Abstract
Background:
Ventricular shunts are used to drain cerebrospinal fluid into extra-cranial spaces. Ventriculoatrial (VA) shunts are provided to transfer cerebrospinal fluid from the cerebral ventricle into the right atrium of the heart. A single center experience of indications, procedure, and clinical outcomes in VA shunt was presented in current study.
Methods:
VA shunts were applied in 10 patients who had repeated previous shunt dysfunction or infection. The reasons, clinical findings, replacement methods, and postoperative clinical follow-ups and outcomes were recorded retrospectively.
Results:
There were seven female (70%) and three (30%) male patients; their ages ranged from 5 to 13 years (mean ± SD; 8.5 ± 2.6 years). Shunt re-placement reasons were as follows: Shunt occlusion in five patients, intraperitoneal infection in four patients and a distal catheter was kinked and knotted in one patient. Postoperative early complications were seen in one patient as early catheter thrombosis and catheter revision were applied. Late complications were seen in two patients as follows: Catheter infection and infective endocarditis occurred in one patient and pulmonary thrombus occurred in one other patient. There was not any catheter-related mortality observed at the one year follow-up period.
Conclusion:
VA shunts may be an option for cerebrospinal fluid drainage at necessary conditions. However, sterilization and general training on asepsy and antisepsy are the most important determinants affecting the clinical outcome due to the cardio systemic relationship.
Keywords: Infection, outcome, thrombosis, ventriculoatrial shunts
INTRODUCTION
There are limited options for continuous cerebrospinal fluid drainage. The ventriculoperitoneal (VP) option is more popular than ventriculoatrial (VA) shunts. However, shunt revisions may be required due to shunt infection, obstruction, and migration conditions in VP shunts. In such special events, VA shunts may be an appropriate option for continuous cerebrospinal fluid drainage.[4,5,11] The intraoperative appropriate vein selection and exact shunt placement is important to reduce complications such as obstruction.[4]
Placement strategies and monitoring methods have been improved to achieve more success in VA shunt catheter replacement.[4,8] In the present study, reasons, protocols, and clinical outcomes of VA catheter placements were reported in 10 patients.
MATERIALS AND METHODS
A VA shunt operation was applied in 10 patients who suffered from hydrocephaly; this was done with the collaboration of the departments of neurosurgery and cardiovascular surgery. Age, gender, reasons, complications, additional applications, and clinical outcomes were evaluated retrospectively.
Preoperative scopy scans were applied to monitor the venoatrial route in each patient.
RESULTS
There were seven female (70%) and three (30%) male patients (female to male ratio, 2.3:1). The ages ranged from 5 to 13 years (mean ± SD; 8.5 ± 2.6 years). All patients were diagnosed with hydrocephalus on neurological verification. A VP shunt was applied previously in all patients.
Repetition of hydrocephalus complaints were detected in six patients. Repeated catheter obstruction was determined in five of the six patients. A kinked and knotted catheter was detected in one patient. Fever, abdominal tenderness, and elevated infection markers were detected in other four patients. These four patients were diagnosed with peritonitis.
The ventricular side of catheters was placed by neurosurgeons. After that, neck dissection was performed with a parallel longitudinal incision to the sternocleidomastoid muscle by cardiovascular surgeons. Just behind the muscle, the internal jugular vein was explored and evaluated with its branches. If an appropriate branch was detected, a catheter was placed in the branch. If an appropriate branch was not detected (e.g., too narrow for the catheter's diameter), the catheter was placed in the main body of the internal jugular vein. Before replacement the purse sutures were added to prevent migration and bleeding into the vein. The placement of catheter was demonstrated in Figure 1.
Figure 1.
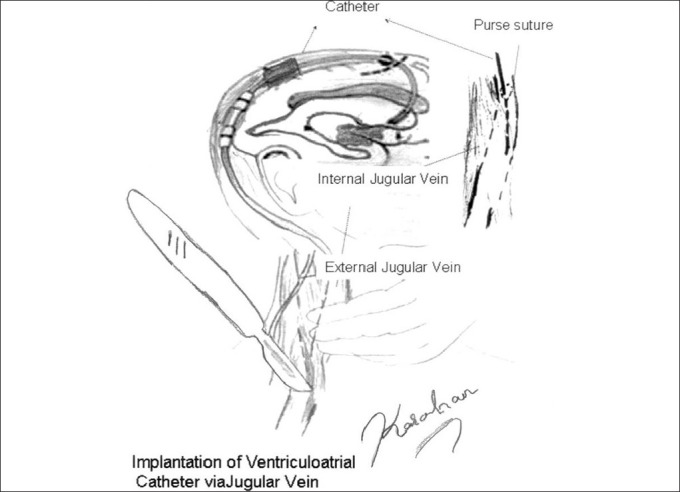
The demonstration of ventriculoatrial catheter implantation
All patients were followed postoperatively for one year. Early complications of catheter thrombosis were seen in one patient on the 15th day following operation. Catheter revision and anticoagulant therapy (0.5 mg/kg enoxaparine prophylaxis was administered) were applied in this patient and no secondary thrombosis was observed. Late complications were seen in two patients as follows: In the first patient, probable catheter-related methicillin-resistant Staphylococcus aureus bacteremia and infective endocarditis were detected in blood cultures the second month after the operation. The catheter was removed urgently and appropriate antibiotherapies (Vancomycin 1 gram IV + Gentamycin 1.5 mg/kg IV) were administered to the patient, according to current literature suggestions.[6] The removal of catheter cultures confirmed the diagnosis. The blood parameters and fever returned to normal ranges after one week of antibiotherapy.
In the second patient, dyspnea and sweating occurred at the postoperative 162nd day. A high resolution computed tomography scan revealed pulmonary thrombus on the small pulmonary artery branches. The catheter was removed immediately and rapid anticoagulation and antiagregant therapy (25000-50000 IU continuous intravenous unfractionated heparin infusion with a partial thromboplastin time (PTT) monitorization in the first two days, 1 mg/kg enoxaparine and 100 mg daily acetylsalicylic acid maintenance therapy was started after two days) was initiated in the patient presenting with pulmonary thromboemboly. The thrombosis treatment was applied with the guidance of the current literature.[10,15] The respiratory complaints were recovered after the first two days of treatment.
There were no additional catheter-related events detected during the follow-up period. Additionally, catheter related mortalities were not observed during the one year follow-up period.
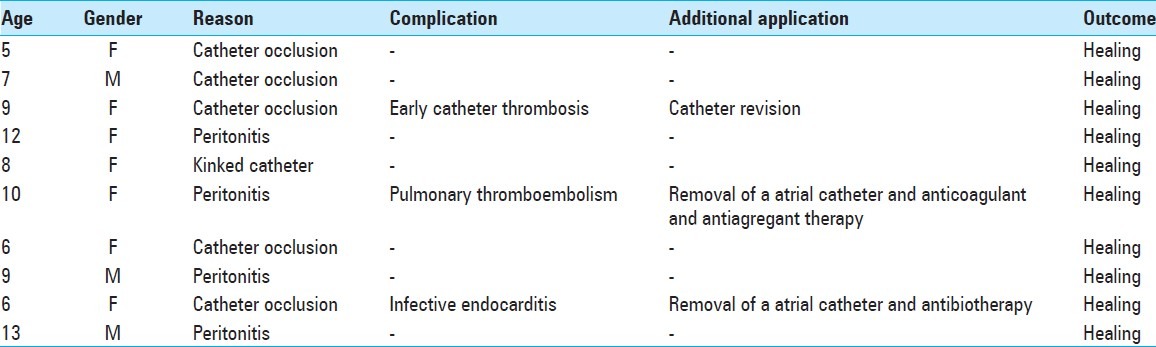
The details of the cases are summarized in Table 1.
Table 1.
Demographic data of ventriculoatrial shunt applications
DISCUSSION
The VP shunts provides a prolonged relief of intracranial pressure, and it is quite easily to be performed. The major limitation is catheter dysfunction in this treatment method. Catheter dysfunction reasons can be listed as follows: Shunt infection, valve obstruction, catheter migration, shunt disconnection, kinked catheter (malposition), or any combination of these reasons. This problem is emergency-like situation that can be lead to mortalities. However, it can be treatable and also, the risk is reduced in shunt-related complications with recent advances in surgical technique and shunt design.[17] In contrast, VA shunts became the standard treatment for intracranial hypertension due to hydrocephalus since 1952. Furthermore, over the subsequent years, the favorable intervention led to notable concerns with the recognition of various range of severe and even life-threatening complications that closely related to the circulatory system.[16] Recent reports suggest that despite VP shunts being the most preferred method; there is a notable patient population that remains where VA shunt is needed.[16] VA shunts may be good option for the desired result cannot be achieved recurrent VP cases in experienced hands. Also, minimal invasive methods and radiographic guidance's are developed for VA shunts too.[12] Thus, VA shunts are important alternative to VP shunts in selected cases.[7] However, complications should not be neglected that range from something simple like an occlusion to other more significant problems like bacteremias and cardiac disorders due to cardiac placement and systemic drainage.[2,7,14]
Therefore, new placement strategies and monitoring methods have been improved to achieve more success and reduced complications in VA shunt catheter replacement.[4,8,9] Chuang, et al. reported the use of percutaneous VA placement with real-time transesophageal echocardiogram monitoring. They claimed that this method can be used less invasively, as well as more accurately, quickly and safely.[4] Endovascular placement of a VA shunt was presented by Gonzales, et al., who reported three advantages of this technique: The venous system can be identified easily, the jugular vein patency can be demonstrated clearly, and the true placement or malposition of the catheter can be determined quickly.[8] In another study, a ventriculosubgaleal shunt was mentioned by Hansasuta, et al., who claimed that this approach is simple and inexpensive.[9] Metellus, et al. also reported that percutaneous placement of a VA shunt with radiographic guidance improves the effectivity and safety of the technique.[12] Ten patients who had previous shunt dysfunction were presented in our report. VA shunts were performed with the guidance of scopy in these patients. Only one catheter obstruction was detected. Catheter thrombosis was determined at the postoperative 15th day in this patient. Additional occlusion and malposition were not observed.
VA shunt approaches may cause potentially life threatening complications. Obstructions, malpositions, and shunt infections are the most frequent problems in VA shunts.[4,13,14] Numerous complications have been reported in the literature and most of them could have been treated or prevented. For example, Elhammady, et al. reported a VA shunt displacement in a case with a partial anomalous pulmonary venous return. They suggested that radiographic evidences are beneficial for the management and treatment of such variations and further scans such as computed tomography should be applied in suspected cases.[7] Arıbas, et al . reported pulmonary hypertension development in a case following a VA shunt implantation. Pulmonary perfusion scintigraphy revealed segmental and subsegmental perfusion defects in this case. They removed the VA shunt and it was replaced with a VP shunt.[1] Cardiac complications can occur during or after VA shunt implantation as Natarajan, et al. reported a case of a 57-year-old male patient who was treated for pneumonia and new-onset atrial fibrillation. According to their report, the patient had a VA shunt since childhood that was implanted for hydrocephalus and there he had no additional health problems. To sum up, they diagnosed catheter-related right heart complications, such as significant calcific tricuspid stenosis and a dilated right atrium that was revealed in transthoracic echocardiography.[14] Ben-Ami, et al. reported a catheter related Gram-positive bacteremia and nephritis in a 47-year-old woman who had a VA shunt for 10 years due to hydrocephalus. The VA shunt was removed; then, vancomycin therapy was started and a new VP shunt was inserted in this case. According to the report, the patient fully recovered.[2] Chaw, et al. reported infective endocartitis in one VA shunt case. They claimed that appropriate treatment should be applied with the removal of foreign material in such cases.[3]
In our study, we implanted all of the VA shunt catheters under scopy scans to appropriately position them in the right atrium. An early catheter revision was made in one patient due to catheter occlusion 15 days following operation. Presumptive diagnoses of catheter-related methicillin-resistant Staphylococcus aureus bacteremia and infective endocarditis were detected in one patient at the second month of application. The catheter was removed urgently and appropriate antibiotherapies (vancomycin 1 g IV + Gentamycin 1.5 mg/kg IV) were administered. The patient fully recovered after therapy. Dyspnea and sweating occurred in another patient at the 162nd day of implantation. A high resolution computed tomography scan revealed pulmonary thrombus on the small pulmonary artery branches. As a result, the catheter was removed immediately and rapid anticoagulation and antiagregant therapy was initiated, and the patient's respiratory complaints were recovered after two days of treatment. Additional catheter-related morbidity and mortality were not observed at the one-year follow-up period.
VA shunts are indispensable options for cerebrospinal fluid drainage in hydrocephalus. However, they may have preventable and treatable life threatening complications. Radiographic or ultrasonographic examinations may have improved outcomes with collaborative study. Nevertheless, all these complications can be cured if appropriately treated with the strict adherence to advanced guidelines. Therefore, reasons, complications, and outcomes should be clearly stated.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/10/106284
Contributor Information
Celal Yavuz, Email: celalyav@hotmail.com.
Sinan Demırtas, Email: sinandemirtas78@hotmail.com.
Ahmet Calıskan, Email: drahmetcaliskan@hotmail.com.
Kaan Kamasak, Email: drkaankamasak@hotmail.com.
Oguz Karahan, Email: oguzk2002@gmail.com.
Orkut Guclu, Email: drorkut@gmail.com.
Suleyman Yazıcı, Email: yazici.suleyman@hotmail.com.
Binali Mavıtas, Email: vasculoceptor@gmail.com.
REFERENCES
- 1.Arıbas A, Akıllı H. Development of pulmonary hypertension after ventriculoatrial shunt implantation. Eur J Gen Med. 2011;8:345–7. [Google Scholar]
- 2.Ben-Ami R, Navon-Venezia S, Schwartz D, Carmeli Y. Infection of a ventriculoatrial shunt with phenotypically variable Staphylococcus epidermidis masquerading as polymicrobial bacteremia due to various coagulase-negative Staphylococci and Kocuria varians. J Clin Microbiol. 2003;41:2444–7. doi: 10.1128/JCM.41.6.2444-2447.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaw HY, Buxton N, Wong PS. Staphylococcal endocarditis with a ventriculo-atrial shunt. J R Soc Med. 2004;97:182–3. doi: 10.1258/jrsm.97.4.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chuang HL, Chang CN, Hsu JC. Minimally invasive procedure for ventriculoatrial shunt-combining a percutaneous approach with real-time transesophageal echocardiogram monitoring: Report of six cases. Chang Gung Med J. 2002;25:62–6. [PubMed] [Google Scholar]
- 5.Chung JJ, Yu JS, Kim JH, Nam SJ, Kim MJ. Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol. 2009;193:1311–7. doi: 10.2214/AJR.09.2463. [DOI] [PubMed] [Google Scholar]
- 6.Cosgrove SE, Fowler VG., Jr Management of Methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46:386–93. doi: 10.1086/533595. [DOI] [PubMed] [Google Scholar]
- 7.Elhammady MS, Benglis DM, Bhatia S, Sandberg DI, Ragheb J. Ventriculoatrial shunt catheter displacement in a child with partial anomalous pulmonary venous return: Case report. J Neurosurg Pediatr. 2008;2:68–70. doi: 10.3171/PED/2008/2/7/068. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez LF, Kim L, Rekate HL, McDougall CG, Albuquerque FC. Endovascular placement of a ventriculoatrial shunt. Technical note. J Neurosurg. 2007;106:319–21. doi: 10.3171/ped.2007.106.4.319. [DOI] [PubMed] [Google Scholar]
- 9.Hansasuta A, Boongird A. Ventriculo-subgaleal shunt: Step-by-step technical note. J Med Assoc Thai. 2007;90:473–8. [PubMed] [Google Scholar]
- 10.Hirsh J, Anand SS, Halperin JL, Fuster V American Heart Association. Guide to anticoagulant therapy: Heparin: A statement for healthcare professionals from the American Heart Association. Circulation. 2001;103:2994–3018. doi: 10.1161/01.cir.103.24.2994. [DOI] [PubMed] [Google Scholar]
- 11.Kim JS, Park YW, Kim HK, Cho YS, Kim SS, Youn NR, et al. Is percutaneous endoscopic gastrostomy tube placement safe in patients with ventriculoperitoneal shunts? World J Gastroenterol. 2009;15:3148–52. doi: 10.3748/wjg.15.3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metellus P, Hsu W, Kharkar S, Kapoor S, Scott W, Rigamonti D. Accuracy of percutaneous placement of a ventriculoatrial shunt under ultrasonography guidance: A retrospective study at a single institution. J Neurosurg. 2009;110:867–70. doi: 10.3171/2008.10.17674. [DOI] [PubMed] [Google Scholar]
- 13.Nash DL, Schmidt K. Complications and management of ventriculoatrial (VA) shunts, a case report. Cerebrospinal Fluid Res. 2010;7(Suppl 1):S42. [Google Scholar]
- 14.Natarajan A, Mazhar S. Right heart complications of ventriculoatrial shunt. Eur Heart J. 2011;32:2134. doi: 10.1093/eurheartj/ehr164. [DOI] [PubMed] [Google Scholar]
- 15.Rondina MT, Wheeler M, Rodgers GM, Draper L, Pendleton RC. Weight-based dosing of enoxaparin for VTE prophylaxis in morbidly obese, medically-Ill patients. Thromb Res. 2010;125:220–3. doi: 10.1016/j.thromres.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vernet O, Rilliet B. Late complications of ventriculoatrial or ventriculoperitoneal shunts. Lancet. 2001;358:1569–70. doi: 10.1016/S0140-6736(01)06670-3. [DOI] [PubMed] [Google Scholar]
- 17.Zhang J, Qu C, Wang Z, Wang C, Ding X, Pan S, et al. Improved ventriculoatrial shunt for cerebrospinal fluid diversion after multiple ventriculoperitoneal shunt failures. Surg Neurol. 2009;72:29–33. doi: 10.1016/j.surneu.2008.03.040. [DOI] [PubMed] [Google Scholar]


