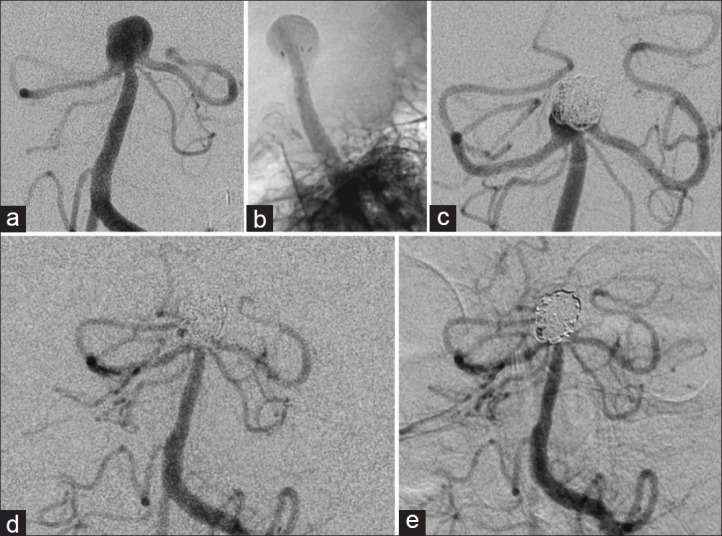
Abstract
Background:
Large wide-necked arterial bifurcation aneurysms present a unique challenge for endovascular coil embolization treatment. One technique described in the literature deploys a Neuroform stent into the neck of the aneurysm in the shape of a waffle-cone, thereby acting as a scaffold for the coil mass. This case series presents four patients with large wide-necked bifurcation aneurysms treated with the closed-cell Enterprise stent using the waffle-cone technique.
Case Description:
Four patients (59 ± 18 years of age) with large wide-necked arterial bifurcation aneurysms (three basilar apex and one MCA bifurcation) were treated with the waffle-cone technique using the Enterprise stent as a supporting device for stent-assisted coil embolization. Three of the patients presented with aneurysmal subarachnoid hemorrhage (Hunt-Hess 2-3; Fisher Grade 3-4). There was no procedural morbidity or mortality associated with treatment itself. One aneurysm was completely obliterated, and three had small residual necks. One patient developed an area of PCA infarct and visual field cut one month after the procedure and required recoiling of the residual neck. The flared ends of the Enterprise stent remodeled the aneurysm neck by conforming to the shape of the neck without any technical difficulty, resulting in a stable scaffold holding the coils into the aneurysm.
Conclusion:
The closed cell construction, flexibility, and flared ends of the Enterprise stent allow it to conform to the waffle-cone configuration and provide a stable scaffold for coil embolization of large wide-necked arterial bifurcation aneurysms. We have had excellent initial results using the Enterprise stent with the waffle-cone technique. However, this technique is higher risk than standard treatment methods and therefore should be reserved for large wide-necked bifurcation aneurysms where Y stenting is needed, but not possible, and surgical clip ligation is not an option.
Keywords: Aneurysm, coil, embolization, enterprise, stent, waffle-cone, wide-necked
INTRODUCTION
Coil loop extrusion from the neck of large, wide-necked arterial bifurcation aneurysms poses a challenge for endovascular treatment in part because they can occlude the parent vessel or its branches.[6] Several techniques have been developed to overcome this problem, one of which is waffle-coning, initially described using the open-celled Neuroform stent and named for the appearance of the flared distal end within the aneurysm fundus.[4] The procedure deploys a stent within the confines of the aneurysm neck, thus acting as a scaffold to support the coil mass and protect parent branches from occlusion.
The Enterprise, a flexible closed-cell stent, was designed to bridge the opening of wide-necked aneurysms during stent-assisted coiling. Additionally, the closed-cell design allows for retrieval of partially deployed stents, thereby improving precise positioning.[3,7] Recently, there was a single case report describing the successful deployment of the Enterprise stent in the waffle-cone configuration of a large basilar trunk aneurysm.[2] This stenting technique can be potentially used in any large wide-necked arterial bifurcation aneurysm in which multiple branches originate from the aneurysm neck, making it difficult to protect against coil extrusion and distal arterial occlusion. We describe our initial experience using the Enterprise for stent-assisted waffle-cone coil embolization of wide-necked aneurysms in a series of four patients, three with basilar apex aneurysms (two ruptured, one unruptured) and the fourth being an MCA bifurcation aneurysm.
CASE REPORTS
Approval from SUNY Upstate Institutional Review Board was obtained to review these cases. All patients [Table 1] signed informed consent for the specific use of the Enterprise stent and another for stent-assisted coil embolization of the intracranial aneurysm.
Table 1.
Aneurysm characteristics of all patients treated with stent-assisted coil embolization using the enterprise stent in the waffle-cone configuration
Waffle-cone technique
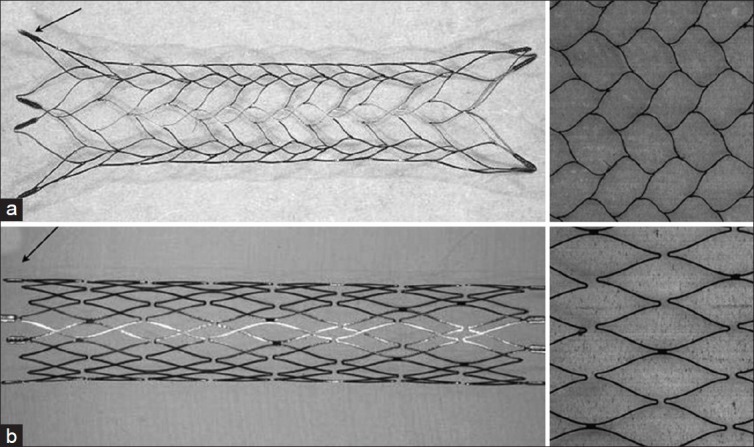
The waffle-cone technique, as described previously for the Neuroform stent,[4] was used with the Enterprise stent in all cases for these four large wide-necked bifurcation aneurysms [Figure 1]. Selective catheterization of the aneurysm and deployment of the Enterprise stent with the distal stent tines being deployed into the proximal neck of the aneurysm were carried out through a Prowler Select Plus microcatheter (Cordis Neurovascular, Miami, FL) in the waffle-cone conformation [Figure 2]. A point within the aneurysm neck measuring greater than the flared ends of the Enterprise stent (>4.5 mm) was identified for deployment of the distal tines to prevent injury and rupture of the aneurysm. This was then followed by packing the aneurysm with a series of appropriately sized coils for the individual aneurysm.
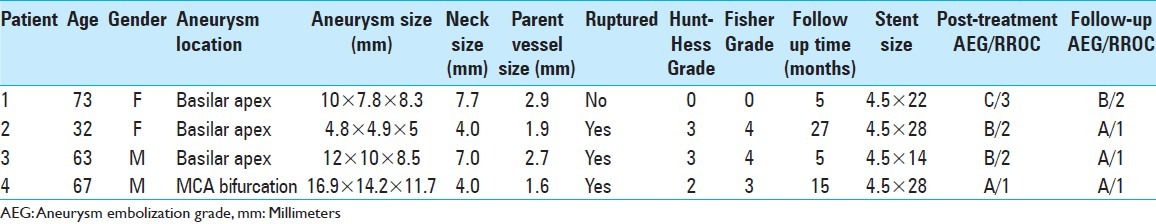
Figure 1.
(a) Enterprise stent with flared tines when deployed and closed-cell design are depicted. (b) Neuroform stent with parallel stent wall and tines when deployed and open-cell designs are depicted. Figure modified and reprinted from Wakhloo,[et al.[12]
Figure 2.
(a) Microcatheter and microwire in the aneurysm neck. (b) Enterprise stent being deployed into aneurysm. (c) Enterprise stent deployed with microwire in aneurysm. (d) Coils deployed through microcatheter in aneurysm. (e) Coiled aneurysm in waffle-cone configuration. Figure and legend modified and reprinted from Horowitz, et al.[4]
All ruptured aneurysm patients were placed on abciximab intravenous drip after coil embolization until external ventricular drainage was not needed, after which they were placed on aspirin 325 mg and clopidogrel 75 mg orally daily for three months, and then aspirin 81 mg daily. The unruptured aneurysm patient was premedicated for one week prior to the intervention with aspirin 325 mg and clopidogrel 75 mg orally daily, followed by the same postprocedure antiplatelet oral regimen described above for the ruptured aneurysms.
Patient cases
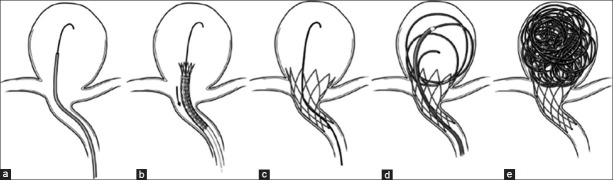
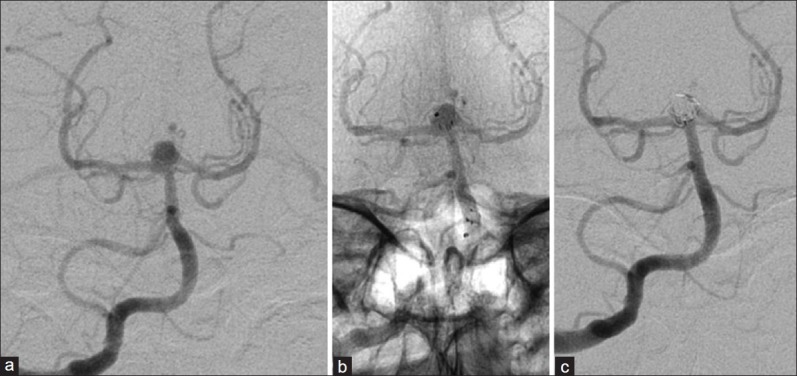
One basilar apex aneurysm [Figure 3] had a small residual (2.5 × 3.0 mm) outside of the stent tines with an Aneurysm Embolization Grade (AEG)[1,11] of “C” [Table 2], where the P1 origin was incorporated into the aneurysm neck. This patient also had a delayed onset of a small posterior cerebral artery stroke with a visual field cut one month after the initial intervention and required the recoiling of the residual neck, which reduced the AEG to “B.” Two year follow-up imaging demonstrated a patent Enterprise stent with no significant in-stent stenosis and no recurrence of the aneurysm nor progression of PCA infarct.
Figure 3.
Patient 1 cerebral angiogram (left vertebral injection). (a) AP view showing a basilar apex aneurysm pretreatment. (b) Lateral view of the Enterprise stent deployed in the aneurysm dome. (c) Follow-up AP view showing small basilar apex aneurysm recurrence before redo treatment. (d) Follow-up AP view after redo coil embolization of recurrent aneurysm. (e) 27-month follow-up AP view after redo coil embolization showing no further recurrence
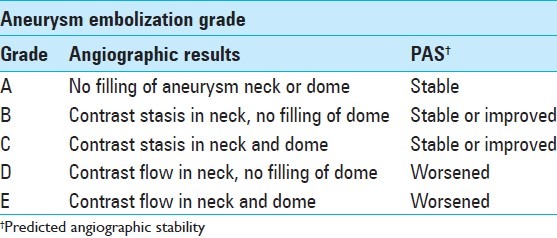
Table 2.
Aneurysm embolization grading scale for predicting likelihood of aneurysm recurrence based on angiographic flow characteristics through the aneurysm neck and dome after embolization. Table modified and reprinted from Deshaies, et al.[1,11]
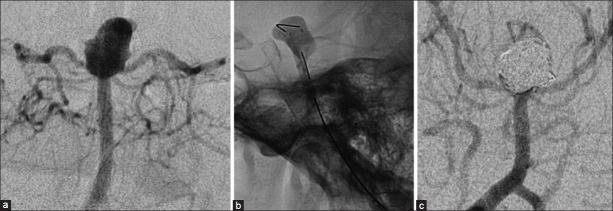
Two other basilar apex aneurysms (one ruptured, one elective) had small residuals with delayed filling at the neck (AEG-“B”), again where the P1 origin was incorporated into the aneurysm neck [Figures 4 and 5]. These small residuals spontaneously thrombosed and the AEG improved from “B” to “A” on follow-up cerebral angiography performed during 1-3 month follow-up.
Figure 4.
Patient 2 cerebral angiogram (right vertebral injection). (a) AP view showing a basilar apex aneurysm pretreatment. (b) AP native view showing placement of the Enterprise stent deployed in the aneurysm dome. (c) AP subtracted view showing the basilar apex aneurysm postembolization
Figure 5.
Patient 3 cerebral angiogram (right vertebral injection). (a) AP subtracted view showing a basilar apex aneurysm pretreatment. (b) Lateral native view showing the Enterprise stent deployed in the aneurysm dome. (c) AP subtracted view showing the basilar apex aneurysm postembolization
The ruptured MCA bifurcation aneurysm was completely obliterated (AEG-“A”) during initial treatment with this technique, without occlusion or compromise of the branching arteries at the bifurcation [Figure 6]. All parent vessels and their respective branches remained patent after all procedures. Abciximab intravenous drip resulted in thrombocytopenia and had to be stopped prior to the intended date and the patient started on aspirin 325 mg orally until the ventriculostomy could be removed, after which time clopidogrel 75 mg daily was added to the regimen for three months.
Figure 6.
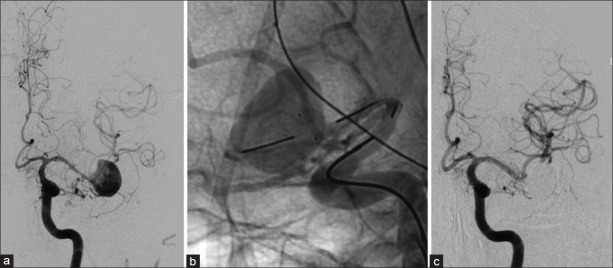
Patient 4 cerebral angiogram (left ICA injection). (a) AP subtracted view showing a left MCA bifurcation aneurysm pretreatment. (b) Lateral native view showing the Enterprise stent deployed in the aneurysm dome. (c) AP subtracted view showing the basilar apex aneurysm postembolization
Periprocedural complications
There were no intraprocedural or immediate postprocedure complications related to technique in any of these cases. None of these patients presented with any symptoms of mass effect or cranial neuropathy from the aneurysm and stent-coil embolization of these vascular lesions did not result in de novo neurological deficits. The electively stent-coiled aneurysm patient was discharged home the next day and the subarachnoid hemorrhage patients had uneventful courses within the neurocritical care unit.
DISCUSSION
Large complex wide-necked intracranial aneurysms, such as those described here, present technical challenges that mandate thinking differently about treatment endeavors. The waffle-cone technique is one such technique that addresses the endovascular challenge of coiling these types of complex bifurcation aneurysms. An advantage of the Enterprise over the Neuroform stent is its flexible closed-cell design which allows it to be retrieved and repositioned when up to 70% is deployed.[3] The Neuroform stent cannot be retrieved once the first set of open cells are deployed, preventing stent repositioning. An additional edge provided by Enterprise is its flared ends that allow it to naturally conform to the waffle-cone shape in the aneurysm neck, unlike the parallel tubular shape of the Neuroform stent. Other closed-cell stents have been designed, such as the Solitaire-AB retrievable stent (eV3/Covidien, Irvine CA, USA),[5] but is currently not FDA approved for use in the United States and therefore not available to us.
The largest of the three basilar tip aneurysms was left with a residual neck at the junction of the P1 origin after initial treatment to avoid PCA occlusion and later required retreatment. This recurrence is consistent with reports in the literature of aneurysm, size greater than 10 mm is an independent predictor of recurrence, and also the fact that residual aneurysm neck was left intentionally to preserve the patency of the P1 origin in this case.[9] A potential downside to using a closed-cell stent is that it can limit access to the distal vascular tree, even though the cell size is 1.3 Fr and should allow passage of most endovascular microcatheters. An additional downside of the Enterprise stent is that the closed-cell design may limit blood flow from the parent artery through the stent tube into the branching arteries where it covers them at their origins. Although we did not encounter this problem in any of our patients and there were not any hemodynamic alterations noted on angiography, the open cell-design of the Neuroform stent would theoretically minimize these potential complications.
As with any stent-assisted coiling in the setting of subarachnoid hemorrhage, antiplatelet therapy is needed to reduce the risk of thromboembolic events from the stent, which increases the risk of hemorrhagic complications from the aneurysm itself or invasive procedures needed for hydrocephalus. Many of these patients will require external ventricular drains, ventriculperitoneal shunts, or other procedures and operations that are higher risk with antiplatelet usage. However, the risk from stent-assisted coiling must be weighed against that of surgical clip ligation of these complex aneurysms.
When compared with the “Y”- stent technique, this approach uses a single stent helping to reduce cost and more importantly, reduce the surface area of exposed metal to the vessel lumen. Reduced exposure of blood to a metal surface should reduce the risk of thromboembolic events and the probability of in-stent stenosis; although some would argue that jailing of the branching artery origins by a closed-cell stent could actually increase the risk of immediate hemodynamic compromise, thromboembolic complications, and delayed in-stent stenosis. Currently, there are no studies that address any actual thromboembolic complication rates of these two stents with this technique. Other techniques of stent placement across the base of a wide-necked basilar apex aneurysm include placement via p-com across the basilar aneurysm neck by deploying into bilateral P1 segments. This technique requires a large p-com with favorable anatomy and also can jail out the P1 origins from the blood flow directed through the basilar artery.[8,10] The waffle-cone technique avoids the need for large communicating vessels with favorable anatomy and the placement of multiple stents needed for the “Y”-stent technique.
However, caution with the waffle-cone technique is warranted, independent of the type of stent used to assist with coil embolization. Treatment of aneurysms with a relatively short dome height could be dangerous with the waffle-cone technique in the event that forward tension on the microcatheter results in forward migration of the stent during deployment. In this situation, aneurysm perforation could occur with disastrous results as it could with any procedure involving the treatment of aneurysms with short domes. Therefore, we believe that the waffle-cone technique is useful only for carefully selected aneurysm morphologies consistent with long dome heights and wide-necks that incorporate the bifurcating vessels, unable to be “Y” stented or surgically clipped. This technique is not recommended for aneurysms with narrow necks or short dome heights where deployment error could result in rupture, or aneurysms with necks less than 4.5 mm (size of the distal stent flare) where the opening distal end of the stent could perforate the aneursym.
CONCLUSIONS
Coil embolization of large wide-necked arterial bifurcation aneurysms has been described here using the waffle-cone technique with the Enterprise stent. The closed-cell design, flexibility, and flared ends of the Enterprise stent allow it to conform to the natural morphology of the aneurysm neck into the waffle-cone configuration providing a stable scaffold for coil embolization. We have had excellent initial results with this technique, but the interventionalist must keep in mind that the technical risk is higher than the traditional stent-assisted and balloon-assisted coiling procedures. Therefore, the waffle-cone technique should be reserved for those bifurcation aneurysms with wide necks incorporating the branching vessel origins, where “Y” stenting is needed but not possible due to the aneurysm neck morphology, and surgical clip ligation is not an option.[12]
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/9/106268
Contributor Information
David J. Padalino, Email: padalind@upstate.edu.
Amit Singla, Email: singlaa@upstate.edu.
Walter Jacobsen, Email: jacobsw@mail.amc.edu.
Eric M. Deshaies, Email: deshaiee@upstate.edu.
REFERENCES
- 1.Deshaies EM, Adamo MA, Boulos AS. A prospective single-center analysis of the safety and efficacy of the hydrocoil embolization system for the treatment of intracranial aneurysms. J Neurosurg. 2007;106:226–33. doi: 10.3171/jns.2007.106.2.226. [DOI] [PubMed] [Google Scholar]
- 2.Gruber TJ, Ogilvy CS, Hauck EF, Levy EI, Hopkins LN, Siddiqui AH. Endovascular treatment of a large aneurysm arising from a basilar trunk fenestration using the waffle-cone technique. Neurosurgery. 2010;67(3 Suppl Operative):ons140–4. doi: 10.1227/01.NEU.0000382977.55504.6C. discussion ons144. [DOI] [PubMed] [Google Scholar]
- 3.Higashida RT, Halbach VV, Dowd CF, Juravsky L, Meagher S. Initial clinical experience with a new self-expanding nitinol stent for the treatment of intracranial cerebral aneurysms: The Cordis Enterprise stent. AJNR Am J Neuroradiol. 2005;26:1751–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms: Eight cases using the waffle cone technique ;58:ONS-258-62. Neurosurgery. 2006;58:ONS-258–62. doi: 10.1227/01.NEU.0000204713.24945.D2. discussion ONS-262. [DOI] [PubMed] [Google Scholar]
- 5.Klisch J, Eger C, Sychra V, Strasilla C, Basche S, Weber J. Stent-assisted coil embolization of posterior circulation aneurysms using solitaire ab: Preliminary experience. Neurosurgery. 2009;65:258–66. doi: 10.1227/01.NEU.0000348295.44970.C8. discussion 266. [DOI] [PubMed] [Google Scholar]
- 6.Lavine SD, Meyers PM. Application of new techniques and technologies: Stenting for cerebral aneurysm. Clin Neurosurg. 2007;54:64–9. [PubMed] [Google Scholar]
- 7.Mocco J, Snyder KV, Albuquerque FC, Bendok BR, Alan SB, Carpenter JS, et al. Treatment of intracranial aneurysms with the Enterprise stent: A multicenter registry. J Neurosurg. 2009;110:35–9. doi: 10.3171/2008.7.JNS08322. [DOI] [PubMed] [Google Scholar]
- 8.Moret J, Ross IB, Weill A, Piotin M. The retrograde approach: A consideration for the endovascular treatment of aneurysms. AJNR Am J Neuroradiol. 2000;21:262–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Peluso JP, van Rooij WJ, Sluzewski M, Beute GN. Coiling of basilar tip aneurysms: Results in 154 consecutive patients with emphasis on recurrent haemorrhage and re-treatment during mid- and long-term follow-up. J Neurol Neurosurg Psychiatry. 2008;79:706–11. doi: 10.1136/jnnp.2007.127480. [DOI] [PubMed] [Google Scholar]
- 10.Pride GL, Jr, Welch B, Novakovic R, Rickert K, White J, Dutton-Johnson K, et al. Retrograde crossing stent placement strategies at the basilar apex for the treatment of wide necked aneurysms: Reconstructive and deconstructive opportunities. J Neurointerv Surg. 2009;1:132–5. doi: 10.1136/jnis.2009.000182. [DOI] [PubMed] [Google Scholar]
- 11.Singla A, Villwock MR, Jacobsen W, Deshaies EM. Aneurysm embolization grade: A predictive tool for aneurysm recurrence after coil embolization. Acta Neurochir (Wien) 2012 doi: 10.1007/s00701-012-1554-3. [In Press] [DOI] [PubMed] [Google Scholar]
- 12.Wakhloo AK, Deleo MJ, 3rd, Brown MM. Advances in interventional neuroradiology. Stroke. 2009;40:e305–12. doi: 10.1161/STROKEAHA.109.548438. [DOI] [PubMed] [Google Scholar]


