Abstract
Background:
Achieving definitive care within the “Golden Hour” by minimizing response times is a consistent goal of regional trauma systems. This study hypothesizes that in urban Level I Trauma Centers, shorter pre-hospital times would predict outcomes in penetrating thoracic injuries.
Materials and Methods:
A retrospective cohort study was performed using a statewide trauma registry for the years 1999-2003. Total pre-hospital times were measured for urban victims of penetrating thoracic trauma. Crude and adjusted mortality rates were compared by pre-hospital time using STATA statistical software.
Results:
During the study period, 908 patients presented to the hospital after penetrating thoracic trauma, with 79% surviving. Patients with higher injury severity scores (ISS) were transported more quickly. Injury severity scores (ISS) ≥16 and emergency department (ED) hypotension (systolic blood pressure, SBP <90) strongly predicted mortality (P < 0.05 for each). In a logistic regression model including age, race, and ISS, longer transport times for hypotensive patients were associated with higher mortality rates (all P values <0.05). This was seen most significantly when comparing patient transport times 0-15 min and 46-60 min (P < 0.001).
Conclusion:
In victims of penetrating thoracic trauma, more severely injured patients arrive at urban trauma centers sooner. Mortality is strongly predicted by injury severity, although shorter pre-hospital times are associated with improved survival. These results suggest that careful planning to optimize transport time-encompassing hospital capacity and existing resources, traffic patterns, and trauma incident densities may be beneficial in areas with a high burden of penetrating trauma.
Keywords: Golden Hour, penetrating trauma mortality, pre-hospital transport time, urban trauma systems
INTRODUCTION
Introduced by Cowley in the 1970s, The “Golden Hour” concept has since governed planning and preparedness in trauma systems development[1] As a major source of morbidity and mortality to the population that contributes to the economy, i.e., people less than 45 years of age, trauma is a significant problem that needs continuous systems improvement.[2] An integrated trauma system improves outcomes for patients of trauma, but the exact parameters that determine effectiveness have yet to be conclusively defined.[3,4]
The relationship between shortened pre-hospital time and improved survival exists, but is most consistently demonstrated when comparing urban and rural locals.[5,6] No data exists that specifically quantifies the relationship between pre-hospital time and outcomes within purely urban areas, and especially in patients sustaining penetrating trauma. These patients are most likely to benefit from expedited transport if definitive surgical management is required.[7] Current literature has failed to study the association between pre-hospital transport time and survival for penetrating trauma patients. The studies that have examined the urban setting have yielded contradictory conclusions; Sloan and Petri in Chicago evaluated blunt and penetrating trauma patients and did not find a relationship between transport time and outcome.[8,9] Pepe in Houston assessed hypotensive patients with penetrating trauma and was unable to demonstrate any relationship.[10] Gervin and Feero, on the other hand, demonstrated that shorter pre-hospital time improved survival.[11,12] The contradictory results may be secondary to the heterogeneity of the trauma patient population at different locations. Trauma centers in many high-volume locations do not have significant number of penetrating trauma patients. This begs further investigation to define the influence of pre-hospital time factors on trauma outcomes in urban environments and in particular, in patients with penetrating trauma.
Our study explores the impact of pre-hospital times on penetrating trauma outcomes within urban centers of Illinois. We hypothesized that there would be a relationship between total pre-hospital time and outcomes in patients with penetrating thoracic trauma, an injury that is potentially lethal without emergent intervention. Since injury severity is strongly associated with mortality, we specifically studied the patients at highest risk, hypotensive patients who would be most likely to have hemorrhage that would benefit from rapid surgical control.[13]
MATERIALS AND METHODS
Data was obtained from the Illinois Trauma Registry between 1999 and 2003. This registry contains data from all traumatically injured patients brought to the 67 Level I and Level II Trauma Centers in Illinois. The data are entered by a registrar at each trauma center and uploaded to the Illinois Department of Public Health, who maintains the data set and website. Not included in this registry are patients who are declared dead-on-scene and not transported to a trauma center and patients not treated at or transferred to a Level I or Level II Trauma Center. The Emergency Medical System (EMS) in Illinois is a tiered system with paramedics trained in both Basic Life Support and Advanced Life Support techniques. The Chicago Committee on Trauma works with the state of Illinois and pre-hospital providers to ensure safe, standardized care and undergoes rigorous quality improvement scrutiny. Data on pre-hospital interventions are not included in this database. The data included werethe most recent data available at the time of the study. This study was approved by the Institutional Review Board of Northwestern University.
The Illinois State Trauma Registry (ISTR) includes approximately 45,000 records per year. To limit our study to urban trauma patients, we selected patients of all ages injured in the major urban areas of Chicago, East St. Louis, and Springfield (More than 2/3 of cases annually). Because our question of interest was the effect of transport time on mortality, we excluded all transfer patients, as well as walk-in and self-transport patients (10% of cases annually). We identified patients with penetrating injuries using information regarding the primary mechanism of injury recorded in the database (approximately 2,500 cases per year) and then classified those patients with thoracic trauma using ICD-9CM codes. The final list of ICD-9 codes was limited to penetrating thoracic injuries (codes 860-862, approximately 150 cases per year), consistent with the Center for Medicaid and Medicare Services (CMS) designations.[14] The pre-hospital vital sign data were poorly conserved with fifty percent missing; for that reason, “hypotension” was defined as a systolic blood pressure (SBP) less than 90 mmHg on the first reading in the Emergency Department. Total pre-hospital time consisted of response time, scene time, and transport time. Each of these variables was evaluated separately and in aggregate as total pre-hospital time.
Patient demographics along with injury details and outcomes were obtained. Bivariate and regression statistics were performed using STATA® statistical software (v9.2). Student's t-test was used as the test statistic for the comparisons of mean pre-hospital time between cohorts. The injury severity score (ISS) was used as an anatomic marker of injury severity and was highly conserved in the data set (<3% missing data). A two-sample test of proportions and Pearson's Chi-squared test were used to compare survival among patients with ISS <16 and ≥16 and total pre-hospital time. Logistic regression statistics were performed to determine the independent effect of transport time on mortality when controlling for age, race, and severity of injury for both hypotensive patients with penetrating thoracic injuries (HPTI) and non-hypotensive patients with penetrating thoracic injuries (NPTI). For the models, transport times were categorized into 15 min intervals to determine the independent effect of successively longer transport times.
RESULTS
A total of 908 patients with penetrating thoracic injuries (PTI)were evaluated during the study period. One-hundred forty-three patients (16%) were hypotensive on presentation, with a systolic blood pressure less than 90mmHg (hypotensive PTI group = HPTI), while 765 patients (84%) had systolic blood pressures greater than 90 mmHg (normotensive PTI group = NPTI). The majority of these injuries occurred in Chicago. The mean age was approximately 27 years (age range 11-78, 99% between ages 15 and 55) and the majority of patients were African American, male and uninsured [Table 1]. Thirty percent (230) of NPTI patients had an ISS greater than 16, while 55% (79) of HPTI patients had an ISS greater than 16 (P < 0.001).
Table 1.
Patient demographics
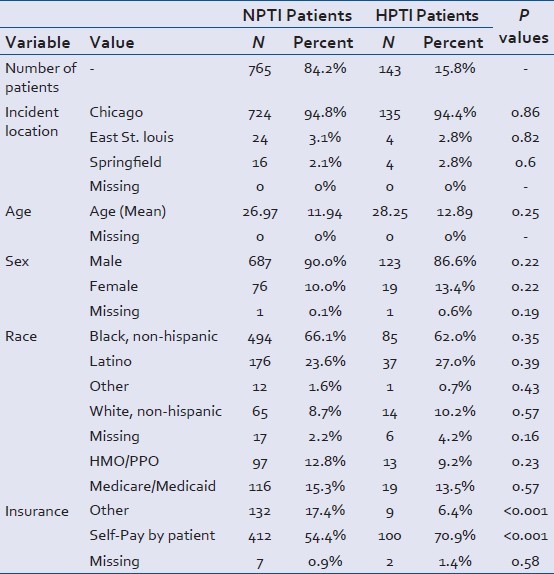
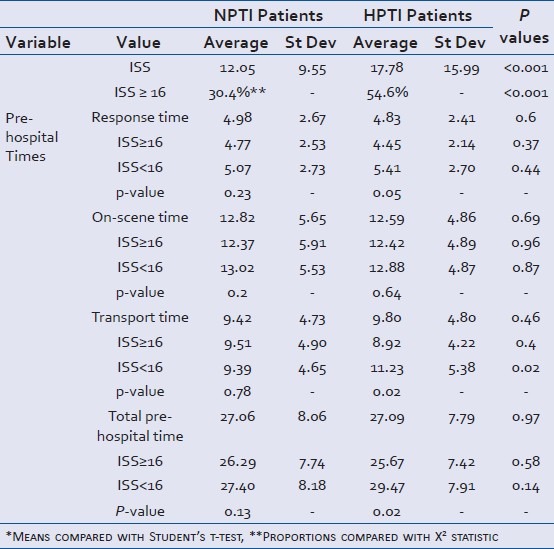
The time for paramedics to get to the scene (mean response time, 4.5 min vs. 5.4, P = 0.05), mean transport time (8.9 min vs. 11.2, P = 0.02) and total pre-hospital time (25.67 vs. 29.47, P = 0.02) were significantly shorter for HPTI patients with an ISS ≥ 16 compared to HPTI patients with ISS < 16. However, mean scene times did not differ (P = 0.64) [Table 2].
Table 2.
Injury severity and transport times, bivariate statistics
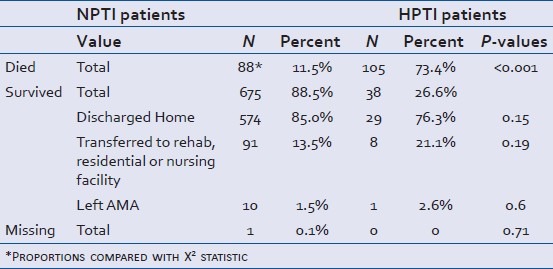
Crude mortality was higher for HPTI patients compared with NPTI patients (73% vs. 12%, P < 0.001). Hypotensive patients with penetrating thoracic injuries (HPTI) patients showed increased mortality with increased total pre-hospital time [Figure 1]. The odds ratio (OR) of death for HPTI patients, similarly, increased with increasing total pre-hospital time [Table 3, Figure 2]. For instance, if pre-hospital time was greater than 40 min, then the OR was increased to 13 (P < 0.001). Table 3 reports the regression results for HPTI patients. Non-hypotensive patients with penetrating thoracic injuries (NPTI) regression results are not included, but the covariates for age, race, gender, and ISS were of similar direction and magnitude. Conversely, NPTI patients with longer total pre-hospital times exhibited decreased mortality (OR 0.93, 95% CI 0.83-0.99, P < 0.001).
Figure 1.
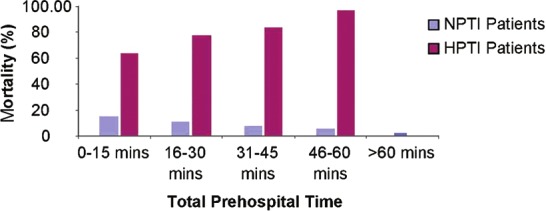
Death ratefor non-hypotensive patients with penetrating thoracic injuries and hypotensive patients with penetrating thoracic injuries patients grouped by pre-hospital time
Table 3.
Adjusted risk of death for HPTI patients by pre-hospital time
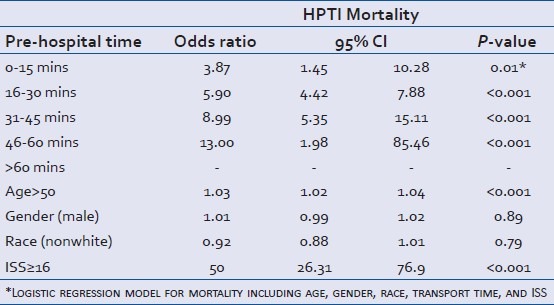
Figure 2.
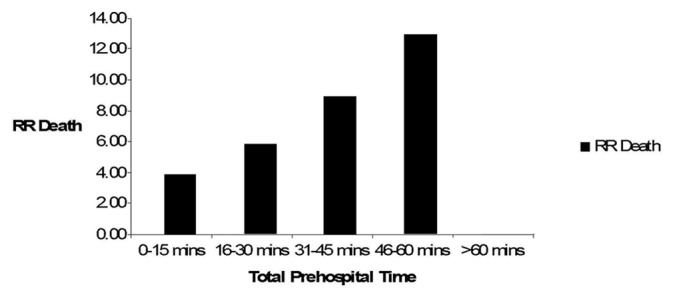
RR of death for hypotensive patients with penetrating thoracic injuries vs. non-hypotensive patients with penetrating thoracic injuries patients grouped by pre-hospital time
Of the survivors, the majority of patients, in both NPTI and HPTI groups, were discharged directly to home. There were no significant differences in the discharge destination for NTPI and HPTI patients [Table 4].
Table 4.
Discharge disposition, bivariate statistics
DISCUSSION
The study investigates association between transport time and outcome for urbanvictims of penetrating thoracic trauma. The analysis indicates that more severely injured patients may survive devastating injuries with rapid transit: The sicker the patient, the quicker they should be in the trauma bay. A significantly positive finding of this study was that patients with higher injury severity experienced shorter pre-hospital transport time. This finding in our study is not unique; Newgard demonstrated this in a multi-institutional study mixed population of blunt and penetrating trauma.[15] Given the significant correlation between pre-hospital time and mortality for HPTI patients, this is clearly a success of the urban trauma system.
The association of transport time with mortality has been well described in rural trauma systems, but never clearly described in the urban setting, with a homogeneous population of patients. This study is one of the first to show a consistent association between pre-hospital time and survival in an urban trauma system with uniform professional pre-hospital EMS care. These findings have important implications for trauma systems management. Variations in transport times might be due to travel distances to the nearest trauma center from incident scenes, traffic congestion or road conditions, or weather conditions. It is possible with new global positioning systems (GPS) data that incorporates traffic congestion and travel distances, pre-hospital times may be shortened. Some rural trauma systems have augmented their pre-hospital services with aeromedical transporter provided increased trauma training for first responders[16] to decrease the impact of longer transport times on injury mortality. These options might be employed to a greater degree in urban trauma systems as well. However, comprehensive changes in a system that is working well for most patients may not be indicated or cost-effective. It is important to note that our findings are limited to a small portion of all trauma patients: In our database, PTI patients comprised approximately 2% of all trauma patients and HPTI patients comprised only 0.4% of all trauma patients. It is likely that many, less severely injured will not experience a survival benefit associated with decreased pre-hospital time; as notably seen in the NPTI group, in whom survival was not adversely affected by increased transport time, and was actually improved. It is important to recognize that the majority of the overall trauma patient population with penetrating thoracic injuries did not benefit from shorter transport times. In addition, pre-hospital data were missing up to 50% of the time, including SBP. It is possible that pre-hospital HPTI patients might have different mortality rates. Finally, these data are now nearly 10 years old. Though no systematic changes have occurred in urban pre-hospital transport during that time, additional years of data should be accessed when available to validate these results.
Despite these limitations, these results suggest that careful planning to optimize transport time-encompassing hospital capacity and existing resources, traffic patterns, and trauma incident densities-may be beneficial in areas with a high burden of penetrating trauma.
CONCLUSION
In conclusion, we have shown that minimizing pre-hospital times does in fact impact survival in patients that are hypotensive victims of penetrating thoracic trauma.
HPTI patients in an optimally designed trauma system should be delivered to definitive care expeditiously.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lerner EB, Moscati RM. The golden hour: Scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8:758–60. doi: 10.1111/j.1553-2712.2001.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 2.Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: Final data for 2005. Natl Vital Stat Rep. 2008;56:1–120. [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 4.Sampalis JS, Denis R, Lavoie A, Fréchette P, Boukas S, Nikolis A, et al. Trauma care regionalization: A process-outcome evaluation. J Trauma. 1999;46:565–79. doi: 10.1097/00005373-199904000-00004. discussion 579-81. [DOI] [PubMed] [Google Scholar]
- 5.Grossman DC, Kim A, Macdonald SC, Klein P, Copass MK, Maier RV. Urban-rural differences in pre-hospital care of major trauma. J Trauma. 1997;42:723–9. doi: 10.1097/00005373-199704000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Esposito TJ, Maier RV, Rivara FP, Pilcher S, Griffith J, Lazear S, et al. The impact of variation in trauma care times: Urban versus rural. Prehosp Disaster Med. 1995;10:161–6. doi: 10.1017/s1049023x00041947. discussion 166-7. [DOI] [PubMed] [Google Scholar]
- 7.Nicholas JM, Rix EP, Easley KA, Feliciano DV, Cava RA, Ingram WL, et al. Changing patterns in the management of penetrating abdominal trauma: The more things change, the more they stay the same. J Trauma. 2003;55:1095–108. doi: 10.1097/01.TA.0000101067.52018.42. discussion 1108-10. [DOI] [PubMed] [Google Scholar]
- 8.Sloan EP, Callahan EP, Duda J, Sheaff CM, Robin AP, Barrett JA. The effect of urban trauma system hospital bypass on pre-hospital transport times and Level 1 trauma patient survival. Ann Emerg Med. 1989;18:1146–50. doi: 10.1016/s0196-0644(89)80049-6. [DOI] [PubMed] [Google Scholar]
- 9.Petri RW, Dyer A, Lumpkin J. The effect of pre-hospital transport time on the mortality from traumatic injury. Prehosp Disaster Med. 1995;10:24–9. doi: 10.1017/s1049023x00041625. [DOI] [PubMed] [Google Scholar]
- 10.Pepe PE, Wyatt CH, Bickell WH, Bailey ML, Mattox KL. The relationship between total pre-hospital time and outcome in hypotensive victims of penetrating injuries. Ann Emerg Med. 1987;16:293–7. doi: 10.1016/s0196-0644(87)80174-9. [DOI] [PubMed] [Google Scholar]
- 11.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med. 1995;13:133–5. doi: 10.1016/0735-6757(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 12.Gervin AS, Fischer RP. The importance of prompt transport of salvage of patients with penetrating heart wounds. J Trauma. 1982;22:443–8. doi: 10.1097/00005373-198206000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Demetriades D, Murray J, Charalambides K, Alo K, Velmahos G, Rhee P, et al. Trauma fatalities: Time and location of hospital deaths. J Am Coll Surg. 2004;198:20–6. doi: 10.1016/j.jamcollsurg.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Center for Medicare and Medicaid Services (CMS) U.S. Department of health and human services. 2012. Available from: http://www.cms.gov/medicare-coverage-database .
- 15.Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, et al. Emergency medical services intervals and survival in trauma: Assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55:235–46.e4. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corfield AR, Adams J, Nicholls R, Hearns S. On-scene times and critical care interventions for an aeromedical retrieval service. Emerg Med J. 2011;28:623–5. doi: 10.1136/emj.2010.091421. [DOI] [PubMed] [Google Scholar]


