediate or long-term postoperative material-related complications collected by the company, were analyzed in accordance with postmarket clinical follow-up surveillance (PMCF) regulations as defined in Directive 93/42/EEC. The authors verified that the data were collected in full compliance with directives of the European Commission Directorate General for Health and Consumers that oversees periodic monitoring through contacts with all users of the devices.
To demonstrate the accuracy of these data, they were compared with the same data extrapolated from unsponsored studies: two already published and two unpublished studies. The unpublished data were provided by the Italian Society of Neurosurgery and the University of Leipzig (Germany).
In the first published study by Staffa,[34] a retrospective clinical series involved 51 patients with 4 adverse events and a postoperative follow-up characterized by “periodic control visits and CT scan at 6 months and 2 years”.
In the second published study by Hardy,[15] 8 patients were evaluated during the study period (from 1997 to 2008) using computed tomography (CT) scan to assess the ossification rate of HA and, as a secondary objective, to determine postoperative morbidity. No patients experienced adverse events.
The third study, unpublished, is a German study conducted by the University of Leipzig, a randomized clinical trial comparing HA versus titanium for craniofacial reconstruction. On December 31, 2010, 16 patients with a HA device were included, and there were no adverse events. The postoperative follow up visit was at 1 and 6 months, with an optional CT scan at 1 and 6 months.
The fourth study, unpublished, by Italian Neurosurgical Society (SINCH), is a prospective, multicentric, observational study in cranial lacunia reconstruction. On December 31, 2010, 48 patients were recruited and 1 adverse event was seen. The postoperative follow-up visits were at 3, 6, 12 months, and CT scan at 6 and 12 months.
Patients who underwent cranioplasty with custom-made porous HA devices were divided into two groups: group A, patients enrolled in four independent (unsponsored) clinical studies, and group B, including the remaining patients whose data were extracted from data collection forms provided to the author by the manufacturer. An inferential statistical analysis was performed to see if the two groups were homogeneous for comparison of the incidence of material-related complications between groups.
For the purposes of this study, complications were defined as any adverse postoperative event involving the implant such as fracture, infection, mobilization that did not allow it to fulfill its proper function. Adverse events related to surgery and irrelevant for the prosthesis function, such as postoperative hematoma, brain edema and ischemia, hydrocephalus, seizures or other reasons causing neurological deterioration were not taken into account.
The patients reported to the company were followed by continuous monitoring by the surgeon who implanted the device, who in case of material-related complications, reported these to the manufacturer. If a problem with the prosthesis arose, patients were required to contact their surgeon who then transmits that information to the manufacturer. No formal evaluation of patients was anticipated.
CHARACTERISTICS OF POUROUS HYDROXYAPATITE AND RATIONALE FOR ITS USE
HA is the main constituent of bone (60%) and thus its use as a prosthetic material appears obvious. HA shows excellent biocompatibility due to the absence of host immune reactions[2,25,30] or systemic/local toxicity.[5] Its composition, with a Ca/P ratio of 1.67, is comparable to that of natural bone (Ca/P ratio of 1.71) and causes accumulation of calcium and phosphate ions, which take part in the formation of new bone tissue on the surface of the implants.[32] However, chemical composition by itself is not sufficient to make HA an ideal substitute; in fact, the prosthetic material needs to be made porous so that osteoblastic cells can migrate inside it. Pores varying from 5 to 14 μm in size are necessary for fibrous tissue growth inside the prosthesis, whereas those varying from 40 to 100 μm in size are necessary for osteoblastic tissue growth. Finally, pores of at least 200 μm are needed for growth of a mature osteon. The prostheses used in this study, made of porous HA, have a high porosity (40-70% of total volume) and are characterized by pores of various sizes;[7,12] macropores with a diameter >200 μm (around 70-80% of the total) can also be identified. These are destined to house cells responsible for bone regeneration, with interconnection pores having a diameter in the 60-200 μm range, which are essential to provide adequate access to nutrients and physiological fluids to cells that colonize the prosthesis. Lastly, the prosthesis also has micropores with a diameter <10 ∝ m, which aid rapid hydration of the medical device. In this way, in addition to chemical mimicry, structural mimicry is also obtained. Experiments in animals[22] and the results of some clinical human explants[27] have revealed that osteoblast migration occurs from 4 to 8 months, after which time the prosthesis shows good perimetric osteointegration. During the first year of implant, the prosthesis has mechanical strength comparable to that of spongy bone by virtue of its porosity. Postfracture self-repairs, observed after the first year of implant, provide evidence of a process of osteointegration that can reach 60-80% of the total mass. However, these are only subjective assessments based on case reports, and not from the study of a homogeneous and statistically reliable population.
RESULTS
From November 1, 1997 to December 31, 2010, 1549 patients (991 male, 558 female) underwent cranioplasty with the implant of 1608 custom-made porous HA devices (Custom-Bone Service Fin-Ceramica, Faenza). Patient age ranged between 7 and 87 years with an average of 32 years. There were 114 pediatric patients who ranged in age from 7 to 14 years. The number of cranioplasties has gradually increased from one in 1997 and 1998, to 378 in 2010 [Figure 2].
Figure 2.
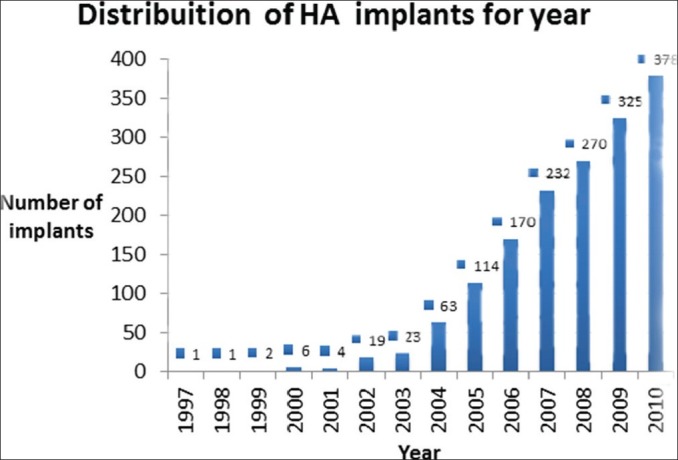
Distribution of hydroxyapatite devices over time
The implants were performed almost entirely in Europe; only 8 were implanted in the Middle East, 6 in Africa, 2 in Canada and 1 in Central America, 1 in Oceania, and 1 in South America. In Europe, the majority of prostheses were used in Italy (n = 717), followed by France (n = 322), and Germany (n = 204). Patients were recruited by 298 neurosurgical centers.
The number of defect localizations is showed in Table 1. HA was used in 833 (53.8%) patients due to decompressive craniectomy after trauma or intracranial hemorrhage, 104 (6.7%) after comminuted fracture, 173 (11.1%) after cutaneous or osseous resection, 31 (2.0%) for cranial malformation, 229 (14.8%) after autologous bone reabsorption or infection, 149 (9.6%) for rejection of previous implanted material and 30 (2%) for other causes. The size of the device ranged from 20 to 308 cm2.
Table 1.
Defect localization and infection related with the site of craniolacunia
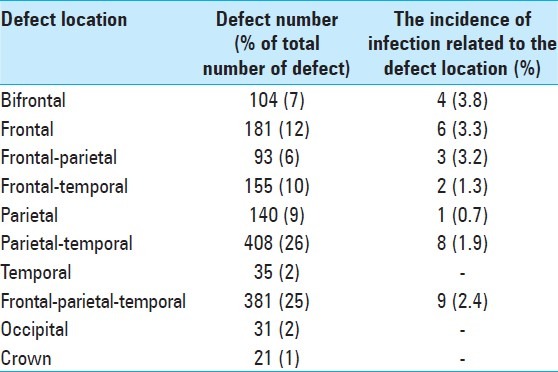
The different localizations are not correlated directly to the etiology of the initial event since the custom-bone was second-line treatment in 378 (24.4%) patients. Sixty-one patients had wide and complex lacunae and required a double prosthesis to reconstruct the necessary curvature; 51 of these (84%) were bifrontal lesions and 10 (16%) frontal-parietal-temporal. There were 72 (4.47%) postoperative adverse events (A-pO-event) as detailed in Table 2. Fourteen (0.8%) cases had complications that led to the selection of another material for a new cranioplasty or reject reoperation, leaving craniolacunia. Concerning the 27 cases of late fracture of the prosthesis, it was noticed that more extensive defects were associated with a greater risk of late fracture. The incidence of adverse events occurring in patients treated as first intention for cranioplasty was 4.78% (56 events/1171 patients) and at second intention was 5.02%, (19 events/378 patients). Thirty-three patients suffered from infections, mainly in those with head injury (27 patients) after decompressive craniectomy (23 patients). As is shown in Table 1, the largest incidence of infection was in patients with a bifrontal defect (3.8%).
Table 2.
Adverse post-operative material-related events
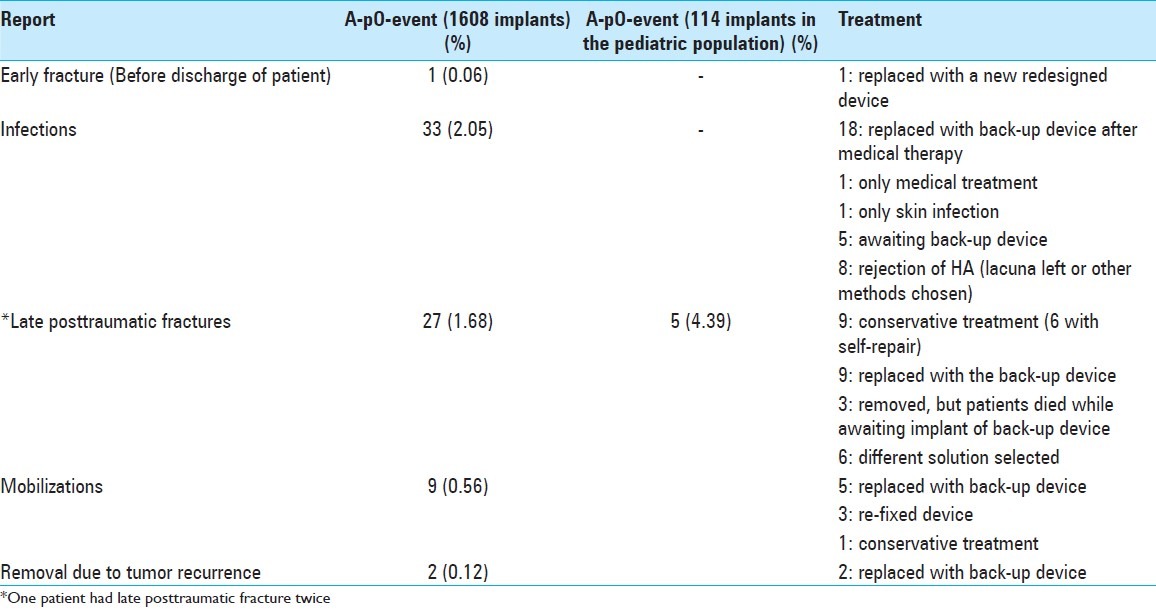
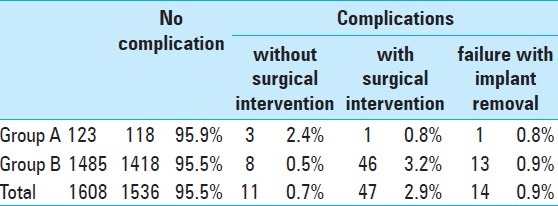
Mobilization of the prosthesis [Figure 3] perceived in four patients as micro-movements was due to breakage of the anchor stitches in two cases and to erroneous resting of the prosthesis on the undetached temporal muscle or periosteum in three patients; the dislocation seen in five patients, on the other hand, was caused by mechanical action of the underlying structures following intracranial hypertension (subdural hematoma or swelling of the brain) [Figure 4]. Dislocations and mobilizations were always correlated, however, with the technical problem of inadequate anchoring by stitches of the prosthesis to the skull [Figure 5].
Figure 3.
Spontaneous mobilization of the two devices to reconstruct the necessary curvature of bifrontal bone after removal
Figure 4.
Dislocation of the device due to brain swelling
Figure 5.

Technical note: Necessary to ensure adherence to the bone edge, which must be freshened to guarantee the maximum contact between the device and the cranium. The prosthesis is fixed with silk. It is not possible to use rigid fixing systems with this type of material, due to the risk of inducing micro-fractures in the prosthesis when it is still fragile. In the prosthesis design phase, it is required to indicate where to place the anchoring holes, dural, and muscular attachment. This is because once produced, the prosthesis can no longer be modified. The anchoring technique must be even more scrupulous in the case of extensive lacunae, which require two devices to reconstruct the necessary curvature
A characteristic intrinsic only to HA is the possibility of self repair after head trauma, all discovered a few years after the implant, which occurred in six patients.
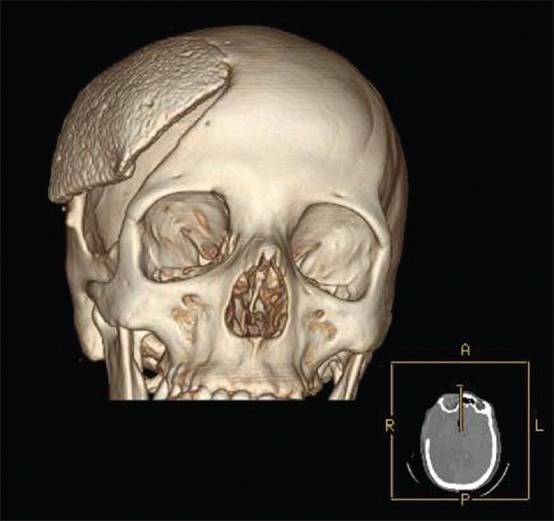
The time elapsed between cranioplasty and the onset of infection was as follows: less than 6 months (22 patients; 66%), within 6-12 months (2 patients; 6%), and after 1 year (9 patients; 28%). The material-related complications were divided [Table 3] into those managed without surgical intervention, such as infection using local treatment or fracture with self-repair, and those managed with surgical intervention with refixation of the prosthesis or use of a back-up device. Furthermore, we identified a number of patients in whom the implant had failed to close the skull and protect the brain, and consequently it was removed. Statistical analysis of groups A and B highlights that their characteristics are highly similar, thus allowing comparison of the incidence of complications.
Table 3.
Distribution of complications managed with or without surgery. Group A: patients enrolled in four independent (unsponsored) clinical trials and Group B: patients whose data were extracted by authors from clinical charts provided by the company
DISCUSSION
Autologous bone is still considered the first choice for repair of craniolacunia because of its good tolerability and favorable biological properties. However, its use presents some problems, yet unresolved, such as unavailability, resorption and unsatisfactory esthetic results in some cases. The unavailability of bone may be due to trauma with multi-fragmentary skull fractures that cannot be reconstructed and preserved, or to skull erosion due to lesions. Furthermore, the resorption of autologous bone can occur following repositioning at the cranial level and has a variable incidence in the literature ranging from 2% to 50%,[28,36] especially frequent in the pediatric population,[13,19] or can occur when the bone is preserved in subcutaneous adipose tissue at the abdominal level.[29] Finally, because of the dimensions of the operculum, which do not coincide with bone lacuna, the use of autologous bone can be encumbered by a lack of fusion and an unsatisfactory esthetic result. To overcome these problems, several safe and reliable materials have been developed in past decades that can be used in repair of craniolacunae, such as polymethylmethacrylate (PMMA),[23] titanium,[3,11] and porous polyethylene.[24]
This study analyzed the material-related complications using bioceramic custom-made porous HA. In this series, infection related to the material was seen in 2.05% of cases, which is comparable to the incidence of infections with other materials such as titanium (1.18%, range 0.7-4.5%),[11,18] and slightly better than PMMA prostheses (5.48%, range 9.1-3.3%).[4,8,23] More than 70% of infections occurred in the first year following the positioning of the biomaterial, and mainly due to existing pathogens or the presence of fistulas in frontal sinus. It has been suggested to treat the frontal sinus and skin coverage with maximal attention when the porous HA device is implanted. Infections occurred more frequently when the patient had head injury or wide craniolacunia, which can most likely be explained by the poorer clinical and neurological conditions. More extensive bone defects were also associated with poorer neurological conditions at the time of decompression. The incidence of infections (9%) in the case of cranioplasty performed after infection of the prosthesis was reassuring. Most likely, suitable antibiotic treatments and appropriate waiting times before a second cranioplasty were used at the neurosurgical centers involved.
Device fractures [Figure 6] occurred in a small number of implanted prostheses, defined as “spontaneous” (discovered during or just after surgical intervention) or “late” (occurring after discharge). In order to reduce the risk of fracture as much as possible, some thickness safety limits were introduced (6.5 mm ± 1.5 mm). Nonetheless, the initial fragility of the prosthesis still remains a problem that the surgeon must keep in mind. Adequate countermeasures, such as a detailed explanation to the patient and relatives to ensure a strict surveillance, should be considered mandatory. Late posttraumatic fractures of the prosthesis (27 of 1549 patients) showed an incidence of head trauma higher than that in a USA cohort (5 in 1000),[1] and may be related to the clinical and neurological status of the patient following the primary pathology and probable incomplete osteointegration. A clinical and neurological condition characterized by difficultly walking with or without assistance my favor easy falls. This also happened in postfracture self-repairs, that demonstrate an osteointegrative capacity[15,35] certainly with different magnitudes, sometimes accompanied by transformation of the prosthesis into an almost “viable” material of porous HA.
Figure 6.
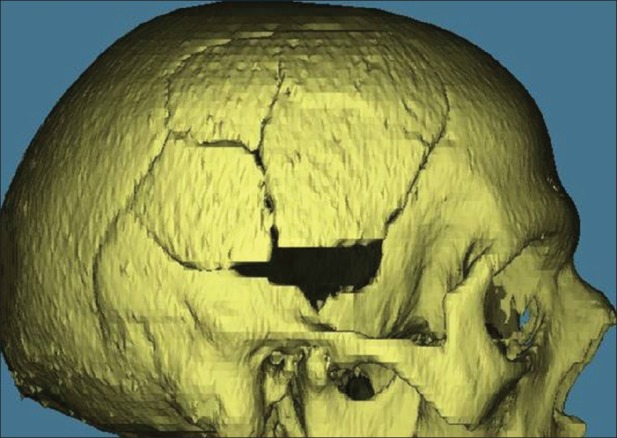
Posttraumatic device fracture
The need for reoperation to refix the prosthesis was inferior with custom-made HA compared with other materials, as shown in Table 4.
Table 4.
Literature review of surgical reintervention rates with implants made of different materials
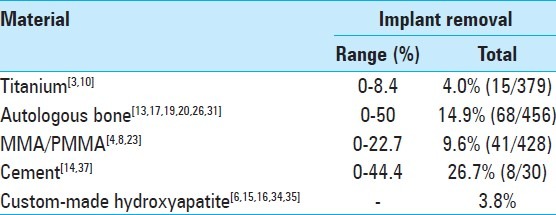
The removal of prefabricated implants [Table 4] varies in the literature depending on the material, with a mean value, respectively, of 4.4%, 9.6%, and 14.9% for titanium, MMA/PMMA, and autologous bone.[3,4,8,11,18,23] Porous HA custom-made bioceramic prostheses showed good reliability as they were removed in only 3.8% of cases. The reliability of the material was also demonstrated by the fact that, after having explanted the ceramic, the surgeon decided not to reuse it, but to use other materials or leave the craniolacunia in only 14 cases.
The slight difference existing between the percentage of adverse events in patients treated as first intention (4.78%) and second intention (5.02%) makes bioceramic porous HA, in our opinion, the material of choice in case of failure of another material, a situation that is often complex and which occurs in patients with a high number of comorbidities.
One limitation of the present study was the source of the data as it was provided by the company that manufactures the prosthesis and reliance on the surgeon for reporting all adverse events. The data are, however, monitored by annual inspections at the company by the Ministry of Italian Health that foresees periodic monitoring through contact with all users of the device. In addition, comparison of the data relative to complications in group A coming from retrospective and prospective studies performed at the national and international level[15,34] with group B, whose data are from the manufacturer, showed that the incidence of complications was 4.0% and 4.5%, respectively. Furthermore, the only two retrospective single-center series[16,35] have confirmed the reliability of the data from the manufacturer. Therefore, it can be argued that the neurosurgeons using this new material paid greater attention to monitoring patients.
Finally, there were no differences between material-related complications in pediatric and adult patients.
CONCLUSION
This extensive series of cranioplasties with a single material, previously unreported in the literature, demonstrates that porous HA is a safe and effective material that is well tolerated in both adult and pediatric patients, and that it meets the requirements necessary to repair craniolacunia. The initial fragility (lower strength) of the prosthesis has led to the design of a thicker prosthesis and to meticulous refinement of surgical technique, which the surgeon must be familiar with beforehand.
ACKNOWLEDGMENTS
The authors thank Dr. Nataloni Angelo of Fin-Ceramica Faenza S.p.A., responsible for clinical surveillance, for providing clinical data and Dr. Marco Fricia for providing the images.[37]
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/12/106290
Disclaimer:The authors Roberto Stefini and Franco Servadei received limited grants from Johnson and Johnson (sales company) for educational purposes and do not have any financial or patent-related interests with this company. The authors have never received any grants from Fin-Ceramica Faenza Company (Manufacturer Company) and do not have any financial or patent-related interests with the company
Contributor Information
Roberto Stefini, Email: roberto.stefini@alice.it.
Giacomo Esposito, Email: espositogiacomo82@tiscali.it.
Bruno Zanotti, Email: bruno.zanotti@rivistamedica.com.
Corrado Iaccarino, Email: ciaccarino@ao.pr.it.
Marco Maria Fontanella, Email: marco.fontanella@tin.it.
Franco Servadei, Email: fservadei@ao.pr.it.
REFERENCES
- 1.Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998-2000. Brain Inj. 2005;19:85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- 2.Boyde A, Corsi A, Quarto R, Cancedda R, Bianco P. Osteoconduction in large macroporous hydroxyapatite ceramic implants: Evidence for a complementary integration and disintegration mechanism. Bone. 1999;24:579–89. doi: 10.1016/s8756-3282(99)00083-6. [DOI] [PubMed] [Google Scholar]
- 3.Cabraja M, Klein M, Lehmann TN. Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus. 2009;26:E10. doi: 10.3171/2009.3.FOCUS091. [DOI] [PubMed] [Google Scholar]
- 4.Chiarini L, Figurelli S, Pollastri G, Torcia E, Ferrari F, Albanese M, et al. Cranioplasty using acrylic material: A new technical procedure. J Craniomaxillofac Surg. 2004;32:5–9. doi: 10.1016/j.jcms.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Chistolini P, Ruspantini I, Bianco P, Corsi A, Cancedda R, Quarto R. Biomechanical evaluation of cell-loaded and cell-free hydroxyapatite implants for the reconstruction of segmental bone defects. J Mater Sci Mater Med. 1999;10:739–42. doi: 10.1023/a:1008939524807. [DOI] [PubMed] [Google Scholar]
- 6.Cordaro ER, Calabrese S, Faini GP, Zanotti B, Verlicchi A, Parodi PC. Method to thicken the scalp in calvarian reconstruction. J Craniofac Surg. 2011;22:598–601. doi: 10.1097/SCS.0b013e3182077dca. [DOI] [PubMed] [Google Scholar]
- 7.Denissen H, Martinetti R, van Lingen A, van den Hooff A. Normal osteoconduction and repair in and around submerged highly bisphosphonate-complexed hydroxyapatite implants in rat tibiae. J Periodontol. 2000;71:272–8. doi: 10.1902/jop.2000.71.2.272. [DOI] [PubMed] [Google Scholar]
- 8.D’Urso PS, Earwaker WJ, Barker TM, Redmond MJ, Thompson RG, Effeney DJ, et al. Custom cranioplasty using stereolithography and acrylic. Br J Plast Surg. 2000;53:200–4. doi: 10.1054/bjps.1999.3268. [DOI] [PubMed] [Google Scholar]
- 9.Edwards MS, Ousterhout DK. Autogeneic skull bone grafts to reconstruct large or complex skull defects in children and adolescents. Neurosurgery. 1987;20:273–80. doi: 10.1227/00006123-198702000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Eufinger H, Rasche C, Lehmbrock J, Wehmöller M, Weihe S, Schmitz I, et al. Performance of functionally graded implants of polylactides and calcium phosphate/calcium carbonate in an ovine model for computer assisted craniectomy and cranioplasty. Biomaterials. 2007;28:475–85. doi: 10.1016/j.biomaterials.2006.08.055. [DOI] [PubMed] [Google Scholar]
- 11.Eufinger H, Wehmoller M. Individual prefabricated titanium implants in reconstructive craniofacial surgery: Clinical and technical aspects of the first 22 cases. Plast Reconstr Surg. 1998;102:300–8. doi: 10.1097/00006534-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Fabbri M, Celotti GC, Ravaglioli A. Hydroxyapatite-based porous aggregates: Physico-chemical nature, structure, texture and architecture. Biomaterials. 1995;16:225–8. doi: 10.1016/0142-9612(95)92121-l. [DOI] [PubMed] [Google Scholar]
- 13.Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg. 2004;100(2 Suppl Pediatrics):163–8. doi: 10.3171/ped.2004.100.2.0163. [DOI] [PubMed] [Google Scholar]
- 14.Greenberg BM, Schneider SJ. Alloplastic reconstruction of large cranio-orbital defects: A comparative evaluation. Ann Plast Surg. 2005;55:43–51. doi: 10.1097/01.sap.0000168157.10664.9c. discussion 51. [DOI] [PubMed] [Google Scholar]
- 15.Hardy H, Tollard E, Derrey S, Delcampe P, Péron JM, Fréger P, et al. Clinical and ossification outcome of custom-made hydroxyapatite prothese for large skull defect. Neurochirurgie. 2012;58:25–9. doi: 10.1016/j.neuchi.2011.09.006. (Article in French) [DOI] [PubMed] [Google Scholar]
- 16.Iaccarino CR, Ghadipour R, Carinci F, Servadei F. Porous hydroxyapatite custom made cranioplasty: The 3d design techniques prosteses in 21 patients. J Osteol Biomater. 2011;2:43–53. [Google Scholar]
- 17.Iwama T, Yamada J, Imai S, Shinoda J, Funakoshi T, Sakai N. The use of frozen autogenous bone flaps in delayed cranioplasty revisited. Neurosurgery. 2003;52:591–6. doi: 10.1227/01.neu.0000047891.86938.46. discussion 595-6. [DOI] [PubMed] [Google Scholar]
- 18.Joffe J, Harris M, Kahugu F, Nicoll S, Linney A, Richards R. A prospective study of computer-aided design and manufacture of titanium plate for cranioplasty and its clinical outcome. Br J Neurosurg. 1999;13:576–80. doi: 10.1080/02688699943088. [DOI] [PubMed] [Google Scholar]
- 19.Josan VA, Sgouros S, Walsh AR, Dover MS, Nishikawa H, Hockley AD. Cranioplasty in children. Childs Nerv Syst. 2005;21:200–4. doi: 10.1007/s00381-004-1068-2. [DOI] [PubMed] [Google Scholar]
- 20.Kiyokawa K, Hayakawa K, Tanabe HY, Inoue Y, Tai Y, Shigemori M, et al. Cranioplasty with split lateral skull plate segments for reconstruction of skull defects. J Craniomaxillofac Surg. 1998;26:379–85. doi: 10.1016/s1010-5182(98)80071-1. [DOI] [PubMed] [Google Scholar]
- 21.Kline RM, Wolfe SA. Complications associated with the harvesting of cranial bone grafts. Plast Reconstr Surg. 1995;95:5–13. discussion 14-20. [PubMed] [Google Scholar]
- 22.Kon E, Muraglia A, Corsi A, Bianco P, Marcacci M, Martin I, et al. Autologous bone marrow stromal cells loaded onto porous hydroxyapatite ceramic accelerate bone repair in critical-size defects of sheep long bones. J Biomed Mater Res. 2000;49:328–37. doi: 10.1002/(sici)1097-4636(20000305)49:3<328::aid-jbm5>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 23.Lee SC, Wu CT, Lee ST, Chen PJ. Cranioplasty using polymethyl methacrylate prostheses. J Clin Neurosci. 2009;16:56–63. doi: 10.1016/j.jocn.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Liu JK, Gottfried ON, Cole CD, Dougherty WR, Couldwell WT. Porous polyethylene implant for cranioplasty and skull base reconstruction. Neurosurg Focus. 2004;16:ECP1. doi: 10.3171/foc.2004.16.3.14. [DOI] [PubMed] [Google Scholar]
- 25.Marcacci M, Kon E, Zaffagnini S, Giardino R, Rocca M, Corsi A, et al. Reconstruction of extensive long-bone defects in sheep using porous hydroxyapatite sponges. Calcif Tissue Int. 1999;64:83–90. doi: 10.1007/s002239900583. [DOI] [PubMed] [Google Scholar]
- 26.Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien) 2006;148:535–40. doi: 10.1007/s00701-006-0740-6. discussion 540. [DOI] [PubMed] [Google Scholar]
- 27.Messina G, Dones I, Nataloni A, Franzini A. Histologically demonstrated skull bone integration in a hydroxyapatite prosthesis in a human. Acta Neurochir (Wien) 2011;153:1717–8. doi: 10.1007/s00701-011-1014-5. [DOI] [PubMed] [Google Scholar]
- 28.Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V. Clinical outcome in cranioplasty: Critical review in long-term follow-up. J Craniofac Surg. 2003;14:144–53. doi: 10.1097/00001665-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Movassaghi K, Ver Halen J, Ganchi P, Amin-Hanjani S, Mesa J, Yaremchuk MJ. Cranioplasty with subcutaneously preserved autologous bone grafts. Plast Reconstr Surg. 2006;117:202–6. doi: 10.1097/01.prs.0000187152.48402.17. [DOI] [PubMed] [Google Scholar]
- 30.Olmi RM, Ravaglioni A, Krajewski A, Pizzoferrato A. Impianti di idrossiapatite in femori di conigli. Osservazioni istologiche e microradiografiche. Chir Organi Mov. 1984;69:383–90. [PubMed] [Google Scholar]
- 31.Park JS, Shim JJ, Yoon SM, Choi WR, Doh JW. Large defect may cause infectious complications in cranioplasty. J Korean Neurol Soc. 2007;42:89–91. [Google Scholar]
- 32.Rawlings CE. Modern bone substitutes with emphasis on calcium phosphate ceramics and osteoinductors. Neurosurgery. 1993;33:935–8. doi: 10.1227/00006123-199311000-00027. [DOI] [PubMed] [Google Scholar]
- 33.Servadei F. Clinical value of decompressive craniectomy. N Engl J Med. 2011;364:1558–9. doi: 10.1056/NEJMe1102998. [DOI] [PubMed] [Google Scholar]
- 34.Staffa G, Barbanera A, Faiola A, Fricia M, Limoni P, Mottaran R, et al. Custom made bioceramic implants in complex and large cranial reconstruction: A two-year follow-up. J Craniomaxillofac Surg. 2012;40:e65–70. doi: 10.1016/j.jcms.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 35.Staffa G, Nataloni A, Compagnone C, Servadei F. Custom made cranioplasty prostheses in porous hydroxy-apatite using 3D design techniques: 7 years experience in 25 patients. Acta Neurochir (Wien) 2007;149:161–70. doi: 10.1007/s00701-006-1078-9. discussion 170. [DOI] [PubMed] [Google Scholar]
- 36.Yap C, Macarthur DC, Hope DT. ‘Mind the gap’: Resorption of a bone flap stored subcutaneously for 6 months. Br J Neurosurg. 2002;16:523–4. doi: 10.1080/0268869021000030951. [DOI] [PubMed] [Google Scholar]
- 37.Zins JE, Papay FA. Use of calcium-based bone cements in the repair of large, full-thickness cranial defects: A caution. Plast Reconstr Surg. 2007;120:1332–42. doi: 10.1097/01.prs.0000279557.29134.cd. [DOI] [PubMed] [Google Scholar]


