Abstract
Introduction and Aim:
Emergency thoracotomy is performed either immediately at the scene of injury, in the emergency department or in the operating room. It aims to evacuate the pericardial tamponade, control the haemorrhage, to ease the open cardiac massage and to cross-clamp the descending thoracic aorta to redistribute blood flow and maybe to limit sub-diaphragmatic haemorrhage, bleeding and iatrogenic injury are the common risk factors. We aimed to review our experience in the field of emergency thoracotomies, identify the predictors of death, analyze the early results, detect the risk factors and asses the mortalities and their risk factors.
Patients and Methods:
Our hospital records of 197 patients who underwent emergency thoracotomy were reviewed. We retrospectively analyzed a piece of the extensive experience of the Mansoura University Hospitals and Mansoura Emergency Hospital; Egypt and Saudi German Hospitals; Jeddah in the last 12 years in the management of trauma cases for whom emergency thoracotomy. The aim was to analyse the early results of such cases and to detect the risk factors of dismal prognosis.
Results:
Our series included 197 cases of emergency thoractomies in Mansoura; Egypt and SGH; Jeddah; KSA in the last 12 years. The mean age of the victims was 28 years and ranged between 5 and 62 years. Of the 197 patients with emergency thoracotomy, the indications were both penetrating and blunt chest trauma, iatrogenic and postoperative hemodynamito a surgical cause. The commonest indication was stab heart followed by traumatic diaphragmatic ruptures.
Conclusion:
The results of emergency thoracotomy in our series were cooping with the results of other reports, mainly due to our aggressive measures to achieve rapid stabilization of the hemodynamic condition. We emphasize the importance of emergency medicine education programs on rapid diagnosis of traumatic injuries with early intervention, and adequate hemodynamic and respiratory support. Emergency thoracotomy has an important role in emergency big volume hospitals and can save a lot of lives. Outcome can be improved by increasing the learning curve and the integrated cooperation of the emergency and surgical teams.
Keywords: Emergency thoracotomy, trauma, post-operative
INTRODUCTION AND AIM
Emergency thoracotomy is defined as the thoracotomy performed in the scene of accident, emergency department for patients arriving in extremis or in the operating room with no previous plan. Current indications are severe penetrating or blunt injury with recent witnessed loss of signs of life (SOL) and persistent, severe hemorrhagic shock.[1–6] Outcome varies widely depending on the injury mechanism, anatomic injury location, and physiologic status. Cardiac injury has traditionally been considered a positive prognostic factor, compared to findings of non-cardiac thoracic or abdominal injuries. A meta-analysis by Rhee, et al. determined that survival rates were highest for isolated penetrating cardiac injuries (19%) compared to penetrating non-cardiac thoracic (11%), penetrating abdominal (4%), or multiple penetrating injuries (<1%). Overall survival rates were 17% after stab wounds and 4% after gunshot wounds. Normal neurologic recovery was observed in 92% of the patients who survived their hospitalization. However, the outcome analysis for cardiac wounds was not stratified by injury mechanism.[3–7]
The Advanced Trauma life support (ATLS) guidelines recommended emergency thoracotomy in penetrating thoracic injuries who arrive pulseless with myocardial electrical activity or after a short time with witnessed physiological parameters which are intact pupillary response, spontaneous ventilation, presence of carotid pulse, measurable or palpable blood pressure, extremity movement and cardiac electrical activity. It also recommended that emergency department thoracotomy should be performed in patients with penetrating non-cardiac thoracic injuries and also in patients suffering from exsanguinating abdominal vascular injuries, but it is noted that both groups generally experience a low survival rate even after the procedure, the practice patterns are not always like this depending on many factors.[1,3–8]
In our present study, we sought to assess our recent experience in the emergency thoracotomies. The primary objective of this study was to review our experience in the field of emergency thoracotomies and to identify predictors of death for in such cases. The aim was to analyze the early results of such cases and to detect the risk factors of dismal prognosis. Our end points were the assessment of mortalities and their risk factors.
PATIENTS AND METHODS
A retrospective review of 197 patients undergoing emergency thoracotomy at the Mansoura university emergency hospital; Mansoura; Egypt and Saudi German hospital; Jeddah; KSA from January, 2000 to January, 2012 was conducted. Cases were identified by review of the charts in both centers. This represents a piece of our experience in both big volume centers. Data collected from the hospital records included the available data as patient demographics; mechanism of injury; injury location; use of cardiopulmonary resuscitation (CPR) before reaching the hospital; presence of signs of life, in the form of spontaneous movement, spontaneous respirations, organized electrocardiographic activity, palpable pulse, or pupillary response; obtainable vital signs such as respiratory rate, measureable blood pressure, or palpable pulse; Glasgow coma scale score; use of epinephrine; and the number of patients intubated. Data collected from hospital records included initial electrocardiographic rhythm, presence of obtainable vital signs, presence of signs of life, new injury severity score (NISS), time from loss of vital signs to EDT, units of packed red blood cells given, liters of crystalloid administered, dose of epinephrine given, location of injury, disposition from the ED, overall survival, and neurologically intact survival. The ER team follows: Airway, breathing, and circulation (ABC's) during the primary survey. During initial examination, potentially life-threatening conditions such as tension pneumothorax are immediately treated. The presence of severe chest trauma, mandates good pain control and may mandate endo-tracheal intubation. A second survey is then performed as well as insertion of the appropriate intravenous line. These patients required evaluation and imaging for potential neurologic, intra-abdominal, vascular or extremity trauma. The presence of distended neck veins, tracheal deviation, subcutaneous emphysema, chest wall instability, absent breath sounds or muffled heart sounds are alarming signs for us. Vital signs are monitored specially the respiratory function and arterial saturation. An arterial blood gas should have been sent with the initial laboratory studies, an electrocardiogram and a portable chest radiograph (CXR) should be obtained. A portable CXR yields rapid information about the pleural space, including pneumothorax or haemothorax, which may require chest tube insertion. A focused abdominal sonography for trauma (FAST) of the abdomen and precordium should be rapidly performed. The need, if any, for additional imaging and/or procedure is driven by the patient's cardiopulmonary stability, physical examination, laboratory, and radiographic findings. Our indications for emergency thoracotomy were refractory hypotension persistently unresponsive to aggressive fluid resuscitation from significant intrathoracic haemorrhage (>1500 ml in the chest drain), cardiac tamponade, systemic air embolus or tracheobronchial disruption and or witnessed cardiac arrest after isolated penetrating chest trauma. The patient should be intubated and ventilated. The incision is extended from the sternal border in the 5th intercostal to the mid-axillary line following the infra-mammary fold. This was similar to O’Connor and Adamski (2010), Morgan and Garner (2009), Mollberg, et al. (2011) and others.[5–15]
The management is directed towards the suspected injury. Adequate volume replacement with both crystalloids and colloids to maintain an acceptable mean blood pressure after finishing the procedure, the patient is transferred to the ICU ventilated often paralyzed and monitored. The demographic data of the patients, age, sex, type of trauma, site of trauma, associated injuries, general condition of the patient, resuscitation measures, and management done and follow-up of the survivors. Data and outcomes analyzed. Data were entered into Statistical Package for the Social Sciences (SPSS, Version 16.0.0, SPSS, Inc., Chicago, IL, USA). Statistical analysis done using a Student's t-test for continuous variables and a Fischer's exact test for categorical variables. A P value of less than or equal to 0.05 was considered statistically significant. We used Fisher's exact test for all the variables. Descriptive statistics were calculated for continuous and categorical variables. Univariate logistic regression analysis was performed to identify predictors of survival in the hospital discharge. A P value ≤ 0.05 was considered statistically significant.
RESULTS
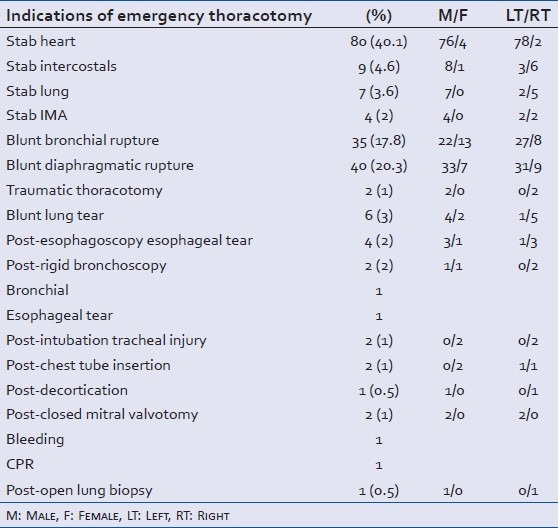
During the study period, 197 patients underwent emergency thoracotomy in two centers in both Egypt and KSA. Of those patients, 100 cases had a penetrating chest trauma. Stab heart was reported in 80, stab intercostals in 9, stab lung in 7 and stab mammaries in 4 cases. We never had impalement chest injuries. Patient demographic and clinical characteristics are depicted in Table 1. We never had impalement chest injuries. Blunt chest trauma was reported in 83 cases of whom blunt traumatic diaphragmatic rupture was reported in 40 cases, bronchial rupture reported in 35, lung tears in 6 cases while traumatic thoracotomy was seen in 2 cases. Iatrogenic cause was responsible for 10 cases. Emergency exploratory thoracotomy was needed in 4 cases in the early postoperative period [Table 1].
Table 1.
Indications and some demographic data of the cases of emergency thoracotomy
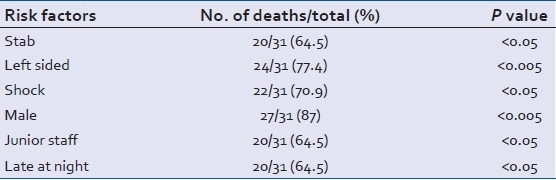
Associated extra-thoracic injuries were found in 68 patients. The commonest were head injuries in 25, abdominal injuries in 21, extremity's fractures in 14, pelvic fracture in 8 cases. Shock was evident on first presentation in 28 patients. Preoperative CPR was needed in 23 cases. Endoscopy trauma was responsible for 6 cases. Thirty one patients died. The cause of death was stab heart in 20, bronchial ruptures in 5, due to blunt tramatic diaphragmatic ruptures in 3, due to esophageal tear in 2 and 1case died after closed mitral valvotomy. The mortality risk factors were found to be stab heart, left sided thoracotomy, unstable hemodynamics on 1st presentation, male gender, junior staff receiving and managing the cases and presentation very late at night or early dawn. They are presented in Table 2.
Table 2.
Mortality risk factors
DISCUSSION
This study represents a piece of the experience of imminent centers in Egypt and Saudi Arabia in the emergency thoracotomy. One hundred and ninety seven cases of emergency thoracotomy was included here as these cases were managed in Mansoura University hospitals 1512 beds and Mansoura emergency hospitals 184 beds that serve more than 20 million of population, and the medical service is completely free of charges. A part of the study was done in SGH; Jeddah; KSA which is a big volume hospital. The indications of emergency thoracotomy as per Morgan and Garner 2009 were hypotension with a systolic blood pressure <70 mmHg) persistently unresponsive to aggressive fluid resuscitation and or inotropic support from significant intrathoracic haemorrhage (>1500 ml in the chest drain), cardiac tamponade, systemic air embolus or tracheobronchial disruption, witnessed cardiac arrest after isolated penetrating chest trauma with definite previous signs of life (<15 minutes of prehospital CPR) and cross-clamping of the thoracic aorta to halt the uncontrollable abdominal haemorrhage as a pre-laparotomy manoeuvre. Their contraindications were absence of signs of life after blunt thoracic trauma (>5 minutes of CPR). No signs of life on scene and on arrival in the emergency department after 15 minutes of cardiopulmonary resuscitation, cardiac arrest in a non-shockable rhythm for over 5 minutes and co-existent severe head injury or multisystem trauma.[5–17] Any ways; we were not far from these indications. We included penetrating chest injuries, blunt chest injuries, iatrogenic injuries and early postoperative hemodynamic instability due to possible surgical aetiology. Chest injuries of any nature in the mediastinum or dangerous triangle of the chest with hemodynamic instability or with positive FAST US chest or chest tube drainage of massive hemothorax, massive air leak or massive surgical emphysema affecting the hemodynamics of the patient or persistent lung collapse despite the insertion of a good size well positioned and functioning chest tube. Our emergency thoracotomies were performed in 100 stab chest (80 stab hearts, 9 stab intercostals, 7 stab lungs and 4 stab internal mammary arteries). Penetrating chest injuries constituted 50.7% of the series. The commonest of these was stab heart (40.6%). Blunt chest trauma was responsible for 42.1%, iatrogenic injuries were responsible for 5% and postoperative emergency redo thoracotomy was performed in only 2.3%. Gwely, et al. (2010),[18] from Mansoura Medical School; Egypt, reported a series of 73 stab heart cases. Of these cases, 94.5% were males. Their mean patient age was 28.5 ± 5.8 years. The hemodynamics were stable in 30.1% and unstable in 35.6%, while 13.7% were in shock and 20.6% suffered from cardiac arrest prior to thoracotomy. They performed emergency room thoracotomy in 24.7% and operative room thoracotomy in 75.3% of their series. The commonest location of stab wounds to the heart was the right ventricle in 38.4% followed by the left ventricle in 34.2%. Their mortality rate was 23.3% and morbidity was 21.4%. They reported the prognostic factors as the clinical status; patients in shock and cardiac arrest. Shocked and arrested patients had a mortality rate of 50% and 60%, respectively. Those who needed cardiopulmonary resuscitation had mortality rate of 68.2%) and ER thoracotomy carried had a mortality rate of 66.7%).[18,19]
We included most of these cases in our study. Blunt trauma was blamed for 83 cases of emergency thoracotomies (42.1%). It ranged between diaphragmatic rupture in 40, blunt bronchial rupture in 35, lung tear in 6 cases and traumatic thoracotomy in 2 cases. The clinical picture was either massive surgical or mediastinal emphysema, massive air leak, persistent lung collapse even after chest tube insertion, Viscera or Nasogastric tube (NGT) in the chest, prominent lung or mediastinal structures through the site of the trauma. A series from our department in 2009 reported 25 cases treated for bronchial rupture. Bronchoscopy followed by thoracotomy was done for most of these cases. Urgent repair was undertaken through a right thoracotomy in 21 patients (84%) and via a left thoracotomy in 4 cases (16%). Direct bronchial suturing and repair were carried out in all except three patients who needed lobectomy. Four patients died due to perioperative cardiac arrest and cerebral hypoxia with failure of resuscitation.[18]
Right thoracotomy enabled us to repair right sided bronchial lesions, tracheal and proximal left main bronchus. Sersar SI 2010 published a series of 40 cases of blunt traumatic diaphragmatic rupture (BTDR) which needed emergency thoracotomy and or laparotomy. Diagnosis was made by either chest X-ray, CT chest, chest X-ray with nasogastric tube with or without gastro-graffin or intra-operatively. Diaphragmatic repair was done either by thoracotomy and or laparotomy. The predictors of mortality in BTDR in his study were male gender, associated injuries especially liver and intestinal tears and combined thoracotomy laparotomy and splenectomy.[19]
Traumatic thoracotomy was observed in 2 cases. Completion of the thoracotomy under complete aseptic conditions with exploration and anatomical repair and closure was done. Blunt lung tear was noted in 6 cases. They were managed by repair of the lung in 4 cases and lobectomy in 2 cases. Esophagoscopy and bronchoscopy was accused in 6 cases. The esophagus was injured in 5 cases and left main bronchus injured in 1 case. They were all repaired primarily on an urgent basis. Post-intubation tracheal rupture was noted in 2 cases in the form of significant postoperative surgical emphysema in the neck. Diagnosis was confirmed by flexible bronchoscopy. They were repaired through a right thoracotomy. By mistake, two chest tubes were inserted in the lung parenchyma in one patient in the ICU. The lungs were repaired consecutively in 2 days. Emergency exploratory thoracotomy was done in a post-decortication patient with extensive adhesions who drained more than 1500 cc blood in the chest tube in the first 3 postoperative hours with hemodynamic instability. Closed mitral valvotomy was complicated by massive bleeding in a case and refractory arrhythmias and hypotension in an other. They needed urgent redo thoracotomy. Lung biopsy for sarcoma was complicated with bleeding and mandated emergency exploration thorcotomy. Death was reported in 31 cases (16.5%); the commonest cause of death was stab heart in 20 patients (64.5%), bronchial rupture in 5 (16.1%), blunt diaphragmatic rupture in 3 (9.67%), esophageal injury in 2 (6.45%) and after closed mitral valvotomy. Left sided thoracotomy was more complicated by death than right sided thoracotomy (24 vs. 7). Unstable hemodynamics on 1st presentation was associated with dismal prognosis (22 vs. 9). Male gender was a risk factor associated with death (27 vs. 4). Junior staff and presentation late evening or early dawn hours were also a risk factor. Asensio, et al. (1998) found that the Glasgow coma score (GCS), revised trauma score and the cardiovascular respiratory score were all highly predictive of survival in penetrating cardiac injuries. In their study, for patients with GCS <8, the mortality was 83.7%, as compared with patients with GCS scores >8, in whom mortality was 27.3%, demonstrating the inverse relationship between GCS score and mortality rate. Mechanism of injury in their study was also a significant predictor of outcome, the mortality from gunshot wound injuries to the heart was 83.8%, significantly higher than the mortality from stab wounds, which was 35.1%. A review of 24 studies by Rhee, et al. (2000) also found that factors reported as influencing outcome in emergency thoracotomy were the mechanism of injury, location of major injury and signs of life.[1,5,6,8,13–22]
In Egypt, Guns are strictly prohibited by law. That is why, we did not report any case of emergency thoracotomy due to gun shots. The other cause if any may be that these gun shots victims die before reaching the hospitals.
Sereide, et al. (2007) found the survival to be the best for isolated penetrating injuries to the heart. It was 31% and the overall survival was 7-8%, while it is 11% after penetrating and 1.6% after blunt trauma. It was better if there are signs of life at the 1st presentation (survival 11% vs. less than 3%), heart injuries better than thoracic injuries better than abdominal better than multiple injuries (30% vs. 20% vs. <5% vs. <1%). They also found the survival of penetrating injuries better than blunt chest injuries and stabs better than gun shots.[18–22]
Limitations
This is a retrospective study with all the defects of retrospective studies as lack of randomizations, heterogeneity of diagnoses and risk factors of the patient population with different surgeons with different practices in two countries in a relatively long period of time.
CONCLUSION
Emergency thoracotomy can save a lot of lives. Risk factors of dismal prognosis are stab heart, left sided thoracotomy, unstable hemodynamics on 1st presentation, male gender, junior staff receiving and managing the cases and presentation very late at night or early dawn.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mollberg NM, Wise SR. Appropriate use of emergency department thoracotomy. J Am Coll Surg. 2012;214:870–1. doi: 10.1016/j.jamcollsurg.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 2.Ekelund M, Victorin A, Bergman O, Nilsson S, Lönroth H. A case report: Young man survived penetrating knife stabs to the heart and lung. Lakartidningen. 2001;98:2936–8. [PubMed] [Google Scholar]
- 3.Lau CK, Chin HF, Ong FH, Eng KH. Emergency department thoracotomy for pericardiac tamponade. Singapore Med J. 2008;49:e382–4. [PubMed] [Google Scholar]
- 4.Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma - A review. Injury. 2006;37:1–19. doi: 10.1016/j.injury.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Balkan ME, Oktar GL, Kayi-Cangir A, Ergül EG. Emergency thoracotomy for blunt thoracic trauma. Ann Thorac Cardiovasc Surg. 2002;8:78–82. [PubMed] [Google Scholar]
- 6.Molina EJ, Gaughan JP, Kulp H, McClurken JB, Goldberg AJ, Seamon MJ. Outcomes after emergency department thoracotomy for penetrating cardiac injuries: A new perspective. Interact Cardiovasc Thorac Surg. 2008;7:845–8. doi: 10.1510/icvts.2008.183293. [DOI] [PubMed] [Google Scholar]
- 7.Athanasiou T, Krasopoulos G, Nambiar P, Coats T, Petrou M, Magee P, Uppal R. Emergency thoracotomy in the pre-hospital setting: A procedure requiring clarification. Eur J Cardiothorac Surg. 2004;26:377–86. doi: 10.1016/j.ejcts.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Esposito TJ, Jurkovich GJ, Rice CL, Maier RV, Copass MK, Ashbaugh DG. Reappraisal of emergency room thoracotomy in a changing environment. J Trauma. 1991;31:881–5. doi: 10.1097/00005373-199107000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: Review of published data from the past 25 years. J Am Coll Surg. 2000;190:288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 10.Miglietta MA, Robb TV, Eachempati SR, Porter BO, Cherry R, Brause J, et al. Current opinion regarding indications for emergency department thoracotomy. J Trauma. 2001;51:670–6. doi: 10.1097/00005373-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons. Committee on Trauma. Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001;193:303–9. doi: 10.1016/s1072-7515(01)00999-1. [DOI] [PubMed] [Google Scholar]
- 12.Morgan BS, Garner JP. Emergency thoracotomythe indications, contraindications and evidence. J R Army Med Corps. 2009;155:87–93. doi: 10.1136/jramc-155-02-02. [DOI] [PubMed] [Google Scholar]
- 13.O’Connor JV, Adamski J. The diagnosis and treatment of non-cardiac thoracic trauma. J R Army Med Corps. 2010;156:5–14. doi: 10.1136/jramc-156-01-02. [DOI] [PubMed] [Google Scholar]
- 14.Mollberg NM, Glenn C, John J, Wise SR, Sullivan R, Vafa A, et al. Appropriate use of emergency department thoracotomy: Implications for the thoracic surgeon. Ann Thorac Surg. 2011;92:455–61. doi: 10.1016/j.athoracsur.2011.04.042. [DOI] [PubMed] [Google Scholar]
- 15.Powell DW, Moore EE, Cothren CC, Ciesla DJ, Burch JM, Moore JB, et al. Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation? J Am Coll Surg. 2004;199:211–5. doi: 10.1016/j.jamcollsurg.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World J Emerg Surg. 2006;1:4. doi: 10.1186/1749-7922-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandola HC. Emergency anaesthetic management of extensive thoracic trauma. Ind J Anaesth. 2007;51:394–400. [Google Scholar]
- 18.Gwely NN, Mowafy A, Khalaf S, Amer S, Hamza U, El-Saeed M. Management of stab wounds of the heart: Analysis of 73 cases in 10 years. Thorac Cardiovasc Surg. 2010;58:210–4. doi: 10.1055/s-0029-1240921. [DOI] [PubMed] [Google Scholar]
- 19.Gwely NN. Blunt traumatic bronchial rupture in patients younger than 18 years. Asian Cardiovasc Thorac Ann. 2009;17:598–603. doi: 10.1177/0218492309349067. [DOI] [PubMed] [Google Scholar]
- 20.Sersar SI. The predictors of early death after repair of blunt traumatic diaphragmatic rupture (BTDR) J Egypt Soc Cardio Thorac Surg. 2010;18:101–4. [Google Scholar]
- 21.Asensio JA, Berne JD, Demetriades D, Chan L, Murray J, Falabella A, et al. One hundred five penetrating cardiac injuries: A 2-year prospective evaluation. J Trauma. 1998;44:1073–82. doi: 10.1097/00005373-199806000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Søreide K, Petrone P, Asensio JA. Emergency thoracotomy in trauma: Rationale, risks, and realities. Scand J Surg. 2007;96:4–10. doi: 10.1177/145749690709600102. [DOI] [PubMed] [Google Scholar]


